Abstract
Background
The human papillomavirus (HPV) is the precursor and the single, most important risk factor for cervical cancer. It is also the most commonly sexually transmitted infection in the United States. An estimated 20 million persons are currently infected with the virus, with an estimated 6 million new infections occurring annually and 12,000 new cervical cancer cases and 4,000 cervical cancer deaths annually. The human papillomavirus (HPV) vaccine is thus an especially important preventive measure for racial/ethnic groups who bear an unequal burden of cervical cancer mortality.
Purpose
This study aimed to develop a culturally and linguistically appropriate intervention to educate and empower Latino and Korean Americans to make an informed HPV vaccination decision for their minor children.
Methods
A parent-focused HPV vaccine education DVD was developed through focus groups and cognitive interviews with Latino and Korean Americans parents of children ages 11-17. A randomized controlled efficacy trial was subsequently conducted with 708 Latino and Korean Americans parents to assess knowledge gains, decisional conflict, decision self-efficacy and informed decision-making resulting from viewing the intervention DVD.
Results
Differences between treatment and control groups for pre-post changes in knowledge, informed decision-making and decisional conflict were statistically significant among the parents exposed to the education intervention DVD.
Conclusion
The study demonstrated that a culturally and linguistically appropriate intervention DVD designed to educate parents about the risks and benefits of the HPV vaccine promoted informed decision-making regarding HPV vaccination among at-risk populations.
Keywords: Uterine Cervical Neoplasms, Papillomavirus vaccine, Parents, Vaccination, United States, Ethnic Groups: Hispanic Americans, Korean Americans
Introduction
Human Papillomavirus (HPV) infection is the most common sexually-transmitted disease in the U.S.1 Its DNA is found in 95-100% of cervical cancers and high-risk HPV strains are detected in 99% of cervical cancer cases.2 HPV is thus the precursor and the single most important risk factor for cervical cancer,2,3 which is a leading cause of cancer mortality among U.S. women. An estimated 25 million individuals are currently infected with HPV in the U.S. and an estimated 6.2 million new cases of genital HPV infection are diagnosed annually.4 Nearly three-fourths of those new cases occur among adolescents and young adults, ages 15-24.4-9 In 2014, an estimated 12,900 new cases of invasive cervical cancer were diagnosed in the U.S. and over one-third of them will result in death.10
Although cervical cancer incidence in the U.S. declined by approximately 70% over the past three decades, the most recent age-adjusted national data11 reveal that Latina, African American and several Asian American groups of women have disproportionately higher rates of cervical cancer compared to non-Hispanic whites.12 Latinas have the highest invasive cervical cancer incidence of the major racial and ethnic groups, with an age-adjusted rate of 9.9 per hundred thousand in 2008-2012, compared to 9.2 for black women, 7.1 for non-Hispanic whites and 6.3 for Asian Americans.13 Among Asian Americans and Pacific Islanders,, Korean, Vietnamese and Filipino women are at very high risk for HPV infection.13-17 The advent of the HPV vaccine presents a unique opportunity to advance primary prevention of cervical cancer in those communities at high risk for HPV infection by improving their vaccination rates. It also creates an urgent need for culturally and linguistically appropriate education materials to inform parents’ HPV vaccination decision.
The HPV vaccine was introduced in the U.S. in 2006 by its manufacturers through aggressive, expensive marketing campaigns that overstated the threat of cervical cancer to all adolescents and ignored those populations most at risk for HPV infection.18-20 Despite widespread media exposure, the extant research literature on the HPV vaccine portrays a generally uninformed public with low levels of HPV related awareness and knowledge in all regions of the nation, and lower HPV vaccination rates in several racially and culturally diverse communities who bear disparate cervical cancer morbidity rates.21,22 The intent of this study was to develop a parent-centered intervention that delivered culturally-competent, language-appropriate information tailored to two diverse, at-risk communities: Latino and Korean-American, hereafter called Korean. This article describes the design of an educational DVD that delivers evidence-based information tailored to different cultural and language groups, and (b) an evaluation of the intervention DVD to assess its efficacy in promoting informed decision-making about HPV vaccination by parents.
Intervention Design
Intervention Content
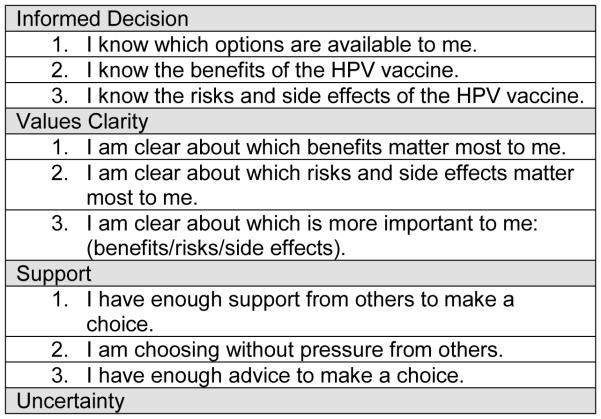
The overarching goal of this health literacy intervention was to develop culturally and linguistically appropriate, evidence-based messages delivered through DVDs to help Latino and Korean parents—two communities at high risk for HPV infection—make an informed decision about HPV vaccination for their 9-17 year old children. As shown in Figure 1, the core content elements of this education intervention addressed: (1) the Human Papillomavirus, (2) the association between HPV infection and cervical cancer, and (3) key aspects of the HPV vaccine. While these core themes were consistent across both racial/ethnic communities, the intervention messages were tailored to the cultural and language attributes of each group as guided by formative research conducted to identify their unique and specific information needs, concerns and preferences. The use of DVDs as the appropriate medium for delivery of the intervention was predicated on the ubiquity of DVD players in the U.S., which enhances intervention reach. DVDs also permit viewing privacy in one’s home at a convenient time chosen by parents themselves, as well as self-directed navigation of the content in their preferred language.
Figure 1.
Intervention Design
Formative Research
Development of the intervention was guided by formative research. Focus groups were conducted to explore knowledge, attitudes and practice pertiment to the HPV vaccine and thus identify parents’ information needs that guide the design of intervention messages responsive to parents’ needs, concerns and preferences. Cognitive interviews were conducted to calibrate and enhance the comprehension of those messages by parents. Recruitment and data collection protocols for this formative research were approved by an Institutional Review Board. The research was conducted in collaboration with community-based organizations: Mexican American Community Services Agency in San Jose, CA for Latino parents and the Korean Health Education, Information and Research center in the Koreatown district of Los Angeles, CA for Korean parents. The formative research sessions were recorded with participant consent and transcribed for subsequent analysis.
