Abstract
Introduction
Bladder exstrophy (BE) is a rare condition that requires complex surgical corrections to achieve the goals of bladder functionality, normal sexual function, continence, and finally cosmesis. The purpose of this study was to identify clinical parameters that predict better quality of life (QOL) scores using a validated questionnaire (SF-36) with young adults after completing surgical reconstruction.
Material and methods
Forty-three young adults (mean age 22.35 years, 29 men and 14 women) treated for BE were evaluated using the Short Form 36 general health questionnaire (SF-36). Clinical assessment involved evaluation of the actual condition regarding continence, sexual function, genital satisfaction and overall cosmesis.
Results
Both genders presented similar QOL scores (p = 0.36). The QOL was not age-related (p = 0.63). Neither genders did not present any differences in the number of procedures (p = 0.27). Although no significant gender difference was found, clinical impairments – such as urinary fistula, incontinence, penile length and infertility – were associated with worse QOL scores and were male-related (p <0.01). The most common complaint after complete surgical repair was about penile length (26/29 patients, 89.6%).
Conclusions
Age and gender were not predictors of better QOL scores. Any clinical impairment, such as urinary leakage due to incontinence or fistula, penile length and infertility, tended to significantly decrease the overall QOL in male patients with BE. The male genitalia seems to be the most troublesome aspect post-adolescence in treated male patients with exstrophy-epispadias. It has an important impact on the overall QOL, mainly having a social affect on those patients.
Keywords: bladder exstrophy, quality of life
INTRODUCTION
Bladder exstrophy (BE) is a rare condition with an incidence of 1 in 50.000 newborns [1, 2]. It is a complex pathology with an unknown etiology and is characterized by a low-lying umbilicus, exposed bladder plate, pubic symphysis diastasis, divarication of the rectus abdominis and pelvic floor, anterior ectopia of anus and vagina and penile epispadias [3].
Bladder exstrophy (BE) demands several surgical interventions to achieve satisfactory continence and genital appearance for a normal social, sexual and reproductive lifestyle [4]. Treatment of children born with classic BE is one of the most technically challenging situations in pediatric urology. A better understanding of functional anatomy, together with improved surgical techniques, has reduced complications and the number of procedures required for satisfactory reconstruction in patients with BE [5].
This urogenital anomaly affects the mental and psychosocial adjustment of children and their families. The appearance and function of external genitalia are among the most important concerns during adolescence and adulthood [6, 7].
Quality of life (QOL) is an elusive concept approachable at varying levels of generality, from the assessment of societal or community welfare to the specific evaluation of the situations of individuals or groups. QOL integrates objective and subjective indicators, collectively reflecting a broad range of life domains by using an individual ranking of the relative importance of each domain [8]. Considering the possible repercussions of BE, our aim was to study the long-term outcome of patients with BE regarding quality of life comparing males and females.
METHODS
This was an observational study approved by the ethics committee of our institution. All patients treated for BE in our institution since 1990 were recruited. In our study period, 96 patients were treated for BE in our institution. Only 51 were successfully contacted, and 43 agreed to participate in the study (29 males and 14 females), all of whom were over 15 years of age and were treated for BE in our institution. Those accepted to participate in the study were interviewed during an office visit using a validated questionnaire, Short Form 36 general health questionnaire (SF-36) [9]. The SF-36 measures a full range of health states and includes multi-item scales measuring each of eight health concepts: physical functioning, gender role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health. All patients signed a consent form prior to beginning the study.
Patients were also asked about their social inclusion with general questions regarding education, work, income, siblings, family, continence, surgeries, sexual life and genital appearance, urinary diversion, and pregnancy. Continence was defined as absence of urine loss or use of only 1 preventive pad daily. Sexual life was assessed as the presence of at least one penile penetrative intercourse per month. Genital appearance was assessed by asking the patients whether they would be satisfied if their genitalia looked like as it does in the moment of the survey for the rest of their life. Questions addressing education, income, siblings and number of pregnancies had their answers grouped by the distribution in three scale groups. For example, education was divided as elementary school, middle grades and college. Statistical analysis was performed using non-parametric tests with a 95% confidence interval for statistical significance (p <0.05). The software used for analysis was StatPlus® v. 2009 for Mac.
RESULTS
The average age of men was 20.4 years (15 to 36 years), and the average age of women was 26.4 years (15 to 48 years). The overall mean age was 22.35 years.
Most patients were of a low-income class (30 out of 43 patients received less than 5 Brazilian minimum wages). There was no statistically significant difference in the income of men and women (p = 0.36). One patient was not included due to non-response. Both genders had similar number of surgical procedures (p 0.27) (Table 1).
Table 1.
