Abstract
Objectives. We assessed whether e-cigarette use is associated with (1) intention to smoke cigarettes among never-smoking youths and youth experimenters, and (2) intention to quit smoking among current youth smokers.
Methods. We categorized participants from the 2012 National Youth Tobacco Survey data (n = 20 193) as never-smoking youth (n = 16 238), youth experimenters (n = 3248), and current youth smokers (n = 707). We matched groups on the basis of a propensity score comprising covariates predicting e-cigarette use.
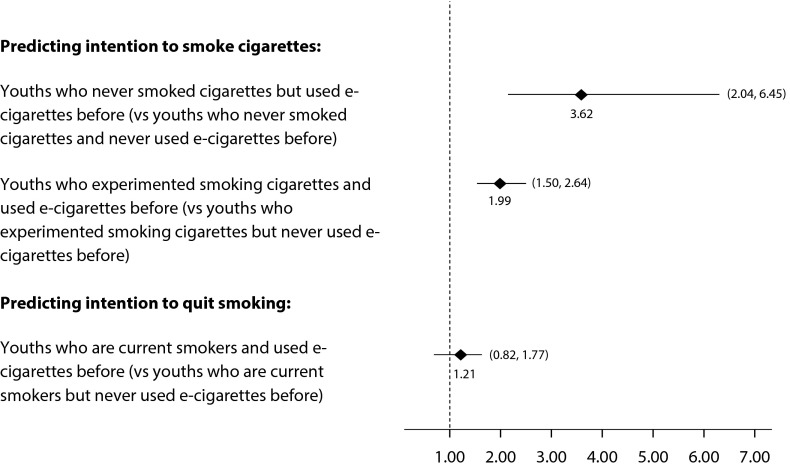
Results. E-cigarette users who had never smoked cigarettes (adjusted odds ratio [AOR] = 3.62; 95% confidence interval [CI] = 2.04, 6.45) and who had experimented with smoking (AOR = 1.99; 95% CI = 1.50, 2.64) had elevated intention to smoke cigarettes compared with their counterparts who had never used e-cigarettes. We did not find any significant association between e-cigarette use and intention to quit smoking among current youth smokers (P = .33).
Conclusions. E-cigarette use among US youths is associated with intention to smoke but not with intention to quit smoking.
In 2014, the 30-day prevalence of e-cigarette use in the United States was 8.7%, 16.2%, and 17.1% among 8th, 9th, and 12th grade students, respectively, which surpassed corresponding prevalence for tobacco cigarette use (4.0%, 7.2%, and 13.6%).1 With the dramatic increase in e-cigarette use, e-cigarettes are rapidly becoming an urgent public health concern in the United States. Specifically, whether e-cigarette use is potentially related to other tobacco use or tobacco cessation is currently a subject of contentious debate in public health.
Although no longitudinal studies have directly measured the relationship between e-cigarette use and the likelihood of being a smoker, a 3-year cross-sectional study revealed that e-cigarette use was associated with an increased intention to smoke cigarettes among never-smoking middle and high school students in the United States.2 However, other researchers contend that e-cigarettes may be a useful smoking cessation aid for smokers. Several studies have examined the effectiveness of e-cigarettes as a tool for quitting. A 6-month prospective pilot study showed that e-cigarette use was associated with an increased likelihood of quitting.3 Among 40 smokers, 13 participants (32.5%) reduced their cigarette consumption by at least 50%, and 9 participants (22.5%) completely quit smoking at the 6-month follow-up.
Another study reported that a 6-month point prevalence of smoking abstinence among e-cigarette users in the sample was 31%; smoking abstinence rates were positively related to higher frequency of e-cigarette use; and 70% of heavy e-cigarette users in the sample (i.e., using e-cigarettes more than 20 times a day) quit smoking at 6 months.4 One study assessing the short-term effect of e-cigarette use on desire to smoke found that use of e-cigarettes containing 16 milligrams of nicotine alleviated the craving to smoke after overnight abstinence.5 However, the efficacy of e-cigarette use as a smoking cessation tool is not conclusive. A 1-year follow-up study at the population level determined that smokers’ e-cigarette use was not related to either quitting or reduced cigarette consumption.6 Furthermore, e-cigarette use has not been shown to be associated with the intention to quit smoking among current cigarette smokers.7
From a public health perspective, learning more about the potential harms and benefits of e-cigarette use in the context of tobacco control and prevention is essential. To date, few studies have examined the potential role of e-cigarette use in quitting or initiating cigarette smoking. To address this critical gap, studies with a more rigorous design are necessary. Propensity score matching (PSM) is a useful statistical technique for estimating treatment effects by balancing covariates in experimental and control groups to reduce selection bias.8 PSM is predicated on the idea that the bias is reduced when the comparison of outcomes is performed between treated and control participants who are as similar as possible, resulting in a more accurate estimation of treatment effects.9
To date, no research has been conducted to establish whether e-cigarette use is associated with intention to smoke or quit smoking in a nationally representative sample of adolescents in the United States using the PSM approach. We used PSM to investigate (1) whether e-cigarette use is associated with future intention to smoke cigarettes among never-smoking youths and youth experimenters, and (2) whether e-cigarette use is associated with intention to quit smoking among current youth smokers in a nationally representative sample of adolescents in the United States.
