Abstract
OBJECTIVES
This study assesses quality of life in relation to prosthetic aortic valve selection and preferences for shared decision-making among non-elderly adult patients after aortic valve replacement (AVR).
METHODS
A single-centre consecutive cohort of 497 AVR patients who underwent AVR between the age of 18 and 60 years was cross-sectionally surveyed 1–10 years after AVR. Health-related quality of life (Short-Form Health Survey, SF-36), valve-specific quality of life, patient experience with and preferences for involvement and final decision in prosthetic valve selection were investigated.
RESULTS
Two-hundred and forty patients (48%) responded. The median age was 57 years (range 26–70). Compared with the general age-matched Dutch population, AVR patients reported worse physical health, but better mental health. Biological valve recipients reported lower general health than mechanical valve recipients. Mechanical valve recipients had more doubts about the decision to undergo surgery, were more bothered by valve sound, the frequency of doctor visits and blood tests, and possible bleeding, but were less afraid of a possible reoperation. Eighty-nine percent were of the opinion that it is important to be involved in prosthetic valve selection, whereas 64% agreed that they actually had been involved. A better patient experience with involvement in prosthetic valve selection was associated with better mental health (P = 0.036).
CONCLUSIONS
Given the observed suboptimal patient involvement in prosthetic valve selection, the broad patient support for shared decision-making, and the positive association between patient involvement in prosthetic valve selection and mental health, tools to support shared decision-making would be useful in the setting of heart valve replacement.
Keywords: Quality of life, Aortic valve replacement, Shared decision-making
INTRODUCTION
For non-elderly adult patients who require aortic valve replacement (AVR), two types of valve substitutes are available: mechanical and biological valves. Mechanical valves are designed to last a lifetime but require lifelong anticoagulation due to their increased thrombogenicity, resulting in an increased bleeding risk and an increased risk of complications during pregnancy. Additionally, patients may notice the typical mechanical valve closing sound. Biological valves do not require long-term anticoagulation, unless another indication is present. However, they are subject to valve deterioration over time, and in particular younger patients may require one or more reoperations later in life.
Additionally, valve repair is now becoming available for younger patients with aortic regurgitation, and is currently being evaluated [1]. Aortic valve repair is showing promise for use in younger patients, but more long-term information is needed.
Several factors play a role in the selection of a prosthetic valve type for AVR, such as patient age, life expectancy, valve durability, haemodynamic properties, surgical risk and (contra) indications for anticoagulation use. Furthermore, for non-elderly adult patients, factors like an active lifestyle or a pregnancy wish should be taken into consideration. Given the different nature of mechanical versus biological prosthetic valve-related risks and benefits, the 2014 ACC/AHA Valvular Heart Disease Guidelines state that the choice of a prosthetic valve type should be a shared decision process, whereas the 2012 ESC/EACTS guidelines highlight the importance of considering informed patient preferences in prosthetic valve selection (Class 1 indication) [2, 3].
Particularly younger patients who require AVR are facing a difficult choice given their long life expectancy and active lifestyle. Prosthetic valve type may influence the quality of life of patients although there is no consensus in the literature [4–7]. In this light, we cross-sectionally investigated the quality of life in patients after AVR, who were between the age of 18 and 60 years at the time of AVR in our institution. Since it has been shown in cancer decision-making research that patient participation in clinical decision-making may improve the quality of life [8], we additionally investigated patient experience with involvement in prosthetic valve selection and preferences for involvement and final decision in prosthetic valve selection in relation to observed quality of life.
MATERIALS AND METHODS
This study was approved by the institutional review board (Erasmus MC MEC no. 2012-163) and written informed consent was obtained from all participants. Between 1 January 2001 and 3 December 2011, a total of 583 consecutive patients between the age of 18 and 60 underwent AVR in our institution. The civil status of all patients was checked through the civil registry. Patients who were alive at the time of the study with an available postal address (N = 497; 85%) were approached by mail and requested to complete and return a postal questionnaire.
Information on patient characteristics, perioperative clinical and procedural characteristics as well as events during follow-up [gender, date of birth, preoperative NYHA class, date of surgery, urgency of surgery, concomitant procedures, reoperation and valve-related events (structural valve deterioration, non-structural dysfunction, valve thrombosis, embolism, bleeding event and endocarditis)] was collected from hospital records.
