Abstract
Background
Rupture of the pectoralis major (PM) tendon is a rare but severe injury. Several techniques have been described for PM fixation, including a transosseus technique, placing cortical buttons at the superior, middle and inferior PM tendon insertion points. The present cadaveric study investigates the proximity of the posterior branch of the axillary nerve to the drill positions for transosseus PM tendon repair.
Methods
Twelve cadaveric shoulders were used. The axillary nerve was marked during a preparatory dissection. Drills were passed through the humerus at the superior, middle and inferior insertions of the PM tendon and the drill bits were left in situ. The distance between these and each axillary nerve was measured using computed tomography.
Results
The superior drill position was in closest proximity to the axillary nerve (three-dimensional distance range 0–18.01 mm, mean 10.74 mm, 95% confidence interval 7.24 mm to 14.24 mm). The middle PM insertion point was also very close to the nerve.
Conclusions
Caution should be used when performing bicortical drilling of the humerus, especially when drilling at the superior border of the PM insertion. We describe ‘safe’ and ‘danger’ zones for the positioning of cortical buttons through the humerus reflecting the risk posed to the axillary nerve.
Keywords: Axillary nerve, pectoralis major, transosseus repair, cadaveric study, axillary nerve injury
INTRODUCTION
Rupture of the pectoralis major (PM) tendon is an uncommon but severe injury, commonly seen in athletes when it can be career-threatening. The reported incidence has risen in recent years and it is assumed that this is a reflection of an increased number of athletes performing high load activities, such as weightlifting and body building [1]. There is also an association with use of anabolic steroids [2]. PM is a fan-shaped muscle considered to have two heads: clavicular and sternal. The muscle fibres blend together before inserting onto the lateral lip of the bicipital groove of the humerus as a ‘bilaminar’ tendon [3]. The actions of PM at the shoulder are adduction, internal rotation and flexion, and the most frequent biomechanical mechanism of rupture is the application of an opposing force when the shoulder is in an extended position, coupled with a sudden and maximal contraction of the muscle. It is this combination of movements that is employed when performing a supine ‘bench press’ exercise and explains why this is associated with a high number of injuries [2]. A tear of the PM tendon can be categorized by the position of the tear, type 1 being in the muscle belly, type 2 at the myotendinous junction and type 3 involving the distal tendon [4], and a tear may involve one or both of the heads, with the sternal head rupturing more commonly than the clavicular head [3]. Early operative fixation is associated with an improved outcome and so is recommended for type 3 injuries [5].
Several techniques have previously been described for PM fixation. These include transosseus suture repair through a bone trough, using one or two rows of drill holes, periosteal sutures, suture anchors and cortical buttons [6–11]. Use of suture anchors relies on good cortical bone quality and repairs that do not require high tendon tension [12]. A new technique for repair using cortical buttons through the posterior cortex of the humerus has recently been described [13]. The ruptured PM tendon is identified at surgery, isolated and mobilised. A Krakow, or other grasping suture, is then sutured in the tendon, with a cortical button being located at the other end of the stitch. A trough is made in the humerus and the tendon is introduced into this trough, lateral to the attachment of the long head of biceps. The cortical buttons are then passed through drill holes in the humerus and secured.
The concern with a technique involving bicortical drilling, such as the cortical button technique, is the risk that is posed to the axillary nerve as it courses posteriorly to the humerus. The axillary nerve originates from the posterior cord of the brachial plexus (nerve roots C5 and C6). It passes anteriorly to subscapularis, traversing the quadrilateral space, before it divides into anterior and posterior branches at the posterior aspect of the humeral neck. The posterior branch supplies motor function to the posterior fibres of deltoid, as well as teres minor, before continuing as the lateral cutaneous nerve of the arm which supplies cutaneous sensation [14].
The present cadaveric study investigates the proximity of the axillary nerve to the position of transhumeral drill passages during PM repair and highlights axillary nerve injury as a potential complication of this technique.