Focus Groups
A total of 42 Latino and 41 Korean parents of children ages 11-17 were recruited, consented and assigned to one of six language-congruent focus groups conducted by trained, bilingual, female facilitators: three groups each were held in Spanish and in English for Latino parents, and three groups in Korean and in English for Korean parents. Focus groups using semi-structured, guided discussion were conducted to identify and explore knowledge, attitudes and perceptions about HPV and the HPV vaccine, information sources on the HPV vaccine, cultural values, beliefs, and practices that influence attention, comprehension, perception and risk/benefit evaluation of HPV vaccine information to inform a vaccination decision. Discussions also explored specific themes, message elements and communication strategies for a patient-centered intervention that enhanced comprehension of the risks and benefits of the vaccine and its health implications. Audio recordings of the discussions were transcribed verbatim, with translations for the non-English sessions confirmed for accuracy by bilingual researchers. All transcripts were then systematically analyzed by the lead investigator for the following overarching themes: (a) knowledge about the HPV vaccine, (b) misconceptions and knowledge gaps about the HPV vaccine, (c) attitudes, concerns and perceptions regarding the HPV vaccine, (d) cultural values and beliefs that influenced their comprehension about the HPV vaccine, and (e) trusted, credible sources of information about the HPV vaccine. The transcripts were also examined for evidence of cognitive and affective factors that either promoted or impeded comprehension of the risks and benefits of HPV immunization. Further examination of the transcripts identified the extent, or lack thereof, of parents’ knowledge about HPV immunization recommendations, awareness of the Vaccines for Children Program, knowledge of the link between HPV and cervical cancer, and the sexual transmission of HPV, and indications of perceived risk, susceptibility and severity of an HPV infection.
Focus Group Findings
There were considerable similarities across both Latino and Korean parents on their awareness, limited knowledge and misconceptions about the HPV vaccine. Very few respondents knew the connection between HPV infection and cervical cancer. A few parents believed the HPV vaccine was a treatment or a cure for an HPV infection. The risk factors associated with HPV infection were not well understood by most parents. Most parents did not have an understanding of how human immunization works and did not know the recommendations regarding who should receive the HPV vaccine and when these vaccinations should occur. Perception about vaccines for many parents was colored by recent media coverage on the H1N1 flu vaccine.
The vast majority of parents were undecided, albeit generally open to the idea of vaccinating their children, but declared they needed more information to make a decision. Only a few parents reported they were opposed to vaccines in general, yet all but one of them was open to learning about the HPV vaccine. None of the parents believed they had sufficient information to make an informed HPV vaccination decision. They favored getting information from experts and from other parents who had their children vaccinated. Latino and Korean parents had a comparable hierarchy of concerns and information they needed to make an informed decision about the vaccine; safety, efficacy and side effects from the vaccine topped their list of salient concerns. Possible infertility was the most feared long-term side effects of the HPV vaccine. Parents generally did not like the idea of giving the HPV vaccine to their preadolescent children, and preferred to wait until they were older and their bodies more developed before giving them the vaccine. Notably, cost was not a major barrier for parents despite their financial status; none of the parents were aware of the Vaccines for Children Program, which covers vaccine cost for low-income children under age 18. Sexual promiscuity also was not a major concern; only a few parents expressed some concern that the vaccine would encourage sexual activity.
Notwithstanding these similarities, there were some notable difference between Latino and Korean parents on their perceptions, concerns and attitudes about the vaccine, HPV transmission and preferred sources of information about the vaccine. Latinos generally did not understand the etiology of HPV infection, while some Korean parents believed it was caused by a lack of feminine hygiene. Latino parents believed their children were at risk for HPV infection, yet Korean parents did not hold that view. Korean parents were not aware of the high prevalence of cervical cancer in their community and believed their children would refrain from having sex before marriage and thus would not be exposed to an HPV infection. Latino parents preferred getting information from a doctor or nurse. Korean parents generally distrusted doctors and pharmaceutical companies, and thus preferred getting information from government, public health sources or women’s clinics. Both groups favored information from other parents who had their children vaccinated. Notably, some Korean parents reported getting HPV vaccine information from television programs broadcast from Korea, from relatives in Korea or their travels in Korea; most often that information was inconsistent with the U.S. Advisory Committee on Immunization Practices (ACIP) HPV vaccination recommendations. Some Latino parents believed it was a matter of chance whether you got an HPV infection, and that it could not be prevented. A few Korean parents believed HPV was in your genes at birth. A widely held misconception among parents in both groups was that HPV was transmitted by sneezing or touching an infected surface. A few of them also believed HPV was transmitted through semen or that the HPV vaccine itself could cause cervical cancer. Most Korean parents were not informed about the HPV vaccine by physicians, yet a few reported their doctors told them not to get the vaccine, or to wait until their children were in high school; one doctor told a parent the vaccine was to cure prostate cancer in boys. Two parents reported their doctor told them the vaccine was not for Koreans, but for Latino and black youth, who were more likely to be sexually active. Corroboration in the research literature for the aforementioned focus group results is presented in the Discussion section below.
Intervention Materials
The multilingual, multicultural intervention materials were developed in four versions: English/Latino, Spanish/Latino, English/Korean, Korean/Korean. The challenge of developing four versions was addressed by producing a core of intervention messages common to the four versions, each augmented by messages tailored to the unique attitudes, knowledge gaps and misconceptions of each group that featured language, characters, situations and settings appropriate to each audience. Knowledge gaps identified by the focus groups were addressed in the common-core messages included: (a) the association between HPV infection and cervical cancer to underscore the severity of the disease, (b) the prevalence of HPV infection among Latinos and Koreans to foster an informed perception of risk and susceptibility, (c) how an HPV infection is transmitted to correct prevailing misconceptions, (d) the basics of human immunization to help parents understand the importance of vaccinating children at an age that precedes exposure to HPV, (e) delineation of the ACIP recommendations for age, gender and schedule of the vaccine to edify parents and dispel any confusion or misinformation, (f) the Food and Drug Administration’s (FDA) review process for approval of the HPV vaccine and subsequent Centers for Disease Control and Prevention (CDC) monitoring of vaccine recipients for adverse effects, and type and extent of reported side effects to inform and reassure parents about HPV vaccine safety, efficacy and side effects, (g) the cost of the three doses of the HPV vaccine, and existence of the Vaccines for Children Program, which ensures access to the vaccine for families that cannot afford it, and (h) the role of vaccination in an HPV risk-reduction strategy as an important prevention measure for communities at high risk for HPV infection. Both Latino versions (English/Spanish) of the intervention featured a Latina doctor and Latino parents. The Korean versions (English/Korean) specifically addressed the low perceived risk for HPV infection, their distrust of doctors and pharmaceutical companies, and preference for research and government sources for accurate and impartial information about the vaccine. These versions featured a Korean professor of Urology at University of California, Los Angeles who emphasized the high risk for HPV infection and correspondingly high cervical cancer morbidity in the Korean community. They also featured a kitchen conversation by two Korean-American mothers discussing their concerns about the HPV vaccine, weighing its risks and benefits and modeling their decision-making process to increase salience of the intervention messages.