The questionnaire consisted of questions about educational level, NYHA class, health-related quality of life, valve-specific quality of life, patient experience with involvement in prosthetic valve selection and preferences for involvement and final decision in prosthetic valve selection.
Educational level and NYHA class were assessed with multiple choice questions.
Health-related quality of life was assessed with the Dutch version of the Short-Form Health Survey (SF-36) [9, 10]. This questionnaire consists of 36 health-related questions, grouped into eight domains: physical functioning, role limitations because of physical health problems, bodily pain, general health perceptions, vitality, social functioning, role limitations because of emotional problems and general mental health. The Physical Component Scale (PCS) is a summary scale consisting of the physical functioning, physical role functioning, bodily pain and general health scales. The Mental Component Scale (MCS) is a summary scale composed of vitality, social functioning, emotional role functioning and mental health indexes. Scale scores are obtained by summing the items together within a domain, dividing this outcome by the range of scores and then transforming the scores to a scale from 0 to 100. The mean score of the PCS and MCS is 50 with a standard deviation of 10. A higher score represents a better health status [11].To compare quality of life between the study patients and the general Dutch population, the results of the MORGEN study were used [12]. Valve-specific quality of life was assessed with seven valve-specific questions [5].
Patient experience with involvement in prosthetic valve selection and their preferences for involvement and final decision in prosthetic valve selection were assessed with multiple choice questions and a Control Preferences Scale [13, 14]. For a detailed description, see Supplementary Material 1.
Statistical methods
Continuous variables were displayed by the mean and standard deviation if normally distributed and by the median and range if there was no normal distribution. The distribution of the continuous variables was tested using the Kolmogorov–Smirnov test. Group comparison was done using the unpaired t-test or the Mann–Whitney U-test in case of ordinal data or no normal distribution.
Categorical variables were displayed as counts and percentages. Group comparison was done using the χ2 test or the Fisher's exact test where appropriate.
The one-sample t-test was used to compare health-related quality of life between the study population and the general Dutch population.
A general linear model (GLM) with bootstrap method was used to assess the association between time since surgery and: (i) health-related quality of life, (ii) patient experience with involvement in prosthetic valve selection and (iii) their preferences for involvement and final decision in prosthetic valve selection.
The same method (GLM with bootstrap) was used to assess the association between health-related quality of life and: (i) patient experience with involvement in prosthetic valve selection and (ii) their preferences for involvement and final decision in prosthetic valve selection [15].
All tests were two-sided, and a P-value of 0.05 or lower was considered statistically significant. All statistical analyses were performed using IBM-SPSS 20 (IBM Corp., Armonk, NY, USA).
RESULTS
In total, 240 patients (48%) returned the questionnaire. These patients received the following types of aortic valves prostheses: 190 mechanical valves, 26 bioprostheses, 19 allografts and 3 autografts. Two patients underwent an aortic valve repair. Bioprostheses, allografts, autografts and aortic valve repair were combined to one group called ‘biological valves’ for further analyses.
Perioperative clinical and procedural characteristics are presented in Table 1. Patient characteristics at the time of the questionnaire are presented in Table 2. For a detailed description of the patient characteristics by biological valve type, see Supplementary Material 2. The 240 patients who returned the questionnaire were older compared with non-responding patients [median age: 57 (range 26–70) vs 54 (range 19–71) years, respectively; P = 0.003] and more often males (73 vs 62%, respectively; P = 0.005). Five percent of the participating patients underwent a reoperation after their primary AVR, and 6% experienced a valve-related event (2 paravalvular leak, 2 embolism, 4 bleeding and 6 endocarditis), with no difference between mechanical and biological valve recipients.
Table 1:
Perioperative clinical and procedural characteristics
| All (N = 240) | Mechanical (N = 190) | Biological (N = 50) | |
|---|---|---|---|
| Preoperative NYHA class, n (%)a | |||
| I | 70 (30) | 54 (30) | 16 (32) |
| II | 94 (41) | 73 (40) | 21 (42) |
| III | 52 (23) | 41 (23) | 11 (22) |
| IV | 15 (7) | 13 (7) | 2 (4) |
| Emergency surgery, n (%) | |||
| Yes | 34 (14) | 27 (14) | 7 (14) |
| No | 206 (86) | 163 (86) | 43 (86) |
| Concomitant procedures, n (%)b | |||
| Yes | 109 (45) | 79 (42) | 30 (60) |
| No | 131 (55) | 111 (58) | 20 (40) |
n = 231.
