Abstract
Introduction: Opportunistic screening is an effective means of identifying subjects with Atrial Fibrillation (AF). Previous studies of opportunistic screening have been performed areas with high population density and before the development of novel oral anticoagulant drugs. We performed a study to determine feasibility of AF screening in a predominantly rural, low population density area.
Methods: Over 6 months, subjects 65 years and older were screened by local General Practitioners using radial pulse palpation confirmed by 12 lead Electrocardiogram. Data were recorded electronically and those with newly identified AF were followed up to examine management post diagnosis.
Results: In total, 7262 subjects were screened and an irregular pulse was found in 916 (12.6%) of whom 735 (10.1%) had known AF and 55 (0.76%) had newly detected AF. Of these 55 patients with newly documented AF, 28 (50.9%) were women, 38 (69.1%) had hypertension and eight (14.5%) had a smoking history. Mean body mass index in subjects with newly documented AF was 28.9 kg/m2(SD 5.6) There was no significant difference in gender mix (P = 0.4), smoking history (P = 0.8) or alcohol history (P = 0.8) with the overall population. Fifty-one (92.7%) subjects had a CHA2DS2VaSC score ≥ 2 of whom 33 (64.7%) were eventually anticoagulated and nine (17.6%) commenced on Aspirin. The rate of newly identified patients in AF was lower than in previous reported key studies because of a higher rate of subjects with known AF.
Conclusion: Opportunistic AF screening in a rural environment identified a substantial number of new cases, although less than in previous screening studies.
Introduction
Atrial fibrillation (AF) is a cardiac dysrhythmia found most commonly in older subjects and is associated with a substantially increased risk of cardioembolic stroke and peripheral embolism. Subjects in the highest risk group of the CHA2DS2VaSC risk calculator1 may have an annual risk of stroke in excess of 15%. Only 50% of subjects with AF may be aware of their arrhythmia2 and thus screening for the condition is considered of potential value. A study by Fitzmaurice et al.3 showed that opportunistic screening in UK General Practices (primary care facilities) using palpation of the radial pulse supported by follow up electrocardiograms (ECG) was as effective as organized screening where subjects over 65 were identified from practice lists and contacted to attend for formal screening, but was more cost effective. Both forms of screening were superior in identifying undetected AF than usual care.
Ireland has been found to have a comparatively high relative prevalence of AF-related cardioembolic stroke with up to one-third of all strokes identified from this source.4 Cardioembolic infarcts tend to be more disabling and more severe than other subtypes. However, Ireland has a lower population density and lower level of urbanization than much of Western Europe making screening of any type more challenging. This is particularly the case in the west of Ireland. We performed a study to examine the feasibility of opportunistic screening in this area.
Materials and Methods
Expressions of interest were first sought from hospitals with interested local groups of general practitioners (family doctors working in independent practices) from across the country. Proposals were evaluated by a group including senior hospital physicians, primary care doctors and health service mangers using a pre-agreed rating score. Elements considered in chosing sites inclused availability of information technology in local practices, development of the local primary care education and training network, active involvement of both hospital physicians and general practitioners in making the proposal, consistent local practice in referring subjects to secondary care services with AF and local availability of facilities to adequately investigate AF. Hospitals in Galway and Sligo, supporting primary care services in counties Galway, Sligo and Leitrim, were identified as the most suitable locations in which to undertake the study. In each case the local hospital was the primary source for secondary care for subjects seen in the community and this facilitated collection of information about management after referral to secondary care. All three counties involved are in the west of Ireland and, with the exception of urban areas of Galway city and Sligo town, these counties have a predominantly rural, dispersed population. Only one secondary care anticoagulation service was available in the selected area with most INR monitoring performed in primary care. The population density of each county at the time of the 2011 census were Galway (40.7/km2), Sligo (35.5/km2) and Leitrim (19.9/km2). This compares with a mean population density of 76.6/km2 for the island of Ireland and a density of 430/km2 for the UK West Midlands area where the benchmark study of opportunistic screening by Fitzmaurice et al.3 was performed.
All general practitioners in Galway, Sligo and Leitrim were invited to participate in the study. Inclusion criteria for practices were that they had to have their own ECG machine and access to a secure personal computer running Microsoft Excel. Local training was provided in each area and each participating practice was provided with a resource pack including information sheets, educational material and a treatment algorithm for AF (Supplementary Appendix 1). A bespoke data collection tool was created using Microsoft Excel and provided to each participating practice and training and support videos were produced by a senior cardiologist. A helpline was also provided to answer queries. Participating physicians were not paid for involvement but each practice was provided with funding to purchase a small piece of diagnostic equipment to acknowledge their participation. Funding was provided to each local hospital to cover the cost of additional imaging, echocardiography and cardiac monitoring that may arise from the study.