Cognitive Interviews
Following production of culturally-tailored, language appropriate videos for a parent education DVD, 40 individual, language-concordant cognitive interviews were conducted: 10 Spanish-speaking and 10 English-speaking Latino parents and 10 Korean-speaking and 10 English-speaking Korean parents. Open-ended, discursive methods were used to assess the clarity and comprehension of the intervention messages, and identify changes that would enhance the clarity and resonance of those messages. The interviews also explored whether those messages offered timely and meaningful information parents could use, were intended for persons like themselves, whether the characters and contexts shown were credible and culturally familiar, and whether the language and terms used were familiar and easy to comprehend. Cognitive interview transcripts were systematically examined to assess four dimensions of the intervention messages (a) clarity, coherence, and comprehension ease, (b) perceived credibility and objectivity, (c) cultural proximity and resonance, and (d) salience, relevance and utility. These four dimensions invoke basic communication constructs related to cognition and learning germane to an education intervention. Particular attention was paid to whether any message elements stood out, were annoying or distracting, triggered an association or encouraged reflection and evaluation. Concepts, terms characters, images and contexts that were not readily comprehensible, did not have an affinity with the respondents’ cultural values and beliefs, were not responsive to parents’ information needs and concern, or were not perceived to have value and utility were marked for revision to improve the ability of the intervention messages to help parents make an informed HPV vaccination decision.
The cognitive interviews confirmed that the messages were generally clear and comprehensible to parents, were responsive to their information needs and concerns and were directed at parents like themselves. However, the interviews also identified the need for additional voice-overs and animation to clarify the ACIP recommendations and stress the scrutiny and diligence of the FDA approval process for the vaccine and the subsequent monitoring for vaccine safety and side effects. Another finding of these interviews was the need to clarify that boys were also susceptible to HPV infection and that HPV vaccination was also recommended for young males. Korean parents commented that the videos were too long and suggested segments that could be deleted. The videos were subsequently edited to address these specific issues, and multilingual versions of the intervention DVD were produced for use in a randomized clinical trial to assess their effectiveness in helping Latino and Korean parents make informed HPV vaccination decisions.
Efficacy Evaluation
The populations of interest for this efficacy study were Latinos and Koreans, communities at high risk for HPV infection and cervical cancer in the U.S. 9-19,21 who also experience economic, cultural or linguistic barriers to accessing health care. Their commonalties in access and utilization of preventive care, rather than their racial/ethnic difference explain their cervical cancer disparities.23 Indeed, studies on social determinants of health suggest that social inequalities faced by marginalized groups account for the health disparities they experience.24-34
Recruitment and Accrual
Parents of children who had not been previously vaccinated with the HPV vaccine were recruited by a trained, bilingual, bicultural, research assistant in their respective region: Latinos in Santa Clara County, CA and Koreans in the Los Angeles, CA basin. The inclusion criteria for participation in this efficacy study were: (a) self-identified member of either Korean or Latino communities, (b) either a parent/guardian of an unvaccinated child ages 11-12, or an unvaccinated adolescent ages 13-17, and (c) have telephone access to permit participation in a post-test interview.
Study Design
The Theory of Planned Behavior addresses the role of perception and cognition as antecedents to behavioral intention and motivation to perform a specific behavior.35-39 It is a well-suited theoretical framework for an efficacy evaluation that assesses the perceptual and cognitive effects of exposure to a health literacy intervention. This study employed a randomized controlled design in which knowledge, decisional conflict and making an informed decision are dependent variables and language and race/ethnicity are independent variables. Study participants were randomly assigned to either an intervention or control condition in equal numbers after administration of a pretest. The intervention group was then exposed to an education intervention on the HPV vaccine; the control group was exposed to a language-appropriate CDC flyer on the HPV vaccine. Four weeks from baseline, a post-test was administered to participants in both study arms. The hypotheses examined in this study were:
H1 Participants exposed to the intervention will report making an informed decision about HPV vaccination with greater frequency than control group participants.
H2 Participants exposed to the intervention will have higher levels of knowledge about HPV vaccine related topics at post-test compared to control group participants.
H3 Participants exposed to the intervention will have lower levels of decisional conflict in making an HPV-vaccination decision at post-test compared to control group participants.
H4 Participants exposed to the intervention will have higher levels of (a) decision self-efficacy in making an HPV-vaccination decision and (b) decision satisfaction about their HPV vaccine decision at post-test compared to control group participants.
Power Calculation and Sample Size
A sample of 750 parents will provide the ability to detect a difference between the study arms of 12 percentage points in persons who report making an informed HPV vaccination decision between pre/post-test. An estimated 80% retention rate for participants will detect this difference with 80% power at the 0.05 level (2- sided). A difference of this magnitude in the proportion making a decision was found by a randomized trial on hormone replacement therapy comparing an interactive videodisc decision aid with usual care.40 For an intention-to-treat analysis, in which study dropouts are regarded as not making an informed decision, the detectable difference is 13 percentage points in the retained sample. The study will also have more than 80% power to detect a difference between the study arms of 0.25 standard deviation (SD) in mean scores of continuous variables; this is smaller than the median effect sizes of 0.4 SD for decisional conflict and 0.8 SD for knowledge found by a meta-analysis of patient decision aids.41
Outcome Measures
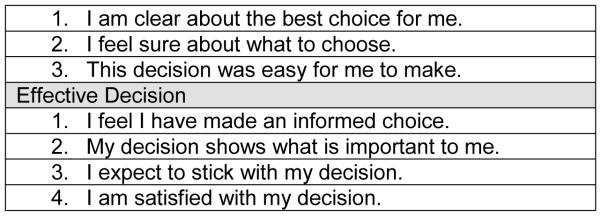
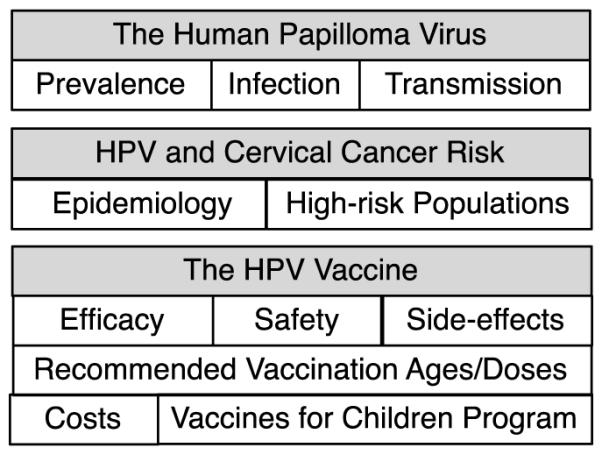
The outcome of primary interest in this study was an informed decision regarding HPV vaccination. Outcome measures for gauging intervention efficacy were knowledge gains and decisional attributes related to a vaccination decision. Knowledge measures included 12 true/false items (e.g., HPV infection may lead to cervical cancer) that were derived from the HPV and cervical cancer scales from the 2007 National Institutes of Health Health Information National Trends Survey (HINTS) and the 2007 California Health Information Survey (CHIS) scales on HPV knowledge and awareness. Both instruments are available in English and Spanish; CHIS is also available in Korean. Additional content-specific questions that correspond to unique messages developed for this intervention were included in the knowledge questions. The criteria for making an informed decision in this study were (a) making a vaccination choice, i.e. to have their child or children vaccinated, or not to have them vaccinated, (b) affirming that the decision was an informed choice, and (c) having a knowledge score of at least 7 of 12 knowledge items correct. Decisional attributes were measured with a validated instrument: the Decisional Conflict Scale, which measures the level of decisional conflict perceived.42,43,44 This instrument, which is well accepted in patient decision-aid studies, has Likert scale items with acceptable levels of validity and reliability.42,45,46 We used the Uncertainty subscale to measure decision self-efficacy and the Effective Decision subscale to measure decision satisfaction. See Figure 2.