P < 0.05 mechanical valves versus biological valves.
Table 2:
Patient characteristics at the time of the questionnaire
| All (N = 240) | Mechanical (N = 190) | Biological (N = 50) | |
|---|---|---|---|
| Males, n (%) | 177 (73) | 141 (73) | 36 (72) |
| Age (years)a | 57 (26–70) | 57 (26–70) | 58 (27–69) |
| Educational level, n (%)b,c | |||
| Less than high school | 41 (17) | 37 (20) | 4 (8) |
| High school graduate | 112 (48) | 91 (49) | 21 (44) |
| College graduate | 69 (29) | 48 (26) | 21 (44) |
| Other | 13 (6) | 11 (6) | 2 (4) |
| Time since surgery (years)a,c | 7 (0–11) | 6 (0–11) | 10 (0–11) |
| NYHA class, n (%)d | |||
| I | 145 (61) | 117 (63) | 28 (57) |
| II | 66 (28) | 53 (28) | 13 (27) |
| III | 21 (9) | 14 (7) | 7 (14) |
| IV | 4 (2) | 3 (2) | 1 (2) |
Values are median (range).
n = 235.
P < 0.05 mechanical valves versus biological valves.
n = 236.
Health-related quality of life is presented in Table 3. Compared with the general age-matched Dutch population, AVR patients scored lower on the PCS (P < 0.001), but higher on the MCS (P < 0.001). A longer period from surgery was associated with a higher MCS (P = 0.037). Other patient characteristics, perioperative clinical and procedural characteristics and follow-up events were not associated with quality of life. The results of the valve-specific questionnaire are presented in Table 4.
Table 3:
Health-related quality of life (SF-36)a
| All (N = 240) | Mechanical (N = 190) | Biological (N = 50) | |
|---|---|---|---|
| Physical functioning | 49 ± 10 | 49 ± 10 | 49 ± 11 |
| Role-physical | 47 ± 15 | 47 ± 15 | 43 ± 16 |
| Bodily pain | 54 ± 10 | 54 ± 9 | 54 ± 10 |
| General healthb | 47 ± 11 | 48 ± 11 | 44 ± 12 |
| Vitality | 54 ± 10 | 55 ± 10 | 53 ± 10 |
| Social functioning | 50 ± 10 | 51 ± 9 | 48 ± 11 |
| Role-emotional | 49 ± 15 | 49 ± 14 | 48 ± 15 |
| Mental health | 53 ± 10 | 53 ± 10 | 52 ± 10 |
| PCS | 48 ± 10 | 48 ± 9 | 46 ± 12 |
| MCS | 53 ± 10 | 53 ± 10 | 52 ± 10 |
MCS: Mental Component Scale; PCS: Physical Component Scale.
Values are mean ± SD.
P < 0.05 mechanical valves versus biological valves.
Table 4:
Valve-specific quality of life
| All (N = 240) | Mechanical (N = 190) | Biological (N = 50) | |
|---|---|---|---|
| If I had to do it over again, would I make the same decision to have surgery?a | |||
| Yes | 71% | 67% | 84% |
| Probably | 20% | 23% | 8% |
| I don't know | 6% | 8% | 2% |
| Probably not | 1% | 1% | 2% |
| No | 2% | 2% | 4% |
| Is there a valve sound that bothers me?a | |||
| Never | 44% | 35% | 80% |
| Rarely | 18% | 21% | 8% |
| Occasionally | 26% | 30% | 8% |
| Frequently | 6% | 6% | 2% |
| Always | 7% | 8% | 2% |
| Following my valve surgery, the frequency of doctor visits and blood tests bothers me.a | |||
| Never | 49% | 46% | 61% |
| Rarely | 16% | 15% | 18% |
| Occasionally | 27% | 30% | 12% |
| Frequently | 4% | 5% | |
| Always | 4% | 3% | 8% |
| The possibility of complications due to my implanted valve concerns me. | |||
| Never | 43% | 44% | 39% |
| Rarely | 28% | 29% | 25% |
| Occasionally | 24% | 21% | 35% |
| Frequently | 3% | 3% | 2% |
| Always | 3% | 3% | – |
| I am concerned about possible bleeding caused by my anticoagulant medication.a | |||
| Never | 39% | 31% | 67% |
| Rarely | 25% | 27% | 14% |
| Occasionally | 28% | 31% | 16% |
| Frequently | 6% | 7% | – |
| Always | 3% | 3% | 2% |
| I am afraid that my valve may fail. | |||
| Never | 57% | 59% | 49% |
| Rarely | 23% | 22% | 27% |
| Occasionally | 17% | 15% | 25% |
| Frequently | 2% | 2% | – |
| Always | 1% | 2% | – |
| I am afraid that I may need another valve operation.a | |||
| Never | 45% | 48% | 33% |
| Rarely | 27% | 28% | 23% |
| Occasionally | 22% | 21% | 27% |
| Frequently | 3% | 2% | 6% |
| Always | 4% | 2% | 10% |
aP < 0.05 mechanical valves versus biological valves.
