Abstract
Lipoma is a tumour of soft tissue with rare occurrence in oral cavity accounting for only 1–4% of benign oral tumours. Most common sites of involvement are the buccal mucosa, tongue and floor of the mouth with typical presentation of an asymptomatic, soft, smooth-surfaced, nodular and yellowish mass. Histopathologically, a classical lipoma resembles normal adipose tissue and it has multiple variants which are less commonly seen except fibrolipoma. The article presents a case report of a relatively large oral classical lipoma in a 60-year-old man on a rare site, mandibular buccal vestibule, along with a review of the literature and special emphasis on its various histopathological variants.
Background
Lipomas are the commonest form of benign mesenchymal neoplasms of human body composed of mature adipocytes, usually surrounded by a fibrous capsule.1 2 They are often seen in the subcutaneous and retroperitoneal spaces which contain fat3 and can occur anywhere in the body and thus are called as the universal tumour or ubiquitous tumour.4 Lipoma was considered as an inadvertent growth of adipose tissue called ‘the hypertrophy theory’,5 an aberrant differentiation of mesenchymal cells into lipoblast called ‘the metaplasia theory’6 and a congenital origin from embryonic multipotent cells which differentiate into lipoma under hormonal influence during adolescence.7 Although the unavailability of lipids for metabolism coupled with the autonomous growth of lipoma have rendered it to be a true benign neoplasm.8
Trauma and chronic irritation have also been cited as triggers for the proliferation of fatty tissue into a benign tumour.9 Hereditary and chromosomal abnormalities including rearrangements of 12q, 13q and 6p chromosomes have also been cited in a few cases.10 They usually occur in fourth and fifth decades of life with peak incidence age at 40 years and slight male predilection.3 11 In the oral cavity, the most common sites are the buccal mucosa, tongue, palate, mandible and lip.3
The aetiology and pathogenesis remain unclear although mechanical, endocrinal and inflammatory influences have been reported.8 This case report discusses such a case with histopathological literature review.
Case presentation
A 60-year-old man reported with symptoms of difficulty in chewing food, swelling and discomfort in the left mandibular buccal vestibule opposite to the canine and premolars since 6 months. The swelling gradually increased in size to attain its present size. Medical, dental, family and personal history were unremarkable and the review of his systems appeared normal. Clinically, the swelling was a fluctuant, lobulated mass with smooth margins. It was non-tender, fragile and solitary, measuring 2.5×2.3×2.5 cm approximately. The oral mucosa over the mass appeared normal (figure 1). Based on history and clinical findings, a provisional diagnosis of lipoma was made.
Figure 1.
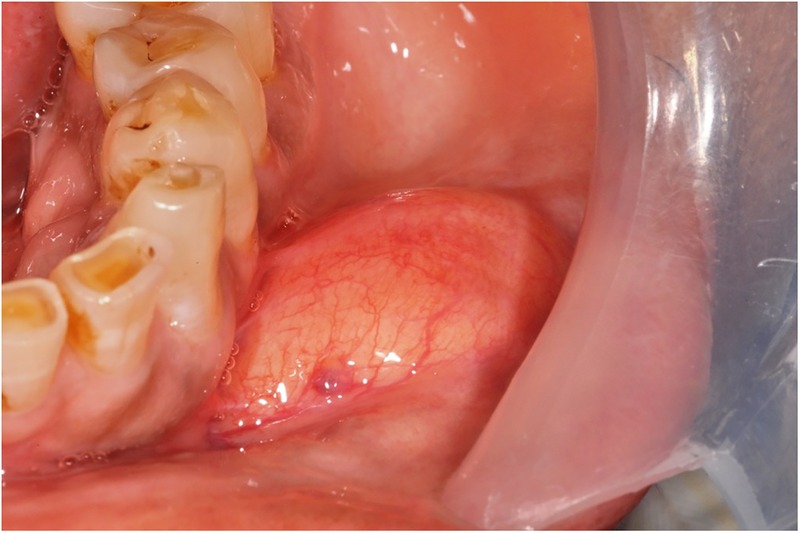
Photograph showing a yellowish, lobulated, soft fluctuant swelling mass in the left mandibular buccal vestibule opposite to the canine and premolars.
Investigations
Routine blood investigations, serum/urea electrolytes and urine analysis were carried out and all were found to be within normal limits.