Figure 2.
Decisional Conflict Subscales
Data Collection
Data collection was conducted in major population centers in California for the respective communities of interest to this study: San Jose (Latino) and Los Angeles (Korean) following protocols of the study methods and measures approved by an IRB review for the lead investigator’s institution. An individual, language-concordant pretest interview was conducted at baseline by trained, bilingual, bicultural research assistants. Participants were then randomized, stratified by study site (Los Angeles or San Jose), using a programmed algorithm on the laptop computer and assigned to an intervention or control study arm. Intervention group participants were given an HPV vaccine education DVD while control group participants were given a two-sided CDC flyer on the HPV vaccine. Participants were asked to make a vaccination decision within the next four weeks. A post-test telephone interview was conducted with study participants in both study arms four weeks from baseline. This post-test documented knowledge and decisional conflict, as well as the reported decision. It also ascertained whether respondents acted on their stated vaccination decision. Participants received incentives in the form of a $30 and $45 gift card for their pretest and post-test, respectively.
Data Analysis Procedures
The treatment and control groups were compared with respect to baseline demographic characteristics using chi-square tests for categorical variables and t-tests for numeric variables. The change from pre- to post-test in having made an informed decision was assessed within each study arm using McNemar’s test; the study arms were compared with respect to pre-post change in informed decision-making using a z-test that accounts for within-person correlation. Change from pre- to post-test in knowledge score and in the decisional conflict subscales and total score was assessed within each study arm using paired t-tests; the study arms were compared with respect to pre-post change using 2-sample t-tests. A multivariable logistic regression model was used to assess the treatment effect on having made an informed decision at post-test, controlling for having made an informed decision at pre-test and demographic characteristics posited to be associated with decision-making. Multiple linear regression was used to model the effects of treatment on pre-post change in knowledge score and pre-post change in decisional conflict total score controlling for demographic characteristics and the pre-test level of the outcome variable (knowledge or decisional conflict, respectively). Statistical significance was assessed at the 0.05 level (2-sided).
RESULTS
Study participants included 708 parents of children ages 9-17 who had not previously been vaccinated with the HPV vaccine. As shown in Table 1, over half of the participants were recruited from San Jose, and were between the ages of 35-44, female, had 12 years of education or less, married, and with 1-2 children. Most had a regular doctor for their children. The overwhelming majority of study participants were also born outside the U.S. and were interviewed in a language other than English. A total of 608 participants (86%) completed the post-test.
Table 1.
Demographic characteristics of Korean and Latino HPV vaccine education study participants by group at pre-test
| Control (n=344) n (%) |
Intervention (n=364) n (%) |
p | |
|---|---|---|---|
| Site | |||
| Los Angeles | 153 (44.5) | 167 (45.9) | 0.71 |
| San Jose | 191 (55.5) | 197 (54.1) | |
|
| |||
| Age | |||
| < 35 years | 40 (11.9) | 47 (13.2) | 0.27 |
| 35-39 | 86 (25.6) | 72 (20.3) | |
| 40-44 | 109 (32.4) | 136 (38.3) | |
| 45-49 | 58 (17.3) | 64 (18.0) | |
| 50+ | 43 (12.8) | 36 (10.1) | |
|
| |||
| Female | 322 (93.6) | 330 (90.9) | 0.18 |
|
| |||
| Married/living together | 253 (73.6) | 262 (72.0) | 0.64 |
|
| |||
| Number of children | |||
| 1-2 | 178 (51.7) | 192 (52.8) | 0.66 |
| 3-4 | 134 (39.0) | 145 (39.8) | |
| 5+ | 32 ( 9.3) | 27 ( 7.4) | |
|
| |||
| Education | |||
| <= 6 years | 76 (22.1) | 63 (17.3) | 0.003 |
| 7-11 years | 48 (14.0) | 70 (19.2) | |
| 12 years | 70 (20.4) | 61 (16.8) | |
| 13-15 years | 44 (12.8) | 26 ( 7.1) | |
| 16+ years | 106 (30.8) | 144 (39.6) | |
|
| |||
| Child has regular doctor | 287 (83.4) | 306 (84.3) | 0.75 |
|
| |||
| Language | |||
| Spanish | 176 (51.2) | 176 (48.4) | 0.38 |
| Korean | 150 (43.6) | 160 (44.0) | |
| English | 18 ( 5.2) | 28 ( 7.7) | |
|
| |||
| Birthplace | |||
| Latin America | 175 (51.5) | 177 (48.9) | 0.61 |
| Asia | 151 (44.4) | 162 (44.8) | |
| U.S. | 14 ( 4.1) | 23 ( 6.4) | |
|
| |||
| Years in the U.S. (foreign-born) | |||
| <=5 years | 55 (16.9) | 44 (13.0) | 0.42 |
| 6-10 | 63 (19.4) | 62 (18.3) | |
| 11-15 | 92 (28.3) | 96 (28.4) | |
| 16+ | 115 (35.4) | 136 (40.2) | |
|
| |||
| Mean (SD) | Mean (SD) | ||
|
| |||
| Age | 41.7 ( 6.4) | 41.7 ( 6.3) | 0.89 |
| Years in U.S. | 13.9 ( 8.5) | 14.7 ( 8.2) | 0.22 |
| Number of children | 2.8 ( 1.3) | 2.7 ( 1.2) | 0.62 |
Note: missing values for age (8 control, 9 intervention), gender (1 intervention), child has regular doctor (1 intervention), birthplace (4 control, 2 intervention), years in U.S. (5 control, 3 intervention)
As shown in Table 2, between pretest and post-test participants in the intervention group had significantly greater increases in their knowledge about HPV and cervical cancer compared to controls. Intervention participants also had significantly greater decreases in their perceived decisional conflict, as well as a greater increase in the proportion who had made an informed decision. As shown in Table 3, being in the intervention group and having made an informed decision at pretest significantly predicted whether participants reported making an informed decision at post-test. Intervention group participants had 2.4 times the odds of making an informed decision compared to control group participants, and participants who had made an informed decision at pretest had 3.3 times the odds of making an informed decision at post-test. As shown in Table 4, on average, pre-post change in knowledge was 1.7 points greater in the intervention group than in the control group (p<.0001), after adjustment for pretest knowledge level and demographic characteristics; participants with 6 or fewer years of education experienced smaller knowledge gains than college graduates (−0.9 point, p=0.01). Intervention group participants reported an average decrease in decisional conflict approximately 8 points greater in magnitude than that of control group members (p<.0001), adjusting for pretest level of decisional conflict and demographics; participants who were interviewed in English reported larger decreases in decisional conflict than those interviewed in Spanish or Korean (−6 points, p=0.03).