Patient experience with involvement in prosthetic valve selection is presented in Table 5. There was no association between time since surgery and patient experience with involvement in prosthetic valve selection.
Table 5:
Patient experience with involvement in prosthetic valve selection
| All (N = 240) | Mechanical (N = 190) | Biological (N = 50) | |
|---|---|---|---|
| Do you know there are different prosthetic valve types? | |||
| Yes | 93% | 92% | 96% |
| No | 7% | 8% | 4% |
| The doctor has involved me in prosthetic valve selection. | |||
| (Totally) agree | 64% | 62% | 74% |
| Not agree/disagree | 8% | 9% | 4% |
| (Totally) disagree | 21% | 23% | 14% |
| Not applicable | 17% | 7% | 8% |
| I know the risks and benefits of different prosthetic valve types. | |||
| (Totally) agree | 73% | 70% | 82% |
| Not agree/disagree | 8% | 8% | 4% |
| (Totally) disagree | 16% | 18% | 10% |
| Not applicable | 4% | 4% | 4% |
| I have received enough information to make a deliberate choice. | |||
| (Totally) agree | 60% | 59% | 62% |
| Not agree/disagree | 11% | 11% | 12% |
| (Totally) disagree | 21% | 22% | 16% |
| Not applicable | 9% | 9% | 10% |
| I think it is important to be involved in prosthetic valve selection.a | |||
| (Totally) agree | 89% | 87% | 96% |
| Not agree/disagree | 9% | 10% | 4% |
| (Totally) disagree | 2% | 3% | – |
| I am satisfied with my prosthetic aortic valve. | |||
| (Totally) agree | 89% | 89% | 92% |
| Not agree/disagree | 8% | 9% | 6% |
| (Totally) disagree | 3% | 3% | 2% |
aP < 0.01 mechanical valves versus biological valves.
Patient preference for final decision in prosthetic aortic valve selection is presented in Fig. 1. There was no association between time since surgery and patient preferences for involvement and final decision in prosthetic valve selection.
Figure 1:
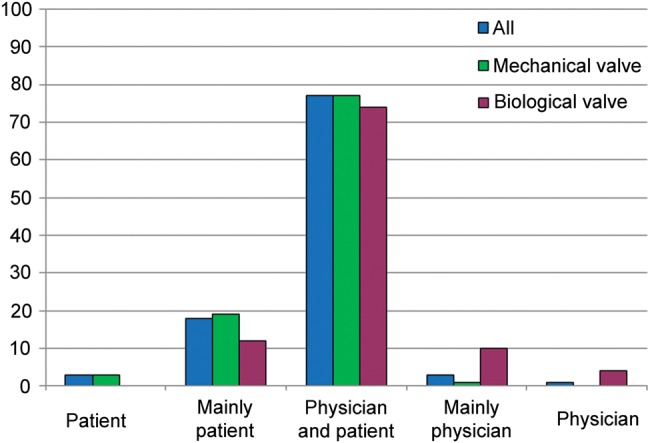
Displays patient preference for final decision in prosthetic aortic valve choice. Differences between mechanical and biological valves (P < 0.01).
A better patient experience with involvement in prosthetic valve selection was associated with a higher MCS (P = 0.036). Patient preferences for involvement and final decision in prosthetic valve selection were not associated with health-related quality of life.
