Abstract
OBJECTIVES
The short-term feasibility and safety of non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia for thoracic surgery remains unknown. Therefore, we conducted a meta-analysis to provide evidence for the short-term efficacy and safety profile of non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia for thoracic surgery.
METHODS
We performed a systematic literature search in PubMed, Embase, Cochrane Library databases and Google Scholar, as well as American Society of Clinical Oncology to identify relevant studies comparing non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia with conventionally intubated video-assisted thoracoscopic surgery under general anaesthesia, dated up to 31 August 2015. Data concerning global in-operating room time, hospital stays, rate of postoperative complications and perioperative mortality were extracted and analysed. We conducted a meta-analysis of the overall results and two subgroup analyses based on study design (a meta-analysis of randomized controlled trials and a second meta-analysis of observational studies).
RESULTS
Four randomized controlled trials and six observational studies with a total of 1283 patients were included. We found that in the overall analysis, patients treated with non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia achieved significantly shorter global in-operating room time [weighted mean difference = −41.96; 95% confidence interval (CI) = (−57.26, −26.67); P < 0.001] and hospital stays [weighted mean difference = −1.24; 95% CI = (−1.46, −1.02); P < 0.001] as well as a lower rate of postoperative complications [relative risk = 0.55; 95% CI = (0.40, 0.74); P < 0.001] than patients treated with intubated video-assisted thoracoscopic surgery under general anaesthesia. Subgroup meta-analyses based on study design achieved the same outcomes as overall analysis. In our meta-analysis, no perioperative mortality was observed in patients treated with non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia.
CONCLUSIONS
Non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia for thoracic surgery proved to be feasible and safe. Future multicentre and well-designed randomized controlled trials with longer follow-up are needed to confirm and update the findings of our study, as well as the long-term efficacy of non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia.
Keywords: Video-assisted thoracoscopic surgery, Non-intubated, Anaesthesia, Thoracic surgery, Meta-analysis
INTRODUCTION
Video-assisted thoracoscopic surgery (VATS) has become globally accepted and utilized as a minimally invasive surgical technique [1], which usually requires conventionally intubated general anaesthesia with single-lung ventilation by using a double-lumen tube or endobronchial blocker to obtain a quiet, optimally visualized and better surgical environment [2]. However, the adverse effects of general anaesthesia with intubation such as intubation-related airway injury, ventilation-induced lung injury, residual neuromuscular blockade and postoperative nausea and vomiting cannot be neglected. Ventilation-related lung injury occurs in ∼4% of major lung resections and carries a mortality rate as high as 25% [3]. Sugasawa et al. [4] found that single-lung ventilation could induce inflammatory responses during lung resection, which may be associated with postoperative complications. Therefore, to prevent serious complications related to conventional general anaesthesia with intubation and comply with the need for smoother patient recovery, the non-intubated VATS technique under loco-regional anaesthesia has recently been intensively investigated, reported and advocated [5]. These non-intubated VATS procedures were usually carried out under loco-regional anaesthetic techniques, such as thoracic epidural anaesthesia, intercostal nerve blocks and paravertebral blocks, without tracheal intubation, during which patients were awake or mildly sedated with spontaneous breathing. In 1997, Nezu et al. retrospectively compared thoracoscopic wedge resection of blebs under local anaesthesia with the same surgical procedure under general anaesthesia with intubation. They found that thoracoscopic wedge resection under local anaesthesia was safe and offered the benefit of shorter hospital stays than intubated VATS under general anaesthesia [6]. Since then, many clinical trials have been carried out to explore the feasibility of non-intubated VATS under loco-regional anaesthesia in the management of diverse oncological conditions, such as malignant pleural effusion, peripheral lung nodules, mediastinal tumours and non-oncological indications including pneumothorax, emphysema, pleural infections and interstitial lung disease [7].
Previously, Hausman et al. [8] had found that the application of regional anaesthesia in patients with chronic obstructive pulmonary disease was associated with a lower risk of postoperative morbidity than general anaesthesia with intubation, which indicated that patients could benefit from regional anaesthesia. In addition, many clinical studies [9, 10] had revealed that patients treated with non-intubated VATS under loco-regional anaesthesia yielded fewer postoperative pulmonary complications than intubated VATS under general anaesthesia. Therefore, non-intubated VATS under loco-regional anaesthesia seemed to be a good alternative surgical option for thoracic surgery. Although many studies had pointed out that non-intubated VATS under loco-regional anaesthesia yielded a faster postoperative recovery and fewer complications than intubated VATS under general anaesthesia, all of them were either case reports or small cohort studies which lacked strong evidence to elucidate the general feasibility and safety of non-intubated VATS under loco-regional anaesthesia [11, 12]. Therefore, the general short-term feasibility and safety of non-intubated VATS under loco-regional anaesthesia for thoracic surgery still remains unknown. Thus, in this study, we aimed to conduct a meta-analysis to generate a valid picture of the short-term feasibility and safety of non-intubated VATS under loco-regional anaesthesia for thoracic surgery.
MATERIALS AND METHODS
Search strategies
Systematic computerized searches in the PubMed, Embase, Cochrane Library databases and Google Scholar, as well as American Society of Clinical Oncology (ASCO) for studies dated up to 31 August 2015, were performed with the following search terms: ‘video-assisted thoracoscopic surgery or VATS’; ‘wake or awake’; ‘non-intubated or nontracheal intubation’; ‘regional anaesthesia or local anaesthesia’. All reference lists from the studies selected by electronic searching were scanned to further identify relevant studies.
