Abstract
This report is aimed to describe a life-threatening case of anti-N-methyl-d-aspartate receptor (NMDAR) encephalitis secondary to ovarian teratoma with rapid recovery in 1 day after the removal of the tumour. A 23-year-old woman presented with sudden headache, personality changes and seizure. After neurological assessment, limbic or herpes encephalitis was provisionally diagnosed and treated with intravenous immunoglobulin, acyclovir and steroids. The patient had progressive severe neurological symptoms, requiring prolonged intubation and mechanical ventilation. An anti-NMDAR antibody test revealed positive in serum and cerebrospinal fluid at 3 weeks of admission. Pelvic ultrasound examination and CT scan revealed bilateral small ovarian teratomas. Bilateral ovarian cystectomy was performed by open surgery. The patient showed rapid improvement and no longer needed intubation 2 days after the operation. In conclusion, we described a catastrophic case of ovarian teratoma-associated encephalitis with delayed diagnosis but rapid recovery after ovarian cystectomy. This information can probably be helpful to neurologists and gynaecologists.
Background
Paraneoplastic encephalitis is a rare neurological disorder characterised by acute behavioural changes, seizures, disorientation and central hypoventilation. Several cases have been linked to ovarian teratoma which was first described in 1997.1 2 Until 2007, ovarian teratoma-associated paraneoplastic encephalitis was found to be related to an autoantibody, N-methyl-d-aspartate receptor (NMDAR) antibodies, which targets cell membrane antigens,3 4 affecting the central nervous system leading to subacute encephalopathy. The cerebrospinal fluid often shows evidence of inflammatory abnormalities, and neurological syndromes improve after tumour resection, immunotherapy or both. Though, during the past few years, several cases of ovarian teratoma-associated encephalitis have been reported,5–7 there are still a limited number of cases available on PubMed especially on gynaecology-related journals. According to a systematic review by Acien et al,8 including 119 articles consisting of 174 cases, it is concluded that ovarian teratoma-associated anti-NMDAR encephalitis is relatively unknown or not reported in many countries and among gynaecologists. Additionally, the disease is titre-dependent and has a variety of neurological or psychiatric manifestations with various degrees of severity from mild emotional changes to life-threatening, therefore a more number of cases with various clinical profiles are needed to add to the existing body of knowledge. The objective of this report is aimed to describe a life-threatening case of anti-NMDAR encephalitis secondary to ovarian teratoma with a rapid and complete recovery after the removal of the tumour and to encourage gynaecologists to thoroughly take history of neurological or psychiatric changes among patients with an ovarian mass and neurologists to be aware of ovarian teratoma among patients with such symptoms.
Case presentation
A 23-year-old Thai nulliparous woman was referred from a private hospital due to progressive severe encephalopathy without significant response to medical treatment. The patient presented with severe headache, personality changes and seizures which had suddenly developed with increasing severity for nearly 2 weeks prior to admission. Blood tests were unremarkable and MRI of the brain indicated no obvious abnormalities but the examination was suboptimal because of orthodontic braces. After neurological assessment and initial work-up, limbic or herpes encephalitis was provisionally diagnosed and treated with acyclovir and steroids as well as antiepileptic drugs. Nevertheless, after 2 weeks of medical treatment, the conditions started worsening. She developed apnoea and had progressively severe neurological symptoms, which required prolonged intubation and mechanical ventilation. The EEGs showed severe encephalopathy with status epilepticus. Cerebrospinal fluid examinations as well as serum viral analysis were unable to clarify the aetiology of the patient's symptoms. Anti-NMDAR encephalitis was considered as a potential diagnosis and paraneoplastic markers were tested. The anti-NMDAR antibody test revealed positive in serum and cerebrospinal fluid at 3 weeks of admission whereas other paraneoplastic markers were negative, including antineuronal nuclear antibody (ANNA)-1, ANNA-3, purkinje cell cytoplasmic antibody (PCA)-1, PCA-2, Pprkinje cell cytoplasmic antibody, Type Tr (PCA-Tr), glutamic acid decarboxylase (GAD), amphiphysin, collapsin response mediator protein (CRMP)-5, N-Methyl-D-aspartate (NMDA), 2-amino-3-(5-methyl-3-oxo-1,2-oxazol-4-yl) propanoic acid (AMPA), gamma-amino-butyric acid type B (GABA-b), Vvltage-gated potassium channel (VGKC) and signal recognition particle (SRP)-54. Since anti-NMDAR antibody could be associated with ovarian teratomas, pelvic ultrasound and whole abdomen CT scans were investigated, which showed bilateral small ovarian cystic teratomas, measuring 5.5×4.3 cm (right) and 2.6×2.2 cm (left; figure 1). Therefore, anti-NMDAR encephalitis secondary to ovarian teratomas was diagnosed and laparotomy was performed. Intraoperatively, the left and right ovaries were observed to be enlarged, as seen in the preoperative imaging, respectively. Bilateral ovarian cystectomy was performed by open surgery. The patient showed rapid improvement of her neurological symptoms and no longer needed intubation 2 days after operation. EEG on day 7 after surgery showed marked improvement when compared with that before surgery (figures 2 and 3). Pathological examination confirmed the diagnosis of a mature right ovarian cystic teratoma and left ovarian teratoma with small immature component (figures 4 and 5). There was no prominent intratumourous lymphoid infiltrates. The patient was also scheduled for a follow-up at the gynaecological oncology unit for immature teratoma grade I.