Over a period of 6 months, January to June 2014, practices were requested to each screen consecutive patients aged 65 years and older, using digital palpation of the radial artery. Where an irregular pulse was detected the doctor was asked to confirm the diagnosis of AF with a 12 lead ECG and consent was sought to include the subject in the study. Where AF was detected, the doctor could then manage the patient according to their clinical judgement. Demographic data were collected for all screened patients with further data collected with respect to vascular risks and risks for developing AF (Table 1). Where a subject was detected as having new AF subsequent data were collected by the study team from the participating general practices and hospitals with respect to further management, including choice of antithrombotic therapy and reasons for not chosing to anticoagulate.
Table 1.
Screened population and New AF patients
| All Screened | New AF | |
|---|---|---|
| No. of patients | 7262 | 55 |
| Men (%) | 3390 (45.3) | 27 (49.1) P = 0.4 |
| Median age | 74.0 | 76.0 |
| Age < 75 (%) | 3768 (51.9) | 23 (41.8) P = 0.13 |
Results
Screening
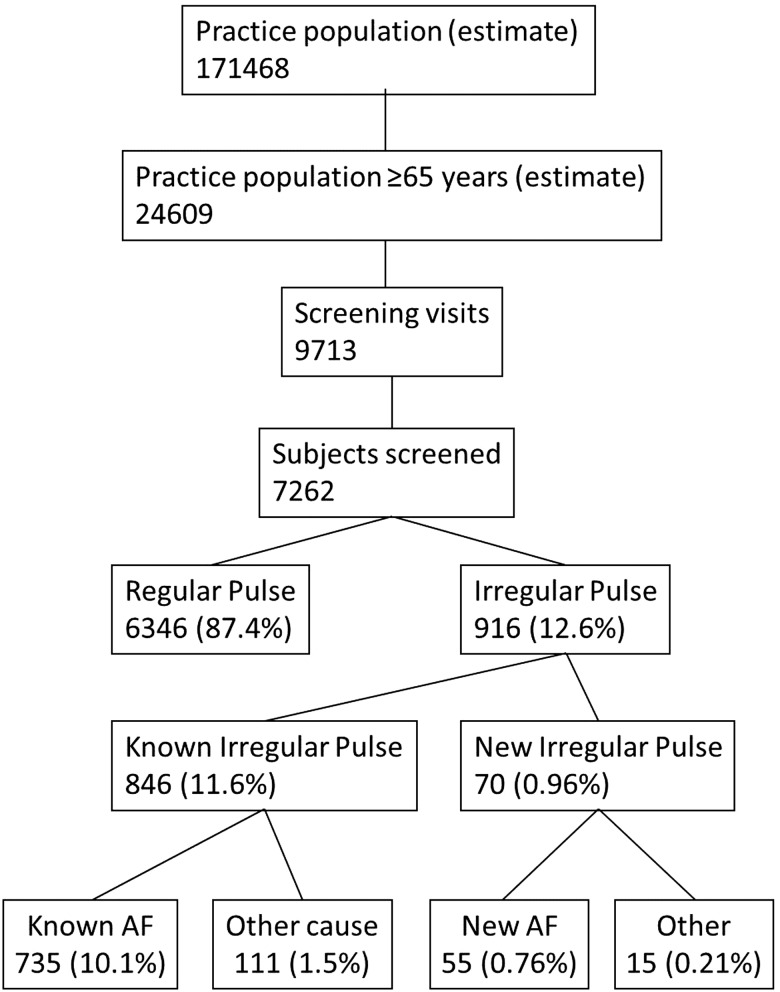
Forty-five practices, staffed by 100 physicians, were initially recruited to participate in the study. The estimated population served by these practices was 185 018 of whom 27 464 (14.8%) were 65 and older. Of these, 37 (82%) practices and 89 physicians eventually participated in and completed the study, serving an estimated population of 171 468 and with 24 609 subjects 65 years and older (Figure 1). Over 6 months January to June 2014, there were 9713 consultations, involving 7262 subjects (29.5% of population ≥ 65 years), where screening for AF was performed. Demographic characteristics of this population are summarized in Table 1.