Study selections
The following inclusion criteria were used for study selection: (i) either randomized controlled trials (RCTs) or observational studies (case–control or cohort studies) comparing non-intubated VATS under loco-regional anaesthesia (case group) with conventionally intubated VATS under general anaesthesia (control group) for thoracic surgery; (ii) in each study, all patients received the same surgical procedures under VATS; (iii) sufficient data could be obtained for the estimate of weighted mean differences (WMDs) or relative risk (RR); and (iv) the most recent or complete studies were included if the studies were based on overlapping patients.
Meanwhile, the exclusion criteria were as follows: (i) studies without comparison of non-intubated VATS under loco-regional anaesthesia with intubated VATS under general anaesthesia for thoracic surgery; (ii) patients in case and control groups treated with different surgical procedures; (iii) papers not published in English; (iv) case reports, abstracts, conference reports or experiments; and (v) papers without any relevant data that could be extracted for analysis.
Data extraction and quality assessment
To avoid bias, three authors (Han-Yu Deng, Zi-Jiang Zhu and Yun-Cang Wang) independently extracted data from the studies included in our meta-analysis and compared the results. Discrepancies were resolved by the fourth author's (Wen-Ping Wang) adjudication. Data were carefully retrieved from these studies by using a standardized data collection method. The following data were collected from each study: first author, year of publication, number of patients, surgical procedure and study design. The outcomes for analyses included global in-operating room time, hospital stays, postoperative complications (including air leakage, atelectasis, pneumonia, urinary retention and atrial fibrillation) and perioperative mortality. The Jadad scale was used for quality assessment of the RCTs, which contained randomization (0–2 points), blinding of the studies (0–2 points) and withdrawals (0–1 point). The high-quality study was defined as a study with a quality score of ≥3 points. Observational studies were evaluated by the Newcastle–Ottawa scale (NOS) [13], which consists of three factors: patient selections, comparability of the study groups and assessment of outcomes. A score of 0–9 (allocated as stars) was assigned to each observational study and the high-quality study was defined as a study with a quality score of ≥7 stars. Risk of bias analysis was conducted by using Review Manager® Version 5.1.7 for Windows (The Cochrane Collaboration, Software Update, Oxford, UK). The name of the first author and the publication year for each article were used for identification.
Statistical analysis
Studies were grouped based on study design (RCTs and observational studies). A meta-analysis of overall results and two subgroup meta-analyses (a meta-analysis of RCTs and another meta-analysis of observational studies) were conducted. This was done to examine the consistency of results across different study designs with potential biases. All analyses were performed by using the STATA 12.0 package (Stata Corp., College Station, TX, USA). We used WMDs with 95% confidence intervals (CIs) to analyse the continuous variables in the same scale (global in-operating room time and hospital stays). When the mean or standard deviation (SD) was not reported in the study, it was estimated according to the recommendation of the Cochrane Collaboration. The dichotomous data (rate of postoperative complications) were calculated using RR.
For each study, the between-study heterogeneity was assessed using χ2-based Q statistics and I2 test. A random-effects model was used if high heterogeneity of the studies (P < 0.1 or I2 > 50%) was observed; otherwise, a fixed-effects model was used. Sensitivity analysis was performed by sequential removal of each study. A funnel plot was used to estimate potential publication bias. Asymmetry of the funnel plot was tested by Begg's test and Egger's test [14]. Statistical significance was set at P < 0.05.
RESULTS
Description of studies
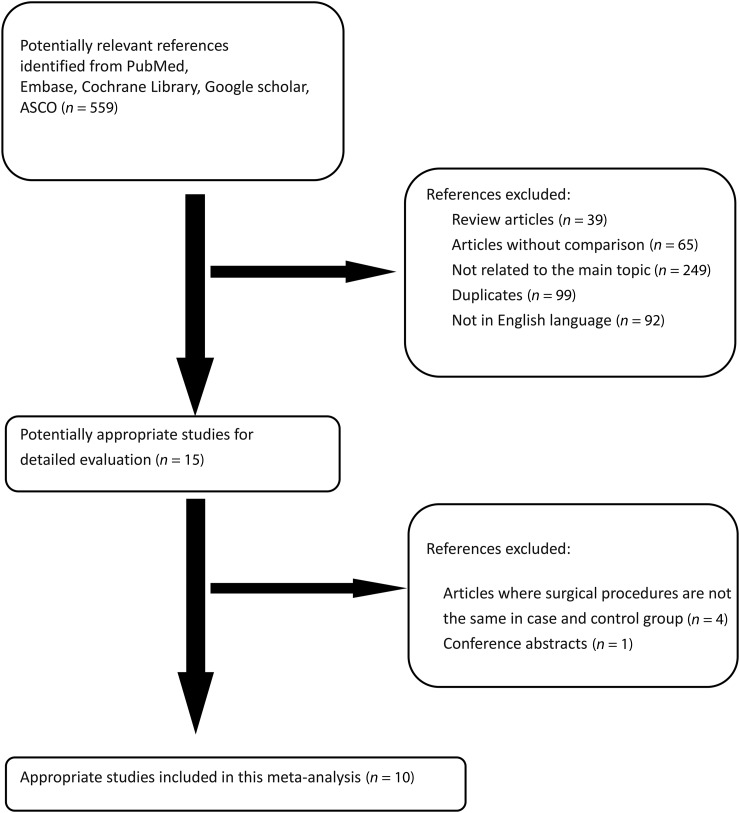
A flow chart of our study is shown in Fig. 1. Four RCTs [9, 12, 15, 16] (490 patients) and six observational studies [6, 10, 17–20] (793 patients) that satisfied the criteria were identified, with a total of 1283 patients for final analyses. For patients in the group of non-intubated VATS under loco-regional anaesthesia, the anaesthetic techniques consisted of mild sedation and regional or local anaesthesia without endobronchial intubation, while for patients in the group of intubated VATS under general anaesthesia, conventional general anaesthesia with endobronchial intubation was applied. The main data extracted from these studies included in our meta-analysis are listed in Table 1. The baseline data of the patients in each study were comparable or well matched. Data for analyses consisted of global in-operating room time, hospital stays, rate of postoperative complications and perioperative mortality. Postoperative complications reported in these studies were non-fatal complications including prolonged air leaks, pneumonia, atelectasis, atrial fibrillation and urinary retention. Global in-operating room time could be obtained from seven studies [10, 12, 15, 17–20] and hospital stay could be obtained from all studies, except for the one that had no information about the SD of hospital stays [9]. The rate of postoperative complications could also be obtained from all studies excepting one that did not report complications [16].
