Abstract
Background
The present study assessed results of arthroscopy-assisted TightRope (Arthrex, Naples, FL, USA) repair of acute Rockwood grade III and V acromioclavicular (AC) dislocations.
Methods
We retrospectively reviewed the medical records of 57 patients with AC dislocations treated with TightRope fixation: 15 Rockwood grade III and 42 grade V. Functional results were assessed using the Constant score, and Disabilities of Arm, Shoulder and Hand (DASH) and RAND 36-ltem Health Survey scores after a mean 2.6 years of follow-up (range 1.0 years to 4.5 years). Radiographic results were assessed using the AC joint coracoclavicular (CC) distance.
Results
Postoperative radiographs showed anatomical AC joint reduction in all patients. In nine patients, fixation failed before 6 weeks postoperatively, mainly as a result of suture breakage. For the remaining 47 patients, CC distance was well maintained at 6 weeks. At follow-up, mean (SD) CC distance was significantly increased compared to the contralateral side or postoperative radiographs [17 (4) mm versus 10 (3) mm]. Mean DASH score was 9, Constant score was 88 and the RAND 36 score showed a quality of life similar to the Finnish reference population.
Conclusions
Despite initial good reduction of grade III and V AC dislocations using TightRope fixation, subluxation often recurs after 6 weeks. Patients suffer minor subjective complaints that do not worsen the quality of life.
Keywords: Acromioclavicular dislocation, arthroscopic surgery, treatment outcome
INTRODUCTION
Most acromioclavicular (AC) joint injuries can be successfully treated non-operatively; however, surgery is usually needed to treat more severe, Rockwood grade IV–VI dislocations [1]. The use of surgery to treat Rockwood grade III dislocations is controversial, although several studies recommend operative treatment of these injuries in heavy manual labourers [1,2].
The principle behind most operative techniques for acute AC dislocation treatment is to reduce and temporarily fix the joint in place to allow healing of torn ligaments [1]. The metallic fixation materials often loosen and will usually impair shoulder joint function [3]; therefore, pins, screws or plates must be removed 6 weeks to 12 weeks after surgery, which occasionally leads to recurrence of dislocation or subluxation [2]. New strong suture materials have enabled the use of coracoclavicular fixation without having to remove the fixation device, which may give ligaments more time to heal. Some studies have suggested that sutures may be used to permanently replace coracoclavicular ligaments [4].
There are several options for repairing AC dislocations with sutures or suture anchors [4–8]. Usually, suture anchors have #2 sutures, although flip button anchors can use heavier suture materials (#5). Arthroscopy-assisted techniques help to accurately position coracoid flip button fixation under the coracoid base. Few studies have reported the results of arthroscopic flip button repairs of AC dislocations; these studies have only included small numbers of patients and the results have been controversial [4,9–14].
The present study aimed to assess the radiological and functional results of using arthroscopy-assisted coracoclavicular flip button device (TightRope) repair for Rockwood grade III and V AC dislocations.