MATERIALS AND METHODS
Ethical approval for the present study was granted by the Regional Research and Ethics Committee. Twelve cadaveric human specimen shoulders were used, consisting of six torso specimens. The specimens were prepared and stored at the Department of Anatomy, University of Bristol; they were fresh frozen specimens, stored at −17 °C, and thawed 2 days before use. The specimens were not embalmed. Female and male specimens were used (four male, two female). Mean age at death was 82.83 years (range 70 years to 91 years).
In the supine position, the shoulder specimens were dissected using an anterior deltopectoral approach, and the axillary nerve was identified and marked with 24-gauge (0.51 mm) steel wire. The conjoint tendon was transected and reflected medially, allowing the axillary nerve to be found at the inferior edge of subscapularis. The wire was passed through a cannulated spinal needle into the substance of the nerve (Fig. 1A). The wire was then advanced along the nerve. This technique of marking a nerve with wire has previously been described when marking the lingual and chorda tympani nerves [15]. The specimens were then turned to lie prone, and a posterior approach to the shoulder was performed. The posterior fibres of deltoid were reflected laterally and the nerve was found deep to the inferior edge of teres minor. The nerve wire was then checked to ensure it had progressed within the substance of the nerve, and was then advanced further along the posterior nerve to its terminal division.
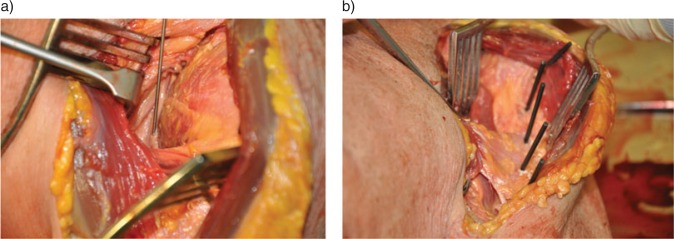
Fig. 1.
Photographs of the wire being inserted into the axillary nerve and the drill bits in situ following insertion into the humerus. The pectoralis major insertion is intact, allowing accurate placement of the drill bits at the superior, middle and inferior insertion points.
After the initial preparation of the specimens, the positions for PM tendon repair were identified with the specimen in the supine position. The positions were at the superior insertion of PM, a middle position and the inferior insertion of PM. A 2.5-mm drill bit was drilled through the humerus at each of these positions to imitate the drilling and placement of transosseus sutures or cortical buttons during PM repair. Over-drilling of the posterior cortex was not deliberately performed. The drill bits used were steel and 95 mm in length. Each was left in situ (Fig. 1B). The skin and superficial tissues were then carefully sutured back to their original position, and the specimens stored in a cold storage room prior to computed tomography (CT) scanning.
A Siemens Somatom Sensation 16 scanner (Siemens, Frimley, UK) was used to obtain images of each shoulder 2 days after drill bit insertion. There was no significant artefact from either the wire or drill bits. The images were interpreted using open access radiological analysis software (OsiriX; http://www.osirix-viewer.com/) [16] and the distances between the axillary nerve wire and the closest point of each drill bit were measured in axial and coronal planes. Each measurement was made by two investigators (SL and OO), two weeks apart. These measurements were used to calculate an overall three-dimensional (3D) distance between the closest point of the wire to where the drill bit passes through the posterior cortex of the humerus. This technique has previously been used to measure distances between structures radiologically [17]. Figure 2 shows the CT images of the drill bits and nerve marked with wire. Measurements were then made from the most superior point of the humeral head to the most superior and inferior points at which the axillary nerve wire passed behind the posterior humerus; this allowed production of ‘danger’ and ‘safe’ zones for the nerve in relation to the humerus.