Figure 1:
Flow chart showing the progress of trials throughout the review. ASCO: American Society of Clinical Oncology.
Table 1:
Characteristics of the studies included in our meta-analysis
| Author (year) | No. of cases/controls | Surgery | Study design | Quality assessment |
|---|---|---|---|---|
| Nezu et al. (1997) [6] | 32/38 | Wedge resections of blebs | Observational study | NOS: 7 stars |
| Pompeo et al. (2004) [15] | 30/30 | Resection of lung nodule | RCT | Jadad score: 3 points |
| Pompeo et al. (2007) [12] | 21/22 | Bullectomy with pleural abrasion | RCT | Jadad score: 3 points |
| Chen et al. (2011) [17] | 30/30 | Lobectomy for lung cancer | Observational study | NOS: 8 stars |
| Pompeo et al. (2011) [10] | 41/19 | Lung volume reduction surgery | Observational study | NOS: 8 stars |
| Noda et al. (2012) [18] | 15/42 | VATS for pneumothorax | Observational study | NOS: 7 stars |
| Pompeo and Dauri (2013) [16] | 20/20 | Pleurodesis of malignant pleural effusion | RCT | Jadad score: 2 points |
| Wu et al. (2013) [19] | 36/48 | Lobectomy for lung cancer | Observational study | NOS: 8 stars |
| Mineo et al. (2014) [20] | 231/231 | Pleurodesis of malignant pleural effusion | Observational study | NOS: 8 stars |
| Liu et al. (2015) [9] | 167/180 | Wedge resection or lobectomy or bullae resection | RCT | Jadad score: 2 points |
RCT: randomized controlled trial; VATS: video-assisted thoracoscopic surgery; NOS: Newcastle–Ottawa scale.
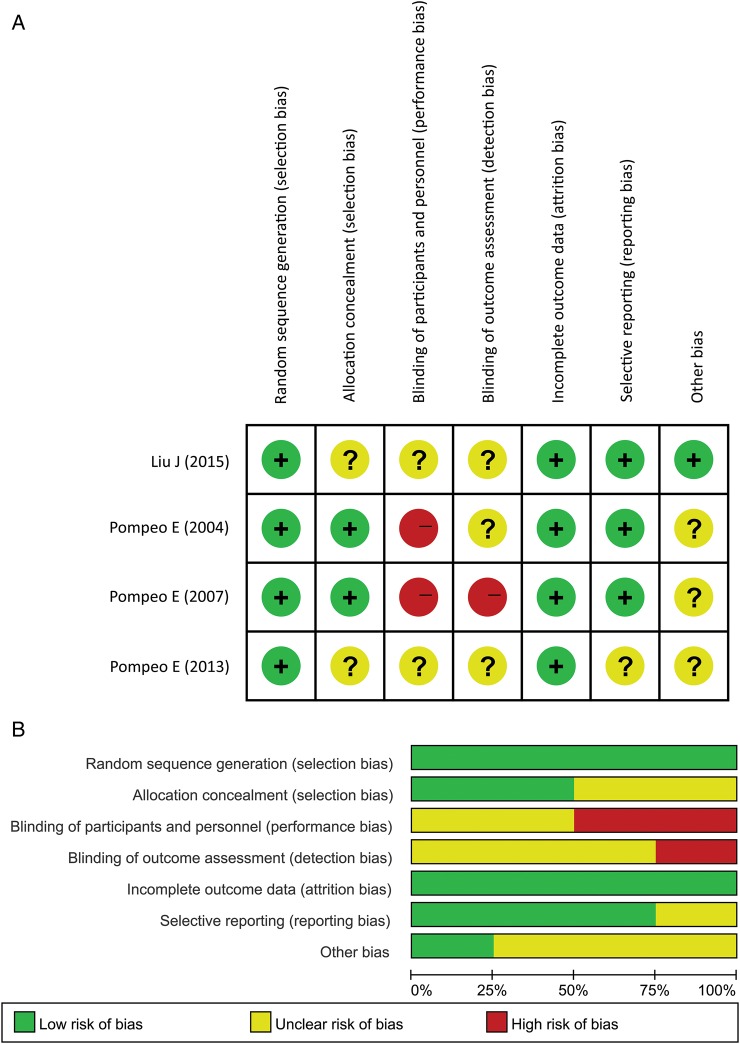
Quality assessment and risk of bias
Quality assessments of these studies included in our meta-analysis are listed in Table 1. Four RCTs were evaluated by Jadad scale, whereas six observational studies were evaluated by NOS. All RCTs mentioned randomization and withdrawal of patients, but none mentioned study blinding. Two RCTs with scores of 3 points used proper methods for randomization [12, 15], whereas the other two RCTs with scores of 2 points did not give detailed methods for randomization [9, 16]. Risk of bias analysis of the RCTs revealed concern about blinding bias of these studies, including performance and detection bias (Fig. 2). Quality evaluation of the observational studies showed that all of them were ranked as studies with high quality, indicating a low risk of bias.