MATERIALS AND METHODS
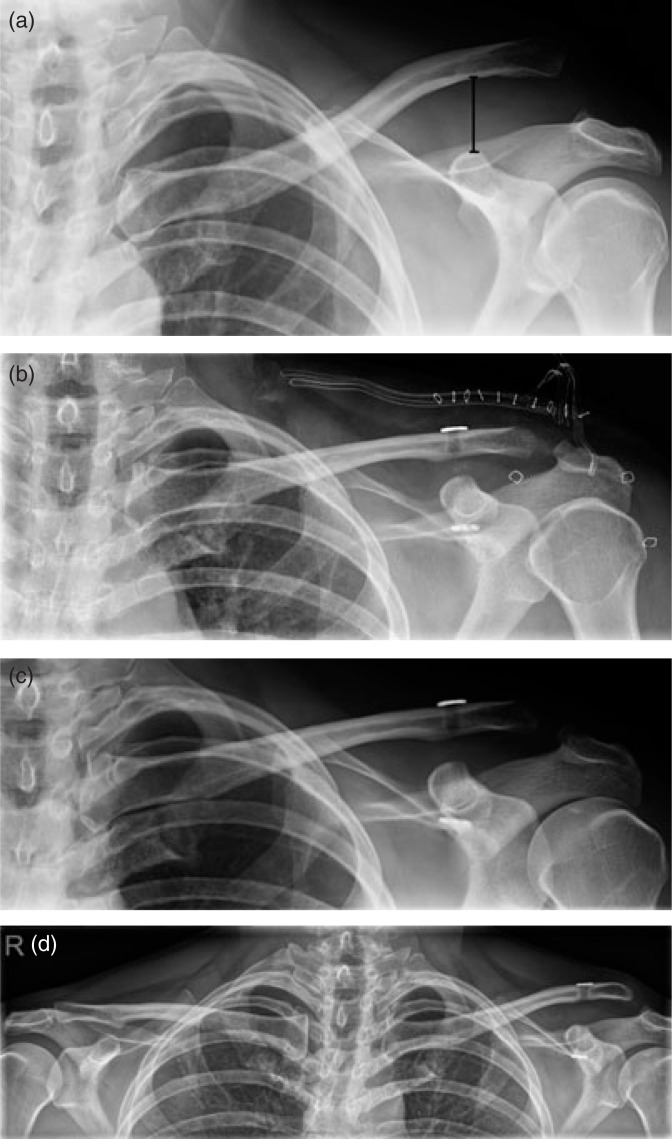
Between 2007 and 2011, 57 patients [six female, 51 male; mean (range) age 40 years (16 years to 74 years)] with an acute (< 2 weeks) AC dislocation were operated on using arthroscopy-assisted coracoclavicular flip button repair in Oulu University Hospital. Our hospital's administration approved the review of medical records and re-examination of the patients at our outpatient clinic. Rockwood classifications were determined using radiographs; 15 patients had grade III dislocation (clavicle displaced up to a bone width in reference to the acromion) and 42 patients had grade V dislocation (displacement more than a bone width) (Fig. 1A) [1]. Indications for surgery to treat grade III dislocations were participation in heavy manual labour or sports activities demanding heavy lifting.
Fig. 1.
(a) Rockwood grade V acromioclavicular (AC) dislocation of a 45-year-old male; coracoclavicular (CC) distance: 27 mm. (b) Postoperative radiograph after TightRope repair; a small (5 mm) resection of distal clavicle as a result of osteoarthritis; CC distance: 8 mm. (c) Follow-up visit at 6 weeks; CC distance: 9 mm. (d) Radiograph of both clavicles after 2 years; subluxation of left AC joint; CC distance: 16 mm; contralateral side: 8 mm; Disabilities of Arm, Shoulder and Hand score: 0; Constant score: 96.
The mechanisms of injury were reported as: bicycle accident (n = 20), sports-related injury (n = 15), falling from standing height (n = 7), motor vehicle accident (n = 7), falling from a height (n = 4), violence (n = 3) and unknown (n = 1).
Operative technique
All operations were carried out with the patient in beach chair position. After diagnostic arthroscopy from a standard posterior portal, a mid-glenoid portal and anterolateral portal were established. The arthroscope was switched to the anterolateral portal, and the coracoid base was identified by following the subscapular tendon. If necessary, the middle glenohumeral ligament was divided and debrided for better visualization. The coracoid base was cleaned from soft tissues using a radiofrequency electrode. A small (4 cm to 5 cm) incision was made across the AC joint to expose the distal clavicle. If osteoarthritic changes were seen in the distal clavicle, a small (5 mm to 8 mm) resection was performed and the sharp edge of the clavicle was rounded. The joint was reduced and temporarily fixed with a Kirschner wire (K-wire) crossing the AC joint. A guide was positioned under the coracoid, and a guidewire was drilled though the clavicle and base of the coracoid under arthroscopic vision. A 4.5-mm hole was drilled over the guidewire through the clavicle and coracoid. A TightRope anchor (Arthrex, Naples, FL, USA) was pulled under the coracoid using a Nitinol wire loop (Arthrex). The suture was tied over another button on the clavicle, the K-wire was removed, the deltotrapezius fascia was closed with nonresorbable sutures and the wound was closed.
The upper arm was immobilized with a sling for 4 weeks, at which time physiotherapist-guided gentle range-of-motion (ROM) exercises were started. Patients visited an outpatient clinic at 6 weeks postoperatively and, if ROM was restored, the patients were allowed to start strengthening exercises. Manual labour was gradually allowed at 2 months after the surgery.