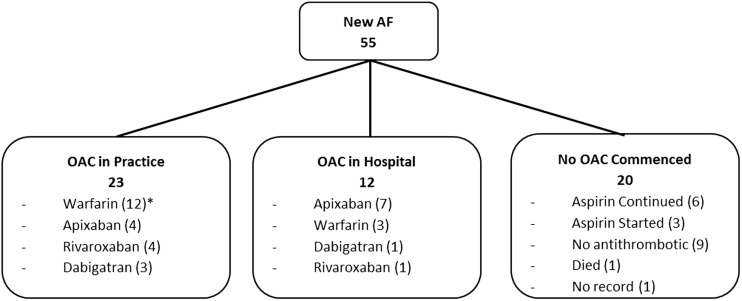
Figure 2.
Anticoagulation therapy. Oral anticoagulation (OAC)/antithrombotic therapy in subjects with new Atrial Fibrillation identified on screening. *Two subjects were receiving OAC for other indications at time of screening.
Figure 1.
Screening process.
An irregular pulse was detected in 916 Subjects (12.6%). Seven hundred thirty-five (83.1%) were already known to have AF and 111 patients (11.6%) were known to have an irregular pulse not attributable to AF. Of the remaining 70 cases, 55 (78.6%) were found to have AF on subsequent practice ECG. Consequently 10.1% of screened subjects were found to have established AF and 55 subjects (0.76%) had newly detected and confirmed AF (0.84% of subjects not already known to have AF) (Table 1).
Subjects with newly diagnosed AF
Twenty-eight (50.9%) subjects were female and median age for women tended to be older, (80.0 vs. 73.0 years, P = 0.21. t-test). Risk factor data were collected for the majority of subjects with newly diagnosed AF. Thirty-eight subjects (69.1%) had a recorded history of hypertension and the mean Blood Pressure (SD) for the 53 subjects with available data was 128.6 (14.3)/75.7 (10.2) mmHg and two (3.8%) subjects had a Systolic Blood Pressure ≥ 150 mmHg. Thirty-one of 55 (56.4%) subjects drank alcohol and of these four (12.9%) were reported to drink more than 14 units/week. Forty-five of 53 (84.9%) subjects with data available were never smokers with only three (5.7%) being current smokers. Mean Body Mass Index (BMI) on 53 subjects was 28.9 kg/m2 (5.6 SD) and 24 subjects (45.3%) had a BMI ≥ 25 kg/m2. There was no significant difference in gender mix (χ2, P = 0.4), smoking history (P = 0.8) or alcohol history (P = 0.8) with the overall population.
At presentation 17 (32.1%) of the subjects were tachycardic (Heart rate ≥110 bpm) and one had a heart rate <60 bpm. Twenty-seven of 54 subjects (50%) had no symptoms on presentation. Of the remaining 27 subjects the commonest symptoms were dyspnoea: 15 (55.6%), fatigue: nine (33.3%) and palpitations: seven (25.9%). Only two subjects (7.4%) complained of chest pain.
Management of AF
Fifty-one (92.7%) subjects had a CHA2DS2VaSC score ≥2 implying an indication for anticoagulation. Forty (72.7) of the subjects were referred to secondary care for further evaluation. At the end of the process one subject had died and 33 subjects (60.0% of total group, 64.7% of CHA2DS2VaSC score ≥2 group) were placed on an anticoagulant. Thirteen (39.4%) were commenced on Warfarin in addition to two who were already receiving Warfarin for other indications and 20 on a novel anticoagulant. Nine additional subjects were prescribed Aspirin–six who were already on Aspirin and three who were commenced on Aspirin after referral to hospital.
Discussion
The results of this study confirms that opportunistic screening using radial pulse palpation supported by 12 lead ECG is an effective way of identifying subjects with AF, including subjects with previously undiagnosed AF even in a rural, dispersed population.
Despite the high prevalence of AF and AF-related stroke internationally, a recent Cochrane review5 found that the Fitzmaurice et al.3 cluster, randomized controlled trail remained the sole study meeting criteria for review and providing objective evidence for screening. Despite this the review concluded that opportunistic screening was as effective as organized screening but was more cost effective and that both forms of screening were more effective than standard care.
