Abstract
Increasingly, many patients are diagnosed with a second lung cancer after curative thoracotomy. It is very difficult to manage such patients surgically due to the significant loss of pulmonary function. Especially on the right side, avoiding a completion pneumonectomy may contribute to reducing postoperative functional loss and surgical complications as well as the morbidity of post-pneumonectomy syndrome. A technique is needed to prevent torsion of the preserved middle lobe. Following recently published cases utilizing a latissimus dorsi muscle flap, in this case report, we describe the use of the serratus anterior muscle flap as an alternative.
Keywords: Lung cancer surgery, Completion pneumonectomy, Lobar torsion, Serratus anterior muscle
CASE REPORT
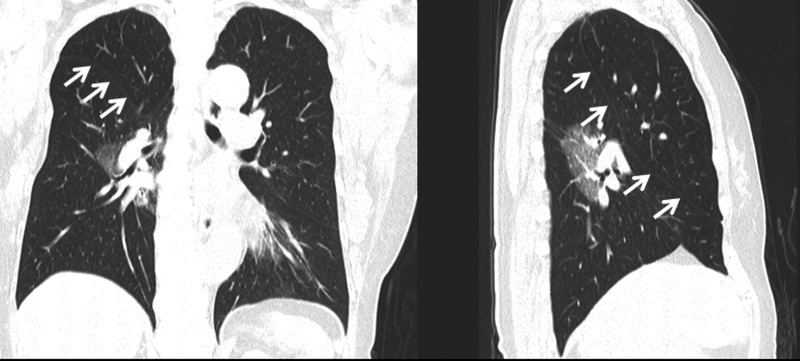
A 62-year old female was referred, who had undergone right upper lobectomy for lung adenocarcinoma 15 years previously. A computed tomography (CT) scan showed a mass in right S6 that was diagnosed as primary lung adenocarcinoma (Fig. 1).
Figure 1:
Preoperative CT images: the arrows indicate a major fissure between the middle and lower lobes 15 years after initial surgery. The residual middle lobe is relatively larger.
The patient's pulmonary function was as follows: forced vital capacity (FVC) was 2540 ml or 105% of the predicted value and forced expiratory volume in 1 s (FEV1) was 1760 ml or 70% of FVC. A pulmonary perfusion scan showed unexpected right-side dominance with 59% of all detected.
We decided to avoid a completion pneumonectomy by preserving the middle lobe. A posterolateral incision with a fifth intercostal thoracotomy seemed to have been performed in the previous operation. We performed the same posterolateral incision on the line of the previous scar with a sixth rib-bed thoracotomy. There was no parietal pleural adhesion. After cautious exfoliation of tightly adhered hilar structures, the affected right lower lobe was removed. Mediastinal lymph node dissection was not performed due to the presence of tight adhesions, which were likely caused by the previous operation. Only one pulmonary artery branch was distributed into the middle lobe. This artery and the middle lobe bronchus formed a stalk-like bundle that was likely to rotate itself. This observation suggested a threat of middle lobe torsion after the procedure.
As a corrective measure, we made use of a muscle flap. The serratus anterior muscle exhibited no signs of dissection performed during the previous operation, unlike the latissimus dorsi muscle. The fibres of the serratus anterior muscle were detached from the third to the seventh rib. Then, the muscle was detached from the inner rim of the scapula, with care taken to preserve both incoming branches of the thoracodorsal and lateral thoracic arteries.
To transpose the muscle flap into the pleural cavity, we dissected the fourth intercostal muscle at the upper rim of the fifth rib with a length of 6 cm. The muscle flap was ligated to the right lower lobe stump using 3-0 non-absorbable twisted threads. The preserved middle lobe looked as if it was laid on a muscle ‘hammock’. The volume of the residual middle lobe was estimated to be about 350 ml at full expansion.
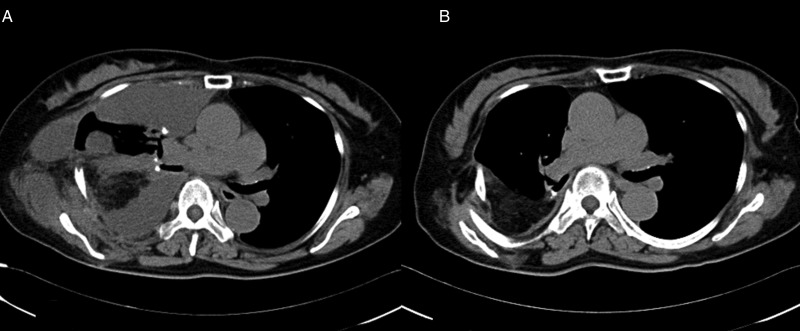
The postoperative course was fair, but a month later over-retention of pleural effusion required 2 weeks of readmission and chest drainage (Fig. 2A).
