Abstract
Good short term results have led to increased use of synthetic ligaments for acute and chronic acromioclavicular joint (ACJ) disruption. They have proved quite safe in the short term but we present two cases of osteolysis following ACJ reconstruction using a synthetic ligament, reminding surgeons of potential complications with artificial ligaments. A high index of suspicion is needed to diagnose such complications early before irretrievable bone loss to osteolysis.
Keywords: Acromioclavicular joint dislocation, coracoid process, osteolysis, Surgilig
INTRODUCTION
The Nottingham Surgilig™ (Surgicraft, Redditch, UK) was introduced in 2001 as a means of addressing failed acromioclavicular joint (ACJ) surgery [1]. The ligament comprises a braided synthetic polyester ligament with loops on both ends to reconstruct the disrupted coracoclavicular ligaments. The technique involves looping the ligament around the coracoid and securing to the distal clavicle with a screw, thus providing strong fixation. Its use has increased over last 5 years and, although originally intended for failed ACJ reconstructions, it is increasingly being used as primary method of stabilization [2,3] in Rockwood type III–V injuries [4].
Potential complications reported so far include coracoid fracture [1] and skin irritation from the retaining screw, necessitating removal [2]. A recent case report [5] described distal clavicle osteolysis following primary fixation of a Rockwood type III injury using Surgilig. This mode of failure presents challenge for the salvage as a result of the bone loss involved, and can be particularly difficult if it leads to significant erosion of the coracoid process. We report two cases of osteolysis in our practice, one of which involved the coracoid process, following fixation with Surgilig.
CASE REPORTS
Case 1
A 43-year-old right-handed computer consultant was referred for ongoing pain following reconstruction of the left AC joint using Surgilig in November 2009. The original indication for surgery was a grade IV ACJ dislocation following a motorbike accident that was repaired acutely. He had symptomatic relief for 1 year after surgery; however, he then developed recurrent pain, including discomfort at rest. Functional pain was experienced during overhead and cross-arm movements. He also complained of difficulty in lying on the shoulder, leading to sleep disturbance.
Examination revealed a well-healed surgical scar with tenderness of the ACJ and positive cross-arm adduction test but no significant instability. However, there was also significant tenderness around the coracoid process. His Oxford shoulder score [6] (new system) on presentation was 26.
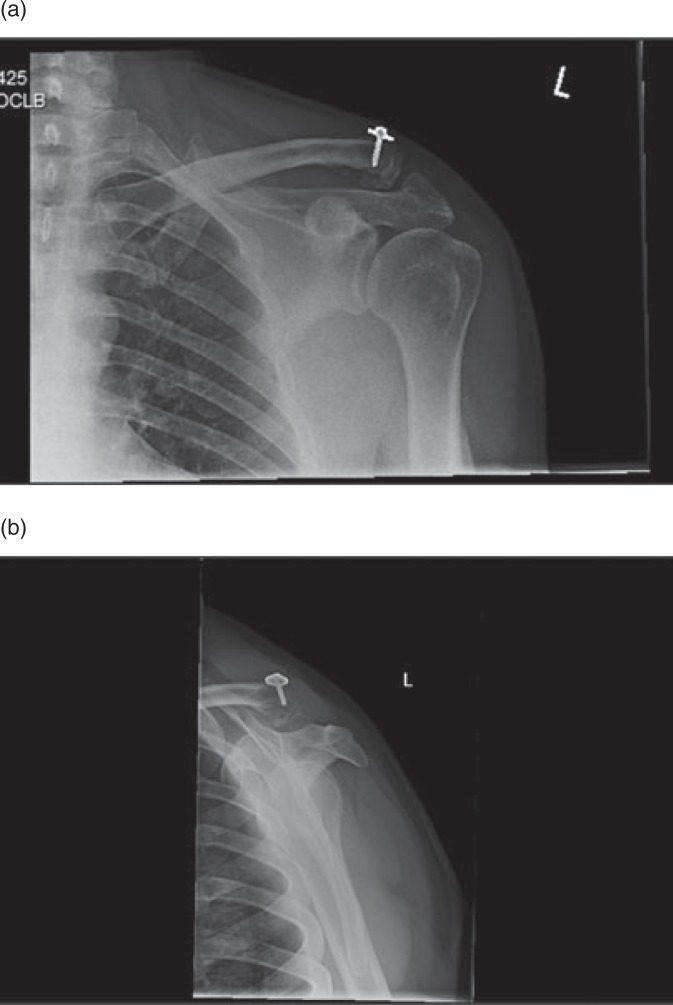
An X-ray (Fig. 1a,b) and computed tomographic scan (Fig. 2) revealed degenerative changes around the AC joint along with scalloping and erosion of the base of coracoid and lateral clavicle. An ultrasound-guided triamcinolone injection to the AC joint was performed to assess whether symptoms were originating from the clavicle/ACJ or the coracoid process. The injection had no effect, which suggested that the pathology around coracoid process was contributing to the pain. A revision procedure was therefore proposed.