We compared our results to those of the opportunistic screening arm of Fitzmaurice et al’s paper. Mean ages of screened populations was identical at 75.1 years. Rate of newly identified patients in AF as a proportion of subjects without AF was significantly lower in our study (55/6472 vs. 75/4500. P = 0.0001, χ2), however the proportion of people with known AF is substantially higher (735/6472 vs. 415/4500. P = 0.001, χ2). When combined, the overall prevalence of AF (known and new) was significantly higher in our study population (P = 0.03, χ2).
Our study differs from Fitzmaurice and colleagues’ study in three important aspects. The first is that, in contrast to the UK, access to primary health care in Ireland is not automatically free of charge to the whole population. Whilst the great majority of over 70s have access to free care by means of a ‘medical card’, access to this card is means tested. Those under 70 years have a much lower access to free care with <50% being in possession of a medical card. It has been found that subjects in Ireland > 50 years without access to free primary care make on average 1.5 less visits to their GPs per annum6 than those with and thus their opportunity for screening is substantially less.
The second difference is in the distribution of the population we studied and consequent challenge of routine access to primary and secondary care. The density of population in the area of our study is about one tenth that where Fitzmaurice and colleagues conducted their study in the UK West Midlands. Our study was conducted in some of the least populated and least urbanized areas of Western Europe. Accordingly, the practices attended tended to be small with a median of two doctors, and access to anticoagulation was typically through these practices. There is only one anticoagulation clinic in secondary care in the nearly 10 000 km2 area covered in this study.
Finally, this study was performed following national and European approval of the novel oral anticoagulants for preventing cardioembolism in AF. It is arguable that the impact of such medications on AF management in areas with dispersed populations is more than that in urban areas due to the comparative difficulty in accessing anticoagulation monitoring for Warfarin and hence a greater reluctance to prescribe such agents.7 It is of note that more than 57% of our subjects with new AF who were started on anticoagulation were started on a new oral anticoagulant (NOAC). This is lower than the 73% rate of NOAC prescription in the recent Swedish STOPSTROKE study of organized screening of over 75 year olds.8 It is also of note and some concern that more than one-third of subjects with new AF were not started on anticoagulation.
Our study may have a number of limitations. It was carried out over a 6-month period, January to June, with many of the subjects recruited in the first 3 months as many in the over 65 population were repeat attenders to the practice in the 6-month period. This period is associated with higher rates of cardiovascular and respiratory morbidity in the northern hemisphere9 and thus a potentially higher incidence of new AF precipitated by such factors. In contrast the rate of visits of ‘well’ older subjects typically increases during the late autumn as they attend to receive the annual influenza vaccine, which is free to all over 65s in Ireland, potentially lowering the prevalence of at risk subjects. However, the case detection of new AF identified in this study was significantly lower that of the Fitzmaurice paper. This may be due to the fact that the prevalence of known AF was higher in our study (10.1% vs. 8.4%) and thus the ‘at risk‘group of untreated patients in which to detect AF may have been smaller.
There is some evidence that subjects newly identified AF detected in this study may be at higher risk than those with AF in the general population. CHA2DSVaSC score and anticaogulation practice was not recorded in subjects with known AF in this study, but the total rate of AF is similar to that reported in the representative Irish Longitudinal Study of Ageing2 with a similar pattern of AF associated risk (Median CHA2DS2VaSC Score = 2). There was however a higher proportion of subjects in our study with a CHA2DS2VaSC Score ≥2 (92.7% vs. 67.8% P = 0.0006, χ2) suggesting a higher cumulated risk in our subjects. Anticoagulation therapy in our study population with newly diagnosed AF was better than thought found in the general population identified in TILDA. 64.7% of our subjects with a CHA2DS2VaSC Score ≥2 were anticoagulated compared with 40.7% of the TILDA population (P = 0.007, χ2). Although TILDA identified some subjects under 65 years with AF, more than 95% were 65 years or over.
Although the majority of individuals identified with AF in this study were already known to have the condition, there may still be benefit in screening to ‘re-identify’ those with chronic AF and review their treatment in an era where anticoagulation has arguably become easier.10 The rate of effective anticoagulation of subjects in known AF is often poor, the North Dublin Stroke study showed that in an Irish population half of those suffering AF related stroke had known AF but only 27% of those were receiving anticoagulation therapy at stroke onset.11 It is unlikely that the use of anticoagulants is higher outside of the capital2 but the consequences of suffering a cardioembolic stroke may be more significant in an era of more effective but highly time-dependent interventions such as thrombolysis and thrombectomy.12–14
The rate of new AF detected in both these studies was lower than the recently published STOPSTROKE study (9.3%).8 This study was performed in an older population however and despite this the rate of known AF was lower than in either the UK or Irish Study. Another limitation is that ∼70% of the estimated practice population ≥65 years were not screened in their general practice in the study period. We know from the Irish Longitudinal Study on Ageing (TILDA) that older subjects attended their general practitioner between 4.2 and 5.7 times on average in the preceding 12 months15, however we have no published data on what proportion never attended their doctor or what proportion attending as part of the study were not screened.