Outcome measures
One patient was lost to follow-up before the 6-week outpatient clinic visit; therefore, only 56 patients’ medical records and radiographs were available for 6 weeks postoperatively. Patients were sent Disabilities of Arm, Shoulder and Hand (DASH) questionnaires [15] to assess function and symptoms of upper arm, as well as RAND 36-Item Health Survey questionnaires [16] to evaluate quality of life. Fifty-two patients returned these questionnaires. Forty-one patients were examined at the outpatient clinic; an independent examiner (E.I.) performed the Constant scoring [17], and radiographs were obtained of both clavicles and AC joints. The mean (range) follow-up was 2.6 years (1.0 years to 4.5 years). Twelve patients who could not visit the outpatient clinic were contacted by telephone, and six of them had radiographs at their primary health care centre. One patient was unwilling to participate in the study. Four patients were lost to follow-up; they did not respond to repeated letters, could not be contacted by telephone and had not contacted our hospital regarding their shoulder injury after the 6-week control visit, and no reoperations had been carried out at our institute.
RAND 36 scores were compared to age- (5-year intervals) and sex-specific reference values from the Finnish population [16]. The DASH score in the normal population was considered as 10 [18]. Patients were also asked to evaluate their symptoms, work ability and recreation activities, as well as satisfaction with their shoulder.
Radiographic measurements
The reduction of the AC joint was assessed using the coracoclavicular (CC) distance. The upper border of the coracoid process and undersurface of the clavicle were used as reference points, and the distance was measured (mm) (Fig. 1A). Anteroposterior radiographs were taken after injury, after operation and at 6 weeks, and were used to measure changes in CC distance. Postoperative reduction of the joint was confirmed using also axillary lateral and Y-projection of the shoulder joint (AC-joint congruent). At a later follow-up visit, radiographs of both clavicles and AC-joints (central beam at midline) were obtained to compare the CC distance of injured and uninjured sides. Digital imaging was used and the measurements were performed using NeaView software (Neagen Inc., Oulu, Finland).
Statistical analysis
Summary data are presented as the mean (SD) unless otherwise stated. A t-test or analysis of variance was used to compare means of continuous variables. Spearman's correlation was used to test any correlation between variables. p < 0.05 was considered statistically significant. IBM SPSS Statistics, version 20 (IBM Corp., Armonk, NY, USA) was used to perform the calculations.
RESULTS
Radiographic results
Mean (SD) CC distance after injury was 22 (5) mm. Postoperative radiographs showed that the AC joint position was good (Fig. 1B) in all patients [CC distance, 11 (3) mm versus control side distance, 10 (2) mm; p = 0.5]. Early (< 6 weeks) failure of the fixation [CC distance, 19 (5) mm] was noted in nine (16%) patients. This was a result of technical error in two patients; the coracoid bone tunnel was drilled too laterally and the button had cut out. In seven patients, the reason for failure was considered to be breakage of the suture because the buttons were in their original position despite recurred subluxation.
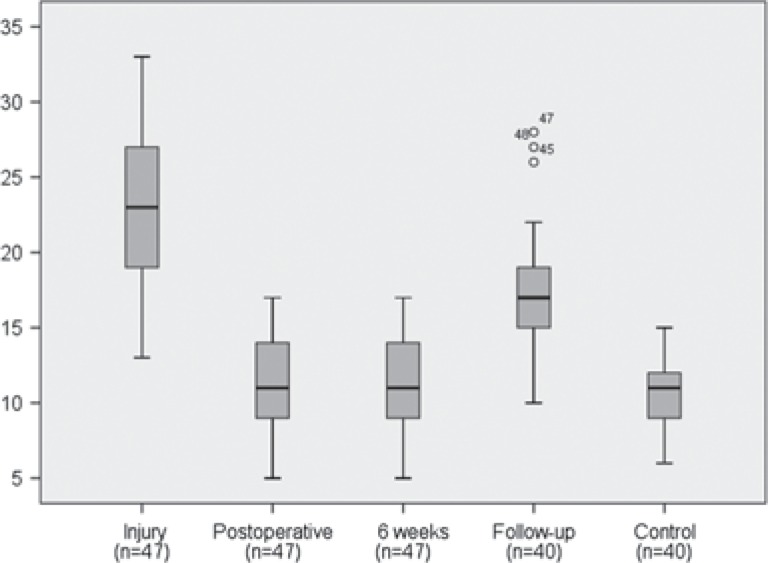
In 47 patients, the reduction was well maintained (Fig. 1C) at the 6-week outpatient visit [CC distance, 11 (3) mm]. At the follow-up visit, CC distance was significantly increased (Fig. 2) compared to postoperative and to the control side [CC distance, 17 (4) mm; p = 0.001]. At follow-up, CC difference was 0 mm to 5 mm in 16 patients, 6 mm to 10 mm in 25 patients and > 10 mm in six patients. The 16 patients with ≤ 5 mm CC difference had primarily a grade V injury in 13 cases and a grade III dislocation in three cases. The reasons for late failure were migration of the clavicle-side button into bone in four patients, as well as suture breakage and insufficient healing or stretching of coracoclavicular ligaments in others (Fig. 1D).