METHODS
We obtained the data for this study from the 2012 National Youth Tobacco Survey (NYTS; n = 20 193). The NYTS is a nationally representative school-based survey for collecting data about tobacco use from US middle and high school students in grades 6 through 12. The NYTS provides in-depth information about tobacco use behaviors, tobacco-related beliefs and attitudes, and exposure to pro- and antitobacco influences among youths.
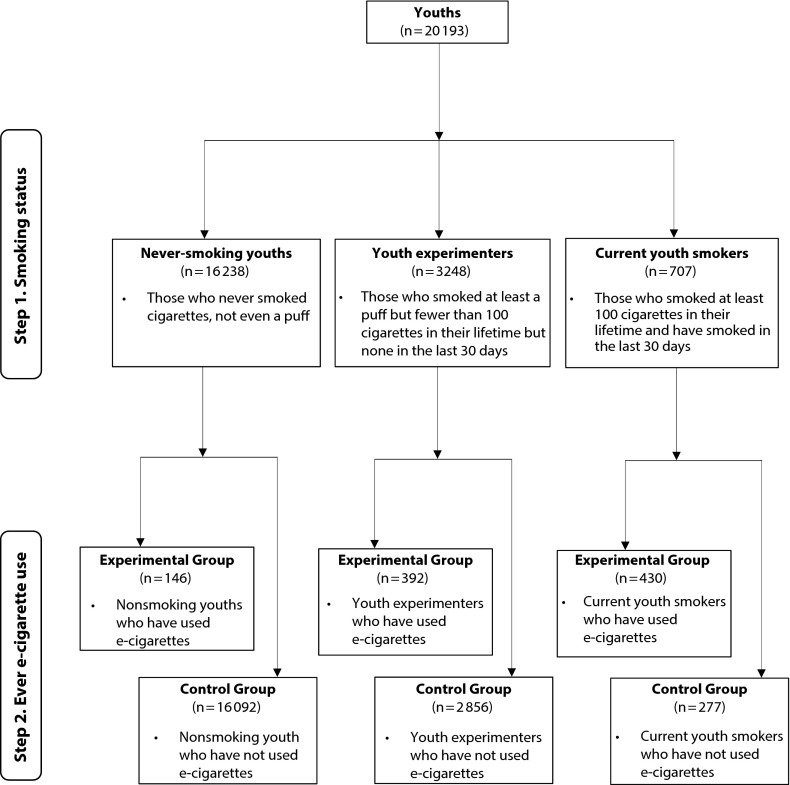
We divided study participants from the 2012 NYTS into 3 groups on the basis of smoking status: (1) never-smoking youths (n = 16 238), who were further broken down into 146 ever e-cigarette users and 16 092 never e-cigarette users; (2) youths experimenters (n = 3248), with 392 ever e-cigarette users and 2856 never e-cigarette users; and (3) current youth smokers (n = 707), with 430 ever e-cigarette users and 277 never e-cigarette users. Never-smoking youths are those who had never smoked cigarettes, not even a puff.10 Experimenters are youths who had smoked at least a puff but fewer than 100 cigarettes in their lifetime but none in the past 30 days.10 Current youth smokers are those who had smoked at least 100 cigarettes in their lifetime and had smoked in the past 30 days.10 In each group, individuals who have ever tried e-cigarettes comprised the experimental group, whereas individuals who have never tried e-cigarettes comprised the control group (Figure 1).
FIGURE 1—
Flow Diagram of Control vs Experimental Group Selection: National Youth Tobacco Survey, United States, 2012
Measures
Study participants were asked, “Have you ever used e-cigarettes such as Ruyan, NJOY or Blu?” We classified individuals as ever e-cigarette users if they answered “yes” and as never e-cigarette users if they answered “no.”
