Abstract
Trichomonas vaginalis (Tv) is an extracellular protozoan parasite that causes the most common non-viral sexually transmitted infection: trichomoniasis. While acute symptoms in women may include vaginitis, infections are often asymptomatic, but can persist and are associated with medical complications including increased HIV susceptibility, infertility, pre-term labor, and higher incidence of cervical cancer. Heightened inflammation resulting from Tv infection could account for these complications. Effective cellular immune responses to Tv have not been characterized, and re-infection is common, suggesting a dysfunctional adaptive immune response. Using primary human leukocyte components, we have established an in vitro co-culture system to assess the interaction between Tv and the cells of the human immune system. We determined that in vitro, Tv is able to lyse T-cells and B-cells, showing a preference for B-cells. We also found that Tv lysis of lymphocytes was mediated by contact-dependent and soluble factors. Tv lysis of monocytes is far less efficient, and almost entirely contact-dependent. Interestingly, a common symbiont of Tv, Mycoplasma hominis, did not affect cytolytic activity of the parasite, but had a major impact on cytokine responses. M. hominis enabled more diverse inflammatory cytokine secretion in response to Tv and, of the cytokines tested, Tv strains cleared of M. hominis induced only IL-8 secretion from monocytes. The quality of the adaptive immune response to Tv is therefore likely influenced by Tv symbionts, commensals, and concomitant infections, and may be further complicated by direct parasite lysis of effector immune cells.
Author Summary
The unicellular parasite Trichomonas vaginalis (Tv) causes the most common non-viral sexually transmitted infection worldwide, with approximately one quarter of a billion people infected annually. Tv infections are linked to pre-term and low-weight infant birth, increased susceptibility to and transmission of HIV infection, and increased aggressiveness of urogenital tract cancers. How the immune system responds to Tv, and how the parasite persists in the presence of the immune system, is not well understood. We show that Tv can kill human immune cells. We found that a clinical isolate of Tv is more efficient at killing immune cells than a laboratory-adapted strain, and that Tv preferentially targets B-cells. This killing activity is mediated by both contact-dependent and soluble factors. Killing immune cells could allow Tv to subvert or disable the immune system. Conversely, we found that cells of the immune system respond to Tv by secreting soluble inflammatory mediators called cytokines, mainly interleukin-8. However, these cells secrete greater amounts, and a broader profile of inflammatory cytokines when they encounter Tv harboring its symbiont bacterium, Mycoplasma hominis. We conclude that Tv may interact with immune cells in different ways, depending on the strain of Tv and the symbiont it harbors.
Introduction
Trichomonas vaginalis (Tv) is a unicellular, aerotolerant, flagellated protozoan parasite that is an obligate extracellular pathogen, restricted to humans [1]. Tv adheres to and lyses host epithelial cells [2], followed by phagocytosis of cellular contents [3]. Tv destruction of the epithelial layer in the female reproductive tract (FRT) is apparent in the clinical presentation of “strawberry cervix,” in which red lesions are visible on the external surface of the cervix of infected women [1]. Once thought to be a commensal member of the vaginal microflora, Tv is now known to be pathogenic and is responsible for the most common non-viral sexually transmitted infection (STI) in the United States and worldwide: trichomoniasis [4]. The WHO reports ~275 million cases annually [1], but this number is likely a gross underestimation, as the CDC estimates that at least 50% percent of cases are asymptomatic. In the United States, an estimated 8–10 million new infections occur annually [5]. Alarmingly, trichomoniasis is on the rise in adolescents [6], and in dense urban areas prevalence can be as high as 50% [7]. Because Tv responds well to metronidazole, an antibiotic that specifically kills anaerobic cells [1], most symptomatic cases are successfully treated. However, emergence of metronidazole-resistant strains continues to increase [4,8–12], and metronidazole treatment may not efficacious for preventing pregnancy-related Tv complications [13,14]. Moreover, the association of subclinical infection with complications affecting women’s reproductive health [6,15] necessitates a better understanding of how Tv causes disease, and how the immune system responds to the parasite.