Figure 2:
Risk of bias analysis for the RCTs: (A) risk of bias summary: a review of authors' judgements about each risk of bias item for each included study; (B) risk of bias graph: a review of authors' judgements about each risk of bias item presented as percentages across all included studies.
Meta-analysis of randomized controlled trials
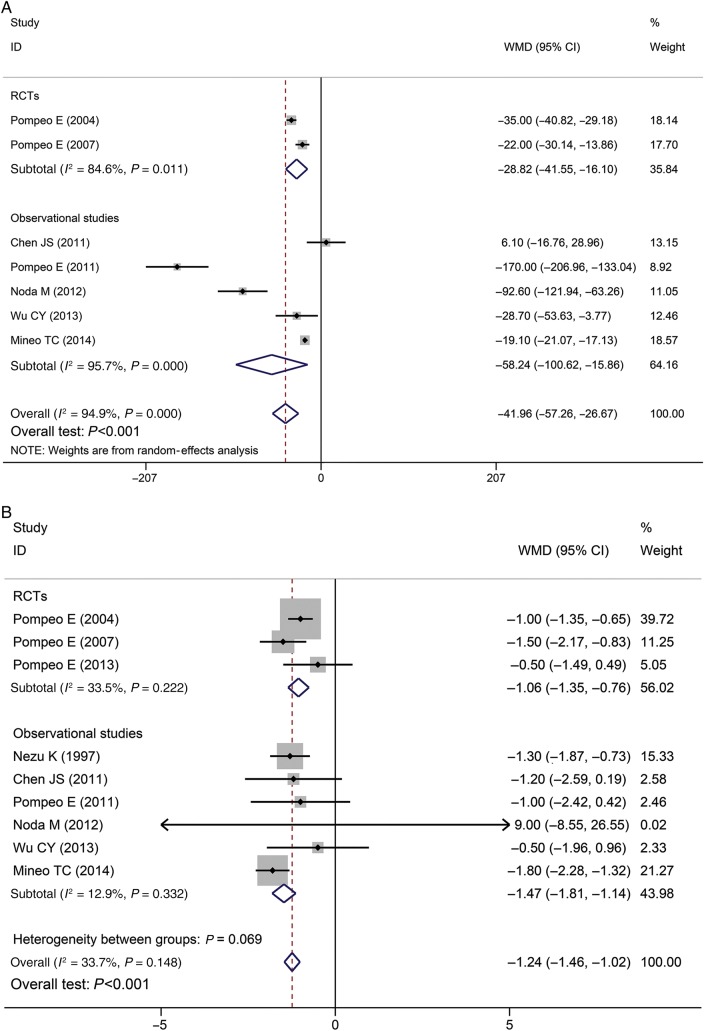
Four RCTs comprising 490 patients were included in the analysis (Table 2). Patients in the case group of non-intubated VATS under loco-regional anaesthesia had significantly shorter global in-operating room time than patients in the control group treated with intubated VATS under general anaesthesia [random effects: WMD = −28.82; 95% CI = (−44.55, −16.10); P < 0.001; I2 = 84.6%, Fig. 3A]. Non-intubated VATS under loco-regional anaesthesia also achieved significantly shorter hospital stays than intubated VATS under general anaesthesia [fixed effects: WMD = −1.06; 95% CI = (−1.35, −0.76); P < 0.001; I2 = 33.5%, Fig. 3B]. Moreover, non-intubated VATS under loco-regional anaesthesia yielded a significantly lower rate of postoperative complications than intubated VATS under general anaesthesia (6.9 and 15.0%, respectively) [fixed effects: RR = 0.46; 95% CI = (0.26, 0.82); P = 0.009; I2 = 23.4%, Fig. 3C]. There was no perioperative mortality in patients of either group.