Number of surgeries and bladder augment
| Number of surgeries | Bladder augment | |||
|---|---|---|---|---|
| Less than 5 | More than 5 | Yes | No | |
| Female | 9 (64.3%) | 5 (35.7%) | 3 (21.42%) | 11 (78.58%) |
| Male | 13 (46.4%) | 15 (53.6%) | 9 (31.03%) | 20 (68.97%) |
The report of incontinence was similar between groups (p = 0.58). Satisfactory cosmesis was numerically better in the female group (71.4%) than the male group (53.6%), but it was not significant (p = 0.26). The most common complaint after complete surgical repair was about penile length (26/29 patients, 89.6%). Two patients were not included due to non-response (Table 2).
Table 2.
Satisfactory cosmesis and Incontinence in the patients treated
| Satisfactory cosmesis | Incontinence | |||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Female | 10 (71.42%) | 4 (28.58%) | 7 (53.84%) | 6 (46.16%) |
| Male | 15 (53.57%) | 13 (46.42%) | 13 (44.82%) | 16 (55.18%) |
Nine out of fourteen (64.3%) women and twenty out of twenty-nine (69.0%) men related sexual activity. Although most men reported normal sexual relations (70.0%), only three (10.3%) were satisfied with their penile length. Twenty-two (75.9%) also reported ejaculation (Table 3). In this study, six out of fourteen (42.85%) women had a pregnancy, and the median number of pregnancies was 1; overall, one patient had 2 and two patients had 3 children.
Table 3.
Male sexual profile
| Satisfactory penile length | Ejaculation | |||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Sexually active (n = 20) | 3 (15.00%) | 17 (85.00%) | 19 (95.00%) | 1 (5.00%) |
| Not sexually active (n = 9) | 0 | 9 (100.00%) | 3 (33.33%) | 6 (66.66%) |
Quality of Life (QOL) – SF-36 assessment
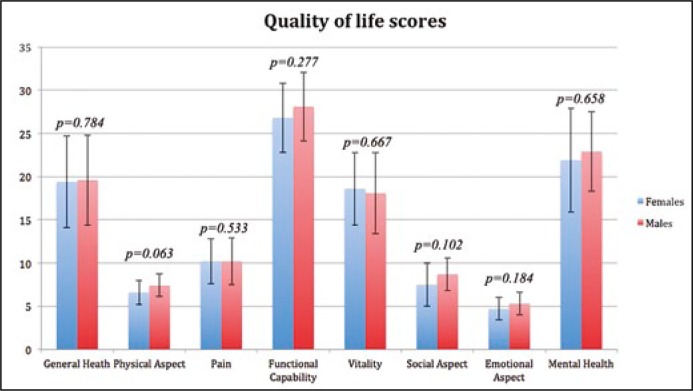
There was no difference in physical aspects, pain, functional capability, general health, vitality, social aspects, emotional aspects and mental health, thus not affecting the overall score (p = 0.36) (Figure 1). The QOL was not age-related (p = 0.63). Although no significant gender difference was found, clinical impairments – such as urinary fistula, incontinence, penile length and infertility – were associated with worse QOL scores and were male-related (p <0.01).
Figure 1.
Values of the domains assessed by SF-36 questionnaire.
DISCUSSION
The perceptions of health status and quality of life, and its treatment, are being widely recognized as a topic of research in clinical and epidemiological studies. Thus, the use of instruments to assess the QOL becomes fundamental to understanding the difficulties faced by patients with BE.
Patients with BE have a wide range of QOL scores, which was expected due to the disease having heterogeneous clinical manifestations and complications among patients [10]. In most areas surveyed by the SF-36, women reported worse QOL scores than men. Most early studies have shown no relation of QOL with income [11]. However, socio-economic differences between countries should be taken into account. In this study, majority of the patients were of a low-income class and were studying or working. Sexual and gynecological issues become increasingly important to patients as they become adults [12]. Previous studies suggested that female BE patients require comparatively fewer surgeries to achieve a satisfactory cosmetic outcome and have fewer problems with sexuality and sexual intercourse [10]. Nevertheless, our findings did not show any difference between genders regarding the number of surgeries, physical aspects or sexual activity. The female mean age was about 6 years older than the male mean age. Even though this difference was not significant, this could be a bias, since the self-perception of a person with 20 years of age is probably different than one with 26 years. Furthermore, 6 years is a significant amount of time for psychological maturation.
Male patients with BE are severely bothered by their penile size, with anxiety and avoidance of sexual interaction. Despite this, Ebert et al showed that approximately 50% of male BE patients are sexually active [13]. Others studies report that only 40-50% of male patients are satisfied with their penile appearance [14]. We found that 70.0% of men had regular sexual activity but that only 10.3% were satisfied with their penile length.
Regarding the points of strength of this study we should mention the sample size acquired for a rare condition such as BE and the data obtained from a long follow-up period in a country without a national database system for diseases. We have presented positive results from a low-income population of a developing country, with very limited resources.
Among the limitations of this study we should mention it's cross sectional design. A prospective and longitudinal study design would be appropriate to evaluate QOL indices during the various stages of life and impact on the daily life of patients. Moreover, there is no comparison between patients with BE and regular population to define a control group.