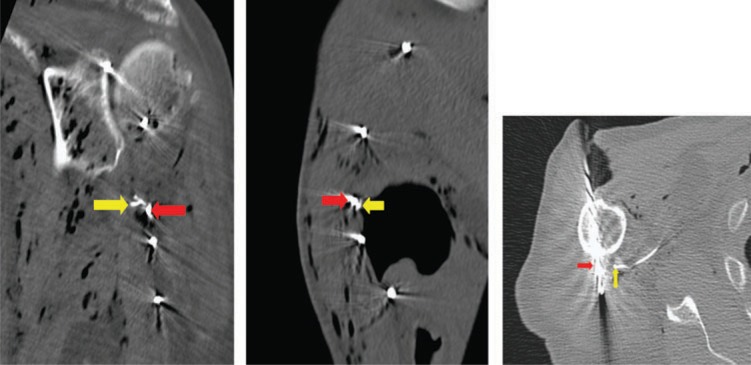
Fig. 2.
Computed tomography images showing the drill bits through the humerus, with the superior endobutton drill bit (red arrow) and the axillary nerve marked by wire (yellow arrow). The two drill bits superior to this drill bit were placed for a separate study.
All specimens were handled according to the University of Bristol, Department of Anatomy standard protocols.
RESULTS
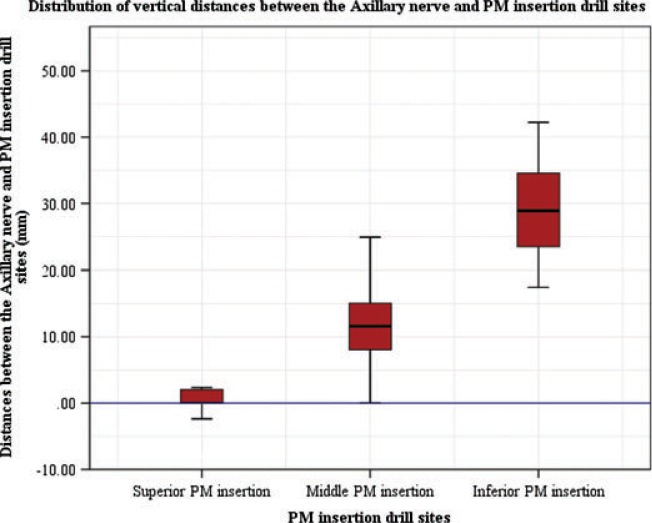
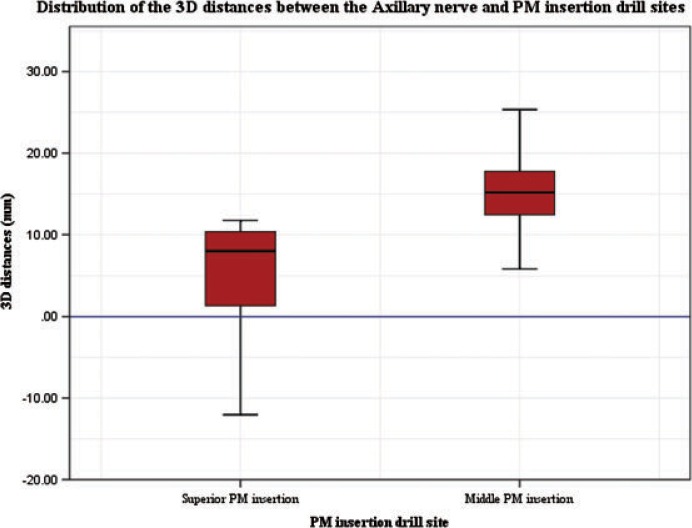
Inter-observer error was excellent (Pearson's correlation = 0.992), which was significant (two tailed ≤ 0.001). The superior drill position was in closest proximity to the axillary nerve (3D distance, range 0 mm to 18.01 mm, mean 10.74 mm, 95% confidence interval 7.24 mm to 14.24 mm), as shown in Table 1. Table 2 shows the results for the middle cortical button insertion point. This drill passage point was also very close to the nerve in some specimens (3D distance, range 1.66 mm to 18.04 mm, mean 10.74 mm, 95% confidence interval 7.01 mm to 14.47 mm). These are represented graphically in the box plots in Figs 3 and 4.
Table 1.