Excisional biopsy was performed (figure 2). The resected yellow-coloured mass was placed in a beaker with normal saline for clearing the blood, where the specimen floated reinforcing the diagnosis of lipoma (figure 3). Then the mass was transferred to 10% buffered formalin and was sent for histopathological examination (figure 4).
Figure 2.
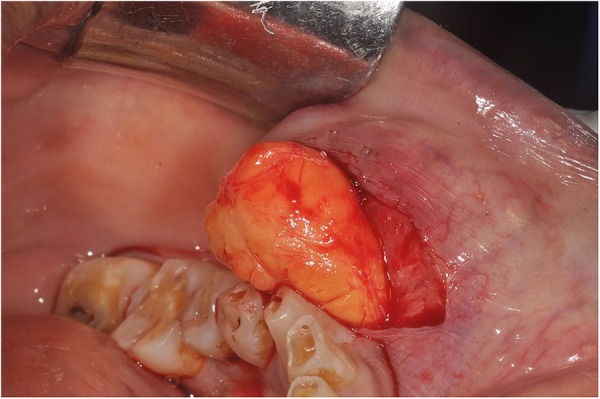
Photograph showing the surgical removal of the entire mass by excisional biopsy.
Figure 3.
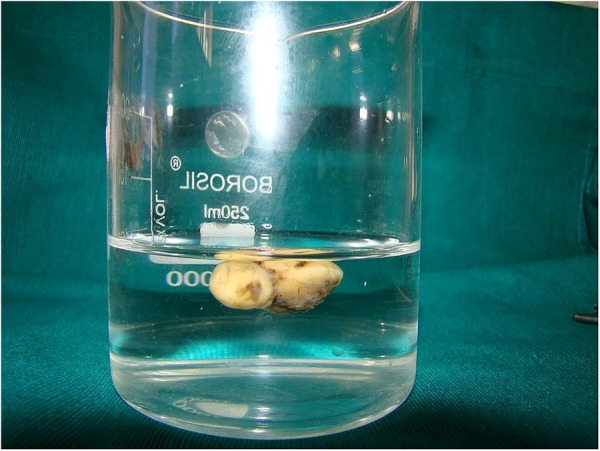
Photograph showing floatation of the resected mass placed in a jar with normal saline.
Figure 4.

Photograph showing the gross specimen.
The microscopic sections of the specimen stained with H&E showed a lobular arrangement of mature adipocytes bounded by a thin fibrous capsule (figure 5). The adipocytes were large round to ovoid cells with clear cytoplasm and eccentric nuclei compressed against the cytoplasmic membrane (figure 6). A final diagnosis of lipoma was made.
Figure 5.

Photomicrograph showing sheets of mature adipocytes in a distinct lobular arrangement with a thin fibrous capsule (H&E staining, ×10).
Figure 6.
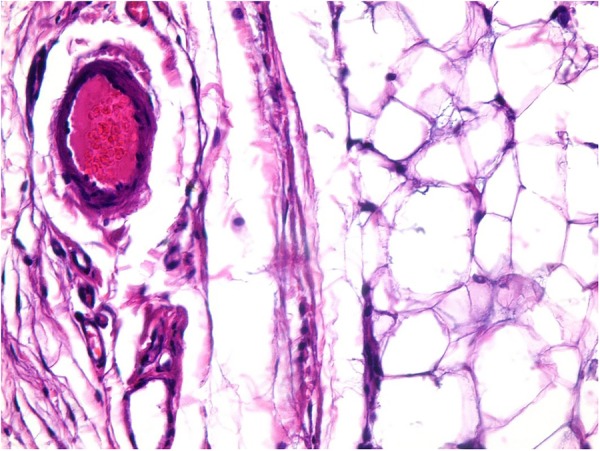
Photomicrograph showing mature adipocytes demonstrating large clear cytoplasms and eccentric nuclei (H&E staining, ×40).
Treatment
Local surgical excision is the treatment of oral lipomas. The entire mass was completely removed during biopsy procedure. Biopsy was performed under local anaesthesia and the wound was sutured with 4.0 vicryl suture material.
Outcome and follow-up
There were no postoperative complications. The patient was discharged after placing sutures and was called after a week for the removal of the sutures.