Fig. 1.
Case 1: X-ray on presentation.
Fig. 2.
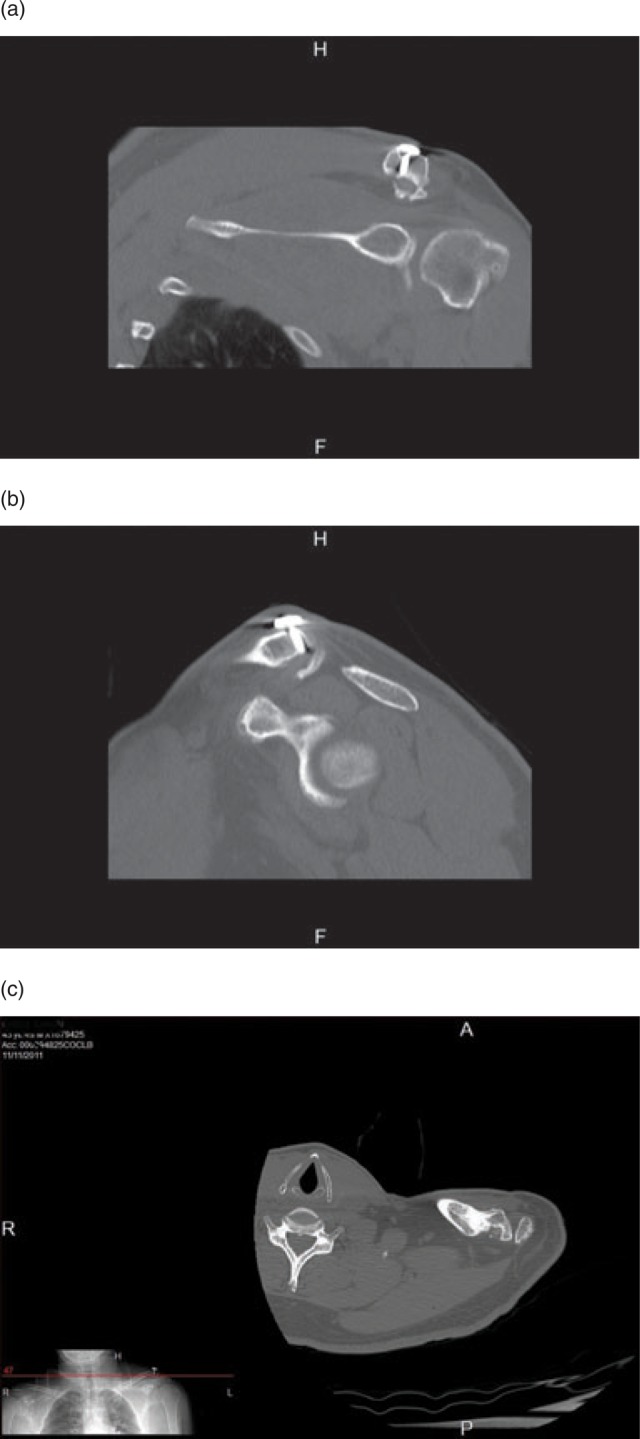
(a) Case 1: Preoperative computed tomography (CT) scan showing clavicle osteolysis. (b) Case 1: Preoperative CT scan showing osteolysis of coracoid process. (c) Axial cut CT scan showing clavicle osteolysis.