Distance (mm) between the axillary nerve and position of superior drill passage position
| Distances from superior endobutton position to axillary nerve (n = 12) |
|||||
|---|---|---|---|---|---|
| Range | Mean | SD | SE | 95% confidence interval | |
| Vertical distance | 0–7.95 | 2.04 | 2.77 | 0.80 | 0.28–3.80 |
| Axial distance | 0–11.8 | 7.40 | 3.69 | 1.07 | 5.05–9.75 |
| Overall (3D) distance | 0–18.01 | 10.74 | 5.51 | 1.59 | 7.24–14.24 |
Table 2.
Distance (mm) between the axillary nerve and position of middle drill passage position
| Distances from middle endobutton position to axillary nerve (n = 12) |
|||||
|---|---|---|---|---|---|
| Range (mm) | Mean (mm) | SD | SE | 95% confidence interval | |
| Vertical distance | 0–25.8 | 12.13 | 7.91 | 2.28 | 7.10–17.16 |
| Axial distance | 1.15–13.2 | 7.54 | 4.27 | 1.23 | 4.82–10.25 |
| Overall (3D)distance | 1.66–18.04 | 10.74 | 5.87 | 1.7 | 7.01–14. |
Fig. 3.
Distribution of the vertical distances between drill sites and axillary nerve (axillary nerve position at 0 on the y-axis). PM, pectoralis major.
Fig. 4.
Distrubution of three-dimensional (3D) distances between drill sites and axillary nerve (axillary nerve position at 0 on the y-axis). PM, pectoralis major.
The inferior insertion drill bit was the most distant from the nerve (vertical distance, range 16.95 mm to 27.35 mm, mean 28.45 mm, 95% confidence interval 23.53 mm to 33.39 mm).
The results for the assessment of a potential ‘danger zone’ where the axillary nerve passes behind the posterior humerus and is at risk of damage from drill passage are shown in Table 3.
Table 3.
‘Danger’ zone measurements (cm): vertical distances between the most superior point of the humerus and the axillary nerve as it passes posteriorly to the humerus
| Axillary nerve ‘danger zone’ measurements (n = 12) | ||||
|---|---|---|---|---|
| Range | Mean | SD | SE | |
| Superior limit | 4.6–6.7 | 5.59 | 0.704 | 0.203 |
| Inferior limit | 5.1–7.4 | 6.47 | 0.698 | 0.202 |
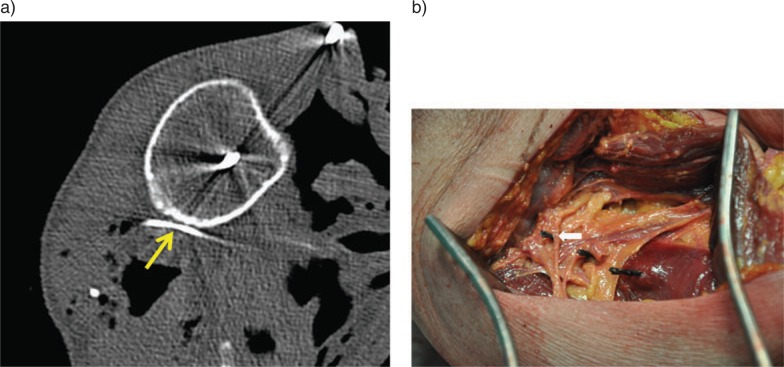
Figure 5A shows an axial view of the proximity of the nerve (yellow arrow) to the posterior humerus and Fig. 5B shows a specimen where it was noted at the time of anatomical preparation that the drill bit had come into contact with the nerve.
Fig. 5.
Computed tomography (axial) image to demonstrate the proximity of the axillary nerve (yellow arrow) to the posterior humerus and photograph of the drill bits following insertion, with the white arrow marking the axillary nerve and its proximity to the superior drill bit.
DISCUSSION
PM tendon rupture was first described in 1822 by Patissier, who observed the injury in a butcher [18]. The tendon is frequently injured during weight-lifting or wrestling, when the arm is externally rotated and abducted, and most ruptures occur at the humerus insertion [19]. Surgical repair offers improved outcomes over conservative management [20].
