Abstract
Please cite this paper as: Spekreijse et al. (2013) Quantification of dust‐borne transmission of highly pathogenic avian influenza virus between chickens. Influenza and Other Respiratory Viruses 7(2) 132–138.
Background Understanding the transmission of highly pathogenic avian influenza virus (HPAIv) between poultry flocks is essential to prevent and control epidemics. Dust, produced in infected chicken flocks, has been hypothesized to be an important mechanical vector for between‐flock transmission of HPAIv.
Objectives The aim of our study was to quantify the amount of virus shed by infected birds and its relation to deposition of virus in the environment and the rate of dust‐borne transmission between groups of chickens.
Methods Four replicate experiments were performed, each replicate with two groups of 14 chickens housed in two separate rooms. In one group, chickens were inoculated with HPAIv. Ventilation forced the air from that room to the second (recipient) group through a tube. Deceased birds in the inoculated group were replaced with new susceptible birds up to day 10 p.i. Dust samples were collected daily. Trachea and cloaca swabs were collected daily to determine virus shedding and virus spread to the recipient group.
Results The amount of virus detected in dust samples in the recipient room was, on average, 103·7 EID50/m3. Virus transmission from the inoculated to the recipient group occurred in two experiments. The transmission rate parameter for dust‐borne transmission was estimated at 0·08 new infections/infectious chicken/day.
Conclusions The results of this study are a first step to elucidate the importance of dust‐borne transmission of HPAIv between flocks and help interpret environmental samples.
Keywords: Airborne transmission, dust, H5N1, highly pathogenic avian influenza virus
Introduction
Highly pathogenic avian influenza (HPAI) is a contagious and devastating viral disease of poultry caused by influenza type A strains carrying the haemagglutinin H5 or H7. Outbreaks of HPAI virus (HPAIv) H5N1 have occurred in several countries in Europe, Asia and Africa, and the virus is currently endemic in, amongst others, China, Egypt and Indonesia, causing economic losses and animal welfare problems. 1 In addition, in 15 countries, human cases were reported since the first outbreak in Hong Kong in 1997, and the disease is considered a threat for public health because of the risk of reassortment with other influenza A viruses which may result in a new pandemic. 2
Eradication of HPAIv is difficult and mainly achieved by culling of large numbers of (infected) poultry. 3 , 4 , 5 , 6 , 7 Because of this massive culling of flocks, improvement of control measures is necessary, which requires more knowledge on the epidemiology of the disease and the role of different routes of transmission between flocks.
One of the routes suggested is airborne transmission. During the 2004 HPAI outbreak in British Colombia live virus was found in dust samples collected around infected flocks, 8 and Chen et al. 9 found RNA of influenza viruses attached to dust particles originating from Asian dust storms and hypothesized the possibility of dust‐borne transmission of HPAIv. Poultry flocks generate high concentrations of dust that consists of bedding, feathers and faeces, but can also contain high concentrations of micro‐organisms. 10 , 11 , 12 , 13 , 14 Previous studies detected Campylobacter, Salmonella, Newcastle disease and Marek’s disease in dust samples collected from broiler flocks. 12 , 15 , 16 , 17 , 18 Because of artificial ventilation systems, but also during transport of birds or manure, dust is emitted into the environment and can become a mechanical vector for micro‐organisms. Dust particles may be subsequently transported by wind over large distances up to kilometres, and in that way may become a route for the spread of infectious particles between poultry flocks. 19 , 20
Up to now, evidence for transmission of HPAIv by dust is sparse and more insight into this matter may be helpful for interpreting results from environmental samples and to develop prevention strategies, for example, minimal acceptable distance between flocks. Moreover, it might improve control measures for personnel working on infected flocks, which may become infected after exposure to contaminated dust particles or to provide insight into the risk of exposure for people living in the proximity to poultry flocks. 9 , 21 , 22 , 23 , 24 , 25 , 26
Studying dust‐borne virus spread of HPAIv during a disease‐free period is difficult, and the only way of gaining insight into distance‐related spread is by doing experiments. In a previous study, the rate of airborne transmission of HPAIv over short distances (up to 1·2 m) within an experimental unit was determined, and it was demonstrated that virus could be transmitted over a short distance and that dust was the possible vector of transmission. 26 A study by Yee et al. 25 demonstrated that airborne transmission of a low pathogenic avian influenza virus could be an important route of transmission of virus in life bird markets. However, in these studies, transmission was only determined qualitatively, meaning that the relation between viral load and probability of infection remains unknown.