Table 2:
Main outcomes extracted from the studies included in our meta-analysis
| Author (year) | Global in-operating room time (min)a |
Hospital stays (days)a |
Postoperative complicationsb |
Perioperative mortalityc |
||||
|---|---|---|---|---|---|---|---|---|
| Case | Control | Case | Control | Case | Control | Case | Control | |
| Nezu et al. (1997) [6] | NR | NR | 4.5 ± 1.3 | 5.8 ± 1.1 | 3/29 | 4/34 | 0/32 | 0/32 |
| Pompeo et al. (2004) [15] | 65 ± 11.9 | 100 ± 11.1 | 2.0 ± 0.7 | 3.0 ± 0.7 | 1/29 | 3/27 | 0/30 | 0/30 |
| Pompeo et al. (2007) [12] | 79.3 ± 12.7 | 101.3 ± 14.5 | 2.2 ± 0.9 | 3.7 ± 1.3 | 3/18 | 2/22 | 0/21 | 0/22 |
| Chen et al. (2011) [17] | 229.3 ± 43.7 | 223.3 ± 46.6 | 5.9 ± 2.2 | 7.1 ± 3.2 | 3/27 | 10/20 | 0/30 | 0/30 |
| Pompeo et al. (2011) [10] | 127 ± 15.6 | 297 ± 81.5 | 6.0 ± 1.5 | 7.0 ± 3.0 | 7/34 | 8/11 | 0/41 | 0/19 |
| Noda et al. (2012) [18] | 116.5 ± 35.2 | 209.1 ± 77.1 | 26.3 ± 33.8 | 17.3 ± 13.0 | 4/11 | 13/29 | 0/15 | 4/38 |
| Pompeo and Dauri (2013) [16] | NR | NR | 3.8 ± 1.7 | 4.3 ± 1.5 | NR | NR | NR | NR |
| Wu et al. (2013) [19] | 247.9 ± 38.5 | 276.6 ± 76.1 | 6.7 ± 3.3 | 7.2 ± 3.5 | 9/27 | 17/31 | 0/36 | 0/48 |
| Mineo et al. (2014) [20] | 65.8 ± 7.5 | 84.9 ± 13.3 | 3.1 ± 2.5 | 4.9 ± 2.8 | 12/219 | 20/211 | 0/231 | 5/226 |
| Liu et al. (2015) [9] | NR | NR | NR | NR | 11/156 | 30/150 | 0/167 | 0/180 |
NR: not reported.
aExpressed as mean ± standard deviation.
bExpressed as number of patients with complications/number of patients without complications.
cExpressed as no. of dead/no. of alive.
Figure 3:
Forest plot of: (A) global in-operating room time; (B) hospital stays; (C) postoperative complications in patients treated with non-intubated VATS under non-general anaesthesia. RCTs: randomized controlled trials; VATS: video-assisted thoracoscopic surgery; WMD: weighted mean difference; CI: confidence interval.
Meta-analysis of observational studies
Six observational trials comprising 793 patients were included in the present analysis (Table 2). Patients treated with non-intubated VATS under loco-regional anaesthesia obtained significantly shorter global in-operating room time than patients in the group of intubated VATS under general anaesthesia [random effects: WMD = −58.24; 95% CI = (−100.62, −15.86); P = 0.007; I2 = 95.7%, Fig. 3A]. Non-intubated VATS under loco-regional anaesthesia also achieved significantly shorter hospital stays than intubated VATS under general anaesthesia [fixed effects: WMD = −1.47; 95% CI = (−1.81, −1.14); P < 0.001; I2 = 12.9%, Fig. 3B]. Moreover, non-intubated VATS under loco-regional anaesthesia achieved a significantly lower rate of postoperative complications than intubated VATS under general anaesthesia (9.9 and 17.7%, respectively) [fixed effects: RR = 0.59; 95% CI = (0.41, 0.84); P = 0.003; I2 = 0.0%, Fig. 3C]. There was no perioperative mortality in patients treated with non-intubated VATS under loco-regional anaesthesia, whereas the perioperative mortality rate for patients treated with intubated VATS under general anaesthesia was 2.3%.
Overall analysis
We performed a combined meta-analysis of RCTs and observational studies to get the overall feasibility and safety profiles of non-intubated VATS under loco-regional anaesthesia for thoracic surgery. Seven studies reported global in-operating room time. Patients obtained significantly shorter global in-operating room time with non-intubated VATS under loco-regional anaesthesia than with intubated VATS under general anaesthesia [random effects: WMD = −41.96; 95% CI = (−57.26, −26.67); P < 0.001; I2 = 94.9%, Fig. 3A]. Nine studies reported detailed data about hospital stays. Patients treated with non-intubated VATS under loco-regional anaesthesia had significantly shorter hospital stays than patients treated with intubated VATS under general anaesthesia [fixed effects: WMD = −1.24; 95% CI = (−1.46, −1.02); P < 0.001; I2 = 33.7%, Fig. 3B].
The rate of postoperative complications could be obtained from nine studies. Overall analysis of postoperative complications showed that non-intubated VATS under loco-regional anaesthesia achieved a significantly lower rate of postoperative complications than intubated VATS under general anaesthesia (8.8 and 16.7%, respectively) [fixed effects: RR = 0.55; 95% CI = (0.40, 0.74); P < 0.001; I2 = 0.0%, Fig. 3C]. In addition, there was no perioperative mortality in patients treated with non-intubated VATS under loco-regional anaesthesia, whereas patients treated with intubated VATS under general anaesthesia had a perioperative mortality rate of 1.4%.