Differential diagnosis
Oral dermoid/epidermoid and lymphoepithelial cysts must be differentially diagnosed from the superficially located oral lipomas.12 Similarly, lipomas located deep with normal surface colour should be differentiated clinically from salivary gland tumours and benign mesenchymal neoplasms.13 Subcutaneous lipomas are usually thinly encapsulated and have distinct lobular patterns, whereas, deep-seated lipomas have a more irregular configuration, largely depending on the site of origin. Histopathology remains the gold standard in making a diagnosis of lipoma.14 The microscopic appearance of a circumscribed but unencapsulated to thinly capsulated aggregate of mature adipocytes with clear cytoplasm is the diagnostic feature of classic lipoma11 as seen in the present case. All are well vascularised, but under normal conditions, the distended adipocytes may compress the vascular network and is thus not clearly discernible.14
Microscopic differential diagnoses include normal fatty tissue, hibernoma and other histological variants of lipoma such as fibrolipoma, infiltrating or intramuscular lipoma, angiolipoma, myxolipoma, angiomyxolipoma, spindle cell lipoma, pleomorphic lipoma, myolipoma, angiomyolipoma, chondroid lipoma, osteolipoma or ossifying lipoma, neurofibrolipoma (NFL), sialolipoma and adenolipoma. Lipomas can be multiple in number with or without association with a syndrome and they can be present intraosseously.11 15
Discussion
Lipomas are the adipose mesenchymal tumours which account for 15–20% cases involving the head and neck region and only 1–4% affect the oral cavity. The first description of an oral lesion was provided in 1848 by Roux where he referred lipoma as ‘yellowish epulis’.14
Lipomas are similar in microscopic appearance to a normal fat tissue. Like fat, they are composed of mature fat cells, but the cells vary slightly in size and shape and are somewhat larger (measuring up to 200 mm in diameter) and have higher metabolism when compared to normal adipocytes.8 14 Despite their different metabolism, they are not used as an energy source as in a normal adipose tissue, probably due to high lipoprotein lipase activity in neoplastic lipoma cells.2 16 Since there is a histological similarity between normal adipocytes and lipoma cells, accurate clinical and surgical information is very important in making a definitive diagnosis.15
Lipomas are occasionally altered by the admixture of a fibrous connective tissue, which is often hyalinised known as fibrolipomas and can be diagnosed based on the presence of mature adipose tissue interspersed by bands of broad or fascicles of dense connective tissue fibres. The greater proliferative rate of fibrolipoma compared to a classic lipoma indicates the need for its accurate diagnosis.14
Quite often, however, lesional fat cells are seen to infiltrate into the surrounding tissues, perhaps producing long thin extensions of a fatty tissue radiating from the central tumour mass. This histological type is called as infiltrating lipoma. When located within striated muscle, this infiltrating variant is called intramuscular lipoma.14 15 Occasional tumours exhibiting abundant vascular channels are termed as angiolipomas. Histopathological evaluation of such tumours reveal mature adipose tissue intermixed with dilated vascular elements, often containing thrombi in the lumen.17
When there is myxoid background stroma, then it is called myxoid lipoma or myxolipoma.14 It is composed of solid proliferation of mature adipocytes admixed with abundant myxoid substances which contains scattered short spindle-shaped cells.18
Another histopathological variant, angiomyxolipoma is a benign uncommon lesion characterised by sheets of mature adipocytes interspersed with proliferation of vascular channels and associated with bland spindle cells scattered within an abundant myxoid component.19
Spindle cell lipoma is a relatively uncommon benign lipomatous tumour in which areas of spindle-shaped cells are seen interspersed among normal adipocytes. It is characterised by replacement of the mature adipose tissue by proliferation of collagen-producing spindle cells.8 14 20 Bland mitotically inactive spindle cells with little cytoplasm and elongated nuclei are arranged in parallel registers between the fat cells, associated with thick rope-like collagen bundles.21 When dysplastic spindle-shaped cells, pleomorphic giant cells with or without hyperchromatic enlarged nuclei are admixed with adipocytes the term pleomorphic lipoma is applied. Spindle cell lipoma is on a spectrum with pleomorphic lipoma, and these are histologically, clinically and genetically identical tumours, with the addition of the floret giant cell in the pleomorphic lipoma.22 When the spindle cells admixed with mature adipocytes are of smooth muscle origin, the term myolipoma is used. It is termed angiomyolipoma when smooth muscles appear to be derived from the walls of arterioles. Rarely, chondroid or osseous metaplasia may be seen in a lipoma which is described as chondroid lipoma, osteolipoma or ossifying lipoma.14