Outcomes.
There were 2 dependent variables for this study. One was intention to smoke cigarettes among never-smoking youths and youth experimenters. The other was intention to quit smoking among current youth smokers. We measured intention to smoke cigarettes among never-smoking youths and youth experimenters as an ordinal variable on the basis of an NYTS questionnaire item: “Do you think you will try a cigarette soon?” Response options were “definitely no,” “probably no,” “probably yes,” and “definitely yes.” We also measured intention to quit smoking among current youth smokers as an ordinal variable on the basis of an NYTS questionnaire item: “Are you seriously thinking about quitting cigarettes?” Response options were “no,” “yes, but not within the year,” “yes, within the year,” “yes, within the next 6 months,” and “yes, within the next 30 days.”
Covariates.
We included several covariates on the basis of previous literature.2,6,11–13 The covariates we included to test the intention to smoke cigarettes were age, gender (male and female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, or other), having a positive attitude toward smoking (e.g., “Smoking cigarettes makes young people look cool or fit in” and “Young people who smoke cigarettes have more friends”), having a negative attitude toward smoking (e.g., “All tobacco products are dangerous”), self-efficacy (e.g., “If one of your friends were to offer you a cigarette, would you smoke it?”), and exposure to tobacco advertising (e.g., “When using the Internet/newspaper or magazine, how often do you see ads for cigarettes and other tobacco products?”).
The covariates we included to test the intention to quit smoking cigarettes were age, gender, race/ethnicity, having positive or negative attitudes toward smoking, self-efficacy (e.g., “If one of your friends were to offer you a cigarette, would you smoke it?” and “If you try to quit smoking cigarettes, how likely are you to succeed?”), age of smoking onset, frequency of smoking (< 1 cigarette per day, 2–5 cigarettes per day, 6–10 cigarettes per day, 11–20 cigarettes per day, > 20 cigarettes per day), and past quit attempts (did not try quit during 12 months, 1 time, 2 times, 3–5 times, 6–10 times, or ≥ 10 times).
Statistical Analysis
A propensity score (PS) is a predicted probability that a participant receives the treatment because of his or her baseline measurements.14 PS matching attempts to create matched sets of treated and untreated participants who show similar values of the PS.15–17 In optimal matching, a matched sample that minimizes the total within-pair difference of the PS is formed.17 Once the matched sample has been formed, the treatment effect can be estimated by comparing outcomes between the treated and untreated participants in the matched sample.17
Propensity score estimation.
To estimate PS, or the estimated probability of using e-cigarettes, we performed logistic regression analyses. To help specify a correct PS model, we applied a stepwise logistic regression to include all important conditioning variables in the model. Specifically, as suggested in Rosenbaum,14 we included covariates whose group differences met a low threshold for significance (t > 1.5; P = .134). We evaluated differences on observed covariates using the t test for continuous variables and the χ2 test for categorical variables. As a result, we included gender, age, self-efficacy, having positive or negative attitudes toward smoking, and exposure to tobacco advertising in the logistic regression analyses to estimate PS among never-smoking youths. We included race/ethnicity, age, and exposure to tobacco advertising in the logistic regression analyses to estimate PS among youth experimenters. For current youth smokers, we included gender, race/ethnicity, self-efficacy, having a positive attitude toward smoking, and frequency of smoking in the logistic regression analyses to estimate PS.
Optimal matching.
Because nearest neighbor within caliper matching or greedy matching fails if there is no sizable common support region (i.e., overlap of estimated PS between experimental and control groups),18 we examined the common support region through boxplots and histograms. We found that the common support region was too narrow to permit greedy matching.18 As an alternative, we chose optimal matching, which substantially reduces the narrow common support region problem as a matching method.18
To select the best method among the 3 types of optimal matching (i.e., optimal pair matching, optimal variable matching, and optimal full matching),19 we examined the total sample distance of PS for each type of matching and chose the method that produced the smallest total distance. As a result, we used 2 types of matching: optimal pair matching using the Optmatch package in R version 3.2.0 (R Foundation for Statistical Computing, Vienna, Austria) for never-smoking youths and youth experimenters and optimal full matching using the MatchIt package in R version 3.2.0 for current youth smokers. Unlike optimal pair matching, optimal full matching creates a series of matched sets in which each participant in the experimental group is matched to 1 or more participants in the control group.
Imbalance check.