The technique for cortical button repair of the PM tendon is a newly-described technique, and it was suggested to be a stronger fixation technique than previously described methods [13]. The present anatomical study highlights the proximity of the axillary nerve during bicortical drilling during this procedure. Surgeons should use appropriate caution when using this method of PM repair.
In their series of five cases using this technique, Uchiyama et al. reported no postoperative or neurological complications for this method of fixation [13] and we were unable to identify any other studies describing axillary nerve damage during PM repair. There have, however, been previous cadaveric studies investigating the proximity of the axillary nerve to the proximal humerus. In their study, Saran et al. measured the distances between screw positions of proximal humerus locking plates and the axillary nerve. They measured the distances during dissections, but found that some screw holes, particularly those located at the surgical neck, were very close to the nerve, with one specimen nerve being only 2 mm away from a screw in that area (mean 6.6 mm) [21].
Strength of repair is obviously important for patient satisfaction and outcome. Although some studies have reported the cortical button method to be stronger than other fixation methods, a recent cadaveric study reported no significant difference between the biomechanical failure rates of this method compared to suture anchor and transosseus fixation [22]. A further study found transosseus fixation to be superior to cortical button fixation [23]. Failure of the fixation tends to be through the tendon suture itself [22,23].
The limitations of the present study include the fact that overdrilling of the posterior cortex was avoided and therefore the distances between the nerve and the tips of the drill bits will underestimate the actual distances that occur during surgery. There is also the question of orientation of the drill passages, which will not affect the vertical distance between nerve and drill bit, although it may affect axial distances. When considering the course of the axillary nerve in relation to the posterior humerus, it is clear that aiming a transosseus drill anteriorly will reduce the risk of nerve injury. In the present study, the drill bits were aimed perpendicularly to both the cortex of the anterior humerus at the point of PM insertion and the vertical line of the shaft of the humerus. Drill–nerve distance will differ with a variation in drill trajectory and this would need to be considered when performing PM repair; a more anterior drill passage will tend to increase the drill–nerve distance, increasing the margin of safety. Furthermore, protection of the axillary nerve may be attempted during drilling by guarding the posterior cortex; no protection of this kind was used during the present study.
We highlight the age of the specimens at death (83 years); patients who suffer PM tendon ruptures are generally young, athletic individuals, and so the anatomy of our specimens will undoubtedly differ from those who are most likely to suffer this injury. The use of cadavers itself may be seen as a limitation. Tissue quality is different from in vivo tissue; however, the specimens were fresh frozen and carefully preserved to be as clinically accurate as possible. Finally, the preparation of the axillary nerve with the wire may have disrupted the anatomy; however, this is an acceptable technique, which has been used previously in neuro-anatomical investigations [15].
Following this investigation, we have suggested ‘safe’ and ‘danger’ zones (Fig. 6) with regard to the posterior branch of the axillary nerve as it courses posteriorly to the humerus. These measurements are in keeping with previous studies; Liu et al. reported the range of the axillary nerve to be 4.0 cm to 6.7 cm from the superior aspect of the humerus, with a mean of 5.2 cm [24], and Bono et al. gave a similar range of 4.5 cm to 6.9 cm, with a mean of 6.09 cm [25]. Both of these studies measured the distance during dissection, and it is encouraging that our results are similar, given that we have used radiological methods to measure the distances.
Fig. 6.
