Stanley and colleagues explore whether changes in insulin levels and insulin signaling are a cause or consequence of AD.
Abstract
Individuals with type 2 diabetes have an increased risk for developing Alzheimer’s disease (AD), although the causal relationship remains poorly understood. Alterations in insulin signaling (IS) are reported in the AD brain. Moreover, oligomers/fibrils of amyloid-β (Aβ) can lead to neuronal insulin resistance and intranasal insulin is being explored as a potential therapy for AD. Conversely, elevated insulin levels (ins) are found in AD patients and high insulin has been reported to increase Aβ levels and tau phosphorylation, which could exacerbate AD pathology. Herein, we explore whether changes in ins and IS are a cause or consequence of AD.
Alzheimer’s disease (AD) is a devastating neurodegenerative disorder affecting roughly 30 million people worldwide. Although some cases of AD (<1%) are caused by autosomal-dominant inherited mutations that typically lead to clinical disease onset before the age of 60, the majority of AD is late-onset AD (LOAD) where age, genetics, environment, and other diseases likely play a role (Holtzman et al., 2011; Musiek and Holtzman, 2015). AD is characterized by a cascade of pathological events, including the formation of amyloid plaques (made up of aggregated forms of Aβ), neurofibrillary tangles (composed of aggregated, hyperphosphorylated tau), synapse loss, brain hypometabolism, neuroimflammation, and brain atrophy that is accompanied by severe and progressive cognitive impairment. Amyloid plaques, consisting of aggregated forms of Aβ in the extracellular space, are generated in a concentration-dependent manner. The buildup of hyperphosphorylated and aggregated tau protein leads to the development of intracellular neurofibrillary tangles. Accumulation of Aβ occurs ∼15 yr before patients experience cognitive decline, whereas tau begins to accumulate in the neocortex later but before the onset of dementia, adding to the complexity of this disease. Many risk factors for LOAD, both genetic and nongenetic, have been identified. Apart from aging, the strongest known risk factor for LOAD is genetic variation in the apolipoprotein E (APOE) gene. The APOE4 allele increases AD risk by 12-fold (two copies) or 3.7-fold (one copy) in part by influencing Aβ accumulation. However, APOE4 is only present in ∼50–60% of individuals with AD, suggesting that other factors are involved in AD pathogenesis (Holtzman et al., 2011).
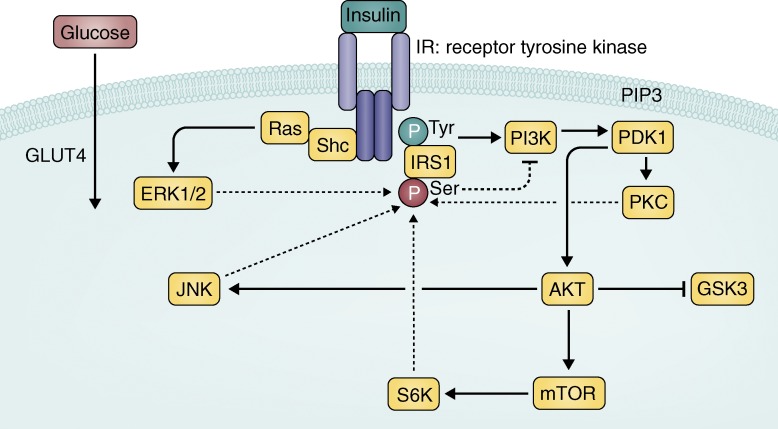
One such risk factor for LOAD, which has received considerable attention is type 2 diabetes (T2D), which increases AD risk by at least twofold (Sims-Robinson et al., 2010). Also a disease of aging, T2D is characterized by hyperglycemia, hyperinsulinemia, and insulin resistance (a lack of response in the insulin signaling [IS] pathway). Normally, insulin binds to the insulin receptor (IR) which phosphorylates IR substrate (IRS) on a tyrosine residue, leading to activation of the canonical signaling cascade (Fig. 1). In peripheral tissues, such as muscle, fat, and liver, this signaling ultimately leads to the uptake and sequestration of glucose to satisfy cellular energy requirements and plays a key role in lipid metabolism (Dimitriadis et al., 2011). Contrary to the periphery, where glucose uptake is largely insulin dependent, the brain uses nearly 20% of all glucose in the body in a process that is largely insulin independent. However, brain IS is robust and has pleotropic effects due to the widespread distribution of IRs throughout the brain and the complexity of IR signaling. For example, hippocampal activation of IR signaling can modulate memory (McNay et al., 2010) and IR signaling in the hypothalamus can affect feeding behavior and peripheral metabolism (Brief and Davis, 1984). Similar to AD, pathological changes in insulin occur years before patients receive a diagnosis of T2D, which typically occurs once pancreatic β cell dysfunction and insulin resistance produce chronic hyperglycemia (Dankner et al., 2009). Interestingly, T2D alone has been associated with cognitive decline (Allen et al., 2004), brain hypometabolism (Roberts et al., 2014), and regional brain atrophy (Last et al., 2007). The cognitive deficits in T2D are proposed to be mediated by changes in brain IS (McNay and Recknagel, 2011), although there is little data from T2D patients measuring insulin/IS in the CNS to support this assertion (Liu et al., 2011).
Figure 1.
Canonical IR signaling cascade. Insulin binds to the insulin receptor (IR), a receptor tyrosine kinase, which autophosphorylates and activates a cascade of phosphorylation events. IRS1 is phosphorylated on a tyrosine residue to activate further signaling, which ultimately leads to the translocation of glucose transporter 4 (GLUT4) to the membrane and uptake of glucose for energy in peripheral tissues. Solid arrows represent activation upon insulin stimulation. Blocked arrows represent inhibition. Glycogen synthase kinase 3 (GSK3) is serine phosphorylated and inhibited in response to insulin stimulation. Dashed arrows represent downstream effectors that have been found to phosphorylate IRS1 on a serine residue (p(Ser)-IRS1), which is thought to lead to less activation of the signaling cascade through negative feedback (dashed blocked arrow). p(Ser)-IRS1 is a marker of insulin resistance.
There are two broad ways in which T2D could influence the risk of AD: (1) T2D can lead to small vessel disease, which can cause or contribute to dementia, independent of or together with AD pathology, by disrupting proper function of the brain vasculature (Biessels and Reijmer, 2014), and (2) T2D can result in changes of brain function directly or interact with key proteins or pathways involved in AD pathology, such as Aβ or tau. This review will focus on mechanisms specific to AD pathology, but acknowledges the significant impact that vascular alterations may have on the brain in AD and other dementias.
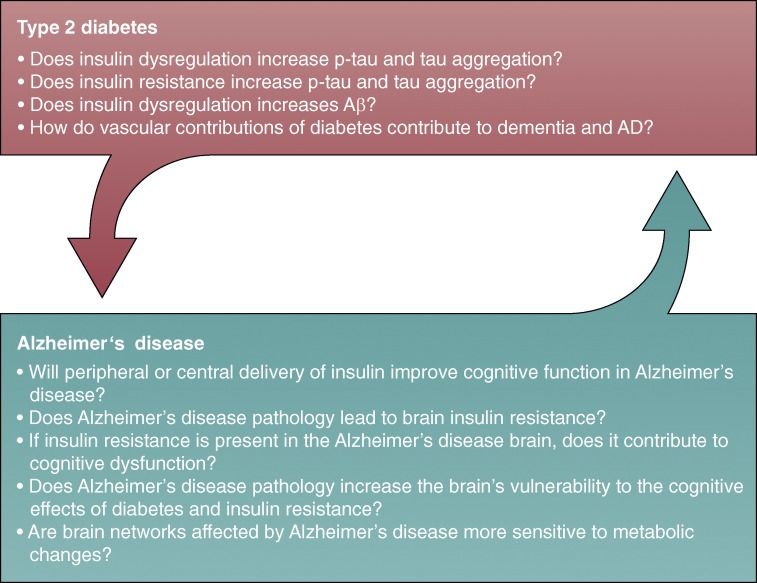
Over the past 15 yr, many studies have reported changes in insulin levels (ins) or IS (ins/IS) in LOAD patients (Table 1), suggesting that individuals with AD experience hyperinsulinemia and brain insulin resistance. One interpretation is that the brain becomes insulin resistant as a consequence of AD pathology and hyperinsulinemia is compensatory, producing what has been termed type 3 diabetes (Steen et al., 2005). Insulin resistance in the AD brain may lead to cognitive impairment, similar to that observed in T2D patients, therefore treating individuals with AD with intranasal insulin to improve memory is currently under investigation in clinical trials (Reger et al., 2008; Craft et al., 2012; Wadman, 2012). Conversely, hyperinsulinemia and insulin resistance can modulate Aβ and tau in ways that can put the brain at risk to develop further AD pathology, so that changes in the ins/IS in AD patients may represent a contributor/cause of disease progression (Fig. 2). If so, increasing brain insulin could exacerbate AD pathology and cognitive decline over time. This proposes a unique problem as it relates to AD; whereas insulin treatment may lead to modest cognitive improvement in AD patients, it could also worsen underlying pathology. In this review, we will analyze the changes in ins/IS that have been reported in AD and speculate if they are a cause or consequence of disease based on experimental evidence and the timeline of AD progression. Critical evaluation of this literature as well as a determination of essential future experiments is crucial, as rates of both T2D and AD are on the rise and insulin therapy is actively being pursued worldwide in older adults and patients.