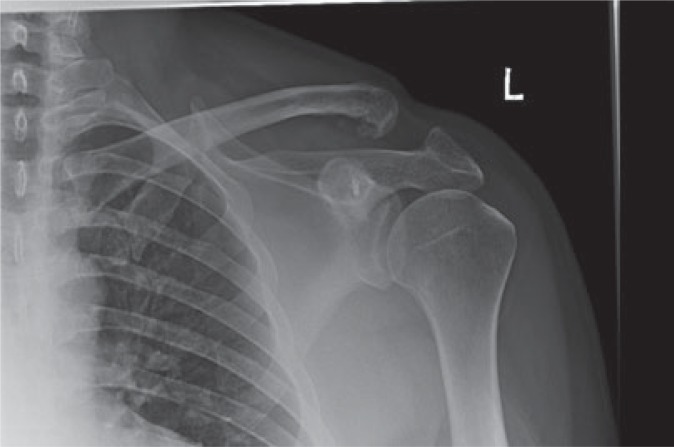
In January 2012, a revision surgery was performed. The clavicle was found to be unstable in anterior–posterior direction but stable in the superior–inferior plane. There was marked erosion of the coracoid, particularly superiorly, causing a groove of approximately 30% to 40% of coracoid thickness. Erosion of the superior clavicle was also noted beneath the Surgilig. The Surgilig was removed and tissue was sent for extended culture, which did not grow any organism. A Weaver–Dunn procedure was performed and reinforced with suture anchor into the base of coracoid. The patient was immobilized in a sling for 4 weeks and had regained a full range of movement by 10 weeks post-operatively. There was no residual AC joint instability and he resumed sporting activities after 3 months. Radiographs at 6 months showed a well reduced joint and a satisfactory coraco–clavicular distance (Fig. 3). More importantly, he had complete resolution of his pain. His Oxford score at discharge was 48.
Fig. 3.
Case 1: Post-operative radiograph.
Case 2
A 24-year-old right-handed investment banker presented with painful left shoulder in November 2010. He had sustained a grade III ACJ dislocation in June 2007 and underwent delayed stabilization using Surgilig in February 2008. He made a good recovery but reported that the shoulder never regained full strength. However, approximately 18 months later, he developed positional pain radiating down the arm. Initially, there was no recurrent rest pain, although he did have difficulty lying on the shoulder with sleep disturbance.
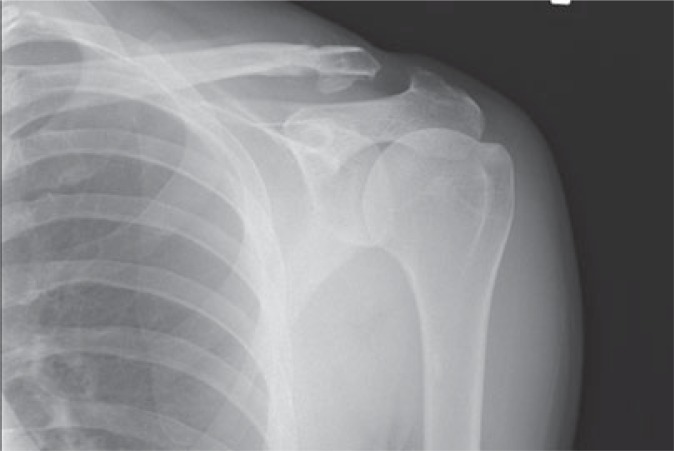
Examination revealed a well-healed scar with a stable and congruent AC joint. Range of movement was full and pain free, impingement tests were mildly positive, and rotator cuff had normal strength. His Oxford score at the time of presentation was 34. An X-ray of the shoulder confirmed erosion of superior border of clavicle (Fig. 4) where Surgilig appeared to be eroding through the cortex. Surgery was therefore planned to pre-empt the development of a fracture through a possible stress riser.
Fig. 4.
Case 2: X-ray on presentation.
Surgical exploration in January 2011 revealed a 5-mm groove into clavicle as a result of erosion by Surgilig. The ACJ itself remained stable after removing the Surgilig along with the screw, and the lateral end of clavicle was resected by another 5 mm. Tissue samples and the excised ligament were sent for extended culture microbiology, although no growth was obtained.