Figure 1.

Abdomen CT scan shows bilateral ovarian cysts suggestive of teratoma, measuring 5.5×4.3 cm (right) and 2.6×2.2 cm (left), note the calcifications in the right cyst (arrow head).
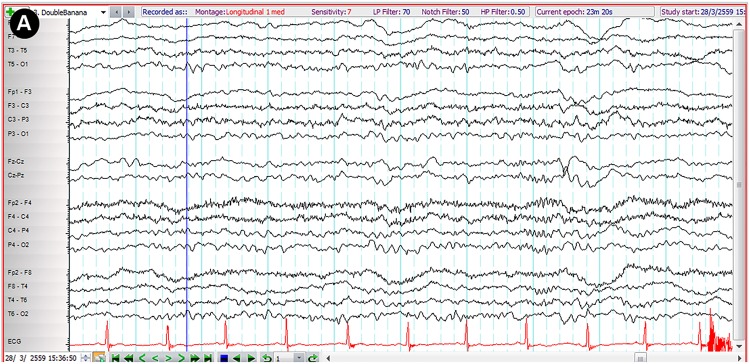
Figure 2.
EEG (before operation) shows continuous generalised δ activity. This is with severe diffuse encephalopathy.
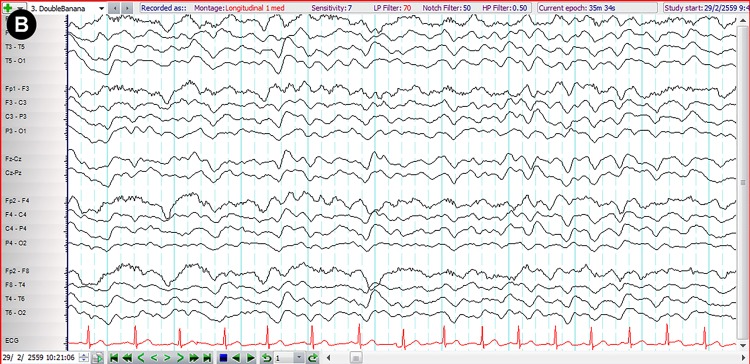
Figure 3.
EEG (at 1 week after operation) shows the background slowing, representing a mild degree of encephalopathy.
Figure 4.
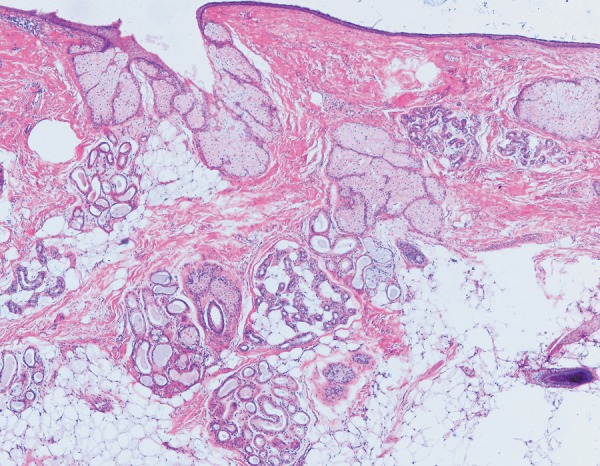
Pathological examination: the cyst is lined by skin with its appendages of the right ovary.
Figure 5.