Therefore, quantitative data are necessary for the risk assessment on transmission of virus to human and animal. However, up to now, no data are available on the amount of shedding by infected birds and its relation to environmental deposition of dust‐borne virus and the rate of dust‐borne transmission. In this study, we performed four animal experiments in which we quantified the amount of virus shed by infected birds and its relation to deposition of virus in the environment and the rate of dust‐borne transmission between groups of chickens.
Materials and methods
Animals
Embryonated eggs from White leghorn chickens were purchased from a commercial AIV‐free poultry breeder farm and hatched at the Central Veterinary Institute (CVI) in Lelystad. After hatching, the chickens were housed in one room. At 5 weeks of age, the chickens were tested for the presence of antibodies against AI using a modified indirect double‐antibody sandwich (IDAS) nucleoprotein (NP)‐blocking ELISA. 27 The chickens were housed on the floor with bedding material of wood shavings and sawdust. Irradiated rearing feed and tap water were provided ad libitum.
Inoculum
For inoculation, the HPAI virus strain A/turkey/Turkey/1/2005 H5N1 (clade 2·2) was used as challenge strain. 28 , 29 The virus was grown in the embryonated SPF eggs, and vials with a known egg infectious dose (EID50) titre were stored at −70°C until use. On the day of challenge, one vial was thawed and diluted in 10‐fold dilution steps in tryptose phosphate buffer (TPB) to obtain the necessary inoculation dose of 104 EID50. Chickens were inoculated with 0·1 ml inoculum applied intranasally and 0·1 ml inoculum applied intratracheally using a blunt needle, according to a standard protocol. 29 , 30
Experimental design
Four replicate experiments, 1–4, were carried out consecutively (Table 1). The experiments complied with the Dutch law on animal experiments and were reviewed by an animal ethics committee. Each of the four replicate experiments consisted of two separately housed groups of 14 chickens. Each group was housed in an isolation unit (volume of 22 m3) under BSL3+ conditions at the CVI in an open cage of 2 m2. The two isolation units were connected with a tube (Figure 1). The inlet of the tube started above the open cage from the first isolation room and the outlet of the tube ended above the open cage from the second room. Ventilation forced all air from the first room to the second room through the tube. The units were ventilated at an average flow of 225 m3/hour (range from 217–233 m3/hour) through the tube. At this air flow, dust deposition on the plastic smooth tube is unlikely. Room temperature was kept at 21°C and a relative humidity of 55%.
Table 1.
Summary of variables and virus detection with RT‐qPCR (expressed as log10 EID50 equivalents/m2 of wall or m3 of air) in the different dust samples p.i of the four replicate experiments. Samples not available are ‘na’
| Trial | Dust sampling | Virus titre (log10 EID50/m2 or/m3) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Room | Apparatus | Sampling time (minutes) | Area (m2) | Number of infected birds | Number of non‐infected birds | Days post‐inoculation | ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 13 | 14 | |||||||
| 1 | Inoculated | 48 | 0 | |||||||||||||||
| Recipient | MD8 | 90 | 0 | 14 | 0 | 2·9 | 2·1 | 3·1 | 2·6 | 2·8 | 2·9 | 2·7 | 0 | 0 | na | na | ||
| 2 | Inoculated | 35 | 1 | |||||||||||||||
| Recipient | Andersen – non‐respirable | 90 | 14 | 0 | 0 | 0 | 0 | 2·3 | 0 | 1·5 | 0 | 0 | 0 | 0 | na | na | ||
| Recipient | Andersen – respirable | 90 | 0 | 0 | 0 | 0 | 2·0 | 0 | 0 | 0 | 2·2 | 2·8 | na | na | ||||
| 3 | Inoculated | Dust cloths | 0·1 | 30 | 7 | 0 | 3·9 | 5·0 | 3·7 | 4·9 | 5·1 | 4·8 | 4·9 | 4·8 | 4·4 | 4·9 | 3·5 | |
| Recipient | Dust cloths | 0·1 | 0 | 14 | 0 | 2·9 | 4·0 | 3·9 | 3·9 | 4·5 | 4·0 | 4·4 | 4·5 | 3·9 | 3·8 | 2·7 | ||
| Recipient | Andersen – non‐respirable | 270 | 0 | 0 | 0 | 2·5 | 0 | 3·1 | 0 | 3·1 | 2·4 | 2·5 | 2·7 | 3·4 | ||||
| Recipient | Andersen – respirable | 270 | 0 | 2·4 | 0 | 2·9 | 2·7 | 0 | 0 | 3·3 | 2·5 | 3·2 | 2·5 | 2·8 | ||||
| 4 | Inoculated | Dust cloths | 0·1 | 47 | 0 | 0 | 3·3 | 4·5 | 4·6 | 4·1 | 4·6 | 4·9 | 4·8 | 5·0 | 4·9 | 5·4 | 3·9 | |
| Recipient | Dust cloths | 0·1 | 14 | 0 | 0 | 0 | 3·5 | 3·2 | 3·9 | 4·1 | 4·7 | 4·8 | 3·9 | 4·2 | 4·7 | 3·5 | ||
| Recipient | MD8 | 270 | 0 | 2·5 | 2·9 | 3·5 | 3·2 | 4·1 | 3·9 | 3·5 | 4·0 | 3·7 | 3·5 | 3·7 | ||||
Figure 1.