An important step in PSM is to check imbalance on observed covariates between the experimental and control groups. For each matching attempt, we conducted an imbalance test to confirm the statistical equivalence between ever e-cigarette users and never e-cigarette users by comparing absolute standardized difference for each covariate before and after matching, as suggested by Haviland et al.20 The absolute standardized difference for each covariate typically declines after matching. We performed imbalance checks at the 0.01 level owing to the multiple comparisons for the same data set using the IMBALANCE command developed by Guo21 in Stata version 13 (StataCorp LP, College Station, TX).
Ordinal logistic regression analyses.
We performed ordinal logistic regression analyses on each matched sample to predict ordinal dependent variables. We computed adjusted odds ratios (AORs) with 95% confidence intervals (CIs) to examine intention to smoke cigarettes among never-smoking youths and youth experimenters and intention to quit smoking among current youth smokers using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Descriptive statistics for each study sample are available as a supplement to the online version of this article at http://www.ajph.org as Tables A and B. The pair-matching procedure matched 146 ever e-cigarette users to the 146 never e-cigarette users among never-smoking youths, and 392 ever e-cigarette users to the 392 never e-cigarette users among youth experimenters. The full matching procedure matched 430 ever e-cigarette users and 277 never e-cigarette users among current youth smokers. Matched ever e-cigarette users and never e-cigarette users in each study sample did not differ significantly on observed covariates.
Table 1 provides ordinal logistic regression results for predicting intention to smoke cigarettes among never-smoking youths. Ever e-cigarette use and having a positive attitude toward smoking and self-efficacy were associated with future intention to smoke cigarettes among never-smoking youths. Ever e-cigarette users who had never smoked cigarettes were more likely to have intention to smoke cigarettes than were never e-cigarette users who had never smoked cigarettes (AOR = 3.62; 95% CI = 2.04, 6.45). Never-smoking youths who believed that smoking cigarettes makes young people look cool or fit in were more likely to have intention to smoke cigarettes than were their counterparts in the fully adjusted model (AOR = 2.32; 95% CI = 1.08, 4.95).
TABLE 1—
Odds Ratios of Intention to Smoke Cigarettes Among Never-Smoking Youths and Youth Experimenters: National Youth Tobacco Survey, United States, 2012
| Variable | Never-Smoking Youths, AOR (95% CI) | Youth Experimenters, AOR (95% CI) |
| Ever e-cigarette use | ||
| Experimental group | 3.62 (2.04, 6.45) | 1.99 (1.50, 2.64) |
| Control group (Ref) | 1 | 1 |
| Gender | ||
| Female | 0.61 (0.34, 1.09) | 1.18 (0.89, 1.57) |
| Male (Ref) | 1 | 1 |
| Age | 1.06 (0.92, 1.21) | 1.06 (0.97, 1.15) |
| Race/ethnicity | ||
| Non-Hispanic White | 0.65 (0.33, 1.30) | 1.29 (0.91, 1.82) |
| Non-Hispanic Black | 0.71 (0.26, 1.93) | 0.35 (0.19, 0.66) |
| Hispanic (Ref) | 1 | 1 |
| Other | 2.05 (0.73, 5.74) | 0.84 (0.38, 1.87) |
| Positive attitude toward smoking | ||
| Smoking cigarettes makes young people look cool or fit in | ||
| Yes | 2.32 (1.08, 4.95) | 2.20 (1.49, 3.26) |
| No (Ref) | 1 | 1 |
| Young people who smoke cigarettes have more friends | ||
| Yes | 0.85 (0.43,1.69) | 1.04 (0.72, 1.52) |
| No (Ref) | 1 | 1 |
| Negative attitude toward smoking | ||
| All tobacco products are dangerous | ||
| Agree | 0.48 (0.20, 1.13) | 0.81 (0.53, 1.24) |
| Disagree (Ref) | 1 | 1 |
| Self-efficacy | ||
| If a friend offers me a cigarette, I would smoke it | ||
| Yes | 30.31 (10.97, 83,76) | 17.88 (12.13, 26.34) |
| No (Ref) | 1 | 1 |
| Exposure to tobacco advertising | ||
| How often I see cigarettes ads when using the Internet | ||
| Never (Ref) | 1 | 1 |
| Sometimes | 0.91 (0.41, 1.99) | 1.21 (0.77, 1.90) |
| Most of time | 1.40 (0.54, 3.65) | 0.94 (0.53, 1.65) |
| How often I see cigarette ads when reading a newspaper or magazine | ||
| Never (Ref) | 1 | 1 |
| Sometimes | 1.51 (0.75, 3.03) | 1.10 (0.76, 1.61) |
| Most of time | 1.04 (0.43, 2.51) | 1.17 (0.70, 1.95) |
Note. AOR = adjusted odds ratio; CI = confidence interval.