This study represents a timely assessment of the young adult population with BE. It should be noted that some issues covered in this study are not standardized in the SF-36. The direct relationship between the SF-36 and variables such as number of surgeries, bladder augment and incontinence demands further studies to standardize the quality of life questionnaires for patients with BE. The results underscore the need for further development of surgical and psychosocial interventions.
CONCLUSIONS
Although age and gender were not predictors for better QOL score, any clinical impairment – such as urinary leakage due to incontinence or fistula, penile length and infertility – tended to significantly decrease the overall QOL in male patients with BE.
Incontinence had a widespread negative impact on almost all aspects of the quality of life questionnaire. The male genitalia seems to be a troublesome aspect post-adolescence in male patients treated for BE, which has an important impact on the overall QOL, mainly affecting these patients socially.
Physical, mental, and psychosocial problems have important clinical implications and underscore the need for further development of surgical and psychosocial interventions.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Caton AR, Bloom A, Druschel CM, Kirby RS. Epidemiology of bladder and cloacal exstrophies in New York State, 1983-1999. Birth Defects Res A Clin Mol Teratol. 2007;79:781–787. doi: 10.1002/bdra.20402. [DOI] [PubMed] [Google Scholar]
- 2.Cervellione RM, Mantovani A, Gearhart J, et al. Prospective study on the incidence of bladder/cloacal exstrophy and epispadias in Europe. J Pediatr Urol. 2015;11:e1–6. doi: 10.1016/j.jpurol.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 3.K VS, Mammen A, Varma KK. Pathogenesis of bladder exstrophy: A new hypothesis. J Pediatr Urol. 2015;11:314–318. doi: 10.1016/j.jpurol.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 4.Csontai A1, Merksz M, Pirót L, Tóth J. Results of surgical treatment in children with bladder exstrophy. Br J Urol. 1992;70:683–685. doi: 10.1111/j.1464-410x.1992.tb15844.x. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Chaim J, Binyamini Y, Segev E, Sofer M, Bar-Yosef Y. Can Classic Bladder Exstrophy Be Safely and Successfully Reconstructed at a Low Volume Center? J Urol. 2015;195:150–154. doi: 10.1016/j.juro.2015.06.094. [DOI] [PubMed] [Google Scholar]
- 6.Avolio L, Koo HP, Bescript AC, Snyder HM, 3rd, Canning DA, Duckett JW., Jr The long-term outcome in men with exstrophy/epispadias: sexual function and social integration. J Urol. 1996;156:822–825. doi: 10.1097/00005392-199608001-00075. [DOI] [PubMed] [Google Scholar]
- 7.Mureau MA, Slijper FM, Nijman RJ, van der Meulen JC, Verhulst FC, Slob AK. Psychosexual adjustment of children and adolescents after different types of hypospadias surgery: a norm-related study. J Urol. 1995;154:1902–1907. [PubMed] [Google Scholar]
- 8.Taskinen S, Suominen JS, Mattila AK. Health-related Quality of Life and Mental Health in Adolescents and Adults Operated for Bladder Exstrophy and Epispadias. Urology. 2015;85:1515–1519. doi: 10.1016/j.urology.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 9.Gupta AD, Goel SK, Woodhouse CR, Wood D. Examining long-term outcomes of bladder exstrophy: a 20-year follow-up. BJU Int. 2014;113:137–141. doi: 10.1111/bju.12389. [DOI] [PubMed] [Google Scholar]
- 10.Park W, Zwink N, Rosch WH, et al. Sexual function in adult patients with classic bladder exstrophy: A multicenter study. J Pediatr Urol. 2015;11:125.e121–126. doi: 10.1016/j.jpurol.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Deans R, Liao LM, Wood D, Woodhouse C, Creighton SM. Sexual function and health-related quality of life in women with classic bladder exstrophy. BJU Int. 2015;115:633–638. doi: 10.1111/bju.12811. [DOI] [PubMed] [Google Scholar]
- 12.Dy GW, Willihnganz-Lawson KH, Shnorhavorian M, et al. Successful pregnancy in patients with exstrophy-epispadias complex: A University of Washington experience. J Pediatr Urol. 2015;11:213.e211–216. doi: 10.1016/j.jpurol.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Ebert AK, Bals-Pratsch M, Seifert B, Reutter H, Rösch WH. Genital and reproductive function in males after functional reconstruction of the exstrophy-epispadias complex-long-term results. Urology. 2008;72:566–569. doi: 10.1016/j.urology.2007.11.166. [DOI] [PubMed] [Google Scholar]
- 14.Suominen JS, Santtila P, Taskinen S. Sexual Function in Patients Operated on for Bladder Exstrophy and Epispadias. J Urol. 2015;194:195–199. doi: 10.1016/j.juro.2015.01.098. [DOI] [PubMed] [Google Scholar]