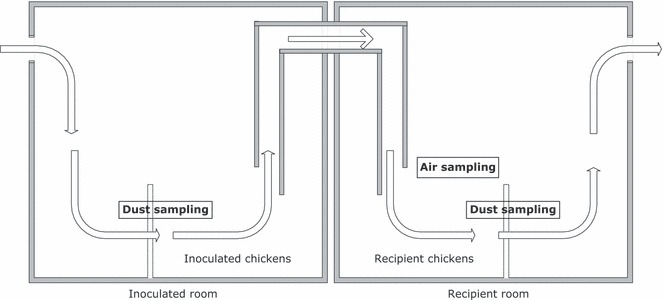
Overview of the connected rooms with locations of the groups of chickens, dust sampling and air sampling. The arrows represent the airflow from the inoculated to the recipient room.
In the first room, eight of 14 chickens were inoculated with HPAI H5N1 virus. The remaining six birds were contact‐exposed p.i. Deceased birds in this inoculated group were replaced daily with new susceptible ones up to 10 days p.i. to generate a constant source of virus shedding that was verified by taking swabs. In the second room, birds were not treated. Deceased birds in this recipient group were removed but not replaced.
Sampling procedures
At day 1 p.i., swabs from trachea and cloaca were collected from inoculated chickens and at days 2 to 10 p.i., from all chickens. In experiments 3 and 4, swabs from trachea and cloaca were also collected on days 13 and 14 p.i. because of the results of experiments 1 and 2. The swabs were put in 2 ml of 2·95% TPB with 5 × 103 IU of penicillin–sodium and 5 mg streptomycin/ml and stored at −70°C until analysed.
In experiments 3 and 4, from day 1 to 10, 13 and 14 p.i., additional dust samples were collected from the wall (Figure 1) of the inoculated and recipient units, using electrostatic dust cloths (Swiffer, Procter and Gamble, U.S.). Per room, a defined section of 0·1 m2 of wall was marked and sampled daily to determine viral deposition in 24 hours. The dust cloths were put in 10 ml of 2·95% TPB with 5 × 103 IU of penicillin–sodium and 5 mg streptomycin/ml and stored at −70°C until analysed.
Air samples were collected during days 1–10 p.i. from the air flowing to the recipient group (Figure 1) using either an MD8 air‐scan air sampling device (Sartorius, Nieuwegein, the Netherlands) (experiments 1 and 3) or a two‐stage viable Andersen Cascade Impactor (Thermo Scientific, Franklin, MA, USA) (experiments 2 and 4). In experiments 3 and 4, air samples were also collected on days 13 and 14.
MD8 air samples were taken at an air speed of 2 m3/hour using sterile gelatine filters of 80 mm diameter and 3 μm pore size, and Andersen air samples were taken at an air speed of 1·7 m3/hour (28·3 l/minutes) using sterile gelatine filters to collect the dust. In the latter, the particles were grouped by their aerodynamic diameters. 31 The fractions of dust collected with the Andersen were divided into a non‐respirable fraction (PM > 8 μm) and a respirable fraction (PM ≤ 8 μm). In experiments 1 and 2, air was sampled for 90 minutes; in experiments 3 and 4, this time was increased to 270 minutes.
After sampling, the gelatine filters were dissolved in 10 ml of 2·95% TPB with 5 × 103 IU of penicillin–sodium and 5 mg streptomycin/ml at a temperature of 37°C. Dissolved filter solutions were stored at −70°C until analysed. Viral load was determined for each gelatine filter, and positive RT‐qPCR results were confirmed with virus isolation. The experiments were terminated 21 days p.i. by euthanizing surviving birds with an intracardiac injection of T‐61.