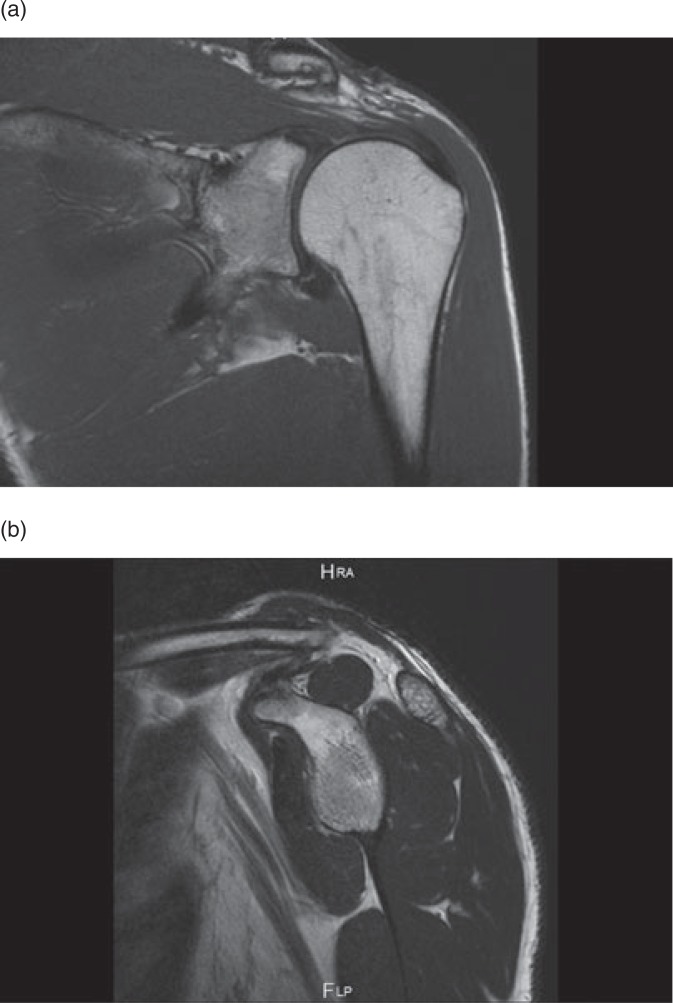
At 3 months post-operatively, he had regained a full range of movement and his symptoms had improved. He reported some persistent discomfort despite a stable AC joint but no progressive scalloping of coracoid process or clavicle was seen on on the X-rays (Fig. 5) and MRI scan (Fig. 6a,b). The symptoms then continued to improve with physiotherapy and, at 6 months, he was discharged with an Oxford score of 46.
Fig. 5.
Case 2: Post-operatively.
Fig. 6.
Case 2: Post-operatively. Magnetic resonance imaging.
DISCUSSION
Although management of Rockwood type III AC joint dislocation still remains controversial, there is general consensus about the need for conservative management of grades I and II and surgery for type IV to VI [4]. Our preference, similar to most other units, is to treat grade III injuries conservatively in the acute phase. If patients complain of persistent instability, manifested by pain and clicking during cross-arm adduction, they are offered stabilization using Surgilig. We have extensive experience in the use of Surgilig and have previously reported excellent mid-term results in both acute and chronic settings [2].
The primary aim of any surgery for ACJ disruption is to restore the joint alignment. The alignment can be maintained using a variety of techniques; a detailed discussion on various fixation techniques is beyond the scope of the present case report. Coracoclavicular ligament reconstruction using artificial ligaments has gained popularity as a result of a ready availability, the predictable strength of the implant, and restoration of the normal coracoclavicular distance.
Previously, synthetic materials such as Dacron graft (DuPont, Wilmington, DE, USA) used in anterior cruciate ligament reconstruction have been reported to cause as much as 85% periligamentous femoral osteolysis as a result of a suspected sterile reaction [7]. Fullerton et al. reported the failure of Dacron grafts in ACJ stabilization long ago [8]. Various other suture materials, including PDS (Ethicon Inc., Somerville, NJ, USA) [9], Merselene (Ethicon Inc.) [10] and carbon fibres [11], have been used to stabilize the ACJ, although they suffer from an increased risk of bone erosion and subsequent failure as a result of a small contact surface area with the bone and resulting high stress. There have also been reports of foreign body reactions using other materials, such as PDS (Ethicon Inc.) [12] and Gore Tex graft (Gore, Flagstaff, AZ, USA) [13].
Surgilig is a specially designed sling to replace the coracoclavicular ligament and is reported to be biologically inert. It is designed to loop around the coracoid (similar to a luggage tag technique) and fixed to clavicle under optimal tension using screw and washer. The fixation is durable and secure, and has been shown to provide good stability and function in the medium term [1,2].
Surgilig was considered to be at a lower risk of cutting through the bone because the ligament itself is quite broad, thereby evenly distributing the stress over a larger surface area. However, the surgical technique demands a tight loop around the coracoid to afford stability, and one hypothesis is that this can cause strangulation of the blood supply of coracoid. A relatively avascular bone with poor healing potential will then be more prone to erosion. On the other hand, if the loop is put in too loose, it abrades the bone as a result of increased micromotion, which in turn can lead to osteolysis. There has been a similar case reported recently that was attributed to a sterile foreign body reaction to the synthetic ligament being the cause of osteolysis [5]. Although these can all be valid hypotheses, the exact cause of such osteolysis remains unclear.