Table 1. Insulin-related changes in AD.
| Parameter | AD ↑ ↓ | Study | Details |
|---|---|---|---|
| Blood insulin | ↑ | Bucht et al., 1983; Fujisawa et al., 1991; Stolk et al., 1997; Craft et al., 1998; Ma et al., 2016 | -Fasting or after glucose tolerance test -In women only (1 study) -Only in non-APOE4 and moderate/severe AD (1 study) -Meta-analysis of 11 studies: 5 report overall ↑, 1 ↑ in women, 1 ↑ with advanced stage (Ma et al., 2016) |
| CSF insulin | ↑ | Fujisawa et al., 1991 | -Also found small increase with vascular dementia |
| ↓ | Craft et al., 1998; Gil-Bea et al., 2010 | -Only in non-APOE4 and moderate/severe AD -No relationship to APOE or AD severity | |
| No change | Molina et al., 2002 | -No relationship with AD severity or cognition | |
| Brain insulin | No change | Frölich et al., 1998 | -Comparing controls >65 y/o and AD patients |
| ↓ | Frölich et al., 1998; Rivera et al., 2005; Steen et al., 2005 | -Comparing controls <65 y/o and AD patients -mRNA: in hippocampus and hypothalamus -mRNA: progressive reduction with Braak stage | |
| Brain IR (total) | ↓ | Frölich et al., 1998; Rivera et al., 2005; Steen et al., 2005 | -Comparing controls <65 y/o and AD patients -mRNA and protein -mRNA: progressive reduction with Braak stage |
| ↑ | Frölich et al., 1998 | -Comparing controls >65 y/o and AD patients | |
| No change | Moloney et al., 2010; Liu et al., 2011; Ho et al., 2012; Talbot et al., 2012 | -Potential changes in cellular distribution -Also no change in p-IR -Only reduced in patients with T2D and AD | |
| Brain p-IR and activity | ↓ | Frölich et al., 1998; Rivera et al., 2005; Steen et al., 2005 | -In hippocampus -Reduced insulin binding -TK activity reduced compared to all controls |
| Brain IRS1 (total) | ↓ | Steen et al., 2005; Moloney et al., 2010 | -mRNA in 3 regions -Also reductions in IRS2 |
| No change | Liu et al., 2011; Talbot et al., 2012 | -Also no change in IRS2 -Only reduced in patients with T2D and AD | |
| Brain p(Ser)-IRS1 | ↑ | Moloney et al., 2010 Talbot et al., 2012 Bomfim et al., 2012 Yarchoan et al., 2014 | -Regardless of APOE status and reduced ex vivo insulin stimulation -Highest in AD, but also elevated in some tauopathies |
| Brain AKT (total) | ↓ | Griffin et al., 2005; Liu et al., 2011 | -Reduced in AD and in patients with T2D and AD |
| No change | Steen et al., 2005; Talbot et al., 2012 | ||
| Brain p-AKT | ↑ | Pei et al., 2003; Griffin et al., 2005; Talbot et al., 2012; Yarchoan et al., 2014 | -Associated with tangles |
| ↓ | Steen et al., 2005 | -In hippocampus | |
| No change | Liu et al., 2011 | -Only reduced in patients with T2D and AD | |
| Brain GSK3 (total) | ↓ | Ho et al., 2012 | -With advanced AD |
| No change | Steen et al., 2005; Liu et al., 2011; Talbot et al., 2012 | -Only reduced in patients with T2D or T2D and AD | |
| Brain p(Ser)-GSK3 | ↓ | Steen et al., 2005 Griffin et al., 2005 | -In hippocampus |
| No change | Liu et al., 2011 | -Only reduced in patients with T2D or T2D and AD | |
| Brain p-GSK3 | ↑ | Pei et al., 2003 | -Associated with tangles |
| Brain p-JNK | ↑ | Bomfim et al., 2012; Talbot et al., 2012 | |
| Other IR signaling molecules | ↓ | Griffin et al., 2005; Liu et al., 2011; Talbot et al., 2012 | -PDK1, p-PDK1 and p-PI3K -PIP3, PKC, p-mTOR, p-ERK2 -PTEN |
Reported alterations in ins and brain IS in AD are categorized by the specific component measured, whether there have been reports of an increase, decrease (up and down arrows), or no change in individuals with AD, the studies that report this specific alteration, and important details. For blood and CSF insulin, AD diagnosis was based on clinical criteria. For postmortem analysis of brain insulin and IS components, AD was confirmed by clinical diagnosis and histological analyses. All reported changes were at the protein level unless mRNA is specified in the details. Overall, data from this table supports a higher level of blood insulin in individuals with AD and some degree of brain insulin resistance.
Figure 2.
Connections between T2D and AD: cause or consequence? Big picture questions that need to be addressed to determine if insulin-related changes represent a cause or consequence of AD. In regards to the evidence that T2D increases the risk of AD, answering the questions in the top arrow will determine how and why T2D is a risk factor and the potentially causal role of insulin/IS. In regards to the idea that AD progression may lead to a diabetic phenotype, answering the questions in the bottom arrow will determine if and how AD pathology may affect insulin homeostasis and the potential consequences of these changes on cognition.
INSULIN-RELATED CHANGES IN AD
Brain insulin
Many groups have analyzed postmortem brain tissue from AD patients of varying severity and controls to look for alterations in Ins/IS through changes in mRNA, protein, or phosphorylation (Table 1). Insulin has been measured in relatively low levels in brain tissue of humans and rodents (Banks et al., 1997; Frölich et al., 1998). Only one study reports insulin levels in the AD brain. They found that brain insulin was equally reduced in AD patients and age-matched controls, indicating that reductions in brain insulin are likely a result of age, not AD (Frölich et al., 1998).Two other groups report reductions in insulin mRNA in AD (Rivera et al., 2005; Steen et al., 2005), yet questions remain as to whether insulin is synthesized in the brain to an appreciable level because there is evidence that a majority of brain insulin comes from the blood (Banks, 2004). Specifically, one study could not detect insulin mRNA in the cortex (Steen et al., 2005) but another did (Rivera et al., 2005), making this mRNA data difficult to interpret. Ultimately, a greater understanding of insulin in the brain relative to the severity of AD and age-matched controls needs to be obtained in order to fully comprehend insulin’s function in healthy and diseased brains.
Brain IS
IRs are widely distributed throughout the brain, with relatively high concentrations in the olfactory bulb, hypothalamus, and hippocampus (Fernandez and Torres-Alemán, 2012). IRs are largely localized to neurons (Unger et al., 1989), although IR mRNA is present in glia and endothelial cells (Zhang et al., 2014). Although alterations in IR levels (Frölich et al., 1998; Steen et al., 2005) and its phosphorylation (Steen et al., 2005) are reported in AD, other studies found no differences (Moloney et al., 2010; Liu et al., 2011; Ho et al., 2012; Talbot et al., 2012). The most convincing, consistent change in IS is a lower level of IR substrate 1 (IRS1) and higher p(Ser)-IRS1, a marker of insulin resistance, in AD brains (Steen et al., 2005; Moloney et al., 2010; Bomfim et al., 2012; Talbot et al., 2012; Yarchoan et al., 2014). Higher p-JNK, which can lead to p(Ser)-IRS1, has also been found in AD brains (Bomfim et al., 2012; Talbot et al., 2012), suggesting some level of insulin resistance in AD. Questions still remain as to what are the physiological and pathological implications of increased markers such as p(Ser)-IRS1 and p-JNK and how that relates to AD pathology and brain function.