Fig. 2.
Boxplot diagram of coracoclavicular distance (mm) of 47 patients whose fixation was maintained at the 6-week outpatient visit.
Functional results
The mean (SD) DASH score was 9 (9) (control 10; p = 0.3) [12]. The Constant score was lower for the injured side compared to the uninjured side [88 (10) versus 92 (6); p = 0.002]. RAND 36 scores were not significantly different from those in the control population (Table 1). Rockwood grade, the amount of primary dislocation or final radiological outcome assessed as CC distance, did not correlate with the DASH, Constant or RAND 36 scores.
Table 1.
RAND 36-Item Health Survey scores of 52 patients and means of age- and sex-matched references from the Finnish reference population of Aalto et al. [16]
| Measured, mean (SD) | Reference, mean | p * | |
|---|---|---|---|
| General health | 71 (18) | 65 | 0.02 |
| Physical functioning | 91 (31) | 88 | 0.09 |
| Mental health | 81 (17) | 73 | 0.01 |
| Social functioning | 88 (19) | 82 | 0 03 |
| Vitality | 74 (19) | 65 | <0.01 |
| Bodily pain | 77 (20) | 77 | 0 99 |
| Role functioning/physical | 85 (14) | 78 | 0 13 |
| Role functioning/emotional | 86 (33) | 77 | 0 05 |
Student's t-tests.
Forty-one patients returned to their previous occupation, four patients had to change their line of work, two patients had changed occupation as a result of shoulder problems and five patients were already retired at the time of the injury. Thirty-eight patients returned to their previous level of recreational activities, 14 patients had to change their activities because of their shoulder. Twenty-six patients regarded their result as good or excellent, 15 as satisfactory, six as poor and five patients could not answer. The most common complaints were pain [mean (SD) visual analogue scale of 13 (2) in Constant score] and cosmetic problems (eight patients).
Seven patients had reoperations, including three new stabilization operations, three AC resections as a result of painful osteoarthritis and one manipulation under anesthesia as a result of postoperative frozen shoulder.
DISCUSSION
Early failure of TightRope fixation was common; the reduction also sometimes failed gradually after 6 weeks. Shoulder function returned to a good level, although patients experienced some subjective symptoms in the upper extremity; these symptoms did not worsen quality of life compared to a reference population.
Earlier studies of TightRope fixation of AC dislocations have involved only small numbers of patients and the results have been controversial. Thiel et al. and Defoort and Verborgt studied 12 and 15 patients, respectively, and each reported fixation failure in one-third of the patients with grade III and VAC dislocations [9,11]. By contrast, El Sallakh studied 10 patients and reported only one failure of fixation, which was the result of a technical error [12]. Our fixation failure rate was 16%. Scheibel et al. and Salzmann et al. studied 27 and 23 patients, respectively, who received double TightRope fixation that was intended to fix and replace both conoid and trapezoid parts of coracoacromial ligament [4,10]; early failures were rare but they reported slight losses of reduction at up to 6 months postoperatively, which did not affect clinical results. Patzer et al. compared single and double TightRope fixation and found that early failures were more frequent when a single implant was used but late loss of reduction was similar in both groups [13]. Functional results have been good in all previous studies.
Biomechanical studies have shown that Tightrope anchors are stronger than native coracoacromial ligaments [19]. However, they appear to fail easily in cyclic loading because suture breakage was the main reason for both early and late failures. In clinical practice, healing ligaments are usually allowed to carry some load after 6 weeks to 12 weeks [20]. However, animal studies have shown that, under load, healing knee medial collateral ligaments creep and elongate permanently [21]. It is also possible that they do not achieve the mechanical strength of intact ligaments even at 1 year postoperatively [20,21]. Our results suggest that this may be the case in AC dislocation. Some studies have proposed that torn CC ligaments should be replaced with tendon grafts even in acute injuries because tendon grafts stretch less than healing ligaments [20,22].