Table 2.
Korean and Latino HPV education study participants Changes from pre-test to post-test in knowledge, decisional conflict and made informed decision
| Control (n=318) Mean (SD) or n (%) |
Intervention (n=290) Mean (SD) or n (%) |
Difference P* |
|||||
|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | p | Pre-test | Post-test | p | ||
| Knowledge | 4.7 ( 2.2) | 7.1 ( 2.0) | <.0001 | 4.9 ( 2.4) | 8.9 ( 1.6) | <.0001 | <.0001 |
| Decisional conflict Informed Values clarity Support Uncertainty Effective decision Total |
57.3 (20.9) 53.3 (24.1) 39.0 (21.1) 37.8 (21.5) 29.6 (21.0) 42.5 (15.1) |
32.3 (21.4) 32.8 (22.1) 30.0 (20.4) 28.2(21.5) 23.3(19.7) 29.0 (17.3) |
<.0001 <.0001 <.0001 <.0001 <.0001 <.0001 |
56.4 (23.1) 51.8 (26.2) 38.2 (22.6) 36.8(22.7) 28.9(20.3) 41.6 (17.9) |
19.7(15.8) 20.3 (15.1) 22.8(17.1) 22.0(18.9) 19.1(16.6) 20.7 (13.4) |
<.0001 <.0001 <.0001 <.0001 <.0001 <.0001 |
<.0001 <.0001 0.0023 0.0159 0.0766 <.0001 |
|
Made informed decision |
35 (11.0) | 132 (41.5) |
<.0001 |
40 (13.8) | 182 (62.8) |
<.0001 |
<.0001 |
p-value for difference between intervention and control in pre-post change
Note: missing values for values clarity (2 control), effective decision (2 intervention), decisional conflict total (2 control, 2 intervention)
Table 3.
Korean and Latino HPV education study participants Effect of intervention on made informed decision at post-test (n=585)
| OR (95% CI) | p | |
|---|---|---|
| Intervention vs. Control group | 2.38 (1.68, 3.37) | <.0001 |
| Site: Los Angeles vs. San Jose | 0.59 (0.26, 1.37) | 0.22 |
| Language: English vs. non-English | 0.69 (0.32, 1.48) | 0.34 |
| Made informed decision (pretest): yes vs. no | 3.30 (1.84, 5.93) | <.0001 |
| Age < 40 years vs. 40 or more | 0.92 (0.62, 1.37) | 0.69 |
| Gender: male vs. female | 0.52 (0.26, 1.05) | 0.07 |
| Education <= 6 years vs. 16 or more Education 7-12 years vs. 16 or more Education 13-15 years vs. 16 or more |
0.44 (0.18, 1.10) 0.61 (0.27, 1.37) 0.72 (0.35, 1.46) |
0.08 0.23 0.36 |
| Not married vs. married/living together | 0.95 (0.62, 1.47) | 0.83 |
| <= 10 years in the U.S. vs. 11 or more/U.S. born | 1.22 (0.79, 1.88) | 0.38 |
| 1-2 children vs. 3 or more | 0.93 (0.63, 1.37) | 0.70 |
| Child has regular doctor | 1.14 (0.66, 1.94) | 0.65 |
Table 4.
Korean and Latino HPV education study participants Effect of Intervention on pre-post change in knowledge and decisional conflict total
| Change in Knowledge n=585 |
Change in Decisional Conflict n=581 |
|||
|---|---|---|---|---|
| Estimate (SE) | p | Estimate (SE) | p | |
| Intervention vs. Control group | 1.68 (0.14) | <.0001 | −7.82 (1.26) | <.0001 |
| Site: Los Angeles vs. San Jose | 0.37 (0.34) | 0.28 | −2.01 (2.97) | 0.50 |
| Language: English vs. non-English | −0.50 (0.32) | 0.11 | −6.05 (2.81) | 0.03 |
| Pre-test level of outcome | −0.76 (0.03) | <.0001 | −0.75 (0.04) | <.0001 |
| Age < 40 years vs. 40 or more | 0.06 (0.16) | 0.72 | 0.57 (1.42) | 0.69 |
| Gender: male vs. female | −0.09 (0.29) | 0.76 | 0.72 (2.50) | 0.77 |
| Education <= 6 years vs. 16 or more Education 7-12 years vs. 16 or more Education 13-15 years vs. 16 or more |
−0.93 (0.37) −0.42 (0.33) −0.44 (0.29) |
0.01 0.20 0.13 |
4.70 (3.26) −0.26 (2.89) 0.66 (2.55) |
0.15 0.93 0.80 |
| Not married vs. married/living together | −0.10 (0.18) | 0.55 | 0.13 (1.56) | 0.93 |
| <= 10 years in the U.S. vs. 11 or more/U.S. born | 0.06 (0.18) | 0.75 | −0.11 (1.58) | 0.94 |
| 1-2 children vs. 3 or more | 0.12 (0.16) | 0.45 | −0.21 (1.42) | 0.88 |
| Child has regular doctor | 0.13 (0.22) | 0.56 | −0.75 (1.98) | 0.71 |
DISCUSSION
The intervention was successful in promoting informed decision-making, increasing knowledge, and decreasing decisional conflict. The principal qualitative finding of this study was that despite their cultural differences, there were many similarities in the levels of knowledge, awareness, attitudes, and concerns between Latino and Korean parents. Both groups had an acute lack of knowledge and many misconceptions about HPV and the HPV vaccine. Both Latino and Korean parents were generally unaware of the association between HPV and cervical cancer, and were equally uninformed about the ACIP recommendations regarding the ages, gender and number of doses at specific intervals for HPV vaccination and corresponding costs. Concerns about the safety, efficacy and side effects of the vaccine were paramount in both groups. Parents in both groups were hesitant to vaccinate their preadolescent children and preferred to wait until they were older. The findings on a lack of knowledge about the HPV vaccine are consistent with other studies,47-62 as are concerns about the safety, efficacy and potential side effects of the vaccine.47,50-52,58,63-68 The commonly held perception that pre-pubescent children were too young to get the HPV vaccine has also been reported in a prior study.62,63 The distrust of doctors and pharmaceutical companies by Korean parents observed in this study has been reported for African American and other groups.64,69 The finding that very few parents believed the vaccine would encourage sexual promiscuity was also reported in several other studies.57,70
The finding of low perceived HPV susceptibility among Korean parents is significant given that other studies found perceived susceptibility to be among the most important factors in parental decision-making regarding the HPV vaccine.62,66,71 The basic concepts of human immunization and the advantage of HPV vaccination at a younger age were not well understood by parents; these findings in this study have not been previously reported. Moreover, the finding that parents were completely unaware of the Vaccine for Children Program has not been previously reported in the research literature. Anecdotal accounts of misinformation about the HPV vaccine given to Korean parents from some of their doctors has also not been previously reported, and should be examined further because it represents a significant barrier given that prior studies have noted the pivotal role of health care providers in parental acceptance of the vaccine.72,73 The assertion in a recent study that Latina parents were minimally involved in the decision regarding the HPV vaccine74 is not corroborated by this study, which observed that Latinas are eager to learn more about the vaccine so they can make informed decisions regarding their children’s health.