Canonical IS posits that, upon activation of AKT by insulin, glycogen synthase kinase 3 (GSK3) is serine phosphorylated to reduce its activity. Active GSK3 phosphorylates tau among other substrates, suggesting that overly active GSK3 may exacerbate tau phosphorylation and, ultimately, its aggregation. In postmortem brain samples, there are reductions in p-AKT and p(Ser)-GSK3, suggesting increased GSK3 activity, which can lead to tau phosphorylation (Steen et al., 2005; Liu et al., 2011). In contrast, other groups report increases in p-AKT and p(Ser)-GSK3, even in the presence of elevated phosphorylated tau (p-tau) and tangles (Pei et al., 2003; Griffin et al., 2005; Yarchoan et al., 2014), making this particular signaling component difficult to interpret. Reductions in the level or phosphorylation of other IS molecules are reported in AD brains (Liu et al., 2011; Talbot et al., 2012) and ex vivo activity assays have shown that tyrosine kinase activity, insulin binding, and insulin stimulation are reduced in AD brains (Frölich et al., 1998; Rivera et al., 2005; Talbot et al., 2012).
Overall, there does appear to be some level of insulin resistance in the AD brain. However, this is not specific to insulin, as there are also reductions in both the levels and signaling of insulin-like growth factor (IGF) I and II (Steen et al., 2005; Moloney et al., 2010) and leptin signaling (Maioli et al., 2015). Although brain insulin and IGF resistance in the human AD brain are seen as detrimental, mouse studies have paradoxically shown that deleting IRs or IGF1 receptors in the brain is protective against amyloid plaque deposition (Freude et al., 2009; Stöhr et al., 2013) and improves survival (Freude et al., 2009), demonstrating that there is much left to elucidate about the physiological consequences of reduced insulin or IGF1 signaling in the brain.
Blood and cerebrospinal fluid (CSF) insulin
Studies reported alterations in blood insulin in AD as early as 1983 (Table 1). Fasted blood insulin or insulin in response to a glucose challenge are higher in AD patients (Bucht et al., 1983; Fujisawa et al., 1991; Stolk et al., 1997; Craft et al., 1998; Ma et al., 2016). The transport of insulin from blood to brain and CSF is a receptor-mediated process. This transport is saturable within physiological levels and is affected by numerous variables (Banks, 2004). The CSF/serum insulin ratio is subtly decreased with age (Sartorius et al., 2015). Craft and colleagues also found the CSF/serum insulin ratio to be lower in AD, where higher blood and lower CSF insulin was more prominent with disease progression. Interestingly, they only found this change in AD patients without an APOE4 allele (Craft et al., 1998). Other groups who measured CSF insulin reported reductions but no difference with APOE4 (Gil-Bea et al., 2010), no difference (Molina et al., 2002), or increases with higher CSF/plasma ratios (Fujisawa et al., 1991), making interpretations of this data difficult. While reports of CSF insulin are variable, current data suggests that AD patients are likely to experience higher blood insulin. When trying to determine if this hyperinsulinemia could be a cause or consequence of disease, it is important to consider when hyperinsulinemia occurs in relation to the development of AD. Table 1 demonstrates that blood insulin is higher in AD patients, and it may increase with disease progression (Craft et al., 1998), but other studies suggest that higher blood insulin, before diagnosis, may be present and influencing disease progression.
Changes in ins and IS: cause of AD?
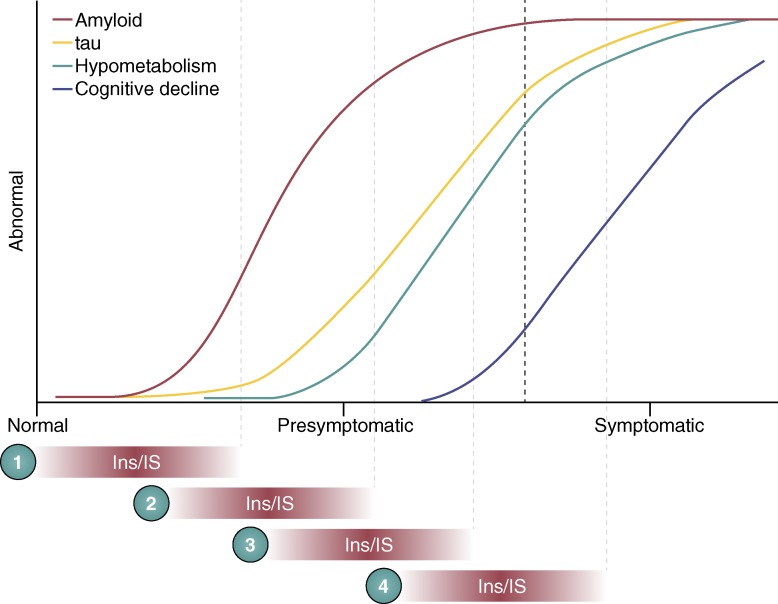
A longitudinal study found that fasting hyperinsulinemia, even without T2D, doubled the risk of developing AD (Luchsinger et al., 2004). A cross-sectional study found that in AD patients without an APOE4 allele, hyperinsulinemia was also associated with an increased risk of AD (Kuusisto et al., 1997) and higher insulin was associated with amyloid deposition, visualized by amyloid imaging on positron emission tomography (PET) scans, before symptom onset (Willette et al., 2015). Taken together, these studies suggest that high insulin could play a causative role in AD, although the AD population can be heterogeneous and it is possible that causal mechanisms differ across subgroups of patients. Since Aβ and tau deposition begin to occur ∼15 yr before symptom onset, these studies are difficult to interpret (Fig. 3). For example, high blood insulin before the onset of AD pathology could increase the risk of Aβ/tau deposition because ins/IS is a primary instigator of disease. In contrast, amyloid accumulation which begins ∼15 yr before cognitive decline could lead to brain insulin resistance, with hyperinsulinemia acting as a secondary indicator of underlying pathology in AD, and contribute to cognitive decline. To properly clarify whether insulin is a cause or consequence of disease, blood and CSF insulin should be tracked longitudinally, beginning before the onset of AD pathology, during AD pathology accumulation while individuals are still normal (preclinical AD), and then during the clinical stage of AD. To date, no such study has been reported. Recent studies have started to analyze the relationship between insulin resistance and AD biomarkers during the asymptomatic, preclinical stage in at-risk populations. In asymptomatic middle-age adults, insulin resistance was associated with higher CSF tau, p-tau (Starks et al., 2015) and Aβ42 (Hoscheidt et al., 2016). CSF insulin was not measured, but baseline levels of blood glucose, insulin, and insulin resistance were no different between APOE4 carriers and noncarriers at this early stage of disease (Starks et al., 2015). Additional studies of this type, measuring CSF insulin in addition to traditional AD biomarkers, will help to determine the temporal relationship between insulin dysregulation and AD progression.
Figure 3.
Where and when do changes in ins and IS affect AD? Colored lines represent our current understanding of the pathological timeline in AD. It is currently unclear when and where changes in ins/IS occur in this timeline. If changes in ins/IS happen early, (1) they could initiate or potentiate amyloid accumulation to casually influence AD. If ins/IS changes appear around the time of symptoms (4), this could be a consequence of years of pathological changes and may be directly related to cognitive decline. If changes in ins/IS occur in the presymptomatic period (2 and 3), they could be interacting with Aβ, tau, or metabolism to contribute to disease progression. Conversely, presymptomatic changes could be a result of tau or Aβ accumulation or metabolic perturbation. Additionally, it is possible that changes in ins/IS could simply push the symptomatic period to the left (earlier) without directly interacting with these pathologies.
Ins, IS, and Aβ
There are many studies suggesting that hyperinsulinemia may be directly influencing the risk of AD by modulating Aβ. In vitro studies demonstrate that high insulin can lead to higher extracellular Aβ by affecting clearance mechanisms and Aβ degrading enzymes. Both insulin and Aβ are degraded by insulin degrading enzyme (IDE), and in the presence of high insulin, IDE will preferentially degrade insulin over Aβ (Qiu et al., 1998). In vivo experiments corroborate in vitro findings where Aβ clearance is significantly reduced in rats in the presence of high insulin (Shiiki et al., 2004). In addition to affecting Aβ clearance, in vitro work demonstrates that high insulin increases extracellular Aβ concentrations by increasing production through IS (Gasparini et al., 2001). Conversely, inhibition of PI3K leads to reduced Aβ production (Stöhr et al., 2013). Crossing neuronal IR knockout mice to an APP transgenic mouse abolishes IR signaling in the brain and leads to reduced Aβ levels and amyloid deposition, indicating that endogenous IS elevates Aβ in vivo (Stöhr et al., 2013). A recent study in mice found that injection of supraphysiological levels of insulin increased brain IS and possibly Aβ (Sajan et al., 2016). In earlier work by Craft and colleagues, intravenous infusion of insulin in healthy older adults by hyperinsulinemic-euglycemic clamps improved performance on a declarative memory task, but increased CSF Aβ in ‘older’ participants (Watson et al., 2003). These clamps also increased plasma and CSF Aβ in another cohort, and increased inflammatory markers in the CSF (Fishel et al., 2005). Collectively, data suggests that elevated ins can modulate Aβ, suggesting T2D could exacerbate AD pathogenesis over time via this mechanism.