Although our radiological results did not correlate with any of the functional outcome measures, this must be interpreted with caution. The displacement at follow-up was approximately half of that seen on radiographs after injury (Fig. 2). Surgery can reduce the severity of an injury, especially in grade V dislocations, and it is probably important to fix the anatomy within certain limits. All of the heavy manual labourers who received surgery for grade III injuries could eventually return to their previous occupation.
Functional results were assessed using valid and widely used outcome instruments, which showed good shoulder and upper extremity function. However, patients reported minor impairments, especially pain of the shoulder and upper arm, which were not revealed by the DASH and RAND 36 scores. These scores may underestimate real impairments as a result of AC joint problems. There are scores designed to specifically assess impairments in the AC joint, including the Taft score, Imatani score, Walsh score and Acromioclavicular Joint Instability score [10,23–25]. We did not use those scores because they have not been validated and their responsiveness to clinical change has not been studied.
The present study has several weaknesses. The design was retrospective and not all patients underwent clinical examination at follow-up. Radiological measurements were performed using routine radiographs and are subject to error, although CC distance is regarded as the most accurate measurement and is most commonly used in studies. The definitions of grade III and Grade V AC dislocation are somewhat ambiguous and there may be some overlap between these injuries. The inter-observer reliability of the Rockwood classification from radiographs has been shown to be only satisfactory, although the intra-observer reliability is good [26].
Our results support the finding of Motta et al. [27] indicating that the #5 suture of the TightRope implant is too weak. In newer implants, the buttons and suture of the implant both have been replaced by stronger ones, which probably helps to prevent early fixation failures. This may lead to better healing of the ligaments; however, it may also lead to increased bony complications, as seen with artificial ligaments in open AC reconstructions [28,29].
In conclusion, initial good reduction of arthroscopy-assisted TightRope repair of grade III and V AC dislocations is often lost and subluxation frequently recurs. However, the severity of the injury can be lowered and the functional results are good. Early failures are too common, and newer implants with stronger suture material are probably better options than a TightRope anchor. Patients should be advised that the displacement often partially recurs even after 6 weeks.
Preliminary results of the present study were presented at the annual meeting of the Finnish Orthopedic Association (22 November 2012, Helsinki); Abstract book [in Finnish].
Footnotes
Conflicts of Interest The authors declare no conflict of interests
References
- 1. Collins DN. Disorders of the acromioclaviculer joint. In: Rockwood CA, Matsen FA, III, Wirth MA, Lippitt SB, eds. The shoulder, 4th edn. Philadelphia, PA, Saunders; 2009:453–526. [Google Scholar]
- 2. Johansen JA, Grutter PW, McFarland EG, Petersen SA. Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg 2011; 20: S70–82. [DOI] [PubMed] [Google Scholar]
- 3. Lyons FA, Rockwood CA., Jr Migration of pins used in operations on the shoulder. Traumatic anatomy and the importance of the deltoid and the trapezius. J Bone Joint Surg Am 1990; 72-A: 1262–7. [PubMed] [Google Scholar]
- 4. Salzmann GM, Walz L, Buchmann S, Glabgly P, Venjakob A, Imhoff AB. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med 2010; 38: 1179–87. [DOI] [PubMed] [Google Scholar]
- 5. Wolf EM, Pennigton WT. Arthroscopic reconstruction for acromioclavicular joint dislocation. Arthroscopy 2001; 17: 558–63. [DOI] [PubMed] [Google Scholar]
- 6. Chernchujit B, Tischer T, Imhoff AB. Arthroscopic reconstruction of acromioclavicular joint disruption: surgical technique and preliminary results. Arch Orthop Trauma Surg 2006; 126: 575–81. [DOI] [PubMed] [Google Scholar]
- 7. Choi SW, Lee TJ, Moon KH, Cho KJ, Lee SY. Minimally invasive coracoclavicular stabilization with suture anchors for acute acromioclavicular dislocation. Am J Sports Med 2008; 36: 961–5. [DOI] [PubMed] [Google Scholar]