RNA isolation and quantitative real‐time reverse transcriptase PCR (RT‐qPCR)
RNA isolation was performed with the MagNA Pure LC 2·0 instrument (Roche Applied Science, Mannheim, Germany) using the MagNA Pure LC total Nucleic Acid Isolation Kit (Roche Applied Science). The viral RNA was isolated from 200 μl of swab fluid or filter solution according to the manufacturer’s instructions. The nucleic acids were collected in elution buffer and stored at −70°C or directly processed for the quantitative real‐time reverse transcriptase PCR (RT‐qPCR). The RT‐qPCR and data analysis were performed using the MX4000 Quantitative PCR system (Stratagene, Santa Clara, CA, USA) with version 4·20 software. To detect the matrix gene of the influenza A virus, 5 μl of the elution buffer with extracted RNA was used for RT‐qPCR as described in van der Goot. 32 The viral RNA concentration of each sample could be calculated using a calibration curve of serial dilutions of a standard batch of the virus with a known EID50 titre. Dilutions of the standard batch were run along with the unknown samples. Quantification of the viral concentration in each sample was based on the calibration curve generated by plotting the cycle threshold value against known virus titres. Results are given in 10 log virus titres, expressed as equivalent units of EID50/ml.
Serology
Blood samples were taken from the ulnar vein 7 days before and at days 7, 14 and 21 p.i. from all chickens. The blood was coagulated at room temperature and serum collected and stored at −20°C until use. Sera were incubated for 30 minutes at 56 °C and tested using a modified IDAS nucleoprotein (NP)‐blocking ELISA to detect antibodies against the nucleoprotein of influenza A. 27
Virus isolation
For virus isolation, for each swab, three embryonated SPF chicken eggs incubated for 9–11 days were inoculated in the allantoic cavity with 0·2 ml swab fluid/egg and candled daily. Dead embryos were stored at 4°C. After 72 hour, the allantoic fluid was harvested from all eggs and a standard hemagglutination assay (HA) with chicken red blood cells was performed, and allantoic fluid was tested with RT‐qPCR. 33 When at least one egg of three eggs was positive in HA, the swab was considered to be positive. Viral load in the different fractions of dust and on the gelatine filters used in the MD8 air scan was determined using RT‐qPCR and confirmed by virus isolation.
Data analysis
Chickens from the recipient group were considered to have been infected with HPAIv H5N1 if they tested positive in RT‐qPCR and subsequently died from infection. In the recipient group, infection was assumed to have been caused by birds from the inoculated group if at least 2 days prior to infection no infectious chickens had been present in the recipient group. The day of infection of the chickens of the recipient group was defined as the first day of virus excretion minus a 1 day latent period. 29
Transmission rate parameters (average number of new infections caused by an infected chicken/day) between chickens in the same group and between chickens in the inoculated group and chickens in the recipient group were estimated using a generalized linear model assuming a stochastic SIR (Susceptible – Infectious – Recovered) transmission process. 34
To determine whether the amount of virus excreted by the inoculated groups was comparable across the four experiments, the amounts of virus detected in the swabs of the chickens of the four inoculated groups were compared using ANOVA. To find the relation between time, amount of virus shed and virus present in the dust or air samples, log‐transformed data of the amount of virus detected in swabs, on the Swiffer dust cloths or on the gelatine filters were analysed using a linear mixed effect model with experiment as random effect and days post‐inoculation as fixed effect. All statistical tests were performed assuming a 2‐sided alternative hypothesis; P values smaller than 0·05 were considered significantly different. Analysis was performed using commercially available statistical software (SPSS 16·0; SPSS Inc., Chicago, IL, USA).
Results
All inoculated and contact birds housed in the inoculated group became infected. The number of birds replaced in the inoculated groups is listed in Table 1. RT‐qPCR detected on average 105·9 EID50/day (95% C.I.: 105·7–106·0 EID50) in the swabs of the inoculated group up to 10 days p.i. No significant differences were detected between the four experiments. No correlation in time was found between the amount of virus shed and the amount of virus detected in the environment. Results from each individual chicken are listed in Table S1.