A crucial, remaining question is whether physiological, peripheral hyperinsulinemia seen in AD or T2D raises brain insulin enough in vivo to actively compete with IDE, activate IS, or increase Aβ since insulin transport across the blood brain barrier (BBB) is saturable at normal physiological levels (Banks, 2004). A recent paper found that in several mouse models of T2D and in T2D monkeys, hyperinsulinemia was associated with higher brain IS and higher Aβ levels at baseline. Murine Aβ was reportedly measured by Western blot in these experiments but the concentration is typically so low that this method may not be sufficient to detect small changes. Regardless, insulin injection did not further increase IS or Aβ, which could be due to transport or receptor saturation (Sajan et al., 2016). Overall, it still appears that hyperinsulinemia can positively regulate Aβ, though further studies are needed to clarify this.
While high blood insulin may indicate higher brain ins/IS, it is also possible that lower brain ins/IS leads to higher blood insulin as an attempt to compensate for the reduction. A longitudinal study found that both the highest and lowest quartiles for fasting insulin were associated with the development of dementia (Peila et al., 2004). One mouse model of AD was found to have reduced brain insulin and some changes in IS that preceded the deposition of Aβ (Chua et al., 2012). These results suggest that low brain ins/IS may also affect Aβ. Unfortunately, they did not measure blood or CSF insulin to know how these measures fluctuate overtime in relation to amyloid deposition and brain ins/IS.
GSK3 can increase Aβ levels in vitro and inhibition of GSK3 by lithium can reduce APP processing and Aβ levels (Phiel et al., 2003). As shown in Fig. 1, insulin also inhibits GSK3 through canonical signaling which would suggest that adequate ins/IS may contain Aβ levels. So far, this has not been validated experimentally. Lowering blood insulin by destroying insulin-producing cells in a mouse model of AD reduces brain ins/IS and results in elevated Aβ levels (Wang et al., 2010). While the authors conclude that insulin deficiency raised Aβ, these mice also have extreme hyperglycemia which we and others have recently shown can independently increase extracellular Aβ (Macauley et al., 2015; Chao et al., 2016). Moreover, decreasing insulin production would lead to decreased IDE levels, which could affect Aβ since IDE is an Aβ degrading enzyme.
While hyperinisulinemia can initially increase brain insulin and positively regulate Aβ acutely, chronic hyperinsulinemia can down-regulate transport leading to lower blood:brain insulin (Banks et al., 1997). This decrease in BBB transport may also increase Aβ, although there is no direct experimental evidence supporting this claim. Since it is unclear whether chronic hyperinsulinemia (described in Table 1) leads to increased brain insulin or to decreased insulin transport, additional experimental confirmation is required to identify a causal relationship with Aβ and AD.
Ins, IS, and tau phosphorylation
GSK3 activity is often connected to the phosphorylation of tau. Neuronal IR knockout mice have higher p-tau, presumably due to more active GSK3 (Schubert et al., 2004). Interestingly, these IR knockout mice do not have any memory deficits despite evidence that IS is connected to cognition and p-tau is linked with memory deficits in mice (Schindowski et al., 2006). Peripheral injection of supraphysiological insulin is capable of elevating IS in the mouse brain and increases p-tau even though GSK3 is serine phosphorylated by p-AKT to reduce activity and presumably p-tau (Freude et al., 2005). Hyperinsulinemia also increases p-tau in aged, wild-type mice (Becker et al., 2012). In vivo studies from mice agree with the complex findings from AD brains (Table 1) which found GSK3 to be both more active and less active while p-tau was high. Overall, these data suggest, again, that both high ins/IS (from hyperinsulinemia) and low IS (from insulin resistance) may put the brain at risk to exacerbate AD.
One study found that chronically raising blood insulin in mice via a high fat diet had no effect on p-tau in the brain, but they also reported no change in brain IS (Becker et al., 2012). When injected peripherally with supraphysiological insulin, p-tau was unchanged in mice with chronic hyperinsulinemia (Becker et al., 2012). Brain IS in response to the peripheral injection was not measured, but this likely demonstrates that insulin transport is reduced with chronic hyperinsulinemia. Additional evidence from a study in mice and monkeys demonstrates that chronic hyperinsulinemia resulted in higher brain IS and higher p-tau (Sajan et al., 2016). They also found no further increase in IS with insulin injection, confirming that chronic hyperinsulinemia is most likely saturating BBB transport and/or IS. These studies highlight the complexity between acute and chronic changes in blood insulin and insulin sensitivity in the brain that need to be considered when trying to understand how hyperinsulinemia and brain insulin resistance relate to each other and AD.
Changes in ins and IS: consequence of AD?
One AD population study found that up to 80% of AD patients had either T2D or insulin resistance, suggesting that AD may lead to a diabetic phenotype (Janson et al., 2004). Unfortunately, there are no longitudinal studies showing whether or not diabetic phenotypes occur after AD onset or precede AD diagnosis. Tissue analysis (Table 1) supports that brain insulin resistance worsens with advancing AD, but it is unclear how early in disease progression insulin resistance occurs (Fig. 3). If reduced brain IS is associated with cognitive decline, one would expect changes to occur around the time that symptoms start to appear, which may be after blood insulin is already high. In T2D patients, insulin resistance is also associated with brain hypometabolism (Baker et al., 2011). In AD, hypometabolism occurs before symptom onset and is likely related to synaptic dysfunction and neuronal loss, and worsens with disease progression (Sperling et al., 2011). It is unclear how hyperinsulinemia, insulin resistance, brain hypometabolism, and cognitive decline are temporally related in AD (Fig. 3). A recent study used plasma exosomes from neural sources to measure p(Ser)-IRS1, a marker of insulin resistance, longitudinally in individuals with AD, T2D, or healthy controls (Kapogiannis et al., 2015). In these exosomes, p(Ser)-IRS1 was found to be higher in AD and T2D compared with controls, and was elevated up to 1–10 yr before AD diagnosis. However, there was no association of exosome p(Ser)-IRS1 with AD severity or insulin resistance, which is contrary to results from postmortem brain tissue (Table 1). Determining which comes first, hyperinsulinemia or brain insulin resistance, would be the key to understanding which is a cause or consequence of AD and how they relate to AD pathogenesis.
In T2D, hyperinsulinemia is capable of leading to insulin resistance through negative feedback at the IR (Fig. 1). Thus, it is possible that the hyperinsulinemia seen in AD patients may lead to brain insulin resistance or reduced insulin transport, which can modulate both Aβ and p-tau to contribute to AD in a causal way. Although there is currently no longitudinal data demonstrating that hyperinsulinemia precedes the onset of AD pathology, there is mechanistic evidence that it is possible for hyperinsulinemia to drive both insulin resistance and AD. Alternatively, insulin resistance in T2D can also be initiated by other processes, such as cellular stress and inflammation, which activate signaling molecules like p-JNK to increase p(Ser)-IRS1, causing hyperinsulinemia as a compensatory mechanism (Draznin, 2006). Moreover, oxidative stress and neuroinflammation are key features of the AD brain, which may promote brain insulin resistance, but most experiments have yet to explore these mechanisms in the context of AD.
Aβ and brain insulin resistance
There is substantial evidence from in vitro experiments that Aβ may directly contribute to neuronal insulin resistance. Aβ can competitively inhibit the binding of insulin to the IR (Xie et al., 2002). Aβ oligomers (AβO) are thought to be the more toxic species of Aβ, and synthetic AβOs bind to and internalize IRs causing an increase in neuronal p(Ser)-IRS1 and p-JNK, markers of insulin resistance (Zhao et al., 2008; Bomfim et al., 2012). In vivo experiments found higher p(Ser)-IRS1 and p-JNK in human AD brains (Table 1) and aged APP transgenic mice. They also found that intracerebroventricular injection of AβO’s into monkeys elevated p(Ser)-IRS1 and p-JNK, demonstrating that these AβO’s can cause resistance in vivo (Bomfim et al., 2012). AβO’s increase p-tau, which may result from activation of GSK3 as a result of reductions in IS (Ma et al., 2009). Taken together, these data suggest that Aβ has the ability to induce insulin resistance in vitro and in vivo using several different model organisms.