Our cases highlight a potential complication following the use of artificial ligaments for ACJ reconstruction. Persistent or recurrent pain after surgery should be investigated appropriately to rule out potential coracoid or clavicle erosion. In our experience, natural fibrosis enmeshed in the ligament stabilizes the joint over time, and it may be possible to remove the ligament without any further procedure. If there is residual instability, another stabilization procedure, such as the Weaver–Dunn procedure [14], can be performed. However, significant erosion of coracoid with persistent instability presents a more challenging problem because the coraco-acromial ligament is not always available in a revision situation. Clearly, substituting an artificial ligament for another is not feasible; the best chance of salvage thus lies in the early detection of bony erosion. We hope to raise awareness about this possible complication so that early management can be instituted before the bone loss becomes irretrievable.
Footnotes
Conflicts of Interest The authors declare no conflict of interests
References
- 1. Jeon IH. et al. Chronic acromioclavicular separation: the medium term results of coracoclavicular ligament reconstruction using braided polyester prosthetic ligament. Injury 2007; 38: 1247–53. [DOI] [PubMed] [Google Scholar]
- 2. Carlos AJ, Richards AM, Corbett SA. Stabilization of acromioclavicular joint dislocation using the ‘Surgilig’ technique. Shoulder Elbow 2011; 3: 166–70. [Google Scholar]
- 3. Bhattacharya R, Goodchild L, Rangan A. Acromioclavicular joint reconstruction using the Nottingham Surgilig: a preliminary report. Acta Orthop Belg 2008; 74: 167–72. [PubMed] [Google Scholar]
- 4. Galatz LM, Hollis RF, Jr, Williams GR., Jr Acromioclavicular joint injuries. In: Bucholz RW, Heckman JD, Court-Brown CM, eds. Rockwood & Green's fractures in adults. 6th edition. Philadelphia: Lippincott Williams & Wilkins, 2006:3647–749.
- 5. Dearden PM, Ferran NA, Morris EW. Distal clavicle osteolysis following fixation with a synthetic ligament. Int J Shoulder Surg 2011; 5: 101–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dawson J, Rogers K, Fitzpatrick R, et al. The Oxford shoulder score revisited. Arch Orthop Trauma Surg 2009; 129: 119–23. [DOI] [PubMed] [Google Scholar]
- 7. Bartolozzi P, Salvi M, Velluti C. Long-term follow-up of 53 cases of chronic lesion of the anterior cruciate ligament treated with an artificial Dacron Stryker ligament. Ital J Orthop Traumatol 1990; 16: 467–80. [PubMed] [Google Scholar]
- 8. Fullerton LR., Jr Recurrent third degree acromioclavicular joint separation after failure of a Dacron ligament prosthesis. A case report. Am J Sports Med 1990; 18: 106–7. [DOI] [PubMed] [Google Scholar]
- 9. Motamadi AR, Blevins FT, Willis MC, et al. Biomechanics of the coracoclavicular ligament complex and augmentations used in its repair and reconstruction. Am J Sports Med 2000; 28: 380–4. [DOI] [PubMed] [Google Scholar]
- 10. Pearsall AW, Hollis JM, Russel GV, Jr, et al. Biomechanical comparison of reconstruction techniques for disruption of the acromioclavicular and coracoclavicular ligaments. J South Orthop Assoc 2002; 11: 11–17. [PubMed] [Google Scholar]
- 11. Burri C, Neugebauer R. Carbon fiber replacement of the ligaments of the shoulder girdle and the treatment of lateral instability of the ankle joint. Clin Orthop Relat Res 1985; 196: 112–17. [PubMed] [Google Scholar]
- 12. Boldin C, Fankhauser F, Ratschek M, et al. Foreign-body reaction after reconstruction of complete acromioclavicular dislocation using PDS augmentation. J Shoulder Elbow Surg 2004; 13: 99–100. [DOI] [PubMed] [Google Scholar]
- 13. Stewart AM, Ahmad CS. Failure of acromioclavicular reconstruction using Gore-Tex graft due to aseptic foreign-body reaction and clavicle osteolysis: a case report. J Shoulder Elbow Surg 2004; 13: 558–61. [DOI] [PubMed] [Google Scholar]
- 14. Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am 1972; 54: 1187–94. [PubMed] [Google Scholar]