DISCUSSION
Non-elderly adult patients who require AVR are facing a complex choice with regard to the type of valve prosthesis. Factors such as potential desire to become pregnant, lifestyle and occupation, cultural and social factors, other cardiac issues or multiple prior operations need consideration in the selection of a prosthetic valve [16]. Because prosthetic valve selection is a value-sensitive decision that may have a great impact on quality of life, informed patient preferences should be carefully considered in a shared decision-making process [2, 3].
This cross-sectional study shows that in particular, mental health is good in non-elderly adult AVR patients, while physical health is worse compared with the general Dutch population. As expected, valve-specific quality of life differs considerably between mechanical and biological valve recipients, and is driven by valve type-specific limitations.
This study also highlights that there is ample room for improvement in the quality of decision-making in the setting of prosthetic aortic valve selection: 9 of 10 patients find it important to be involved in prosthetic valve selection, but only two-third of patients actually feel involved, only 40% of patients feel that they received insufficient information, and importantly: patient involvement is associated with better mental health.
The present study shows that non-elderly adult AVR patients have a good perceived quality of life. This is consistent with previous studies in young adults after valve replacement [17] and surgical correction for congenital heart disease [18, 19]. Compared with the general Dutch population, non-elderly adult AVR patients experience worse physical health, but better mental health. One might hypothesize that AVR patients experience better mental health than the general Dutch population due to the phenomenon of response shift: patients have different internal standards and values after a life-threatening experience, such as cardiac surgery [18, 20]. The results of this study show that a longer period from surgery seems to be associated with better mental health. This may be due to the fact that patients get used to their life with a prosthetic valve, and accept the limitations. In the literature, there is no consensus about whether prosthetic valve type influences quality of life [4–7]. In our study, biological valve recipients have more impairments in subjective general health than mechanical valve recipients. The reason for this difference remains to be elucidated. It may be that the observed longer time since surgery and the increased anxiety regarding the prospect of another valve operation among biological valve recipients play a role.
The valve-specific questionnaire reveals that patients with a mechanical valve have in retrospect more doubts about the decision to undergo surgery and are more disturbed by valve sound and the frequency of doctor visits and blood tests, and more concerned about bleeding. These differences can be explained by the different nature of mechanical versus biological prosthetic valve-related risks and benefits. Surprisingly, 12% of biological valve recipients are disturbed by valve sound. A previous study, reporting that 8% (n = 125) of patients with an aortic valve repair or autograft implantation were bothered by valve sound, hypothesizes that patients possibly exhibit a high degree of attention to their heart function [5]. In our study, 19% of mechanical valve recipients are afraid of valve failure and as much as 25% are afraid that they may need another valve operation. Mechanical valves are designed to last a lifetime and the risk of a reoperation after mechanical valve implantation is much lower but not absent compared with biological valves, so it is remarkable that a considerable number of mechanical valve patients are afraid that their valve might fail. Maybe this fear is due to a lack of information or the inability to comprehend the information that was provided at the time of surgery.
In this study, almost one-third of patients are of the opinion that they did not receive enough information to contribute to a deliberate choice. This confirms observations in other studies: patients are often not well informed about the risks and benefits associated with treatments [21, 22]. Well-informed patients are essential for engagement in shared decision-making. Only when patients understand the risks and benefits associated with the different treatment options, can they weigh these risks and benefits in their own context and contribute to a deliberate choice. In this respect, there seems to be room for improvement in the information transfer to patients who face AVR. It is known that shared decision-making improves patient understanding of the available treatment options, increases the proportion of patients with realistic expectations of risks and benefits, stimulates patient involvement in decision-making and improves agreement between patient values and treatment choices [23]. In the field of heart valve disease, current clinical practice guidelines advocate shared decision-making in prosthetic valve selection [2, 3]. Despite that, the application of shared decision-making still remains a challenge. The vast majority of patients in the current study are of the opinion that it is important to be involved in prosthetic valve selection, whereas one-third of patients do not feel involved in the decision-making process. This finding is in line with previous research, showing that shared decision-making is not often applied in daily clinical practice in a variety of medical conditions [21, 22], and calls for tools for clinicians and patients to engage in shared decision-making in their routine practice. The use of a decision aid to support shared decision-making may be particularly useful in this setting. A decision aid improves the decision-making process by increasing knowledge, improving risk communication, reducing decisional conflict, increasing participation and increasing the chance that a patient receives care that is in line with their personal values [23]. Perhaps frequently, a clinician will bias the presentation of the treatment options according to his or her opinion or ‘favourite’ procedure. A decision aid encourages a clinician to present in a scientifically unbiased manner.