Insulin treatment for brain insulin resistance
Craft et al. (1996, 1999, 2003, 2012) continue to demonstrate that insulin treatment, either by intravenous infusion or intranasal delivery, can modestly enhance performance on memory tasks in healthy adults and patients with AD or mild cognitive impairment (MCI) at specific doses (Watson et al., 2003; Reger et al., 2008; Claxton et al., 2015). Gender and APOE4 modulate the beneficial effects of insulin (Craft et al., 2000, 2003; Reger et al., 2008; Claxton et al., 2013). In mice, intranasal administration of insulin increases insulin in the cortex and hippocampus to some extent (Salameh et al., 2015), but whether or not it increases IS and confers protection against neuronal damage is still unknown. In vitro studies show that synthetic AβOs co-cultured with neurons can bind to synapses and reduce dendritic spines, an effect that is rescued when treated with high insulin and IS is activated (De Felice et al., 2009). Increasing hippocampal insulin and IS in rats also enhances memory. However, rats with T2D induced by a high fat diet did not show improvement with insulin treatment (McNay et al., 2010), suggesting that once brain insulin resistance has developed, insulin treatment may not be sufficient to overcome resistance at a cellular level. In a mouse model of AD, high fat diet led to insulin resistance and exacerbated amyloid pathology and memory impairment. A single, supraphysiological injection of insulin was found to improve IS in peripheral tissues and reduce soluble Aβ in the brain, but brain IS was not measured (Vandal et al., 2014). If insulin resistance is severe and causing brain insulin to be too low, increasing insulin under these conditions may help mitigate Aβ levels; however, this hypothesis was not directly tested. If brain IS is within normal range, insulin injection can increase IS and possibly Aβ levels (Sajan et al., 2016). Additionally, raising brain insulin by intranasal delivery appears to elevate brain insulin high enough that it may increase Aβ or p-tau, although this has not been addressed in studies to date. Preliminary reports using intranasal insulin in mouse models suggests that this treatment may have some positive effects on memory and pathology (Chen et al., 2014; Zhang et al., 2016). Extendin-4, an antidiabetic medication thought to enhance IS by activating similar pathways, was able to prevent the development of insulin resistance (p(Ser)-IRS1) in neuronal cultures and APP transgenic mice (Bomfim et al., 2012). Insulin sensitizers that are used to treat peripheral insulin resistance, rather than insulin itself, may also be beneficial in AD. However, it is unclear if enhancing IS through insulin sensitizers can also modulate Aβ or p-tau.
The current hypothesis is that intranasal insulin is directly influencing cognition by acting on neuronal IRs to overcome resistance, but this has not been shown directly. Recent evidence has shown that intranasal insulin may be working through indirect pathways to influence cognition. For example, there have been reports of intranasal insulin increasing regional cerebral blood flow and cognition in T2D patients (Novak et al., 2014). Insulin is thought to act through IRs on endothelial cells in the brain, but a recent study could not detect significant IR peptide in this cell type, despite IR mRNA being abundant (Zuchero et al., 2016). Determining the mechanism of intranasal insulin’s cognitive enhancement, and whether or not neuronal IS is necessary, will ultimately allow a more targeted therapeutic approach that may not have the potential side effect of raising Aβ or p-tau.
Concluding remarks
There is substantial experimental evidence that hyperinsulinemia and brain insulin resistance, seen in LOAD patients, is capable of increasing Aβ and p-tau to initiate or exacerbate the pathological cascade associated with AD. If patients experience high blood insulin before early AD alterations, hyperinsulinemia could causally contribute to both AD pathology and insulin resistance. However, there is not significant data to confirm this hypothesis in humans. Alternatively, initial Aβ accumulation can lead to neuronal insulin resistance and secondary hyperinsulinemia, which further exacerbates AD progression. Both longitudinal and biomarker studies need to be performed to properly understand how high insulin in the blood, brain, or CSF, combined with insulin resistance, relate to the progression of AD. Until that time, we should assume that the alterations in ins and IS represent both a cause and consequence of disease and need to be closely monitored as insulin therapy is investigated for AD.
Acknowledgments
This work was supported by a National Science Foundation Graduate Research Fellowship (DGE-1143954; M. Stanley), National Institute on Ageing grant K01 AG050719 (S.L. Macauley), National Institute of Neurological Disorders and Stroke grants F32 NS080320 (S.L. Macauley) and P01 NS080675 (D.M. Holtzman), New Vision Award through Donors Cure Foundation (S.L. Macauley), and the JPB Foundation (D.M. Holtzman).
D.M. Holtzman co-founded and is on the scientific advisory board of C2N Diagnostics. D.M. Holtzman consults for Genentech, AbbVie, Eli Lilly, Neurophage, and Denali. SML consults for Denali. The authors declare no additional competing financial interests.
Footnotes
Abbreviations used:
- Aβ
- amyloid β
- AD
- Alzheimer’s disease
- APOE
- apolipoprotein E
- APP
- amyloid precursor protein
- CSF
- cerebrospinal fluid
- GSK3
- glycogen synthase kinase 3
- ins
- insulin level
- IR
- insulin receptor
- IRS1
- IR substrate 1
- IS
- insulin signaling
- LOAD
- late-onset AD
- p-tau
- phosphorylated tau
- T2D
- type 2 diabetes
References
- Allen K.V., Frier B.M., and Strachan M.W.. 2004. The relationship between type 2 diabetes and cognitive dysfunction: longitudinal studies and their methodological limitations. Eur. J. Pharmacol. 490:169–175. 10.1016/j.ejphar.2004.02.054 [DOI] [PubMed] [Google Scholar]
- Baker L.D., Cross D.J., Minoshima S., Belongia D., Watson G.S., and Craft S.. 2011. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch. Neurol. 68:51–57. 10.1001/archneurol.2010.225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks W.A. 2004. The source of cerebral insulin. Eur. J. Pharmacol. 490:5–12. 10.1016/j.ejphar.2004.02.040 [DOI] [PubMed] [Google Scholar]
- Banks W.A., Jaspan J.B., and Kastin A.J.. 1997. Selective, physiological transport of insulin across the blood-brain barrier: novel demonstration by species-specific radioimmunoassays. Peptides. 18:1257–1262. 10.1016/S0196-9781(97)00198-8 [DOI] [PubMed] [Google Scholar]
- Becker K., Freude S., Zemva J., Stöhr O., Krone W., and Schubert M.. 2012. Chronic peripheral hyperinsulinemia has no substantial influence on tau phosphorylation in vivo. Neurosci. Lett. 516:306–310. 10.1016/j.neulet.2012.04.022 [DOI] [PubMed] [Google Scholar]
- Biessels G.J., and Reijmer Y.D.. 2014. Brain changes underlying cognitive dysfunction in diabetes: what can we learn from MRI? Diabetes. 63:2244–2252. 10.2337/db14-0348 [DOI] [PubMed] [Google Scholar]
- Bomfim T.R., Forny-Germano L., Sathler L.B., Brito-Moreira J., Houzel J.C., Decker H., Silverman M.A., Kazi H., Melo H.M., McClean P.L., et al. 2012. An anti-diabetes agent protects the mouse brain from defective insulin signaling caused by Alzheimer’s disease-associated Aβ oligomers. J. Clin. Invest. 122:1339–1353. 10.1172/JCI57256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brief D.J., and Davis J.D.. 1984. Reduction of food intake and body weight by chronic intraventricular insulin infusion. Brain Res. Bull. 12:571–575. 10.1016/0361-9230(84)90174-6 [DOI] [PubMed] [Google Scholar]