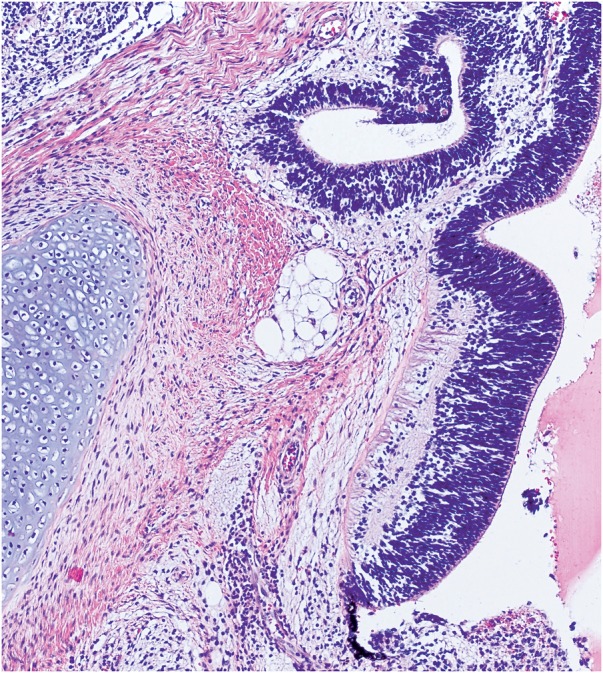
Pathological examination: the left ovarian tumour shows both immature neuroepithelial and mesenchymal components.
Outcome and follow-up
The patient was healthy without any serious sequelae on the follow-up visit at 6 weeks after operation
Discussion
Since its discovery in 2007, the encephalitis associated with anti-NMDAR has become an issue of interest in neurology. The signs and symptoms are generally non-specific, which makes the diagnosis difficult. Definite diagnosis is based on the detection of anti-NMDAR antibodies in serum and cerebrospinal fluid. Ovarian teratoma-related anti-NMDAR encephalitis is relatively rare but it is increasingly being recognised. More than 50% of patients with anti-NMDAR encephalitis aged more than 18 years exhibited teratomas.9 Based on the systematic review by Acien et al,8 the mean age of patients was 24 years, and mature teratoma was identified in most cases, sometimes microscopically following ovary removal or at autopsy. The clinical presentation featured psychiatric symptoms and behavioural changes, with a median delay for surgery of 28 days. Nearly 7% (12 out of 174 cases) of patients died, most frequently from encephalitis-related complications. NMDAR is a ligand-gated cation channel, consisting of NR1 and NR2 subunits, which play a crucial role in synaptic transmission and plasticity.10 Overactivation of the receptors may cause excitotoxicity, leading to the development of epilepsy, dementia and stroke. On the contrary, low NMDAR activity results in psychiatric symptoms like schizophrenia.11 Anti-NMDAR antibodies cause a titre-dependent, reversible decrease of synaptic NMDAR by a mechanism of cross-linking and internalisation. These antibody effects reveal a probable pathogenic relation between the depletion of receptors and the clinical features of anti-NMDAR encephalitis.12 The autoantibodies produced in patients with concurrent encephalitis and teratoma exhibit cross-reactivity with the NMDAR in the teratoma, binding to the NR subunits of NMDAR following entry into the cerebrospinal fluid. Gynaecologists should be aware that even a small ovarian teratoma can induce severe anti-NMDAR encephalitis and removal of the NMDAR-expressing tumour can effectively reduce the serum and cerebrospinal fluid levels of the anti-NMDAR autoantibody.13 Our case is one of the good examples of dramatic response to surgical removal in spite of the catastrophic one. The case presented here was relatively unique in terms of life-threatening severity because of delayed diagnosis and rapid as well as complete recovery after removal of the teratomas. We believe that the disorder is not uncommon and the prevalence is rather high as seen in the increasing number of reports in the past few years. Until recently the association was not known and a great number of cases might presumably have been categorised as encephalitis of unknown causes.
Based on this report and previous studies, an ovarian cystic teratoma is not always simple or benign in nature. Torsion, haemorrhage or infection complications are usually advocated, but neurological or psychiatric symptoms can also be more problematic than expected. The patients diagnosed for ovarian teratoma should be explored for neurological or psychiatric disorders and vice versa. Patients with paraneoplastic encephalitis or personality changes should also be aware of the possibility of ovarian teratoma. The earliest possible detection of ovarian teratoma is especially through transvaginal ultrasound, and surgical removal, as well as early immunotherapy, can shorten the course of disease, improve the survival rates and limit the adverse long-term consequences.
Different from many published cases, our case was very unusual in terms of rapid recovery. Though the reason for rapid response was unclear, several factors might be associated with such a favourable response, including: (1) the patient was young and healthy without any other underlying disease; (2) the tumour size was relatively small which was simply removed without residuals; and (3) there were no prominent lymphoid infiltrates in the tumour. According to previous reports, the degree of response was varied, from rapid complete recovery to incomplete recovery in some cases. Certainly other factors, particularly racial or immunological factors, may play an important role in the high variability of responses. There were no intratumour prominent lymphoid infiltrates in this case, which may partly be associated with a rapid response after tumour removal, since such lymphoid infiltrates are less responsive to surgical removal or even development of neurological symptoms after tumour resection,14 15 and possible infiltrates of extratumour lymphoid elements.