Of course, preferences for involvement in prosthetic valve selection may vary among patients. Biological valve recipients in this study tend towards an active patient role than mechanical valve recipients. This difference may be due to the fact that biological valve recipients in this study are higher educated than mechanical valve recipients as it is known that more educated patients often prefer a more active patient role than patients with a lower education [24]. Even if patients prefer a passive role in decision-making, they should at least be informed about the pros and cons of the different treatment options. Providing patients with information, for example through a decision aid, also stimulates them to take a more active role in decision-making [23].
Patient participation in cancer decision-making may improve quality of life [8], and the present study also shows that perceived involvement in prosthetic valve selection is associated with better mental health. From cancer research, it is known that making decisions regarding healthcare is important for patients and patients prefer to have some control [25]. In the setting of prosthetic valve selection, a lack of patient involvement may cause uncertainty which may have a negative impact on patient well-being.
In this study, standard aortic valve procedures were primarily investigated because longer follow-up times were available. But of course, other options, such as aortic valve repair, are gaining interest and reportedly have good intermediate-term results, including quality-of-life outcomes [1, 5].
Study limitations
This is a single-centre study that represents clinical practice in a university hospital in the Netherlands. Questionnaires were completed 1–10 years after AVR. Due to this wide time range, the accuracy and completeness of the answers may have been influenced by recall bias. Also, the wide time range ignores the fact that there may be temporal trends in quality of life—as was found to be significant for MCS—and patient experience with decision-making. Selection bias may have occurred, because only 48% of the total population responded and responding patients were older and more often male compared with non-responding patients. With regard to patient experience with involvement in prosthetic valve selection, patients had the option to choose ‘not applicable’ in the questionnaire. This term could be misinterpreted by patients since several patients chose the option ‘not applicable’ because their doctor had made the decision with regard to prosthetic valve type. This also applies to the questions about information provision. It is recommended that the option ‘not applicable’ not be added to future questionnaires. We did not ask mechanical valve recipients about their compliance to anticoagulation therapy. Therefore, we were unable to address the possible association between anticoagulation adherence and quality of life and patient experience with decision-making. Due to the observational character of the study, it is possible that other factors may have influenced the association between patient involvement and mental health.
CONCLUSIONS
Non-elderly adult patients after AVR experience impaired physical health but better mental health compared with the general age-matched population, and valve type-specific risks may influence perceived health. Given the observed suboptimal patient involvement in prosthetic valve selection, the broad support among patients for shared decision-making in the setting of prosthetic valve selection, and the positive association between patient involvement and mental health, tools to support shared decision-making may be useful to improve the quality of decision-making.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
ACKNOWLEDGEMENTS
The authors thank all the patients who participated in this study.
Conflict of interest: none declared.
REFERENCES
- 1.de Meester C, Pasquet A, Gerber BL, Vancraeynest D, Noirhomme P, El Khoury G et al. Valve repair improves the outcome of surgery for chronic severe aortic regurgitation: a propensity score analysis. J Thorac Cardiovasc Surg 2014;148:1913–20. [DOI] [PubMed] [Google Scholar]
- 2.Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology, European Association for Cardio-Thoracic Surgery, Vahanian A, Alfieri O, Andreotti F, Antunes MJ et al. Guidelines on the management of valvular heart disease (version 2012). Eur J Cardiothorac Surg 2012;42:S1–44. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP III, Guyton RA et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:e521–643. [DOI] [PubMed] [Google Scholar]