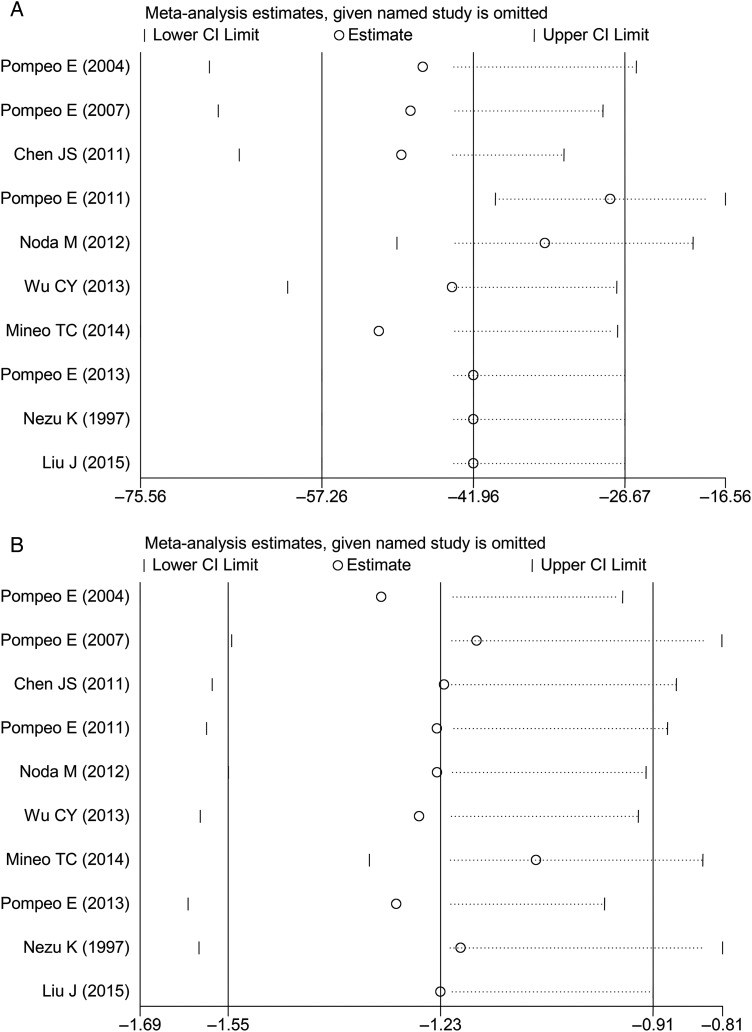
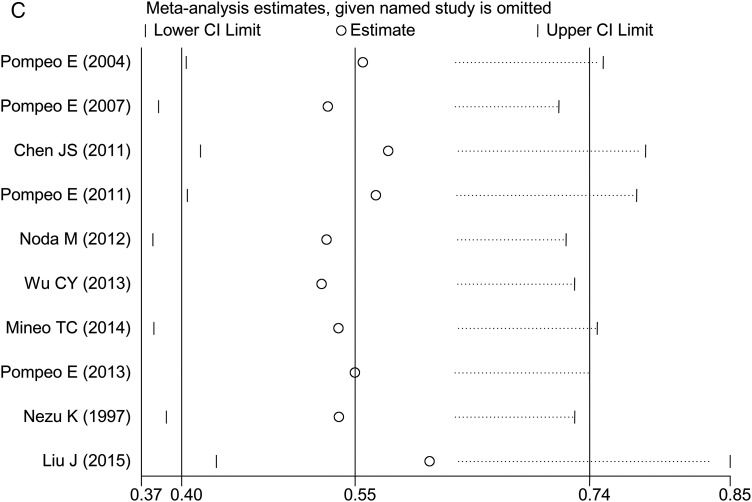
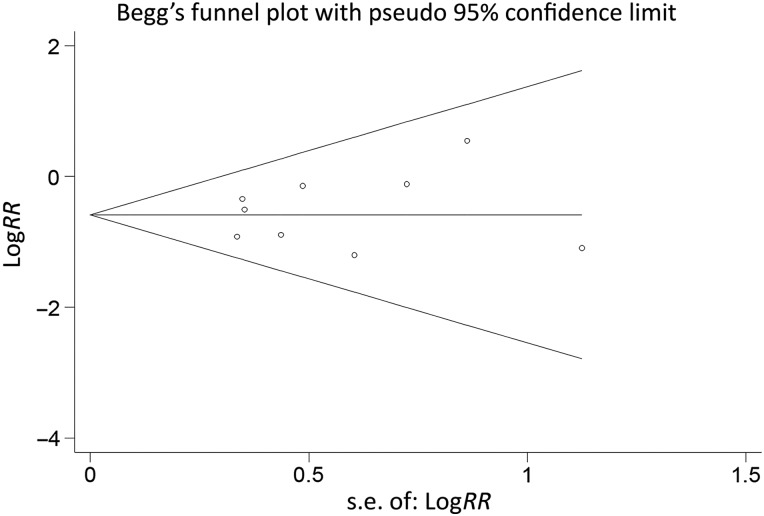
Sensitivity analysis and publication bias
We conducted the sensitivity analysis by sequential removal of each study based on overall analysis to evaluate the stability of our overall results. Sensitivity analysis showed that this method did not change the outcomes of primary overall analysis (Fig. 4). Publication bias was tested by Begg's test and Egger's test, which suggested no publication bias, with symmetrical appearance on funnel plot based on the analysis of postoperative complications (Begg's test: P = 0.446; Egger's test: P = 0.610, Fig. 5).
Figure 4:
Sensitivity analysis for (A) global in-operating room time, (B) hospital stays and (C) complications. CI: confidence interval.
Figure 5:
Funnel plot of the included studies for overall analysis of postoperative complications (Begg's test: P = 0.446; Egger's test: P = 0.610).
DISCUSSION
With the concept of minimal invasiveness in thoracic surgery, VATS has become a globally accepted alternative to thoracotomy for the surgical treatment of patients with various thoracic conditions involving lung, pleura and mediastinum [2]. Recently, as a less invasive surgical technique, non-intubated VATS under loco-regional anaesthesia has gained increasing widespread attention globally. Excellent outcomes of non-intubated VATS under loco-regional anaesthesia were not only reported in some case reports [21], but also in some RCTs with a small sample size [15, 16].
