Learning point for clinicians
Primary myxoma of lung is extremely rare. However, it usually presents as a mass lesion in lung field through chest roentgenogram or computed tomographic scan without clinical symptoms. It deserves our attention because of the potential difficulty in differentially diagnosing it from lung cancer or metastasis.
Introduction
Primary pulmonary myxoma is rare and usually an incidental well-defined lung mass without symptoms. Resection is essential for diagnosis and treatment, because its diagnosis is usually difficult to be made on small biopsy samples or cytology. Herein, we present a primary myxoma of lung in an older man without any previous history of malignancy.
Case presentation
A 73-year-old gentleman had medical histories of hypertension, diabetes mellitus, coronary artery disease and hyperlipidemia under regular medical control. He complained of exertional dyspnea for 2 months. He visited our cardiologists, and ischemic heart disease was suspected. The physical examination showed no particular findings, such as cutaneous pigmentation, enlarged lymph node or palpable mass. Therefore, stress–rest thallium-201 myocardial perfusion single-photon emission computed tomography (CT) was done and revealed myocardial ischemia in anterolateral and inferior walls. However, a thallium-avid lesion at left upper lung field was incidentally found. Herein, chest roentgenogram and CT scan were subsequently arranged. The CT of chest demonstrated a well-circumscribed homogeneous mass in the left upper lobe (Figure 1A) without other intrathoracic abnormalities. Biochemical and hematological blood analyses revealed only mild microcytic anemia (hemoglobin: 11.5 g/dl, MCV: 76.1 fl) without other abnormalities. The radiologists suspected it might be an infectious granuloma, carcinoid tumor or hamartoma. The patient refused to undergo image-guided needle biopsy. Based on the patient’s willing, we performed left upper division lobectomy and mediastinal lymph node dissection under video-assisted thoracoscopy.
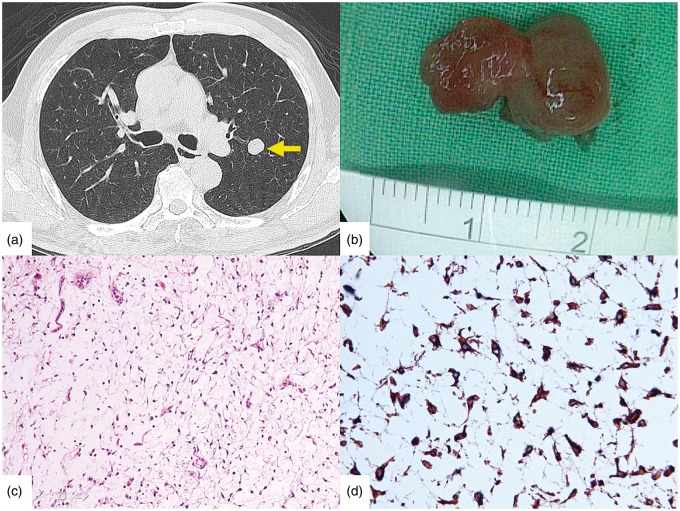
Figure 1.
A, CT revealed a well-circumscribed homogeneous mass in the left upper lobe (yellow arrow). B, The resected tumour was gelatinous and 1.7 × 1.3 × 1 cm. C, Histological examination revealed a hypocellular neoplasm composed of elongated and stellate cells in a myxoid stroma with no mitotic activity, no lipoblasts and delicate blood vessels (haematoxylin and eosin ×200). D, The tumour cells were immunohistochemically positive for vimentin (×400).
Macroscopically, the wedge resection contained a well-circumscribed gelatinous mass that was 1.7×1.3×1 cm (Figure 1B). The cut surface showed jelly-like and gray-tan without areas of hemorrhage or necrosis. Histological examination revealed a hypocellular neoplasm composed of spindle-shaped and stellate cells in an abundant myxoid stroma with no mitotic activity, no lipoblasts and delicate blood vessels (Figure 1C). The tumor cells were immunohistochemically positive for vimentin (Figure 1D), whereas negative for HMB-45, S-100, and cytokeratin. No metastasis was found on microscopic examination of the dissected lymph nodes. The patient had an uneventful postoperative recovery and had survived without recurrence for 14 months postoperatively.
Discussion
Myxomas are characterized by elongated and stellate cells in a myxoid stroma. Soft tissue myxoma, cutaneous myxoma, cardiac myxoma or myxomatous features in many types of sarcomas are relatively common. However, the primary pulmonary myxoma is extremely rare, and only four sporadic cases were reported in the English literature.1–4 Most patients, including our case, were essentially asymptomatic with a median age of 69 years and a median size of 1.8 cm, involving the lung parenchyma and endobronchial tree.1–4 Myxomas are usually single, grow by expansion of the initial lesion and do not metastasize. The diagnosis is usually difficult to be made on small biopsy samples or cytology owing to the hypocellularity and abundant myxoid substance. Moreover, there are also challenges in determining that these tumors are indeed primary lung tumors and not metastases from soft tissue neoplasms. Herein, history taking, preoperative whole-body evaluation and complete surgical resection are essential for diagnosis and treatment.
Conflict of interest: None declared.
References
- 1.Littlefield JB, Drash EC. Myxoma of the lung. J Thorac Surg 1959; 37:745–9. [PubMed] [Google Scholar]
- 2.Abcarian H, Lee HT. Primary endobronchial myxoma. Ann Thorac Surg 1973; 15:287–90. [DOI] [PubMed] [Google Scholar]
- 3.Matsuoka H, Takata Y, Maeda S. Primary pulmonary myxoma. Ann Thorac Surg 2005; 79:329–30. [DOI] [PubMed] [Google Scholar]
- 4.Kalhor N, Marom EM, Moran CA. Primary myxoma of the lung. Ann Diagn Pathol 2010; 14:178–81. [DOI] [PubMed] [Google Scholar]