- 4.Notzold A, Huppe M, Schmidtke C, Blomer P, Uhlig T, Sievers HH. Quality of life in aortic valve replacement: pulmonary autografts versus mechanical prostheses. J Am Coll Cardiol 2001;37:1963–6. [DOI] [PubMed] [Google Scholar]
- 5.Aicher D, Holz A, Feldner S, Kollner V, Schafers HJ. Quality of life after aortic valve surgery: replacement versus reconstruction. J Thorac Cardiovasc Surg 2011;142:e19–24. [DOI] [PubMed] [Google Scholar]
- 6.Sedrakyan A, Hebert P, Vaccarino V, Paltiel AD, Elefteriades JA, Mattera J et al. Quality of life after aortic valve replacement with tissue and mechanical implants. J Thorac Cardiovasc Surg 2004;128:266–72. [DOI] [PubMed] [Google Scholar]
- 7.Perchinsky M, Henderson C, Jamieson WR, Anderson WN Jr, Lamy A, Lowe N et al. Quality of life in patients with bioprostheses and mechanical prostheses. Evaluation of cohorts of patients aged 51 to 65 years at implantation. Circulation 1998;98:II81–6. [PubMed] [Google Scholar]
- 8.Atherton PJ, Smith T, Singh JA, Huntington J, Diekmann BB, Huschka M et al. The relation between cancer patient treatment decision-making roles and quality of life. Cancer 2013;119:2342–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 10.Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R et al. Translation, validation, and norming of the Dutch language version of the SF-36 health survey in community and chronic disease populations. J Clin Epidemiol 1998;51:1055–68. [DOI] [PubMed] [Google Scholar]
- 11.Ware JE Jr, Kosinski M, Bjorner JB, Turner DM, Gandek B, Maruish ME. User's Manual for the SF-36v2 TM Health Survey. 2nd edn Lincoln, RI: Quality Metric Incorporated, 2007. [Google Scholar]
- 12.Smit HA, Verschuren WMM, Bueno de Mesquita HB, Seidell JC. Monitoring van Risicofactoren en Gezondheid in Nederland (MORGEN-Project): Doelstellingen en Werkwijze. Bilthoven: RIVM, 1994. [Google Scholar]
- 13.Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Can J Nurs Res 1997;29:21–43. [PubMed] [Google Scholar]
- 14.Pieterse AH, Baas-Thijssen MC, Marijnen CA, Stiggelbout AM. Clinician and cancer patient views on patient participation in treatment decision-making: a quantitative and qualitative exploration. Br J Cancer 2008;99:875–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Efron B, Tibshirani R. An Introduction to the Bootstrap. Monographs on Statistics and Applied Probability. New York: Chapman & Hall, 1993. [Google Scholar]
- 16.Jaquiss RDB. Bioprosthetic aortic valve replacement in the young: a cautionary tale. Circulation 2014;130:7–9. [DOI] [PubMed] [Google Scholar]
- 17.Ruel M, Kulik A, Lam BK, Rubens FD, Hendry PJ, Masters RG et al. Long-term outcomes of valve replacement with modern prostheses in young adults. Eur J Cardiothorac Surg 2005;27:425–33. [DOI] [PubMed] [Google Scholar]
- 18.Opić P, Roos-Hesselink JW, Cuypers JA, Witsenburg M, van den Bosch A, van Domburg RT et al. Psychosocial functioning of adults with congenital heart disease: outcomes of a 30–43 year longitudinal follow-up. Clin Res Cardiol 2015;104:388–400. [DOI] [PubMed] [Google Scholar]
- 19.Mokhles MM, van de Woestijne PC, de Jong PL, Witsenburg M, Roos-Hesselink JW, Takkenberg JJ et al. Clinical outcome and health-related quality of life after right-ventricular-outflow-tract reconstruction with an allograft conduit. Eur J Cardiothorac Surg 2011;40:571–8. [DOI] [PubMed] [Google Scholar]
- 20.Moons P. Quality of Life in Adults with Congenital Heart Disease: Beyond the Quantity of Life. Leuven: P. Moons, 2004. [Google Scholar]
- 21.Hauptman PJ, Chibnall JT, Guild C, Armbrecht ES. Patient perceptions, physician communication, and the implantable cardioverter-defibrillator. JAMA Intern Med 2013;173:571–7. [DOI] [PubMed] [Google Scholar]
- 22.Zikmund-Fisher BJ, Couper MP, Singer E, Ubel PA, Ziniel S, Fowler FJ Jr et al. Deficits and variations in patients' experience with making 9 common medical decisions: the decisions survey. Med Decis Making 2010;30:85S–95S. [DOI] [PubMed] [Google Scholar]
- 23.Stacey D, Légaré F, Col NF, Bennett CL, Barry MJ, Eden KB et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014;1:CD001431. [DOI] [PubMed] [Google Scholar]
- 24.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med 2005;20:531–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Wain G. Breast cancer survivors' supportive care needs 2–10 years after diagnosis. Support Care Cancer 2007;15:515–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