- Bucht G., Adolfsson R., Lithner F., and Winblad B.. 1983. Changes in blood glucose and insulin secretion in patients with senile dementia of Alzheimer type. Acta Med. Scand. 213:387–392. 10.1111/j.0954-6820.1983.tb03756.x [DOI] [PubMed] [Google Scholar]
- Chao A.C., Lee T.C., Juo S.H., and Yang D.I.. 2016. Hyperglycemia Increases the Production of Amyloid β-peptide leading to decreased endothelial tight junction. CNS Neurosci. Ther. 22:291–297. 10.1111/cns.12503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Zhao Y., Dai C.L., Liang Z., Run X., Iqbal K., Liu F., and Gong C.X.. 2014. Intranasal insulin restores insulin signaling, increases synaptic proteins, and reduces Aβ level and microglia activation in the brains of 3xTg-AD mice. Exp. Neurol. 261:610–619. 10.1016/j.expneurol.2014.06.004 [DOI] [PubMed] [Google Scholar]
- Chua L.M., Lim M.L., Chong P.R., Hu Z.P., Cheung N.S., and Wong B.S.. 2012. Impaired neuronal insulin signaling precedes Aβ42 accumulation in female AβPPsw/PS1ΔE9 mice. J. Alzheimers Dis. 29:783–791. [DOI] [PubMed] [Google Scholar]
- Claxton A., Baker L.D., Wilkinson C.W., Trittschuh E.H., Chapman D., Watson G.S., Cholerton B., Plymate S.R., Arbuckle M., and Craft S.. 2013. Sex and ApoE genotype differences in treatment response to two doses of intranasal insulin in adults with mild cognitive impairment or Alzheimer’s disease. J. Alzheimers Dis. 35:789–797. 10.3233/JAD-122308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claxton A., Baker L.D., Hanson A., Trittschuh E.H., Cholerton B., Morgan A., Callaghan M., Arbuckle M., Behl C., and Craft S.. 2015. Long acting intranasal insulin detemir improves cognition for adults with mild cognitive impairment or early-stage Alzheimer’s disease dementia. J. Alzheimers Dis. 45:1269–1270. 10.3233/JAD-15900 [DOI] [PubMed] [Google Scholar]
- Craft S., Newcomer J., Kanne S., Dagogo-Jack S., Cryer P., Sheline Y., Luby J., Dagogo-Jack A., and Alderson A.. 1996. Memory improvement following induced hyperinsulinemia in Alzheimer’s disease. Neurobiol. Aging. 17:123–130. [DOI] [PubMed] [Google Scholar]
- Craft S., Peskind E., Schwartz M.W., Schellenberg G.D., Raskind M., and Porte D. Jr. 1998. Cerebrospinal fluid and plasma insulin levels in Alzheimer’s disease: relationship to severity of dementia and apolipoprotein E genotype. Neurology. 50:164–168. 10.1212/WNL.50.1.164 [DOI] [PubMed] [Google Scholar]
- Craft S., Asthana S., Newcomer J.W., Wilkinson C.W., Matos I.T., Baker L.D., Cherrier M., Lofgreen C., Latendresse S., Petrova A., et al. 1999. Enhancement of memory in Alzheimer disease with insulin and somatostatin, but not glucose. Arch. Gen. Psychiatry. 56:1135–1140. 10.1001/archpsyc.56.12.1135 [DOI] [PubMed] [Google Scholar]
- Craft S., Asthana S., Schellenberg G., Baker L., Cherrier M., Boyt A.A., Martins R.N., Raskind M., Peskind E., and Plymate S.. 2000. Insulin effects on glucose metabolism, memory, and plasma amyloid precursor protein in Alzheimer’s disease differ according to apolipoprotein-E genotype. Ann. N. Y. Acad. Sci. 903:222–228. 10.1111/j.1749-6632.2000.tb06371.x [DOI] [PubMed] [Google Scholar]
- Craft S., Asthana S., Cook D.G., Baker L.D., Cherrier M., Purganan K., Wait C., Petrova A., Latendresse S., Watson G.S., et al. 2003. Insulin dose-response effects on memory and plasma amyloid precursor protein in Alzheimer’s disease: interactions with apolipoprotein E genotype. Psychoneuroendocrinology. 28:809–822. 10.1016/S0306-4530(02)00087-2 [DOI] [PubMed] [Google Scholar]
- Craft S., Baker L.D., Montine T.J., Minoshima S., Watson G.S., Claxton A., Arbuckle M., Callaghan M., Tsai E., Plymate S.R., et al. 2012. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch. Neurol. 69:29–38. 10.1001/archneurol.2011.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankner R., Chetrit A., Shanik M.H., Raz I., and Roth J.. 2009. Basal-state hyperinsulinemia in healthy normoglycemic adults is predictive of type 2 diabetes over a 24-year follow-up: a preliminary report. Diabetes Care. 32:1464–1466. 10.2337/dc09-0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Felice F.G., Vieira M.N., Bomfim T.R., Decker H., Velasco P.T., Lambert M.P., Viola K.L., Zhao W.Q., Ferreira S.T., and Klein W.L.. 2009. Protection of synapses against Alzheimer’s-linked toxins: insulin signaling prevents the pathogenic binding of Aβ oligomers. Proc. Natl. Acad. Sci. USA. 106:1971–1976. 10.1073/pnas.0809158106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitriadis G., Mitrou P., Lambadiari V., Maratou E., and Raptis S.A.. 2011. Insulin effects in muscle and adipose tissue. Diabetes Res. Clin. Pract. 93:S52–S59. 10.1016/S0168-8227(11)70014-6 [DOI] [PubMed] [Google Scholar]
- Draznin B. 2006. Molecular mechanisms of insulin resistance: serine phosphorylation of insulin receptor substrate-1 and increased expression of p85alpha: the two sides of a coin. Diabetes. 55:2392–2397. 10.2337/db06-0391 [DOI] [PubMed] [Google Scholar]
- Fernandez A.M., and Torres-Alemán I.. 2012. The many faces of insulin-like peptide signalling in the brain. Nat. Rev. Neurosci. 13:225–239. 10.1038/nrn3209 [DOI] [PubMed] [Google Scholar]
- Fishel M.A., Watson G.S., Montine T.J., Wang Q., Green P.S., Kulstad J.J., Cook D.G., Peskind E.R., Baker L.D., Goldgaber D., et al. 2005. Hyperinsulinemia provokes synchronous increases in central inflammation and beta-amyloid in normal adults. Arch. Neurol. 62:1539–1544. 10.1001/archneur.62.10.noc50112 [DOI] [PubMed] [Google Scholar]
- Freude S., Plum L., Schnitker J., Leeser U., Udelhoven M., Krone W., Bruning J.C., and Schubert M.. 2005. Peripheral hyperinsulinemia promotes tau phosphorylation in vivo. Diabetes. 54:3343–3348. 10.2337/diabetes.54.12.3343 [DOI] [PubMed] [Google Scholar]
- Freude S., Hettich M.M., Schumann C., Stöhr O., Koch L., Köhler C., Udelhoven M., Leeser U., Müller M., Kubota N., et al. 2009. Neuronal IGF-1 resistance reduces Abeta accumulation and protects against premature death in a model of Alzheimer’s disease. FASEB J. 23:3315–3324. 10.1096/fj.09-132043 [DOI] [PubMed] [Google Scholar]
- Frölich L., Blum-Degen D., Bernstein H.G., Engelsberger S., Humrich J., Laufer S., Muschner D., Thalheimer A., Türk A., Hoyer S., et al. 1998. Brain insulin and insulin receptors in aging and sporadic Alzheimer’s disease. J Neural Transm (Vienna). 105:423–438. 10.1007/s007020050068 [DOI] [PubMed] [Google Scholar]
- Fujisawa Y., Sasaki K., and Akiyama K.. 1991. Increased insulin levels after OGTT load in peripheral blood and cerebrospinal fluid of patients with dementia of Alzheimer type. Biol. Psychiatry. 30:1219–1228. 10.1016/0006-3223(91)90158-I [DOI] [PubMed] [Google Scholar]
- Gasparini L., Gouras G.K., Wang R., Gross R.S., Beal M.F., Greengard P., and Xu H.. 2001. Stimulation of beta-amyloid precursor protein trafficking by insulin reduces intraneuronal β-amyloid and requires mitogen-activated protein kinase signaling. J. Neurosci. 21:2561–2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil-Bea F.J., Solas M., Solomon A., Mugueta C., Winblad B., Kivipelto M., Ramirez M.J., and Cedazo-Mínguez A.. 2010. Insulin levels are decreased in the cerebrospinal fluid of women with prodomal Alzheimer’s disease. J. Alzheimers Dis. 22:405–413. [DOI] [PubMed] [Google Scholar]
- Griffin R.J., Moloney A., Kelliher M., Johnston J.A., Ravid R., Dockery P., O’Connor R., and O’Neill C.. 2005. Activation of Akt/PKB, increased phosphorylation of Akt substrates and loss and altered distribution of Akt and PTEN are features of Alzheimer’s disease pathology. J. Neurochem. 93:105–117. 10.1111/j.1471-4159.2004.02949.x [DOI] [PubMed] [Google Scholar]