Transmission from the inoculated to the recipient group occurred in experiments 2 and 4. In experiment 2, one bird from the recipient group tested positive in RT‐qPCR on day 3, and this bird died on the same day before infection was transmitted to cage mates. Next, a second infection in this group was observed on day 6 p.i. This infection initiated a chain of infections ending with infection and death of all birds in this group. In experiment 4, two birds of the recipient group were found positive in RT‐qPCR on day 13 p.i. Finally, all other birds in the group became infected and all birds in the recipient group died before the end of the experiment. In experiments 1 and 3, no transmission from the inoculated to the recipient group was observed.
The transmission rate parameter for the inoculated chickens to the recipient chickens was estimated at 0·08 new infections/infectious chicken/day (95% C.I.: 0·04–0·14). The combined transmission rate parameter for direct transmission in the inoculated group was estimated at 1·71/day (95% C.I.: 0·51–5·75) and in the recipient group at 1·45/day (95% C.I.: 0·38–5·57). The estimated parameters for direct transmission differed significantly from the airborne transmission rate parameter (P < 0·05).
In Swiffer dust samples, RT‐qPCR detected virus from day 2 until day 10 p.i. at a mean level of 104·8 EID50/day/m2 (95% C.I.: 104·6–104·9 EID50) for the inoculated group, and 104·2 EID50/day/m2 (95% C.I.: 104·0–104·4 EID50) for the recipient group (Table 1). The amount of virus detected in Swiffer dust cloths in the inoculated room was significantly higher than in the recipient room. The amount of virus detected in the two rooms was correlated in time (P < 0·05). All positive RT‐qPCR results from the dust cloths from the inoculated room tested positive in virus isolation, but no viable virus was found in any of the dust cloths from the recipient room.
MD8 samples contained on average 103·7 EID50/m3 air (95% C.I. 103·4–103·8 EID50) (Table 1). All positive RT‐qPCR results of the MD8 samples tested positive in virus isolation. No change was detected in the amount of virus detected on MD8 samples during the course of the experiment (P > 0·05).
The non‐respirable and respirable fraction, collected by the Andersen, tested in RT‐qPCR on average 102·8 EID50/m3 air (95% C.I.: 100·5–105·2) and 102·9 EID50/m3 air (95% C.I.: 100·9–105·0), respectively (Table 1). No change was detected in the amount of virus detected in the different fractions during the course of the experiment. On day 2, no viable virus was detected in the RT‐qPCR positive fractions. From day 3 to day 10, all fractions positive in RT‐qPCR tested positive in virus isolation.
Discussion
In this study, we determined the amount of virus shed by infected birds and its relation to environmental deposition of dust‐borne virus and the rate of dust‐borne transmission. Virus strain A/turkey/Turkey/1/2005 H5N1 was transmitted through air, but not all recipient groups became infected after exposure. The rate of indirect transmission associated with dust was 20‐fold lower than the rate of direct transmission between chickens housed in the same cage, suggesting that indirect transmission can occur but is probably less efficient.
The amount of virus detected in air samples collected above the cages in the units with the recipient groups was on average 103·7 EID50/m3. A chicken in this group might have been exposed to 103·8 EID50/day, given that a chicken inhales on average 1·2 m3/day. 13 In a previous study, the median infectious dose for the same virus strain (CID50) was estimated to be 102·5 EID50/chicken after inoculation and falls within the range of 101·2–104·7 CID50 as median infectious doses for other HPAI virus strains, suggesting the model used to assess dust‐borne transmission has an application to other HPAIv. 29 , 35 If this CID50 also applied for infection after indirect exposure of chickens to dust‐contaminated particles, we would expect a higher probability of infection. An explanation for this difference between inoculation dose and ‘natural’ infectious dose could be that the innate immune system may be better capable of clearing a small virus load inhaled over a prolonged period of time than when it is overwhelmed with virus at one time. 36 Another explanation is that the amount of viable virus in the air samples was lower than measured in RT‐qPCR, as the latter also detects inactivated virus particles. We detected viable virus in the air samples, but we did not determine the virus titre, and therefore cannot make a real association between RT‐qPCR results and amount of infectious virus. Nevertheless, our trials can help to interpret results from environmental samples in the field like samples taken from live bird markets or during outbreaks, as it may help to get an indication of the probability of airborne transmission or exposure to infectious virus. 8 , 37 , 38 , 39
We collected dust samples using two methods. With the MD8, we collected air samples for 90 or 270 minutes, in which live virus was detected. Samples from dust that was deposited on the wall of the rooms during 24 hours were collected using dust cloths. Dust samples collected from the wall of the recipient room tested only half‐log lower than dust samples collected in the inoculated room (104·8 and 104·2 EID50/day/m2, respectively). However, none of the positive RT‐qPCR dust samples from the wall of the recipient room tested positive in virus isolation test in contrary to the dust samples of the inoculated room, despite infection of chickens in two of these recipient groups. Transport of dust particles into the environment depends on wind, and deposition of dust particles only occurs under certain conditions. 20 Data from our study suggest that transmission of virus to other flocks during an outbreak may only occur during a short time after being produced. It also implies that during an outbreak, the location and technique of environmental sampling in the surroundings of an infected flock is essential to determine the amount of infectious dust deposited in that environment and the implications of these findings for exposure. For example, during the HPAI H7N7 outbreak in British Columbia in 2004, dust samples were collected from the air around infected flocks, and using high‐volume sampling, virus was retrieved in 3 of 16 samples at an average of 102·5 viral doses/m3. Nevertheless, this information was too sparse to explain the transmission of virus to other flocks as the sampling technique was not optimal.