NFL also known as perineural lipoma and intraneural lipoma shows sheets of spindle and oval cells with wavy to oval nuclei in a myxoid background. Nerve bundles and lobules of mature adipocytes can be appreciated in other areas of a tumour as well.23 Sialolipoma reveals a well circumscribed and encapsulated mass of mature adipose tissue in lobular proliferation. The epithelial islets of glandular components are uniformly composed of atrophic, non-neoplastic, duct-acinar units of the salivary gland parenchyma, which is scattered throughout the tumour or is located in the periphery of the tumour.24 An intense lymphoid infiltrate, congested blood vessels, fibrosis and myxoid change may be noted in the adipose tissue.25 Adenolipoma has histological characteristics similar to sialolipoma; but it is composed of mature adipocytes and duct elements without acinar cells. Adenolipoma also differs from sialolipoma due to the lack of organoid arrangement of the ductal type tissue.24
The term lipomatosis has been used to describe a condition in which patients may present with multiple tumours.26 Intraosseous lipomas most commonly occur in the cancellous and long bones of lower extremities. Microscopically, the tissue is composed of areas of mature adipocytes interspersed with few trabeculae of mature lamellated bone and prominent thin-walled, large calibre vascular spaces. Serial sections fail to reveal normal haematopoietic tissues.4
The nature and etiopathogenesis of lipoma is largely unknown but few theories are still relevant.27
Lipomas are slow growing and patients commonly present with a well-circumscribed nodule developing for several years.15 Clinically they may present as solitary or multiple lesions.28 They are usually asymptomatic, mobile, soft, compressible and a submucosal mass with a yellowish hue and doughy consistency but can also present as a fluctuant nodule.3 15 The size of the tumour depends on the location but rarely exceeds 25 mm in diameter and the mean size reported in the literature is 20 mm.11 28 They usually occur in fourth and fifth decades of life with peak incidence age at 40 years and slight male predilection.3 11 In the oral cavity, the most common sites are the buccal mucosa, tongue, palate, mandible and lip.3
In the present case, the site, left mandibular buccal vestibule was rare and the size 25×23×25 mm approximately was relatively large. The duration of the symptom was 6 months which is shorter than the mean duration reported in the literature.
The treatment of oral lipomas, including all the histological variants is simple local surgical excision.14 Although the growth of oral lipomas is usually limited, they can reach great dimensions, interfering with speech and mastication and reinforcing the need for excision.15 Fewer than 5% of lipoma recur locally.26 Infiltrating lipomas are difficult to extirpate and are thus, liable to recurrence. Recurrence is reduced by wide surgical excision.11 Malignant change is virtually unheard of, and only a few cases have been reported in the literature.26
Learning points.
Oral lipomas are uncommon tumours of the oral cavity with half of the reported cases occurring in the buccal mucosa.
The present case reports a relatively unusual site of occurrence and large size.
The features of lipoma are usually straightforward and classical; histopathological diagnosis coupled with complete clinical and surgical details is very important in differential diagnosis of these lesions and is thus imperative to its diagnosis.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Studart-Soares EC, Costa FW, Sousa FB et al. Oral lipomas in a Brazilian population: a 10-year study and analysis of 450 cases reported in the literature. Med Oral Patol Oral Cir Bucal 2010;15:e691–6. 10.4317/medoral.15.e691 [DOI] [PubMed] [Google Scholar]
- 2.Fregnani ER, Pires FR, Falzoni R et al. Lipomas of oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg 2003;32:49–53. 10.1054/ijom.2002.0317 [DOI] [PubMed] [Google Scholar]