Table 1 also provides the results of ordinal logistic regression analyses predicting intention to smoke cigarettes among youth experimenters. Again, ever e-cigarette use and race/ethnicity, positive attitude toward smoking, and self-efficacy were associated with future intention to smoke cigarettes among youth experimenters. Ever e-cigarette users who had experimented with smoking were more likely to have intention to smoke cigarettes than were never e-cigarette users who had experimented with smoking (AOR = 1.99; 95% CI = 1.50, 2.64). Non-Hispanic Blacks had lower intention to smoke cigarettes than did Hispanics, adjusting for all other covariates (AOR = 0.35; 95% CI = 0.19, 0.66).
Table 2 presents the results of ordinal logistic regression analyses predicting intention to quit smoking among current youth smokers. Having a negative attitude toward smoking, self-efficacy, number of past quit attempts, and age of smoking onset were associated with intention to quit smoking among current youth smokers. Current youth smokers who responded that they would smoke a cigarette if a friend offered it to them had lower intention to quit smoking than did their counterparts (AOR = 0.18; 95% CI = 0.05, 0.66). A higher level of self-efficacy of quitting (AOR = 1.38; 95% CI = 1.18, 1.62), more quit attempts (AOR = 1.55; 95% CI = 1.40, 1.72), and older age of smoking onset (AOR = 1.10; 95% CI = 1.02, 1.19) were positively associated with increased odds of considering quitting in the fully adjusted model. However, we found no significant association between e-cigarette use and intention to quit smoking among current youth smokers.
TABLE 2—
Odds Ratios of Intention to Quit Smoking Among Current Youth Smokers: National Youth Tobacco Survey, United States, 2012
| Variable | AOR (95% CI) |
| Ever e-cigarette use | |
| Experimental group | 1.21 (0.82, 1.77) |
| Control group (Ref) | 1 |
| Gender | |
| Female | 0.71 (0.49, 1.03) |
| Male (Ref) | 1 |
| Age | 1.00 (0.88, 1.14) |
| Race/ethnicity | |
| Non-Hispanic White | 1.20 (0.71, 2.03) |
| Non-Hispanic Black | 2.23 (0.95, 5.24) |
| Hispanic (Ref) | 1 |
| Others | 1.16 (0.55, 2.44) |
| Positive attitude toward smoking | |
| Smoking cigarettes makes young people look cool or fit in | |
| Yes | 0.65 (0.42, 1.02) |
| No (Ref) | 1 |
| Young people who smoke cigarettes have more friends | |
| Yes | 1.08 (0.68, 1.74) |
| No (Ref) | 1 |
| Negative attitude toward smoking | |
| All tobacco products are dangerous | |
| Agree | 4.06 (2.56, 6.43) |
| Disagree (Ref) | 1 |
| Self-efficacy | |
| If a friend offered me a cigarette, I would smoke it | |
| Yes | 0.18 (0.05, 0.66) |
| No (Ref) | 1 |
| If you try to quit smoking cigarettes, how likely are you to succeeda | 1.38 (1.18, 1.62) |
| Age of smoking onset | 1.10 (1.02, 1.19) |
| Frequency of smoking | 0.94 (0.80, 1.10) |
| No. past quit attempts | 1.55 (1.40, 1.72) |
Note. AOR = adjusted odds ratio; CI = confidence interval.
Self-efficacy item “If you try to quit smoking cigarettes, how likely are you to succeed” was on a 0–3 scale (0 = very unlikely, 1 = somewhat unlikely, 2 = somewhat likely, and 3 = very likely).
DISCUSSION
Our results reveal a close link between e-cigarette use among US youths and intention to smoke cigarettes in the future. That is, ever e-cigarette users who had never smoked traditional cigarettes or who had experimented with smoking were more likely to have intention to smoke cigarettes in the future than were their counterparts who never used e-cigarettes in a nationally representative sample of US adolescents. By contrast, ever e-cigarette use among current youth smokers was not associated with intention to quit smoking in the same nationally representative sample (Figure 2).