In sum, improved parents’ perceptions and comprehension of the risks and benefits of the HPV vaccine as a result of their exposure to the DVD suggest that the intervention did indeed motivate them to make an informed decision about HPV vaccination for their children. This finding is consistent with the Theory of Planned Behavior, which posits that perception and cognition underpin behavioral intention and motivation to perform a specific behavior. Improved self-efficacy following exposure to the intervention DVD suggests that parents perceived a benefit from HPV vaccination of their children and felt capable of adopting the recommended behavior. Future research should explore ways to further increase intentions to vaccinate among Latino and Korean parents. A promising area of new research among Korean parents76 found that interdependent self-construal—defined as actions based upon the "thoughts, feelings, and actions of specific others in particular social contexts"—mediated the relationship between Theory of Planned Behavior constructs, namely attitudes toward HPV vaccination and normative beliefs about HPV vaccination, and intention to vaccinate their children.
CONCLUSION
The findings of this study suggest that a multicultural, multilingual intervention designed to educate diverse parents about the risks, benefits, safety and efficacy of the HPV vaccine, the susceptibility to HPV infection and its association with cervical cancer enables parents to make an informed decision about HPV vaccination for their children. Culturally and linguistically tailored education materials are essential educational tools for communities at high risk for HPV infection.
LIMITATIONS
A notable limitation of the study is self-selection. Persons who agreed to participate in the study were likely to be more interested in the subject than other parents in their respective communities. Moreover, this study focused on Latino and Korean parents whose views may not reflect those of parents from other racial/ethnic groups across the nation. Hence, the findings of this study cannot be generalized to a larger population.
REFERENCES
- 1.Dunne EF, Unger ER, Sternberg M, McQuillan G, Swan DC, Patel SS, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007 Feb 28;297(8):813–9. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 2.Female Genital Tract Cancer. O’Leary M, Sheaffer J, Finklestein J, Olshan A, Brown J. In: cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. Bleyer A, O’Leary M, Barr R, Ries LAG, editors. National Cancer Institute; Bethesda, MD: 2006. NIH Pub. No. 06-5767. [Google Scholar]
- 3.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 4.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 5.Revzina NV, Diclemente RJ. Prevalence and incidence of human papillomavirus infection in women in the USA: a systematic review. Int J STD AIDS. 2005 Aug;16(8):528–37. doi: 10.1258/0956462054679214. [DOI] [PubMed] [Google Scholar]
- 6.Tarkowski TA, Koumans EH, Sawyer M, Pierce A, Black CM, Papp JR, et al. Epidemiology of human papillomavirus infection and abnormal cytologic test results in an urban adolescent population. J Infect Dis. 2004 Jan 1;189(1):46–50. doi: 10.1086/380466. Epub 2003 Dec 22. [DOI] [PubMed] [Google Scholar]
- 7.Winer RL, Lee SK, Hughes JP, Adam DE, Kiviat NB, Koutsky LA. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003 Feb 1;157(3):218–26. doi: 10.1093/aje/kwf180. [DOI] [PubMed] [Google Scholar]; Am J Epidemiol. 2003 May 1;157(9):858. doi: 10.1093/aje/kwg069. Erratum in: [DOI] [PubMed] [Google Scholar]
- 8.Trottier H, Franco EL. The epidemiology of genital human papillomavirus infection. Vaccine. 2006 Mar 30;24(Suppl 1):S1–15. doi: 10.1016/j.vaccine.2005.09.054. [DOI] [PubMed] [Google Scholar]
- 9.Manhart LE, Holmes KK, Koutsky LA, Wood TR, Kenney DL, Feng Q, et al. Human papillomavirus infection among sexually active young women in the United States: implications for developing a vaccination strategy. Sex Transm Dis. 2006 Aug;33(8):502–8. doi: 10.1097/01.olq.0000204545.89516.0a. [DOI] [PubMed] [Google Scholar]
- 10.American Cancer Society . Cancer Facts and Figures 2015. American Cancer Society; Atlanta: 2015. [Google Scholar]
- 11.Altekruse SF, Korasy TL, Krapcho M, Neyman N, Aminou R, et al., editors. SEER Cancer Statistics Review, 1975-2007. National Cancer Institute; Bethesda, MD: 2010. http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER website. [Google Scholar]
- 12.U.S. Cancer Statistics Working Group . United States Caner Statistics: 1999-2007 incidence and mortality web-based report. U.S. Department of Health and Human Services, Center for Disease Control and Prevention and National Cancer Institute; Atlanta: 2010. Available at www.cdc.goc.uscs. [Google Scholar]
- 13.Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER Cancer Statistics Review, 1975-2012. National Cancer Institute; Bethesda, MD: Apr, 2015. http://seer.cancer.gov/csr/1975_2012/, based on November 2014 SEER data submission, posted to the SEER web site. [Google Scholar]
- 14.Miller BA, Chu KC, Hankey BF, Ries LAG. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;17:227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsui J, Saralya M, Thompson T, Dey A, Richardson L. Cervical cancer screening among foreign-born women by birthplace and duration in the United States. Womens Health. 2007 Dec;16(10):1447–57. doi: 10.1089/jwh.2006.0279. [DOI] [PubMed] [Google Scholar]
- 16.Lauderdale DS, Huo D. Cancer death rates for older Asian-Americans: classification by race versus ethnicity. Cancer Causes Control. 2008;19:135–146. doi: 10.1007/s10552-007-9079-4. [DOI] [PubMed] [Google Scholar]