Our results of dust‐associated virus transmission may also have relevance for human health issues. Personnel working inside stables housing infected flocks may be exposed to large quantities of virus contaminated dust particles. Bos et al. 40 demonstrated that persons involved in inspection and culling of infected poultry during the Dutch H7N7 epidemic had a higher risk for infection. With the results of our study, the level of exposure of humans can be better assessed which may contribute to the optimization of personal protective equipment for personnel working on infected flocks. 41
We also examined the amount of virus attached to particles of different size as smaller dust particles can travel larger distances, and as smaller particles can be deposited more easily in the lower respiratory tract of chickens affecting the probability of infection. 20 , 21 , 23 , 24 Infectious virus was detected on both fractions after 2 days of shedding of virus by the infected birds, but no difference was found between the amount of virus detected in the respirable and non‐respirable fraction. Understanding the biological relevance of these observations requires more research on, for example viral load, particle size and transmission.
The results of this study are a first step to elucidate the importance of the transmission of dust‐borne HPAIv between poultry flocks. Mathematical modelling, using the results described here, can help extrapolating the results from these experimental flocks to the size of commercial flocks to examine whether they can, in part, explain the transmission during epidemics.
Supporting information
Table S1. Overview of the RT‐qPCR results of trachea and cloaca swabs of the four replicate experiments per day p.i. Not available results are ‘na’.
Supporting info item
Acknowledgements
This work was funded by the Dutch Ministry of Economic Affairs (Impulse 422 Veterinary Avian Influenza Research in the Netherlands program). The authors would like to thank J. van den Broek for performing the statistical analysis.
References
- 1. OIE, WAHID interface . HPAI Summary of immediate notifications and follow‐ups, 2011. http://web.oie.int/wahis/public.php?page=disease_immediate_summary?disease_type=Terrestial?disease_id=15 (Accessed 1 November 2011).
- 2. FAO, OIE and WHO . Summary of meeting and key findings of the FAO/OIE/WHO Joint Scientific Consultation on Avian influenza at the human‐animal interface, 2010.