FIGURE 2—
Adjusted Odds Ratios of E-Cigarette Use Predicting Intention to Smoke or Quit Smoking: National Youth Tobacco Survey, United States, 2012
Note. Diamonds represent adjusted odds ratios. Lines represent 95% confidence intervals. We adjusted odds ratios for all the covariates included in each ordinal logistic model, such as gender, age, race/ethnicity, having a positive or negative attitude toward smoking, self-efficacy, and exposure to tobacco advertising. We additionally controlled age of smoking onset, frequency of smoking, and past quit attempts when predicting intention to quit.
Because of the finding of the association between ever e-cigarette use and intention to smoke, identifying risk factors associated with both e-cigarette use and conventional cigarette uptake is important for preventing the development of multiple risk behaviors over the course of adolescence. Previous research found that the odds of having multiple risk behaviors increase over the course of adolescence.22 Indeed, a study of a sample of 10 645 American youths found that 8% of youths aged 12 to 13 years engaged in multiple risk behaviors, whereas 33% of those aged 14 to 17 years and 50% of those aged 18 to 21 years did so.23 Of the multiple risk behaviors, tobacco use appears to be crucial in explaining other risk behaviors. One study found that early onset of smoking (i.e., by aged 11 years) explained 22% of the variance in all other risk behaviors in a sample of adolescents.24
A recent study found that e-cigarette use is associated with risk factors resembling those of conventional cigarette uptake.25 For example, familial socioeconomic disadvantage, vocational school career, and poor school performance were all positively associated with both e-cigarette experimentation and progression to conventional cigarette uptake among Finnish adolescents.25,26 Taken together, tailored interventions aiming to reduce the common set of risk factors associated with both e-cigarette use and conventional cigarette uptake may play a significant role in preventing multiple risk behaviors among youths. Furthermore, intervention efforts that aim to prevent adolescents from initiating smoking conventional cigarettes may help thwart e-cigarette use.
Currently, federal law in the United States does not regulate e-cigarettes. In 2014, the US Food and Drug Administration released a “deeming rule” that would extend authority to regulate additional tobacco-related products, including e-cigarettes. If the deeming rule is adopted, the Food and Drug Administration will regulate the manufacture, marketing, and distribution of e-cigarettes. In the absence of federal law governing e-cigarettes, state laws, such as youth access restriction, smoke-free air laws, and excise taxation, regulate e-cigarettes. As of November 30, 2014, 40 states have laws prohibiting sales of e-cigarettes to minors (younger than 18 years, except in 4 states, Alabama, Alaska, New Jersey, and Utah, where minors are defined as younger than 19 years).27
Only 3 states, New Jersey, North Dakota, and Utah, prohibit the use of e-cigarettes in 3 indoor areas: private worksites, restaurants, and bars.27 Minnesota (in 2012) and North Carolina (in 2014) passed a law imposing an excise tax on e-cigarettes.28 A notable fact about state laws governing e-cigarettes is that youth access restriction plays a major role in regulating e-cigarettes in 40 US states, recognizing that youths are a particularly vulnerable population. Adolescence is a critical period in terms of onset of smoking habits. Of the adults who became daily smokers, 88% started smoking by age 18 years and 99% by age 26 years.29 Thus, policymakers should make a continuous effort to regulate e-cigarettes, as traditional tobacco products are, at the federal level. In particular, all states should initiate prohibiting e-cigarette sales to youths as a means of preventing youth access to e-cigarettes.
Contrary to a previous study, which reported that e-cigarette users claim that they used e-cigarettes to quit smoking or avoid relapse,30 our study findings indicate that e-cigarette use may not be related to intention to quit smoking among current youth smokers. Although this finding is contradictory to the reported benefits of e-cigarettes as a potential cessation aid,3–5,30 it should be noted that such reported benefits of e-cigarettes has not been fully established owing, in large part, to a lack of research evidence because e-cigarettes have been in existence for a relatively short period of time.
What is concerning is that the frequency of online searches for e-cigarettes as a smoking cessation aid has surpassed that of snus and nicotine replacement therapy, which have been on the market longer than have e-cigarettes as a cessation aid and are quickly outpacing varenicline (a.k.a., Chantix), one of the most common prescription medications to help quit smoking in the United States.31 This may reflect massive online marketing of e-cigarettes, which states that “e-cigarette are healthier than conventional cigarettes” and “e-cigarettes are a smoking cessation aid.”32(p141),33(p3),34(p553) However, it is unclear whether e-cigarettes are a safe alternative to conventional cigarettes.35 One study found that e-cigarettes generally require a stronger vacuum to enable inhaling than do conventional tobacco products.36 Therefore, careful consideration should be given to the role of e-cigarettes in tobacco cessation among current youth smokers.