- 17.McCracken M, Olson M, Chen MS, Jemal A, et al. Cancer Incidence, Mortality and associated Risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean and Japanese Ethnicities. CA Cancer J Clin. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 18.Chen MS. Cancer health disparities among Asian Americans: what we know and what we need to do. Cancer. 2005;102(Suppl 12):2895–2902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 19.Rothman SM, Rothman DJ. Marketing and the HPV Vaccine Reply. JAMA. 2009;302(24):2661. doi: 10.1001/jama.2009.1885. [DOI] [PubMed] [Google Scholar]
- 20.Massad LS. Marketing and the HPV vaccine. JAMA. 2009 Dec 23;302(24):2660. doi: 10.1001/jama.2009.1885. author reply 2661. [DOI] [PubMed] [Google Scholar]
- 21.Betensky M. Marketing and the HPV vaccine. JAMA. 2009 Dec 23;302(24):2660–1. doi: 10.1001/jama.2009.1886. author reply 2661. [DOI] [PubMed] [Google Scholar]
- 22.Jeudin P, Liveright E, del Carmen MG, Perkins RB. Race, ethnicity and income as factors for HPV vaccine acceptance and use. Hum Vaccin Immunother. 2013 Jul;9(7):1413–20. doi: 10.4161/hv.24422. [DOI] [PubMed] [Google Scholar]
- 23.Etter DJ, Zimet GD, Rickert VI. Human papillomavirus vaccine in adolescent women: a 2012 update. Curr Opin Obstet Gynecol. 2012 Oct;24(5):305–10. doi: 10.1097/GCO.0b013e3283567005. [DOI] [PubMed] [Google Scholar]
- 24.Cates JR, Ortiz R, Shafer A, Romocki LS, Coyne-Beasley T. Designing messages to motivate parents to get their preteenage sons vaccinated against human papillomavirus. Perspect Sex Reprod Health. 2012 Mar;44(1):39–47. doi: 10.1363/4403912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic Status and Health in Industrial Nations: social, psychological, and biological pathways. New York Academy of Sciences; New York: 1999. [PubMed] [Google Scholar]
- 26.Evans RG, Barer ML, Marmot TR, editors. Why Are Some People Healthy and Others Not?: the Determinants of Health of Populations. Aldine de Gruyter; New York: 1994. [Google Scholar]
- 27.Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. doi: 10.1136/bmj.312.7037.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawachi I, Kennedy BP, Wilkinson RG, editors. The Society and Population Health Reader: Income Inequality and Health. The New Press; New York: 1999. [Google Scholar]
- 29.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self-rated health: a U.S. multi-level analysis. BMJ. 1998;317:917–921. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacIntyre S, MacIver S, Sooman A. Area, class and health: should we be focusing on places or people? Journal of Social Policy. 1993;22:213–234. [Google Scholar]
- 31.Marmot M, Wilkinson RG, editors. Social Determinants of Health. Oxford University Press; New York: 1999. [Google Scholar]
- 32.Wilkinson R, Marmot M, editors. Social Determinants of Health: the solid facts. World Health Organization; 1998. [Google Scholar]
- 33.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304:165–168. doi: 10.1136/bmj.304.6820.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Institute of Health, Office of Behavioral and Social Sciences Research Toward Higher Levels of Analysis: Progress and Promise in Research on Social and Cultural Dimensions of Health. Jun, 2000.
- 35.Willson AE. 2006-08-10 Fundamental Causes of Health Disparities: A Comparative Analysis of Canada and the United States; Paper presented at the annual meeting of the American Sociological Association; Montreal, Quebec, Canada. Montreal Convention Center; Online 2009-05-24, Available from http://www.allacademic.com/meta/p96691_index.html. [Google Scholar]
- 36.Ajzen I. In: From intentions to actions: a theory of planned behavior. Action-control: From cognition to behavior. Kuhl J, Beckman J, editors. Springer; Heidelberg: 1985. pp. 11–39. [Google Scholar]
- 37.Ajzen I. Attitudes, traits, and actions: dispositional prediction of behavior in personality and social psychology. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 20. Academic Press; New York: 1987. pp. 1–63. [Google Scholar]
- 38.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- 39.Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol. 2002;32:665–683. [Google Scholar]
- 40.Ajzen I. 2nd Open University Press / McGraw-Hill; Milton-Keynes, England: 2005. Attitudes, personality, and behavior. [Google Scholar]
- 41.O'Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. Randomized trial of a portable, self-administered decision aid for postmenopausal women considering long-term preventive hormone therapy. Med Decis Making. 1998 Jul-Sep;18(3):295–303. doi: 10.1177/0272989X9801800307. [DOI] [PubMed] [Google Scholar]
- 42.Murray E, Davis H, Tai SS, Coulter A, Gray A, Haines A. Randomised controlled trial of an interactive multimedia decision aid on hormone replacement therapy in primary care. BMJ. 2001 Sep 1;323(7311):490. doi: 10.1136/bmj.323.7311.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Coner AM. Validation of a Decisional Conflict Scale. Medical Decision Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 44.Bunn H, O’Connor A. Validation of client decision-making instruments in the context of psychiatry. Can J Nurs Res. 1996;28:13–27. [PubMed] [Google Scholar]
- 45.Stalmeier PFM, Roosmalen MS, Verhoef LCG, et al. The decision evaluation scales. Patient Educ Couns. 2005;57:286–293. doi: 10.1016/j.pec.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 46.Ottawa Health Research Institute User manual for decision self-efficacy. 2004 Available from http://decisionaid.ohri.ca/eva.html.
- 47.Ottawa Health Research Institute User manual for decisional conflict. Available from http://decisionaid.ohri.ca/eva.html;2004.