- 3. Capua I, Marangon S. The avian influenza epidemic in Italy, 1999–2000: a review. Avian Pathol 2000; 29:289–294. [DOI] [PubMed] [Google Scholar]
- 4. Stegeman A, Bouma A, Elbers AR et al. Avian influenza A virus (H7N7) epidemic in The Netherlands in 2003: course of the epidemic and effectiveness of control measures. J Infect Dis 2004; 190:2088–2095. [DOI] [PubMed] [Google Scholar]
- 5. Webster RG, Guan Y, Poon L et al. The spread of the H5N1 bird flu epidemic in Asia in 2004. Arch Virol Suppl 2005; 19:117–129. [DOI] [PubMed] [Google Scholar]
- 6. Van der Goot JA, van Boven M, de Jong MCM, Koch G. Effect of vaccination on transmission of HPAI H5N1: the effect of a single vaccination dose on transmission of Highly Pathogenic Avian Influenza H5N1 in Peking ducks. Avian Dis 2007; 51(Suppl 1):323–324. [DOI] [PubMed] [Google Scholar]
- 7. Fiebig L, Smieszek T, Saurina J, Hattendorf J, Zinsstag J. Contacts between poultry farms, their spatial dimension and their relevance for avian influenza preparedness. Geospat Health 2009; 4:79–95. [DOI] [PubMed] [Google Scholar]
- 8. Schofield L, Ho J, Kournikakis B, Booth T. Avian Influenza Sampling Campaign in the British Columbia Fraser Valley, 9–19 April 2004: Sampling of Rare Biological Events. DRDC Suffield TR 2005‐032. Suffield, Canada: Defence R&D, 2005. [Google Scholar]
- 9. Chen P‐S, Tsai FT, Lin CK et al. Ambient influenza and avian influenza virus during dust storm days and background days. Environ Health Perspect 2010; 118:1211–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Takai H, Pedersen S, Johnsen JO et al. Concentrations and emissions of airborne dust in livestock buildings in Northern Europe. J Agric Eng Res 1998; 70:59–77. [Google Scholar]
- 11. Aarnink AJA, Roelofs RFMM, Ellen HH, Gunnink H. Dust Sources in Animal Houses. Proceedings on Dust Control in Animal Production Facilities. Horsens, Denmark, Danish: Institute of Agricultural sciences, 1999. [Google Scholar]
- 12. Olsen KN, Lund M, Skov J, Christensen LS, Hoorfar J. Detection of Campylobacter bacteria in air samples for continuous real‐time monitoring of Campylobacter colonization in broiler flocks. Appl Environ Microbiol 2009; 75:2074–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sedlmaier N, Hoppenheidt K, Krist H, Lehmann S, Lang H, Büttner M. Generation of avian influenza virus (AIV) contaminated fecal fine particulate matter (PM 2.5): genome and infectivity detection and calculation of immission. Vet Microbiol 2009; 2:156–164. [DOI] [PubMed] [Google Scholar]
- 14. Cambra‐López M, Aarnink AJA, Zhao Y, Calvet S, Torres AG. Airborne particulate matter from livestock production systems: a review of an air pollution problem. Environ Pollut 2010; 158:1–17. [DOI] [PubMed] [Google Scholar]
- 15. Anderson DP, Beard CV, Hanson RP. Influence of poultry dust, ammonia, and carbon dioxide on the resistance of chickens to Newcastle disease virus. Avian Dis 1966; 10:177. [PubMed] [Google Scholar]
- 16. Hietala SK, Hullinger PJ, Crossley BM, Kinde H, Ardans AA. Environmental air sampling to detect exotic Newcastle disease virus in two California commercial poultry flocks. J Vet Diagn Invest 2005; 17:198–200. [DOI] [PubMed] [Google Scholar]
- 17. Renz KG, Islam A, Cheetham BF, Walkden‐Brown SW. Absolute quantification using real‐time polymerase chain reaction of Marek’s disease virus serotype 2 in field dust samples, feather tips and spleens. J Virol Methods 2006; 132:127–134. [DOI] [PubMed] [Google Scholar]
- 18. Iwabuchi E, Maruyama N, Hara A et al. Nationwide survey of Salmonella prevalence in environmental dust from layer farms in Japan. J Food Prot 2010; 73:1993–2000. [DOI] [PubMed] [Google Scholar]
- 19. Banhazi TM, Seedorf J. Identification of the risk factors for high airborne particle concentrations in broiler buildings using statistical modeling. Biosyst Eng 2008; 101:100–110. [Google Scholar]
- 20. Shao Y. Physics and Modeling of Wind Erosion. 2nd edition, Chapter 8. Springer science and business media B.V, Dordrecht, The Netherlands, 2008. [Google Scholar]
- 21. Van Riel D, Munster VJ, de Wit E et al. H5N1 virus attachment to lower respiratory tract. Science 2006; 312:399. [DOI] [PubMed] [Google Scholar]
- 22. Tsukamoto K, Imada T, Tanimura N et al. Impact of different husbandry conditions on contact and airborne transmission of H5N1 highly pathogenic avian influenza virus to chickens. Avian Dis 2007; 51:129–132. [DOI] [PubMed] [Google Scholar]