This study has limitations. Caution is warranted in inferring a causal relationship between e-cigarette use and intention to smoke or not to smoke among youths because data were obtained from cross-sectional data. Because of the lack of temporality, it is plausible that youths who already had a strong intention to smoke cigarettes experimented with e-cigarettes instead of conventional cigarettes. Future studies using a prospective longitudinal design would be desirable to corroborate the findings of our study.
It is also important to note that the e-cigarette market is changing and growing rapidly and, thus, more recent data are needed to estimate the impact of e-cigarettes on intention to smoke or quit smoking among US youths. Furthermore, there might have been unobserved confounding factors that influenced e-cigarette use, which might have reduced matching efficiency. We used 2 different optimal matching techniques (optimal pair matching and optimal full matching), which minimized the total distance to achieve a finely balanced match.37 The results may be affected by our choice of matching algorithm in small samples; however, as sample size increases, all the PSM estimators will eventually yield the same results.38–40 Considering that our sample size is sufficiently large, it can be assumed that our use of the 2 different optimal matching techniques likely did not affect our findings.
Despite these limitations, our study contributes to the literature in a significant manner. We investigated the potential role of e-cigarette use in intention to smoke or quit smoking in a nationally representative sample of US youths using PSM, yielding statistically sound results that enhance causal plausibility with nonexperimental designs. Because of our finding that e-cigarette use among US youths was related to future intention to smoke, strong enforcement measures should be taken to prevent youths from accessing and using e-cigarettes.
ACKNOWLEDGMENTS
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (award NRF-2015S1A3A2046566).
Note. The funding source had no role in the study design, collection, analysis or interpretation of the data, writing the article, or the decision to submit the article for publication.
HUMAN PARTICIPANT PROTECTION
This study was exempt from institutional review because the data are publically available.
REFERENCES
- 1.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future. National Survey Results on Adolescent Drug Use: 1975–2014. 2014 Overview. Key Findings on Adolescent Drug Use. Ann Arbor, MI: University of Michigan Institute for Social Research; 2015. [Google Scholar]
- 2.Bunnell RE, Agaku IT, Arrazola RA et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine Tob Res. 2015;17(2):228–235. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polosa R, Caponnetto P, Morjaria JB, Papale G, Campagna D, Russo C. Effect of an electronic nicotine delivery device (e-cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786. doi: 10.1186/1471-2458-11-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel MB, Tanwar KL, Wood KS. Electronic cigarettes as a smoking-cessation: tool results from an online survey. Am J Prev Med. 2011;40(4):472–475. doi: 10.1016/j.amepre.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Bullen C, McRobbie H, Thornley S, Glover M, Lin R, Laugesen M. Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tob Control. 2010;19(2):98–103. doi: 10.1136/tc.2009.031567. [DOI] [PubMed] [Google Scholar]
- 6.Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med. 2014;174(5):812–813. doi: 10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sutfin EL, McCoy TP, Morrell HE, Hoeppner BB, Wolfson M. Electronic cigarette use by college students. Drug Alcohol Depend. 2013;131(3):214–221. doi: 10.1016/j.drugalcdep.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 9.Becker SO, Ichino A. Estimation of average treatment effects based on propensity scores. Stata J. 2002;2(4):358–377. [Google Scholar]
- 10.Choi WS, Pierce JP, Gilpin EA, Farkas AJ, Berry CC. Which adolescent experimenters progress to established smoking in the United States. Am J Prev Med. 1997;13(5):385–391. [PubMed] [Google Scholar]
- 11.Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’ in the USA. Tob Control. 2013;22(1):19–23. doi: 10.1136/tobaccocontrol-2011-050044. [DOI] [PubMed] [Google Scholar]
- 12.Ambrose BK, Rostron BL, Johnson SE et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2, suppl 1):S53–S60. doi: 10.1016/j.amepre.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bullen C, Howe C, Laugesen M et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum RR. Observational Studies. 2nd ed. New York, NY: Springer-Verlag; 2002. [Google Scholar]
- 15.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 16.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39(1):33–38. [Google Scholar]
- 17.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grinstein-Weiss M, Manturuk KR, Guo S, Charles P, Key C. The impact of homeownership on marriage and divorce: evidence from propensity score matching. Soc Work Res. 2014;38(2):73–90. [Google Scholar]
- 19.Gu XS, Rosenbaum PR. Comparison of multivariate matching methods: structures, distances, and algorithms. J Comput Graph Stat. 1993;2(4):405–420. [Google Scholar]
- 20.Haviland A, Nagin DS, Rosenbaum PR. Combining propensity score matching and group-based trajectory analysis in an observational study. Psychol Methods. 2007;12(3):247–267. doi: 10.1037/1082-989X.12.3.247. [DOI] [PubMed] [Google Scholar]
- 21.Guo S. IMBALANCE: Stata module to check covariate imbalance before and after Matching. 2008. Available at: http://ideas.repec.org/c/boc/bocode/s457043.html. Accessed February 20, 2015.