- 48.Cates JR, Ortiz R, Shafer A, Romocki LS, Coyne-Beasley T. Designing messages to motivate parents to get their pre-teenage sons vaccinated against human papillomavirus. Perspect Sex Reprod Health. 2012 Mar;44(1):39–47. doi: 10.1363/4403912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friedman AL, Shepeard H. Exploring the knowledge, attitudes, beliefs, and communication preferences of the general public regarding HPV: findings from CDC focus group research and implications for practice. Health Educ Behav. 2007 Jun;34(3):471–85. doi: 10.1177/1090198106292022. [DOI] [PubMed] [Google Scholar]
- 50.Morales-Campos DY, Markham CM, Peskin MF, Fernandez ME. Hispanic mothers' and high school girls' perceptions of cervical cancer, human papilloma virus, and the human papilloma virus vaccine. J Adolesc Health. 2013 May;52(5 Suppl):S69–75. doi: 10.1016/j.jadohealth.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 51.Hofman R, van Empelen P, Vogel I, Raat H, van Ballegooijen M, Korfage IJ. Parental decisional strategies regarding HPV vaccination before media debates: a focus group study. J Health Commun. 2013;18(7):866–80. doi: 10.1080/10810730.2012.757390. [DOI] [PubMed] [Google Scholar]
- 52.Wilson R, Brown DR, Boothe MA, Harris CE. Knowledge and acceptability of the HPV vaccine among ethnically diverse black women. J Immigr Minor Health. 2013 Aug;15(4):747–57. doi: 10.1007/s10903-012-9749-5. [DOI] [PubMed] [Google Scholar]
- 53.Wong LP. Preventing cervical cancer through human papillomavirus vaccination: perspective from focus groups. J Low Genit Tract Dis. 2009 Apr;13(2):85–93. doi: 10.1097/LGT.0b013e3181865f44. [DOI] [PubMed] [Google Scholar]
- 54.Chau J, Kibria F, Landi M, Reilly M, Medeiros T, Johnson H, et al. R I Med J (2013) 2014 May 1;97(5):35–9. [PubMed] [Google Scholar]
- 55.Molokwu J, Fernandez NP, Martin C. HPV awareness and vaccine acceptability in Hispanic women living along the US-Mexico border. J Immigr Minor Health. 2014 Jun;16(3):540–5. doi: 10.1007/s10903-013-9855-z. [DOI] [PubMed] [Google Scholar]
- 56.Gelman A, Nikolajski C, Schwarz EB, Borrero S. Racial disparities in awareness of the human papillomavirus. Womens Health (Larchmt) 2011 Aug;20(8):1165–73. doi: 10.1089/jwh.2010.2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu JP, Porch E, McWeeney M, Ohman-Strickland P, Levine JP. Knowledge and concerns related to the human papillomavirus vaccine among underserved Latina women. J Low Genit Tract Dis. 2010 Jul;14(3):155–61. doi: 10.1097/LGT.0b013e3181d4e747. [DOI] [PubMed] [Google Scholar]
- 58.Patel PR, Berenson AB. Sources of HPV vaccine hesitancy in parents. Hum Vaccin Immunother. 2013 Dec;9(12):2649–53. doi: 10.4161/hv.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bingham A, Drake JK, LaMontagne DS. Sociocultural issues in the introduction of human papillomavirus vaccine in low-resource settings. Arch Pediatr Adolesc Med. 2009 May;163(5):455–61. doi: 10.1001/archpediatrics.2009.50. [DOI] [PubMed] [Google Scholar]
- 60.Reiter PL, Stubbs B, Panozzo CA, Whitesell D, Brewer NT. HPV and HPV vaccine education intervention: effects on parents, healthcare staff, and school staff. Cancer Epidemiol Biomarkers Prev. 2011 Nov;20(11):2354–61. doi: 10.1158/1055-9965.EPI-11-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hendry M, Lewis R, Clements A, Damery S, Wilkinson C. "HPV? Never heard of it!": a systematic review of girls' and parents' information needs, views and preferences about human papillomavirus vaccination. Vaccine. 2013 Oct 25;31(45):5152–67. doi: 10.1016/j.vaccine.2013.08.091. [DOI] [PubMed] [Google Scholar]
- 62.Perkins RB, Apte G, Marquez C, Belizaire M, Clark JA, Pierre-Joseph N. Factors affecting human papillomavirus vaccine use among white, black and Latino parents of sons. Pediatr Infect Dis J. 2013 Jan;32(1):e38–44. doi: 10.1097/INF.0b013e31826f53e3. [DOI] [PubMed] [Google Scholar]
- 63.Zimet GD. Improving adolescent health: focus on HPV vaccine acceptance. J Adolesc Health. 2005 Dec;37(6 Suppl):S17–23. doi: 10.1016/j.jadohealth.2005.09.010. Review. [DOI] [PubMed] [Google Scholar]
- 64.Hull PC, Williams EA, Khabele D, Dean C, Bond B, et al. HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecol Oncol. 2014 Mar;132(Suppl 1):S13–20. doi: 10.1016/j.ygyno.2014.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Allen JD, de Jesus M, Mars D, Tom L, Cloutier L, Shelton RC. Decision-making about the HPV Vaccine among Ethnically Diverse Parents: implications for health communications. J Oncol. 2012;2012:401979. doi: 10.1155/2012/401979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007 Aug-Sep;45(2-3):107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 67.Hendry M, Lewis R, Clements A, Damery S, Wilkinson C. "HPV? Never heard of it!": a systematic review of girls' and parents' information needs, views and preferences about human papillomavirus vaccination. Vaccine. 2013 Oct 25;31(45):5152–67. doi: 10.1016/j.vaccine.2013.08.091. [DOI] [PubMed] [Google Scholar]
- 68.Alexander AB, Stupiansky NW, Ott MA, Herbenick D, Reece M, Zimet GD. Parent-son decision-making about human papillomavirus vaccination: a qualitative analysis. BMC Pediatr. 2012 Dec 14;12:192. doi: 10.1186/1471-2431-12-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu JP, Porch E, McWeeney M, Ohman-Strickland P, Levine JP. Knowledge and concerns related to the human papillomavirus vaccine among underserved Latina women. J Low Genit Tract Dis. 2010 Jul;14(3):155–61. doi: 10.1097/LGT.0b013e3181d4e747. [DOI] [PubMed] [Google Scholar]
- 70.Jeudin P, Liveright E, Del Carmen MG, Perkins RB. Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clin Ther. 2014 Jan 1;36(1):24–37. doi: 10.1016/j.clinthera.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 71.Wong LP. Preventing cervical cancer through human papillomavirus vaccination: perspective from focus groups. J Low Genit Tract Dis. 2009 Apr;13(2):85–93. doi: 10.1097/LGT.0b013e3181865f44. [DOI] [PubMed] [Google Scholar]
- 72.Hofman R, van Empelen P, Vogel I, Raat H, van Ballegooijen M, Korfage IJ. Parental decisional strategies regarding HPV vaccination before media debates: a focus group study. J Health Commun. 2013;18(7):866–80. doi: 10.1080/10810730.2012.757390. [DOI] [PubMed] [Google Scholar]
- 73.Fernández, Allen JD, Mistry R, Kahn JA. Integrating clinical, community, and policy perspectives on human papillomavirus vaccination. Annu Rev Public Health. 2010;31:235–252. doi: 10.1146/annurev.publhealth.012809.103609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cates JR, Shafer A, Carpentier FD, Reiter PL, Brewer NT, McRee AL, et al. How parents hear about human papillomavirus vaccine: implications for uptake. J Adolesc Health. 2010 Sep;47(3):305–8. doi: 10.1016/j.jadohealth.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Allen JD, de Jesus M, Mars D, Tom L, Cloutier L, Shelton RC. Decision-Making about the HPV Vaccine among Ethnically Diverse Parents: implications for health communications. J Oncol. 2012;2012:401979. doi: 10.1155/2012/401979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nan Z, Huh J, Murphy ST, Chatterjee JS, Baezconde-Garbanati L. Self-construal as a predictor of Korean American women's intention to vaccinate daughters against human papillomavirus. Asian Am J Psychol. 2014 Jan;5(2):96–105. doi: 10.1037/a0036097. [DOI] [PMC free article] [PubMed] [Google Scholar]