- Ho L., Yemul S., Knable L., Katsel P., Zhao R., Haroutunian V., and Pasinetti G.M.. 2012. Insulin receptor expression and activity in the brains of nondiabetic sporadic Alzheimer’s disease cases. Int. J. Alzheimers Dis. 2012:321280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman D.M., Morris J.C., and Goate A.M.. 2011. Alzheimer’s disease: the challenge of the second century. Sci. Transl. Med. 3:77sr1 10.1126/scitranslmed.3002369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoscheidt S.M., Starks E.J., Oh J.M., Zetterberg H., Blennow K., Krause R.A., Gleason C.E., Puglielli L., Atwood C.S., Carlsson C.M., et al. 2016. Insulin resistance is associated with increased levels of cerebrospinal fluid biomarkers of Alzheimer's disease and reduced memory function in at-risk healthy middle-aged adults. J. Alzheimers Dis. 12:1373–1383. 10.3233/JAD-160110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janson J., Laedtke T., Parisi J.E., O’Brien P., Petersen R.C., and Butler P.C.. 2004. Increased risk of type 2 diabetes in Alzheimer disease. Diabetes. 53:474–481. 10.2337/diabetes.53.2.474 [DOI] [PubMed] [Google Scholar]
- Kapogiannis D., Boxer A., Schwartz J.B., Abner E.L., Biragyn A., Masharani U., Frassetto L., Petersen R.C., Miller B.L., and Goetzl E.J.. 2015. Dysfunctionally phosphorylated type 1 insulin receptor substrate in neural-derived blood exosomes of preclinical Alzheimer’s disease. FASEB J. 29:589–596. 10.1096/fj.14-262048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuusisto J., Koivisto K., Mykkänen L., Helkala E.L., Vanhanen M., Hänninen T., Kervinen K., Kesäniemi Y.A., Riekkinen P.J., and Laakso M.. 1997. Association between features of the insulin resistance syndrome and Alzheimer’s disease independently of apolipoprotein E4 phenotype: cross sectional population based study. BMJ. 315:1045–1049. 10.1136/bmj.315.7115.1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Last D., Alsop D.C., Abduljalil A.M., Marquis R.P., de Bazelaire C., Hu K., Cavallerano J., and Novak V.. 2007. Global and regional effects of type 2 diabetes on brain tissue volumes and cerebral vasoreactivity. Diabetes Care. 30:1193–1199. 10.2337/dc06-2052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Liu F., Grundke-Iqbal I., Iqbal K., and Gong C.X.. 2011. Deficient brain insulin signalling pathway in Alzheimer’s disease and diabetes. J. Pathol. 225:54–62. 10.1002/path.2912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchsinger J.A., Tang M.X., Shea S., and Mayeux R.. 2004. Hyperinsulinemia and risk of Alzheimer disease. Neurology. 63:1187–1192. 10.1212/01.WNL.0000140292.04932.87 [DOI] [PubMed] [Google Scholar]
- Ma J., Zhang W., Wang H.F., Wang Z.X., Jiang T., Tan M.S., Yu J.T., and Tan L.. 2016. Peripheral blood adipokines and insulin levels in patients with Alzheimer’s disease: a replication study and meta-analysis. Curr. Alzheimer Res. 13:223–233. 10.2174/156720501303160217111434 [DOI] [PubMed] [Google Scholar]
- Ma Q.L., Yang F., Rosario E.R., Ubeda O.J., Beech W., Gant D.J., Chen P.P., Hudspeth B., Chen C., Zhao Y., et al. 2009. Beta-amyloid oligomers induce phosphorylation of tau and inactivation of insulin receptor substrate via c-Jun N-terminal kinase signaling: suppression by omega-3 fatty acids and curcumin. J. Neurosci. 29:9078–9089. 10.1523/JNEUROSCI.1071-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macauley S.L., Stanley M., Caesar E.E., Yamada S.A., Raichle M.E., Perez R., Mahan T.E., Sutphen C.L., and Holtzman D.M.. 2015. Hyperglycemia modulates extracellular amyloid-β concentrations and neuronal activity in vivo. J. Clin. Invest. 125:2463–2467. 10.1172/JCI79742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maioli S., Lodeiro M., Merino-Serrais P., Falahati F., Khan W., Puerta E., Codita A., Rimondini R., Ramirez M.J., Simmons A., et al. Alzheimer’s Disease Neuroimaging Initiative . 2015. Alterations in brain leptin signalling in spite of unchanged CSF leptin levels in Alzheimer’s disease. Aging Cell. 14:122–129. 10.1111/acel.12281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNay E.C., and Recknagel A.K.. 2011. Brain insulin signaling: a key component of cognitive processes and a potential basis for cognitive impairment in type 2 diabetes. Neurobiol. Learn. Mem. 96:432–442. 10.1016/j.nlm.2011.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNay E.C., Ong C.T., McCrimmon R.J., Cresswell J., Bogan J.S., and Sherwin R.S.. 2010. Hippocampal memory processes are modulated by insulin and high-fat-induced insulin resistance. Neurobiol. Learn. Mem. 93:546–553. 10.1016/j.nlm.2010.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina J.A., Jiménez-Jiménez F.J., Vargas C., Gómez P., de Bustos F., Gómez-Escalonilla C., Zurdo M., Tallón A., Martínez-Salio A., Porta-Etessam J., et al. 2002. Cerebrospinal fluid levels of insulin in patients with Alzheimer’s disease. Acta Neurol. Scand. 106:347–350. 10.1034/j.1600-0404.2002.01326.x [DOI] [PubMed] [Google Scholar]
- Moloney A.M., Griffin R.J., Timmons S., O’Connor R., Ravid R., and O’Neill C.. 2010. Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer’s disease indicate possible resistance to IGF-1 and insulin signalling. Neurobiol. Aging. 31:224–243. 10.1016/j.neurobiolaging.2008.04.002 [DOI] [PubMed] [Google Scholar]
- Musiek E.S., and Holtzman D.M.. 2015. Three dimensions of the amyloid hypothesis: time, space and ‘wingmen’. Nat. Neurosci. 18:800–806. 10.1038/nn.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak V., Milberg W., Hao Y., Munshi M., Novak P., Galica A., Manor B., Roberson P., Craft S., and Abduljalil A.. 2014. Enhancement of vasoreactivity and cognition by intranasal insulin in type 2 diabetes. Diabetes Care. 37:751–759. 10.2337/dc13-1672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei J.J., Khatoon S., An W.L., Nordlinder M., Tanaka T., Braak H., Tsujio I., Takeda M., Alafuzoff I., Winblad B., et al. 2003. Role of protein kinase B in Alzheimer’s neurofibrillary pathology. Acta Neuropathol. 105:381–392. [DOI] [PubMed] [Google Scholar]
- Peila R., Rodriguez B.L., White L.R., and Launer L.J.. 2004. Fasting insulin and incident dementia in an elderly population of Japanese-American men. Neurology. 63:228–233. 10.1212/01.WNL.0000129989.28404.9B [DOI] [PubMed] [Google Scholar]
- Phiel C.J., Wilson C.A., Lee V.M., and Klein P.S.. 2003. GSK-3alpha regulates production of Alzheimer’s disease amyloid-βpeptides. Nature. 423:435–439. 10.1038/nature01640 [DOI] [PubMed] [Google Scholar]
- Qiu W.Q., Walsh D.M., Ye Z., Vekrellis K., Zhang J., Podlisny M.B., Rosner M.R., Safavi A., Hersh L.B., and Selkoe D.J.. 1998. Insulin-degrading enzyme regulates extracellular levels of amyloid beta-protein by degradation. J. Biol. Chem. 273:32730–32738. 10.1074/jbc.273.49.32730 [DOI] [PubMed] [Google Scholar]
- Reger M.A., Watson G.S., Green P.S., Wilkinson C.W., Baker L.D., Cholerton B., Fishel M.A., Plymate S.R., Breitner J.C., DeGroodt W., et al. 2008. Intranasal insulin improves cognition and modulates β-amyloid in early AD. Neurology. 70:440–448. 10.1212/01.WNL.0000265401.62434.36 [DOI] [PubMed] [Google Scholar]
- Rivera E.J., Goldin A., Fulmer N., Tavares R., Wands J.R., and de la Monte S.M.. 2005. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer’s disease: link to brain reductions in acetylcholine. J. Alzheimers Dis. 8:247–268. [DOI] [PubMed] [Google Scholar]