- 22.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. J Public Health (Oxf) 2012;34(suppl 1):i3–i10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brener ND, Collins JL. Co-occurrence of health-risk behaviors among adolescents in the United States. J Adolesc Health. 1998;22(3):209–213. doi: 10.1016/S1054-139X(97)00161-4. [DOI] [PubMed] [Google Scholar]
- 24.DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Arch Pediatr Adolesc Med. 1999;153(3):286–291. doi: 10.1001/archpedi.153.3.286. [DOI] [PubMed] [Google Scholar]
- 25.Kinnunen JM, Ollila H, El-Amin SE, Pere LA, Lindfors PL, Rimpelä AH. Awareness and determinants of electronic cigarette use among Finnish adolescents in 2013: a population-based study. Tob Control. 2014 doi: 10.1136/tobaccocontrol-2013-051512. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pennanen M, Haukkala A, de Vries H, Vartiainen E. Longitudinal study of relations between school achievement and smoking behavior among secondary school students in Finland: results of the ESFA study. Subst Use Misuse. 2011;46(5):569–579. doi: 10.3109/10826084.2010.517725. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention. State laws prohibiting sales to minors and indoor use of electronic nicotine delivery systems—United States, November 2014. MMWR Morb Mortal Wkly Rep. 2014;63(49):1145–1150. [PMC free article] [PubMed]
- 28.Cordato R, Curry S. North Carolina’s e-cigarette tax: where bad tax policy meets special interest politics. 2014. Available at: http://www.johnlocke.org/acrobat/spotlights/Spotlight456ECigaretteTaxes.pdf. Accessed March 10, 2015.
- 29. US Public Health Service, Office of the Surgeon General; US National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2012.
- 30.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106(11):2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 31.Ayers JW, Ribisl KM, Brownstein JS. Tracking the rise in popularity of electronic nicotine delivery systems (electronic cigarettes) using search query surveillance. Am J Prev Med. 2011;40(4):448–453. doi: 10.1016/j.amepre.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Tan AS, Bigman CA. E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes. Am J Prev Med. 2014;47(2):141–149. doi: 10.1016/j.amepre.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo C, Zheng X, Zeng DD, Leischow S. Portrayal of electronic cigarettes on YouTube. BMC Public Health. 2014;14:1028. doi: 10.1186/1471-2458-14-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paek HJ, Kim S, Hove T, Huh JY. Reduced harm or another gateway to smoking? Source, message, and information characteristics of e-cigarette videos on YouTube. J Health Commun. 2014;19(5):545–560. doi: 10.1080/10810730.2013.821560. [DOI] [PubMed] [Google Scholar]
- 35.Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23(suppl 2):ii36–ii40. doi: 10.1136/tobaccocontrol-2013-051470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trtchounian A, Williams M, Talbot P. Conventional and electronic cigarettes (e-cigarettes) have different smoking characteristics. Nicotine Tob Res. 2010;12(9):905–912. doi: 10.1093/ntr/ntq114. [DOI] [PubMed] [Google Scholar]
- 37.Yang D, Small DS, Silber JH, Rosenbaum PR. Optimal matching with minimal deviation from fine balance in a study of obesity and surgical outcomes. Biometrics. 2012;68(2):628–636. doi: 10.1111/j.1541-0420.2011.01691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olitsky NH. How do academic achievement and gender affect the earnings of STEM majors? A propensity score matching approach. Res Higher Educ. 2014;55(3):245–271. [Google Scholar]
- 39.Heckman JJ, Ichimura H, Todd PE. Matching as an econometric evaluation estimator: evidence from evaluating a job training programme. Rev Econ Stud. 1997;64(4):605–654. [Google Scholar]
- 40.Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008;22(1):31–72. [Google Scholar]