- 8. Shin S-J, Yun Y-H, Yoo JD. Coracoclavicular ligament reconstruction for acromioclavicular dislocation using 2 suture anchors and coracoacromial ligament transfer. Am J Sports Med 2009; 37: 346–51. [DOI] [PubMed] [Google Scholar]
- 9. Defoort S, Verborgt O. Functional and radiological outcome after arthroscopic and open acromioclavicular stabilization using a doublebutton fixation system. Acta Orthop Belg 2010; 76: 585–91. [PubMed] [Google Scholar]
- 10. Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 2011; 39: 1507–16. [DOI] [PubMed] [Google Scholar]
- 11. Thiel E, Mutnal A, Gilot GJ. Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the TightRope device. Orthopedics 2011; 34: e267–74. [DOI] [PubMed] [Google Scholar]
- 12. El Sallakh SA. Evaluation of arthroscopic stabilization of acute acromioclavicular joint dislocation using the TightRope system. Orthopedics 2012; 35: e18–22. [DOI] [PubMed] [Google Scholar]
- 13. Patzer T, Clauss C, Kühne CA, et al. Die arthroscopisch unterstützte Stabilisierung derakuten AC-Gelenksprengung. Vergleich der klinischen und radiologischen Ergebnisse der Single- vs. Double-TightRope-Technik. Unfallchirurg DOI:10.1007/s00113-011-2135-2. [DOI] [PubMed]
- 14. Murena L, Vulcano E, Ratti C, Cecconello L, Rolla PR, Surace MF. Arthroscopic treatment of acute acromioclavicular joint dislocation with double flip button. Knee Surg Sports Traumatol Arthrosc 2009; 17: 1511–15. [DOI] [PubMed] [Google Scholar]
- 15. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996; 29: 602–8. [DOI] [PubMed] [Google Scholar]
- 16. Aalto AM, Aro AR, Teperi J. RAND-36 as a measure of health-related quality of life: reliability, construct validity and reference values in the Finnish general population. Research Reports 101. Helsinki: Stakes, 1999. (in Finnish with English summary). [Google Scholar]
- 17. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop 1987; 214: 160–4. [PubMed] [Google Scholar]
- 18. Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American academy of orthopaedic surgeons outcomes instruments – normative values from the general population. J Bone Joint Surg 2002; 84-A: 208–15. [DOI] [PubMed] [Google Scholar]
- 19. Walz L, Salzmann GM, Fabbro T, Eichhorn S, Imhoff AB. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med 2008; 36: 2398–406. [DOI] [PubMed] [Google Scholar]
- 20. Woo S L-Y, Abramowitch SD, Kilger R, Liang R. Biomechanics of knee ligaments: injury, healing, and repair. J Biomech 2006; 39: 1–20. [DOI] [PubMed] [Google Scholar]
- 21. Thornton GM, Leask GP, Shrive NG, Frank CB. Early medial collateral ligament scars have inferior creep behavior. J Orthop Res 2000; 18: 238–46. [DOI] [PubMed] [Google Scholar]
- 22. Ranne JO, Sarimo JJ, Rawlins MI, Heinonen OJ, Orava SY. All-arthroscopic double-bundle coracoclavicular ligament reconstruction using autogenous semitendinosus graft: a new technique. Arthrosc Tech 2012; 1: e11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Imatani RJ, Hanlon JJ, Cady GW. Acute, complete acromioclavicular separation. J Bone Joint Surg 1975; 57-A: 328–32. [PubMed] [Google Scholar]
- 24. Walsh WM, Peterson DA, Shelton G, Neumann RD. Shoulder strength following acromioclavicular injury. Am J Sports Med 1985; 13: 153–8. [DOI] [PubMed] [Google Scholar]
- 25. Taft TN, Wilson FC, Oglesby JW, Hill CH. Dislocation of the acromioclavicular joint. J Bone Joint Surg 1987; 69-A: 1045–51. [PubMed] [Google Scholar]
- 26. Krautler MJ, Williams GR, Cohen SB, et al. Inter- and intraobserver reliability of radoigraphic diagnosis and treatment of acromioclavicular joint separations. Orthopedics 2012; 35: e1483–7. [DOI] [PubMed] [Google Scholar]
- 27. Motta P, Maderni A, Bruno L, Mariotti U. Suture rupture in acromioclavicular joint dislocation treated with flip buttons. Arthroscopy 2011; 27: 294–8. [DOI] [PubMed] [Google Scholar]
- 28. Fraschini G, Ciampi P, Scotti C, Ballis R, Peretti GM. Surgical treatment of chronic acromioclavicular dislocation: comparison between two surgical procedures for anatomic reconstruction. Injury 2010; 41: 1103–6. [DOI] [PubMed] [Google Scholar]
- 29. Mares O, Luneau S, Staquet V, Beltrand E, Bousquest P-J, Maynou C. Acute grade III and IV acromioclavicular dislocations: outcomes and pitfalls of reconstruction procedures using a synthetic ligament. Orthop Traumatol Surg Res 2010; 96: 721–6. [DOI] [PubMed] [Google Scholar]