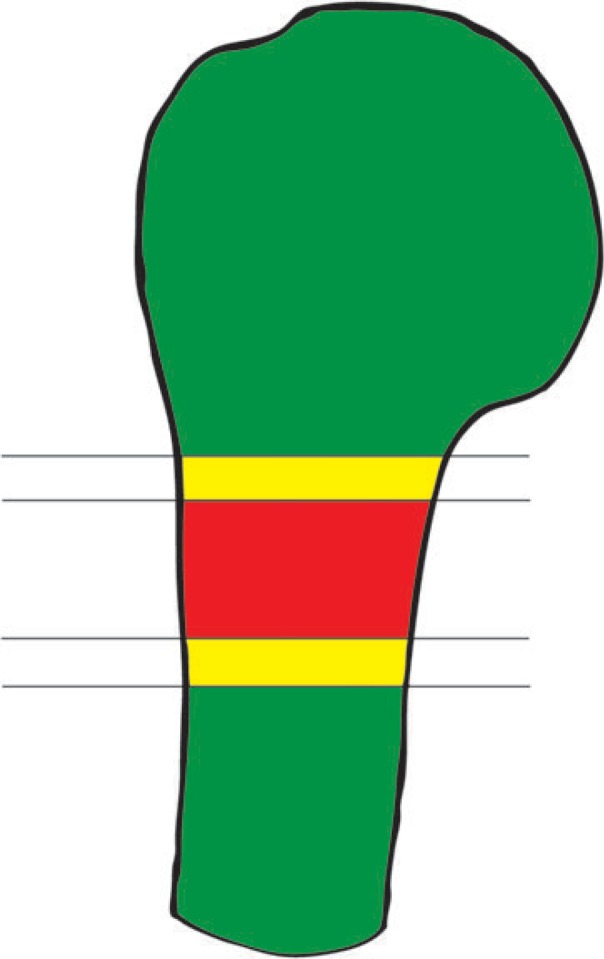
Diagram of ‘safe’ and ‘danger’ zones from the tip of the humerus marking the danger posed to the axillary nerve at these positions. Red ‘danger’ area between 5.6 and 6.5 cm from the superior point of the humerus.
Conclusions
To our knowledge, the present study is the first cadaveric study to investigate the proximity of the axillary nerve specifically during PM repair. It highlights the need for caution when using a technique requiring bicortical drilling. The variability of axillary nerve anatomy places the nerve at risk during the passage of a drill across the humerus during PM repair, particularly in the upper and middle thirds of the PM insertion.
The authors thank Bob Colborne and Anna Halliday at the Versalius Centre, Department of Anatomy, University of Bristol, for their assistance with cadaveric specimen preparation, and Martyn Snow for radiographic imaging of the specimens.
Footnotes
Conflicts of Interest The authors declare no conflict of interests
References
- 1. Kircher J, Ziskoven C, Patzer T, Zaps D, Bittersohl B, Krauspe R. Surgical and nonsurgical treatment of total rupture of the pectoralis major muscle in athletes: update and critical appraisal. Open Access J Sports Med 2010; 1: 201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pochini A, Ejnisman B, Andreoli C, et al. Pectoralis muscle rupture in athletes: a prospective study. Am J Sports Med 2010; 38: 92–8. [DOI] [PubMed] [Google Scholar]
- 3. Connell D, Potter H, Sherman M, Wickiewicz T. Injuries of the pectoralis major muscle: evaluation with MR imaging. Radiology 1999; 210: 785–91. [DOI] [PubMed] [Google Scholar]
- 4. Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma 1980; 20: 262–4. [DOI] [PubMed] [Google Scholar]
- 5. Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S. Rupture of pectoralis major muscle. Am J Sports Med 2004; 32: 1256–62. [DOI] [PubMed] [Google Scholar]
- 6. Berson BL. Surgical repair of pectoralis major rupture in an athlete: case report of an unusual injury in a wrestler. Am J Sports Med 1979; 7: 348–51. [DOI] [PubMed] [Google Scholar]
- 7. Kretzler HH, Jr, Richardson AB. Rupture of the pectoralis major muscle. Am J Sports Med 1989; 17: 453–8. [DOI] [PubMed] [Google Scholar]
- 8. McEntire JE, Hess WE, Coleman SS. Rupture of the pectoralis major muscle: a report of eleven injuries and review of fifty-six. J Bone Joint Surg Am 1972; 54: 1040–6. [PubMed] [Google Scholar]
- 9. Miller MD, Johnson DL, Fu FH, Thaete FL, Blanc RO. Rupture of the pectoralis major muscle in a collegiate football player: use of magnetic resonance imaging in early diagnosis. Am J Sports Med 1993; 21: 475–7. [DOI] [PubMed] [Google Scholar]
- 10. Schepsis AA, Grafe MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle: outcome after repair of acute and chronic injuries. Am J Sports Med 2000; 28: 9–15. [DOI] [PubMed] [Google Scholar]
- 11. Zeman SC, Rosenfeld RT, Lipscomb PR. Tears of the pectoralis major muscle. Am J Sports Med 1979; 7: 343–7. [DOI] [PubMed] [Google Scholar]