- 23. Kuchipudi SV, Nelli R, White GA, Bain M, Chang KC, Dunham S. Differences in influenza virus receptors in chickens and ducks: implications for interspecies transmission. J Mol Genet Med 2009; 3:143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu Y, Han C, Wang X et al. Influenza A virus receptors in the respiratory and intestinal tracts of pigeons. Avia Pathol 2009; 38:263–266. [DOI] [PubMed] [Google Scholar]
- 25. Yee KS, Carpenter TE, Farver TB, Cardona CJ. An evaluation of transmission routes for low pathogenic avian influenza virus among chickens sold in live bird markets. Virology 2009; 394:19–27. [DOI] [PubMed] [Google Scholar]
- 26. Spekreijse D, Bouma A, Koch G, Stegeman JA. Airborne transmission of a highly pathogenic avian influenza virus strain H5N1 between groups of chickens quantified in an experimental setting. Vet Microbiol 2011; 2:88–95. [DOI] [PubMed] [Google Scholar]
- 27. De Boer GF, Back W, Osterhaus ADME. An ELISA for detection of antibodies against influenza A nucleoprotein in humans and various animal species. Arch Vir 1990; 2:47–61. [DOI] [PubMed] [Google Scholar]
- 28. Londt BZ, Nunez A, Banks J, Nili H, Johnson LK, Alexander D.J. Pathogenesis of highly pathogenic avian influenza A/turkey/Turkey/1/2005 H5N1 in Pekin Ducks (Anas platyrhynchos) infected experimentally. Avian Pathol 2008; 37:619–627. [DOI] [PubMed] [Google Scholar]
- 29. Spekreijse D, Bouma A, Stegeman JA, Koch G, de Jong MCM. The effect of inoculation dose of a highly pathogenic avian influenza virus strain H5N1 on the infectiousness of chickens. Vet Microbiol 2011; 147:59–66. [DOI] [PubMed] [Google Scholar]
- 30. Van der Goot JA, Koch G, de Jong MCM, van Boven M. Quantification of the effect of vaccination on transmission of avian influenza (H7N7) in chickens. PNAS 2005; 102:18141–18146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Andersen AA. New sampler for the collection, sizing, and enumeration of viable airborne particles. J Bacteriol 1958; 76:471–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Van der Goot JA, van Boven M, Stegeman JA, van de Water SGP, de Jong MCM, Koch G. Transmission of highly pathogenic avian influenza H5N1 virus in Pekin ducks is significantly reduced by a genetically distant H5N2 vaccine. Virology 2008; 382:91–97. [DOI] [PubMed] [Google Scholar]
- 33. Office International des Epizooties (OIE) . Manual of Diagnostic Tests and Vaccines for Terrestrial Animals. Chapter 2.3.4. Avian Influenza. 2011. http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/2.03.04_AI.pdf (Accessed 1 November 2011).
- 34. Diekmann O, Heesterbeek JAP. Mathematical Epidemiology of Infectious Diseases. Model Building, Analysis and Interpretation. Chichester, UK: John Wiley & Sons, 2000. [Google Scholar]
- 35. Swayne DE, Slemons RD. Using mean infectious dose of high‐ and low‐pathogenicity avian influenza viruses originating from wild duck and poultry as one measure of infectivity and adaptation to poultry. Avian Dis 2008; 52:455–460. [DOI] [PubMed] [Google Scholar]
- 36. Pujol JM, Eisenberg JE, Haas CN, Koopman JS. The effect of ongoing exposure dynamics in dose response relationships. PLoS Comput Biol 2009; 5:e1000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Indriani R, Samaan G, Gultom A et al. Environmental sampling for avian influenza virus A (H5N1) in live‐bird markets, Indonesia. Emerg Infect Dis 2010; 16:1889–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nguyen DC, Uyeki TM, Jadhao S et al. Isolation and characterization of avian influenza viruses, including highly pathogenic H5N1, from poultry in live bird markets in Hanoi, Vietnam, in 2001. J Virol 2005; 79:4201–4212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Suarez DL, Spackman E, Senne DA. Update on molecular epidemiology of H1, H5, and H7 influenza virus infections in poultry in North America. Avian Dis 2004; 47:888–897. [DOI] [PubMed] [Google Scholar]
- 40. Bos ME, Te Beest DE, van Boven M et al. High probability of avian influenza virus (H7N7) transmission from poultry to humans active in disease control on infected farms. J Infect Dis 2010; 201:1390–1396. [DOI] [PubMed] [Google Scholar]
- 41. Te Beest DE, van Boven M, Bos MEH, Stegeman A, Koopmans MPG. Effectiveness of personal protective equipment and Oseltamivir prophylaxis during Avian Influenza A (H7N7) epidemic, the Netherlands, 2003. Emerg Infect Dis 2010; 16:1562–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Overview of the RT‐qPCR results of trachea and cloaca swabs of the four replicate experiments per day p.i. Not available results are ‘na’.
Supporting info item