- Roberts R.O., Knopman D.S., Cha R.H., Mielke M.M., Pankratz V.S., Boeve B.F., Kantarci K., Geda Y.E., Jack C.R. Jr., Petersen R.C., and Lowe V.J.. 2014. Diabetes and elevated hemoglobin A1c levels are associated with brain hypometabolism but not amyloid accumulation. J. Nucl. Med. 55:759–764. 10.2967/jnumed.113.132647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajan M., Hansen B., Ivey R. III, Sajan J., Ari C., Song S., Braun U., Leitges M., Farese-Higgs M., and Farese R.V.. 2016. Brain insulin signaling is increased in insulin-resistant states and decreases in FOXOs and PGC-1α and increases in Aβ1-40/42 and phospho-tau may abet Alzheimer development. Diabetes. 65:1892–1903. 10.2337/db15-1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salameh T.S., Bullock K.M., Hujoel I.A., Niehoff M.L., Wolden-Hanson T., Kim J., Morley J.E., Farr S.A., and Banks W.A.. 2015. Central nervous system delivery of intranasal insulin: mechanisms of uptake and effects on cognition. J. Alzheimers Dis. 47:715–728. 10.3233/JAD-150307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartorius T., Peter A., Heni M., Maetzler W., Fritsche A., Häring H.U., and Hennige A.M.. 2015. The brain response to peripheral insulin declines with age: a contribution of the blood-brain barrier? PLoS One. 10:e0126804 10.1371/journal.pone.0126804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindowski K., Bretteville A., Leroy K., Bégard S., Brion J.P., Hamdane M., and Buée L.. 2006. Alzheimer’s disease-like tau neuropathology leads to memory deficits and loss of functional synapses in a novel mutated tau transgenic mouse without any motor deficits. Am. J. Pathol. 169:599–616. 10.2353/ajpath.2006.060002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M., Gautam D., Surjo D., Ueki K., Baudler S., Schubert D., Kondo T., Alber J., Galldiks N., Küstermann E., et al. 2004. Role for neuronal insulin resistance in neurodegenerative diseases. Proc. Natl. Acad. Sci. USA. 101:3100–3105. 10.1073/pnas.0308724101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiiki T., Ohtsuki S., Kurihara A., Naganuma H., Nishimura K., Tachikawa M., Hosoya K., and Terasaki T.. 2004. Brain insulin impairs amyloid-beta(1-40) clearance from the brain. J. Neurosci. 24:9632–9637. 10.1523/JNEUROSCI.2236-04.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims-Robinson C., Kim B., Rosko A., and Feldman E.L.. 2010. How does diabetes accelerate Alzheimer disease pathology? Nat. Rev. Neurol. 6:551–559. 10.1038/nrneurol.2010.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling R.A., Aisen P.S., Beckett L.A., Bennett D.A., Craft S., Fagan A.M., Iwatsubo T., Jack C.R. Jr., Kaye J., Montine T.J., et al. 2011. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7:280–292. 10.1016/j.jalz.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks E.J., Patrick O’Grady J., Hoscheidt S.M., Racine A.M., Carlsson C.M., Zetterberg H., Blennow K., Okonkwo O.C., Puglielli L., Asthana S., et al. 2015. Insulin resistance is associated with higher cerebrospinal fluid tau levels in asymptomatic APOEɛ4 carriers. J. Alzheimers Dis. 46:525–533. 10.3233/JAD-150072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steen E., Terry B.M., Rivera E.J., Cannon J.L., Neely T.R., Tavares R., Xu X.J., Wands J.R., and de la Monte S.M.. 2005. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease--is this type 3 diabetes? J. Alzheimers Dis. 7:63–80. [DOI] [PubMed] [Google Scholar]
- Stöhr O., Schilbach K., Moll L., Hettich M.M., Freude S., Wunderlich F.T., Ernst M., Zemva J., Brüning J.C., Krone W., et al. 2013. Insulin receptor signaling mediates APP processing and β-amyloid accumulation without altering survival in a transgenic mouse model of Alzheimer’s disease. Age (Dordr.). 35:83–101. 10.1007/s11357-011-9333-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolk R.P., Breteler M.M., Ott A., Pols H.A., Lamberts S.W., Grobbee D.E., and Hofman A.. 1997. Insulin and cognitive function in an elderly population. The Rotterdam Study. Diabetes Care. 20:792–795. 10.2337/diacare.20.5.792 [DOI] [PubMed] [Google Scholar]
- Talbot K., Wang H.Y., Kazi H., Han L.Y., Bakshi K.P., Stucky A., Fuino R.L., Kawaguchi K.R., Samoyedny A.J., Wilson R.S., et al. 2012. Demonstrated brain insulin resistance in Alzheimer’s disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J. Clin. Invest. 122:1316–1338. 10.1172/JCI59903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger J., McNeill T.H., Moxley R.T. III, White M., Moss A., and Livingston J.N.. 1989. Distribution of insulin receptor-like immunoreactivity in the rat forebrain. Neuroscience. 31:143–157. 10.1016/0306-4522(89)90036-5 [DOI] [PubMed] [Google Scholar]
- Vandal M., White P.J., Tremblay C., St-Amour I., Chevrier G., Emond V., Lefrançois D., Virgili J., Planel E., Giguere Y., et al. 2014. Insulin reverses the high-fat diet-induced increase in brain Aβ and improves memory in an animal model of Alzheimer disease. Diabetes. 63:4291–4301. 10.2337/db14-0375 [DOI] [PubMed] [Google Scholar]
- Wadman M. 2012. US government sets out Alzheimer’s plan. Nature. 485:426–427. 10.1038/485426a [DOI] [PubMed] [Google Scholar]
- Wang X., Zheng W., Xie J.W., Wang T., Wang S.L., Teng W.P., and Wang Z.Y.. 2010. Insulin deficiency exacerbates cerebral amyloidosis and behavioral deficits in an Alzheimer transgenic mouse model. Mol. Neurodegener. 5:46 10.1186/1750-1326-5-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson G.S., Peskind E.R., Asthana S., Purganan K., Wait C., Chapman D., Schwartz M.W., Plymate S., and Craft S.. 2003. Insulin increases CSF Aβ42 levels in normal older adults. Neurology. 60:1899–1903. 10.1212/01.WNL.0000065916.25128.25 [DOI] [PubMed] [Google Scholar]
- Willette A.A., Johnson S.C., Birdsill A.C., Sager M.A., Christian B., Baker L.D., Craft S., Oh J., Statz E., Hermann B.P., et al. 2015. Insulin resistance predicts brain amyloid deposition in late middle-aged adults. Alzheimers Dement. 11:504–510.e1. 10.1016/j.jalz.2014.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L., Helmerhorst E., Taddei K., Plewright B., Van Bronswijk W., and Martins R.. 2002. Alzheimer’s β-amyloid peptides compete for insulin binding to the insulin receptor. J. Neurosci. 22:RC221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarchoan M., Toledo J.B., Lee E.B., Arvanitakis Z., Kazi H., Han L.Y., Louneva N., Lee V.M., Kim S.F., Trojanowski J.Q., and Arnold S.E.. 2014. Abnormal serine phosphorylation of insulin receptor substrate 1 is associated with tau pathology in Alzheimer’s disease and tauopathies. Acta Neuropathol. 128:679–689. 10.1007/s00401-014-1328-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen K., Sloan S.A., Bennett M.L., Scholze A.R., O’Keeffe S., Phatnani H.P., Guarnieri P., Caneda C., Ruderisch N., et al. 2014. An RNA-sequencing transcriptome and splicing database of glia, neurons, and vascular cells of the cerebral cortex. J. Neurosci. 34:11929–11947. 10.1523/JNEUROSCI.1860-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Dai C.L., Chen Y., Iqbal K., Liu F., and Gong C.X.. 2016. Intranasal insulin prevents anesthesia-induced spatial learning and memory deficit in mice. Sci. Rep. 6:21186 10.1038/srep21186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W.Q., De Felice F.G., Fernandez S., Chen H., Lambert M.P., Quon M.J., Krafft G.A., and Klein W.L.. 2008. Amyloid beta oligomers induce impairment of neuronal insulin receptors. FASEB J. 22:246–260. 10.1096/fj.06-7703com [DOI] [PubMed] [Google Scholar]
- Zuchero Y.J., Chen X., Bien-Ly N., Bumbaca D., Tong R.K., Gao X., Zhang S., Hoyte K., Luk W., Huntley M.A., et al. 2016. Discovery of novel blood-brain barrier targets to enhance brain uptake of therapeutic antibodies. Neuron. 89:70–82. 10.1016/j.neuron.2015.11.024 [DOI] [PubMed] [Google Scholar]