Ultimately, one of the hopes of the study was to encourage GPs and Practice Nurses to change practice and routinely check for an irregular pulse amongst their patients aged 65 year and older and the study appears to have been successful in that with 86.2% of GPs/Practice Nurses indicating that they now routinely checked pulses in all patients aged 65 and over with a further 3.1% indicating that they already checked prior to the study. This demonstrates that change in practice can occur particularly when it is a quick, non-invasive intervention such as this.
In conclusion, our study has shown that simple, opportunistic screening for AF in primary care an area with dispersed population and restricted access to health care detects a substantial number of people with previously undetected AF. Whether introduction such a screening programme would be of benefit will require a further health technology assessment.
Ethics: Research ethical approval was sought and obtained from the Irish College of General Practitioners Research Ethics Committee.
Funding
The study was entirely funded by the Irish National Clinical Programme for Stroke.
Acknowledgements
The authors would like to acknowlege the efforts of all the doctors and nurses who participated in this study. In particular we would like to thank Dr David Keane, Consulatnt Cardiologist for his help and advice in preparing training and educational resources for the investigators and participants in this study.
Supplementary material
Supplementary material is available at QJMED online.
Conflict of interest: None declared.
References
- 1.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010; 137:263–72. [DOI] [PubMed] [Google Scholar]
- 2.Frewen J, Finucane C, Cronin H, Rice C, Kearney PM, Harbison J, et al. Factors that influence awareness and treatment of atrial fibrillation in older adults. QJM 2013; 106:415–24. [DOI] [PubMed] [Google Scholar]
- 3.Fitzmaurice DA, Hobbs FD, Jowett S, Mant J, Murray ET, Holder R, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007; 335:383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly PJ, Crispino G, Sheehan O, Kelly L, Marnane M, Merwick A, et al. Incidence, event rates, and early outcome of stroke in Dublin, Ireland: the North Dublin population stroke study. Stroke 2012; 43:2042–7. [DOI] [PubMed] [Google Scholar]
- 5.Moran PS1, Flattery MJ, Teljeur C, Ryan M, Smith SM. Effectiveness of systematic screening for the detection of atrial fibrillation. Cochrane Database Syst Rev 2013; 4:CD009586. [DOI] [PubMed] [Google Scholar]
- 6.Hudson E, Nolan A. Public healthcare eligibility and the utilisation of GP Services by older people in Ireland. J Econ Ageing 2015; 6:24–43. [Google Scholar]
- 7.Nicholls SG, Brehaut JC, Arim RG, Carroll K, Perez R, Shojania KG, et al. Impact of stated barriers on proposed warfarin prescription for atrial fibrillation: a survey of Canadian physicians. Thromb J 2014; 12:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation 2015; 131:2176–2184. [DOI] [PubMed] [Google Scholar]
- 9.Frost L, Johnsen SP, Pedersen L, Husted S, Engholm G, Sørensen HT, et al. Seasonal variation in hospital discharge diagnosis of atrial fibrillation: a population-based study. Epidemiology 2002; 13:211–5. [DOI] [PubMed] [Google Scholar]
- 10.Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. , for the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Guidelines for the management of atrial fibrillation. Eur Heart J 2010; 31:2369–429. [DOI] [PubMed] [Google Scholar]
- 11.Hannon N, Sheehan O, Kelly L, Marnane M, Merwick A, Moore A, et al. Stroke associated with atrial fibrillation—incidence and early outcomes in the north Dublin population stroke study. Cerebrovasc Dis 2010; 29:43–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384:1929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372:1019–30. [DOI] [PubMed] [Google Scholar]
- 14.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372:11–20. [DOI] [PubMed] [Google Scholar]
- 15.McNamara A, Normand C, Whelan B. Patterns and Deteminants of Healthcare Utiliasation in Ireland. Dublin, The Irish Longitudinal Study of Ageing, 2013. [Google Scholar]