- 3.Adoga AA, Nimkur TL, Manasseh AN et al. Buccal soft tissue lipoma in an adult Nigerian: a case report and literature review. J Med Case Rep 2008;2:382 10.1186/1752-1947-2-382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basheer S, Abraham J, Shameena P et al. Intraosseous lipoma of mandible presenting as a swelling. Oral Maxillofac Pathol 2013;17:126–8. 10.4103/0973-029X.110705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta TKD. Tumors and tumor-like conditions of the adipose tissue in current problems in surgery. In: Ravitch MM, ed. Year book medical. Chicago, Ill, USA: Year Book Medical Publishers, 1970:1–60. [PubMed] [Google Scholar]
- 6.Ashley DJB. Evans histological appearances of tumors. 3rd edn Edinburgh, UK: Livingstone, 1978. [Google Scholar]
- 7.Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer 1974;34:720–7. [DOI] [PubMed] [Google Scholar]
- 8.Filho GAN, Caputo BV, Santos CC et al. Diagnosis and treatment of intraoral lipoma: a case report. J Health Sci Inst 2010;282:129–31. [Google Scholar]
- 9.Kumar LKS, Kurien NM, Raghavan VB et al. Intraoral lipoma: a case report. Case Rep Med 2014;2014:480130 10.1155/2014/480130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furlong MA, Fanburg-Smith JC, Childers EL. Lipoma of the oral and maxillofacial region: site and subclassification of 125 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:441–50. 10.1016/S1079210404001805 [DOI] [PubMed] [Google Scholar]
- 11.Nayak S, Nayak P. Lipoma of the oral mucosa: a case report. Arch Orofacial Sci 2011;6:37–9. [Google Scholar]
- 12.Anavi Y, Gross M, Calderon S. Disturbed lower denture stability due to lipoma in the floor of the mouth. J Oral Rehabil 1995;22:83–5. 10.1111/j.1365-2842.1995.tb00215.x [DOI] [PubMed] [Google Scholar]
- 13.Tan MS, Singh B. Difficulties in diagnosing lesions in the floor of the mouth-report of two rare cases. Ann Acad Med Singapore 2004;33(Suppl 4):72–6. [PubMed] [Google Scholar]
- 14.Kaur RP, Kler S, Bhullar A. Intra oral lipoma: report of 3 cases. Dent Res J 2011;8:48–51. [PMC free article] [PubMed] [Google Scholar]
- 15.Bandeca MC, de Padua JM, Nadalin MR et al. Oral soft tissue lipomas: a case series. J Can Dent Assoc 2007;73:431–4. [PubMed] [Google Scholar]
- 16.Solvonuk PF, Taylor GP, Hancock R et al. Correlation of morphologic and biochemical observations in human lipomas. Lab Invest 1984;51:469–74. [PubMed] [Google Scholar]
- 17.Altug HA, Sahin S, Sencimen M et al. Non-infiltrating angiolipoma of the cheek: a case report and review of the literature. J Oral Sci 2009;51:137–9. 10.2334/josnusd.51.137 [DOI] [PubMed] [Google Scholar]
- 18.Ono S, Rana M, Takechi M et al. Myxolipoma in the tongue—a clinical case report and review of the literature. Head Neck Oncol 2011;3:50 10.1186/1758-3284-3-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martinez-Mata G, Rocío MF, Juan LE et al. Angiomyxolipoma (vascular myxolipoma) of the oral cavity. Report of a case and review of the literature. Head Neck Pathol 2011;5:184–7. 10.1007/s12105-011-0241-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Junior OC, de Aguiar EC, França Sartori JH et al. Spindle cell lipoma of the tongue: a case report of unusual occurrence. J Oral Maxillofac Pathol 2013;17:148 10.4103/0973-029X.110730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evcimik MF, Ozkurt FE, Sapci T et al. Spindle cell lipoma of the hypopharynx. Int J Med Sci 2011;8:479–81. 10.7150/ijms.8.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnes L. Tumors and tumorlike lesions of the soft tissues. In: Barnes L, ed. Surgical pathology of the head and neck. 3rd edn USA: Informa Healthcare Newyork, 2009:806–12. [Google Scholar]
- 23.Fomete B, Adebayo ET, Ononiwu CN et al. Giant neurofibrolipoma of the tip of the tongue: case report and review of the literature. Ann Afr Med 2014;13:50–2. 10.4103/1596-3519.126954 [DOI] [PubMed] [Google Scholar]
- 24.Binmadi NO, Chaisuparat R, Levy BA et al. Sialolipoma of the lower lip: case report and literature review. Open Dent J 2012;6:208–11. 10.2174/1874210601206010208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Moraes M, de Matos FR, de Carvalho CP et al. Sialolipoma in minor salivary gland: case report and review of the literature. Head Neck Pathol 2010;4:249–52. 10.1007/s12105-010-0187-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldblum JR, Folpe AL, Weiss SW et al. In: Enzinger and Weiss's Soft tissue tumors 6th ed Philadelphia, PA: Saunders/Elsevier, 2014:443–66. [Google Scholar]
- 27.Motagi A, Aminzadeh A, Razavi SM. Large oral lipoma: case report and literature review in Iran. Dent Res J (Isfahan) 2012;9:350–2. [PMC free article] [PubMed] [Google Scholar]
- 28.Hoseini AT, Razavi SM, Khabazian A. Lipoma in oral mucosa: two case reports. Dent Res J (Isfahan) 2010;7:41–3. [PMC free article] [PubMed] [Google Scholar]