However, as mentioned above, the currently available studies about non-intubated VATS under loco-regional anaesthesia were all carried out in a small sample size, which lack strong evidence to elucidate its actual feasibility and safety for thoracic surgery. Therefore, we conducted this meta-analysis aiming to establish the short-term feasibility and safety profile of non-intubated VATS under loco-regional anaesthesia for thoracic surgery. We conducted not only a meta-analysis for overall results (combination of RCTs and observational studies), but also two subgroup analyses based on study design. Although there are some differences between RCTs and observational studies, integration of results from both types of studies may improve the inference based on only RCTs and enable us to generate the most comprehensive summary of the evidence available to date [22], especially for our meta-analysis with a limited number of RCTs and small sample size.
Our meta-analysis suggested that non-intubated VATS under loco-regional anaesthesia exhibited good effects in improving the short-term outcomes of patients and yielded significantly shorter in-operating room time and hospital stays, as well as a significantly lower rate of postoperative complications than intubated VATS under general anaesthesia. Moreover, non-intubated VATS under loco-regional anaesthesia was generally safe, as no perioperative mortality was observed in our analysis. To the best of our knowledge, the present study is the first meta-analysis to evaluate the general short-term feasibility and safety of non-intubated VATS under loco-regional anaesthesia for thoracic surgery.
Non-intubated VATS under loco-regional anaesthesia entails thoracoscopic procedures performed with regional or local anaesthesia in mildly sedated or fully awake patients with spontaneous ventilation, which can avoid intubation-related complications and the adverse effects of general anaesthesia. All of these benefits could contribute to the excellent outcomes of non-intubated VATS under loco-regional anaesthesia for thoracic surgery, when compared with intubated VATS under general anaesthesia. Pompeo et al. [15] and Wu et al. [19] both found that non-intubated VATS under loco-regional anaesthesia achieved a shorter anaesthesia time, due to the benefit that tracheal intubation and subsequent bronchoscopic examination were not required in non-intubated VATS under loco-regional anaesthesia, which may account for shorter global in-operating room time. Preliminary studies showed that a decreased level of inflammatory cytokines (tumor necrosis factor-α and C-reactive protein) [9], and less impairment in lymphocyte activity [23], as well as attenuated stress response, was related to non-intubated VATS under loco-regional anaesthesia when compared with intubated VATS under general anaesthesia [24]. This may explain why patients treated with non-intubated VATS under loco-regional anaesthesia achieved fewer postoperative complications and shorter hospital stays than those treated with intubated VATS under general anaesthesia. No perioperative mortality was observed in patients treated with non-intubated VATS under loco-regional anaesthesia in our analysis, which may be related to the strict inclusion and exclusion criteria for the patients in each study and the reduced invasiveness of non-intubated VATS under loco-regional anaesthesia. Therefore, all the aforementioned evidence proved that non-intubated VATS under loco-regional anaesthesia was feasible and safe for thoracic surgery.
Nevertheless, our meta-analysis had several limitations. Firstly, an important limitation was that our overall analysis included both RCTs and observational studies, which may weaken the strength of our overall results. As we already know, randomized and non-randomized studies were often found to yield different results in systematic reviews [25]. However, in our meta-analysis, both analysis of RCTs and observational studies have obtained the same significant outcomes as overall analysis, which may strengthen confidence in the validity of our results. Secondly, in our meta-analysis, heterogeneity was found during the analysis of global in-operating room time among the included studies and, therefore, a random-effects model was used, which could weaken our analytical power. One explanation for this heterogeneity is that the thoracic surgery in our analysis actually consisted of various surgical procedures such as thoracoscopic talc pleurodesis, lung volume reduction surgery and pulmonary wedge resection. All of these different surgeries required different procedures, operating times and postoperative recovery times, which could cause heterogeneity during the analysis of global in-operating room times. In addition, varying study design (RCT and observational study) could also add to the heterogeneity among these studies. Thirdly, although no publication bias was found in our study, the limited number of trials with a small sample size in our meta-analysis could also affect the analytical power. Moreover, a potential risk of bias such as performance and detection bias was found within the RCTs. Therefore, there is a strong need to carry out more RCTs of high quality and large sample size to confirm and update our results.
Although our present meta-analysis provided evidence supporting the application of non-intubated VATS under loco-regional anaesthesia for thoracic surgery because of its excellent short-term benefits for patients, there are still several implications that need to be addressed for further researches. Firstly, for the safety of patients treated with non-intubated VATS under loco-regional anaesthesia, further studies about its definite indications and contraindications are needed. Secondly, there were still occasions where a small percentage of patients treated with non-intubated VATS under loco-regional anaesthesia required conversion to general anaesthesia with intubation due to extensive pleural adhesion or persistent hypoxia or bleeding requiring thoracotomy [15, 17]. Therefore, the criteria for conversion of loco-regional anaesthesia without intubation to general anaesthesia with intubation need to be established. Finally, the long-term outcomes of non-intubated VATS under loco-regional anaesthesia are still unavailable. Therefore, more evidence is needed to confirm the long-term efficacy of non-intubated VATS under loco-regional anaesthesia for thoracic surgery before it is widely accepted and utilized.
CONCLUSIONS
This meta-analysis aiming to establish the general feasibility and safety profile of non-intubated VATS under loco-regional anaesthesia for thoracic surgery confirmed the short-term benefits for patients. However, the long-term efficacy of non-intubated VATS under loco-regional anaesthesia is still unknown. Multicentre, well-designed RCTs with longer follow-up are needed to confirm and update our findings, as well as the long-term efficacy of non-intubated VATS under loco-regional anaesthesia for thoracic surgery.