- 12. Petilon J, Sekiya J. Pectoralis major muscle repair. In: ElAttrache N, Harner C, Mirzayan R. et al., eds. Surgical techniques in sports medicine. Philadelphia, PA: Lippincott Williams & Wilkins, 2007:197–202. [Google Scholar]
- 13. Uchiyama Y, Miyazaki S, Tamaki T, et al. Clinical results of a surgical technique using endobuttons for complete tendon tear of pectoralis major muscle: report of five cases. Sports Med Arthrosc Rehabil Ther Technol 2011; 3: 20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rashid A, Abdul-Jabar H, Lam F. Nerve injury associated with shoulder surgery. Curr Orthopaedics 2008; 22: 284–8. [Google Scholar]
- 15. Trost O, Rouchy R, Teyssier C, et al. CT-scan imaging of iron marked chorda tympani nerve: anatomical study and educational perspectives. Surgical Radiol Anat 2011; 33: 515–21. [DOI] [PubMed] [Google Scholar]
- 16. Rosset A, Spadola L, Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imaging 2004; 17: 205–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lancaster S, Clark D, Redpath Y, Hughes D, Crowther M, Lewis S. Blockade of the suprascapular nerve: a radiological and cadaveric study comparing landmark and ultrasouns-guided blocking techniques. Shoulder Elbow 2012; 5: 173–7. [Google Scholar]
- 18. Patissier P. Traite des maladies artisans. Paris: 1822 cited in Manske R, Prohaska D. Pectoralis major tendon repair post surgical rehabilitation. North Am J Sports Phys Ther 2007; 2: 22–33. [PMC free article] [PubMed] [Google Scholar]
- 19. Bak K, Cameron E, Henderson I. Rupture of the pectoralis major: a meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc 2000; 8: 113–19. [DOI] [PubMed] [Google Scholar]
- 20. Kakwani R, Matthews J, Kumar K, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle: surgical treatment in athletes. Int Orthop 2007; 31: 159–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Saran N, Bergeron S, Benoit B, Reindl R, Harvey E, Berry G. Risk of axillary nerve injury during percutaneous proximal humerus locking plate insertion using an external aiming guide. Injury 2010; 41: 1037–40. [DOI] [PubMed] [Google Scholar]
- 22. Sherman S, Lin E, Verma N, et al. Biomechanical analysis of the pectoralis major tendon and comparison of techniques for tendo-osseus repair. Am J Sports Med 2012; 40: 1887–94. [DOI] [PubMed] [Google Scholar]
- 23. Rabuck S, Lynch J, Guo X, et al. Biomechanical comparison of 3 methods to repair pectoralis major ruptures. Am J Sports Med 2012; 40: 1635–40. [DOI] [PubMed] [Google Scholar]
- 24. Liu K, Chen T, Shyu J, Wang S, Liu J, Chou P. Anatomic study of the axillary nerve in a Chinese cadaveric population: correlation of the course of the nerve with proximal humeral fixation with intramedullary nail or external skeletal fixation. Arch Orthop Trauma Surg 2011; 131: 669–74. [DOI] [PubMed] [Google Scholar]
- 25. Bono C, Grossman M, Hochwald N, Tornetta P. Radial and axillary nerves. Anatomic considerations for humeral fixation (abstract only). Clin Orthop Relat Res 2000; 373: 259–64. [PubMed] [Google Scholar]