In summary, we described a catastrophic case of ovarian teratoma-associated encephalitis with delayed diagnosis but rapid and complete recovery after ovarian cystectomy. This information can probably be helpful to neurologists and gynaecologists.
Learning points.
Ovarian teratoma can produce antibodies (anti-N-methyl-d-aspartate receptor (NMDAR)) and can be complicated with paraneoplastic encephalitis.
Delayed diagnosis of an ovarian teratoma as a cause of encephalitis can result in a catastrophic outcome.
Anti-NMDAR encephalitis secondary to ovarian teratoma may probably have a good response to removal of the tumour with a rapid recovery.
Acknowledgments
The authors wish to thank the National Research University Project Thailand for financial support.
Footnotes
Contributors: CT was involved in the surgical removal of the tumour, medical review/record and manuscript preparation. AS was involved in neurological management and medical review/record. TP conducted the pathological examination. TT was involved in medical review/record and manuscript preparation.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Okamura H, Oomori N, Uchitomi Y. An acutely confused 15-year-old girl. Lancet 1997;350:488 10.1016/S0140-6736(97)06208-9 [DOI] [PubMed] [Google Scholar]
- 2.Nokura K, Yamamoto H, Okawara Y et al. Reversible limbic encephalitis caused by ovarian teratoma. Acta Neurol Scand 1997;95:367–73. [DOI] [PubMed] [Google Scholar]
- 3.Dalmau J, Tuzun E, Wu HY et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007;61:25–36. 10.1002/ana.21050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tonomura Y, Kataoka H, Hara Y et al. Clinical analysis of paraneoplastic encephalitis associated with ovarian teratoma. J Neurooncol 2007;84:287–92. 10.1007/s11060-007-9372-9 [DOI] [PubMed] [Google Scholar]
- 5.Imai K, Fukuda T, Wada T et al. Complete recovery from paraneoplastic anti-NMDAR encephalitis associated with a small ovarian teratoma following a laparoscopic salpingo-oophorectomy: a case report. Exp Ther Med 2015;9:1723–6. 10.3892/etm.2015.2344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li S, Zhao A. A case of anti-NMDAR encephalitis induced by ovarian teratoma. Cell Biochem Biophys 2015;71:1011–14. 10.1007/s12013-014-0302-0 [DOI] [PubMed] [Google Scholar]
- 7.Liu H, Jian M, Liang F et al. Anti-N-methyl-D-aspartate receptor encephalitis associated with an ovarian teratoma: two cases report and anesthesia considerations. BMC Anesthesiol 2015;15:150 10.1186/s12871-015-0134-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acien P, Acien M, Ruiz-Macia E et al. Ovarian teratoma-associated anti-NMDAR encephalitis: a systematic review of reported cases. Orphanet J Rare Dis 2014;9:157 10.1186/s13023-014-0157-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Florance NR, Davis RL, Lam C et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 2009;66:11–18. 10.1002/ana.21756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch DR, Anegawa NJ, Verdoorn T et al. N-methyl-D-aspartate receptors: different subunit requirements for binding of glutamate antagonists, glycine antagonists, and channel-blocking agents. Mol Pharmacol 1994;45:540–5. [PubMed] [Google Scholar]
- 11.Dalmau J, Gleichman AJ, Hughes EG et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–8. 10.1016/S1474-4422(08)70224-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dalmau J, Lancaster E, Martinez-Hernandez E et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 2011;10:63–74. 10.1016/S1474-4422(10)70253-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seki M, Suzuki S, Iizuka T et al. Neurological response to early removal of ovarian teratoma in anti-NMDAR encephalitis. J Neurol Neurosurg Psychiatr 2008;79:324–6. 10.1136/jnnp.2007.136473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabata E, Masuda M, Eriguchi M et al. Immunopathological significance of ovarian teratoma in patients with anti-N-methyl-d-aspartate receptor encephalitis. Eur Neurol 2014;71:42–8. 10.1159/000353982 [DOI] [PubMed] [Google Scholar]
- 15.Dabner M, McCluggage WG, Bundell C et al. Ovarian teratoma associated with anti-N-methyl D-aspartate receptor encephalitis: a report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol 2012;31:429–37. 10.1097/PGP.0b013e31824a1de2 [DOI] [PubMed] [Google Scholar]