ACKNOWLEDGEMENTS
We thank Liu Jin (Department of Anesthesiology, West China Hospital, Sichuan University) for the good advice on anaesthesia.
Conflict of interest: none declared.
REFERENCES
- 1.Shah RD, D'Amico TA. Modern impact of video assisted thoracic surgery. J Thorac Dis 2014;6:S631–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hung MH, Hsu HH, Cheng YJ, Chen JS. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Bonome C, Fieira E, Aymerich H, Fernandez R, Delgado M et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721–31. [DOI] [PubMed] [Google Scholar]
- 4.Sugasawa Y, Yamaguchi K, Kumakura S, Murakami T, Kugimiya T, Suzuki K et al. The effect of one-lung ventilation upon pulmonary inflammatory responses during lung resection. J Anesth 2011;25:170–7. [DOI] [PubMed] [Google Scholar]
- 5.Pompeo E. Nonintubated video-assisted thoracic surgery under epidural anesthesia—encouraging early results encourage randomized trials. Chin J Cancer Res 2014;26:364–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nezu K, Kushibe K, Tojo T, Takahama M, Kitamura S. Thoracoscopic wedge resection of blebs under local anesthesia with sedation for treatment of a spontaneous pneumothorax. Chest 1997;111:230–5. [DOI] [PubMed] [Google Scholar]
- 7.Mineo TC, Tacconi F. From “awake” to “monitored anesthesia care” thoracic surgery: a 15 year evolution. Thorac Cancer 2014;5:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hausman MS Jr, Jewell ES, Engoren M. Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg 2015;120:1405–12. [DOI] [PubMed] [Google Scholar]
- 9.Liu J, Cui F, Li S, Chen H, Shao W, Liang L et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123–30. [DOI] [PubMed] [Google Scholar]
- 10.Pompeo E, Tacconi F, Mineo TC. Comparative results of non-resectional lung volume reduction performed by awake or non-awake anesthesia. Eur J Cardiothorac Surg 2011;39:e51–8. [DOI] [PubMed] [Google Scholar]
- 11.Mukaida T, Andou A, Date H, Aoe M, Shimizu N. Thoracoscopic operation for secondary pneumothorax under local and epidural anesthesia in high-risk patients. Ann Thorac Surg 1998;65:924–6. [DOI] [PubMed] [Google Scholar]
- 12.Pompeo E, Tacconi F, Mineo D, Mineo TC. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786–90. [DOI] [PubMed] [Google Scholar]
- 13.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. www.ohri.ca/programs/clinical_epidemiology/oxford.asp (15 September 2015, date last accessed).
- 14.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pompeo E, Mineo D, Rogliani P, Sabato AF, Mineo TC. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761–8. [DOI] [PubMed] [Google Scholar]
- 16.Pompeo E, Dauri M. Is there any benefit in using awake anesthesia with thoracic epidural in thoracoscopic talc pleurodesis? J Thorac Cardiovasc Surg 2013;146:495–7.e1. [DOI] [PubMed] [Google Scholar]
- 17.Chen JS, Cheng YJ, Hung MH, Tseng YD, Chen KC, Lee YC. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038–43. [DOI] [PubMed] [Google Scholar]
- 18.Noda M, Okada Y, Maeda S, Sado T, Sakurada A, Hoshikawa Y et al. Is there a benefit of awake thoracoscopic surgery in patients with secondary spontaneous pneumothorax? J Thorac Cardiovasc Surg 2012;143:613–6. [DOI] [PubMed] [Google Scholar]
- 19.Wu CY, Chen JS, Lin YS, Tsai TM, Hung MH, Chan KC et al. Feasibility and safety of nonintubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg 2013;95:405–11. [DOI] [PubMed] [Google Scholar]
- 20.Mineo TC, Sellitri F, Tacconi F, Ambrogi V. Quality of life and outcomes after nonintubated versus intubated video-thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med 2014;17:761–8. [DOI] [PubMed] [Google Scholar]
- 21.Bayram S, Tezel C, Cesur E, Kanbur S, Kiral H, Urek S. The feasibility of awake thoracic epidural anesthesia in patients requiring VATS wedge resection. Eur Respir J 2013;42 Accessed at http://ovidsp.tx.ovid.com/sp-3.18.0b/ovidweb.cgi?&S=LOJNFPIBPDDDBDNFNCJKNGOBIEPKAA00&Abstract=S.sh.26%7c1%7c1. [Google Scholar]
- 22.Shrier I, Boivin JF, Steele RJ, Platt RW, Furlan A, Kakuma R et al. Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles. Am J Epidemiol 2007;166:1203–9. [DOI] [PubMed] [Google Scholar]
- 23.Vanni G, Tacconi F, Sellitri F, Ambrogi V, Mineo TC, Pompeo E. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973–8. [DOI] [PubMed] [Google Scholar]
- 24.Tacconi F, Pompeo E, Sellitri F, Mineo TC. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact CardioVasc Thorac Surg 2010;10:666–71. [DOI] [PubMed] [Google Scholar]
- 25.Kunz R, Oxman AD. The unpredictability paradox: review of empirical comparisons of randomised and non-randomised clinical trials. BMJ 1998;317:1185–90. [DOI] [PMC free article] [PubMed] [Google Scholar]