Figure 2:
(A) CT image 1 month after the operation. Over-retention of pleural effusion required 2 weeks readmission and chest drainage. The density of the muscle flap is less than that of normal chest wall muscles, which may indicate degeneration of the muscle flap. (B) CT image 8 months after the operation. Pleural effusion, as well as the residual pleural space, has almost disappeared with excellent middle lobe expansion and fixation. The serratus anterior muscle flap is fixed backwards in the pleural cavity.
A pulmonary function test 2 years after the operation was excellent: FVC was 1850 ml or 77% of predicted value, and FEV1 was 1380 ml or 74% of FVC. The patient was able to resume her normal activity a couple of months later with minimal physical disturbance, and no decline of activity was noted 3 years later.
DISCUSSION
When a second lung cancer occurs in the right upper lobe after lower lobectomy, or conversely in the right lower lobe after upper lobectomy, completion pneumonectomy is normally selected if the patient's cardiopulmonary function allows it [1]. In our case, the values of the pulmonary function test and pulmonary perfusion scan suggested that a completion pneumonectomy would have caused a considerable decline of cardiopulmonary function, which the patient was unlikely to be able to bear. In addition, there would have been a greater risk of post-surgical complications in the short term and a risk of post-pneumonectomy syndrome in the long term if completion pneumonectomy was performed [2]. CT imaging and pulmonary perfusion scan showed that the patient's right middle lobe held a certain lung volume with more blood flow than was expected. Although the patient's tumour showed a pure ground glass nodule pattern on CT images, intraoperative findings did not permit a limited operation such as extended S6 segmentectomy because the tumour margin was too close to the basal pulmonary artery. Hence, we decided to perform a middle lobe preserving right lower lobectomy.
A procedure in which only the middle lobe is left might lead to a risk of fatal torsion of the preserved middle lobe. Torsion of the middle lobe can occur even after normal right upper lobectomy or lower lobectomy [3]. To avoid such a critical complication, the following measures were undertaken: fixation of the hilar stalk by ligating a transposed muscle flap to the bronchial stump. In a previously reported case [4], a latissimus dorsi flap was utilized to prevent such torsion. Because there are few reports of middle lobe preserving right upper and lower bilobectomy, the most efficient way of stabilizing a preserved middle lobe remains controversial. Moreover, in our case, the latissimus dorsi muscle had been dissected and ligated in a previous operation, resulting in a threat of transposed muscle flap necrosis. This led us to use the serratus anterior muscle flap. The serratus anterior muscle flap might also contribute to a more natural and preferable fixation of the residual middle lobe than the latissimus dorsi muscle flap. Because one end of the serratus anterior is located on the inner rim of the scapula, it would retract the ligated stump backwards (Fig. 2B). In contrast, one end of the latissimus dorsi is located on the humerus. Therefore, the latissimus dorsi flap may move the stump forwards, potentially disturbing middle lobe expansion to some degree.
The technique described here has a couple of advantages: (i) the muscle flap, which partially fills the residual pleural cavity with the middle lobe, may prevent a hyper-shift of the mediastinum; (ii) covering the bronchial stump may prevent bronchopleural fistula. Nonetheless, two adverse effects should also be noted: (i) excessive muscle flap detachment from the scapula may result in winging shoulder; (ii) over-retention of pleural effusion is frequently reported in cases where the serratus anterior muscle flap is transposed [5]. As these adverse effects are less important than the advantages, we conclude that the use of the serratus anterior muscle flap for the prevention of preserved middle lobe torsion is both effective and practical, even though it is unlikely to be adopted as standard practice.
Conflict of interest: none declared.
REFERENCES
- 1.Fabian T, Docekal JW. Avoidance of completion pneumonectomy by sparing the right middle lobe. J Thorac Cardiovasc Surg 2014;147:e80–2. [DOI] [PubMed] [Google Scholar]
- 2.Pan X, Fu S, Shi J, Yang J, Zhao H. The early and long-term effect of completion pneumonectomy: report of 56 cases. Interact CardioVasc Thorac Surg 2014;19:436–40. [DOI] [PubMed] [Google Scholar]
- 3.Cable DG, Deschamps C, Allen MS, Miller DL, Nichols FC, Trastek VF et al. Lober torsion after pulmonary resection: presentation and outcome. J Thorac Cardiovasc Surg 2001;122:1091–3. [DOI] [PubMed] [Google Scholar]
- 4.Moriyama S, Yano M, Sasaki H, Hirosaka Y, Yokota K, Fuji Y. Middle lobe preservation and fixation: right upper and lower sleeve lobectomy. How to do it. Surg Today 2012;42:610–2. [DOI] [PubMed] [Google Scholar]
- 5.Groth SS, Whitson BA, Cunha J, Andrade RS, Landis GH, Maddaus MA. Serratus anterior transposition muscle flaps for bronchial coverage: technique and functional outcomes. Ann Thorac Surg 2009;88:2044–6. [DOI] [PubMed] [Google Scholar]