Trichomoniasis is associated with increased susceptibility to HIV, HSV-2, pelvic inflammatory disorder, pre-term and low-weight infant birth, infertility, and endometritis [15]. Tv infection is also associated with bacterial vaginosis, suggesting a disruption of the microflora [6]. In addition, Tv infection or serostatus has been correlated with an increased incidence of cervical cancer [16,17], especially invasive types [18–20]. Although Tv is typically asymptomatic in men [21], they are commonly infected and trichomonads can be detected in prostate tissue [22]. Tv infection in men has been linked to invasive forms of prostate cancer [23], and infertility [24]. It is thought that Tv- induced inflammation can exacerbate existing neoplastic lesions, increasing chances of malignancy [25,26].
Tv often co-exists with a symbiont bacterium, Mycoplasma hominis [27]. Otherwise axenic cultures of clinical isolates and lab strains of Tv often contain M. hominis, growing both externally to and within Tv [28,29]. This is unlikely to be an artifact of laboratory-introduced contamination, as a recent study of clinical isolates found the prevalence of M. hominis in Tv isolates to be 56% [30]. The prevalence of the biological association of Tv and M. hominis underscores the epidemiological relevance of studying Tv strains containing M. hominis.
Despite the association of Tv with numerous complications of a putative inflammatory etiology, how the immune system responds to and clears Tv is not well understood. Neutrophils are usually abundant during acute infection [31,32]. Antibodies can be detected in sera of infected persons [1,33,34], and after experimental challenge in a mouse model [35]. Peripheral blood mononuclear cells (PBMC) from infected persons proliferate in vitro in response to re-call antigen [36], and CD4+T cells were shown to be present after experimental mouse infection [35]. However, partner re-infection is common [1], indicating that there may be inadequate formation of immunological memory, or that Tv subverts effective adaptive immune responses. Tv has also been shown to induce IL-8 secretion from primary human monocytes [37]. In addition, the Tv symbiont Mycoplasma hominis has been shown to enable induction of an array of inflammatory cytokines in a macrophage cell line following Tv encounter [38]. However, studies examining the cytokine profile following Tv encounter with primary human monocytes have yet to be performed.
Tv shares a niche with numerous other commensal microorganisms in the FRT [39], and infection is often concomitant with other STIs [1,5]. Leukocytes populate mucosal tissues of the FRT [40], where they manage responses to commensals and other STIs. Leukocytes are predominant in the lamina propria, but may also follow trans-epithelial chemokine signals to home to the luminal side of the mucosa [41]. Tv may therefore encounter leukocytes while adhering to epithelial cells on the luminal side of the FRT, or approaching the lamina propria as the epithelial layer is breached by Tv cytolysis of epithelial cells. Tv has been demonstrated to phagocytose human leukocytes [42], indicating that direct leukocyte killing could contribute to Tv immune subversion; however, the efficiency, kinetics, and cell-specificity of this process is unknown.
Characterizing the type of immune response that Tv stimulates and determining whether Tv cytotoxic activity can kill leukocytes will be important to understanding why Tv is often persistent, how Tv infection may lead to inflammatory sequelae, and how Tv infection may affect the microbiome in the FRT. Tv is a human-specific pathogen, and most attempts at experimental mouse infection have failed to sustain adequate parasite titers, with the exception of a model using pre-treatment with estrogen and dexamethasone [43], both of which are immunosuppressive and therefore undesirable for analysis of immune function. In addition, specific host-surface proteins are implicated in pathogenesis [44], so using cells of the natural host for these studies is optimal. Using primary human leukocytes, here we show that Tv is able to kill immune effector cells, showing a preference for B-cells, and that cytokine responses induced by the parasite are largely dependent on the symbiont M. hominis.
Methods
Ethics statement
All work with cells from human blood donation was done in compliance with the UCLA School of Medicine IRB Committee.
Trichomonas vaginalis strains and culture
Tv strains G3 (Beckenham, UK 1973, ATCC-PRA-98), and MSA1132 (Mt. Dora, Fla, USA 2008) were grown in TYM medium supplemented with 10% horse serum (Sigma), 10 U/ml penicillin (Invitrogen), 10 μg/ml streptomycin (Invitrogen), 180 μM ferrous ammonium sulfate, and 28 μM sulfosalicylic acid [45] at 37°C. Strains were passaged daily and maintained at an approximate concentration of 1 x 105–2 x 106 cells/ mL. To generate M. hominis free strains, Tv was grown in the presence of 50 μg/ml chloramphenicol and 5 μg/ml tetracycline (Sigma-Aldrich), supplemented daily for at least 5 days and M. hominis clearance was confirmed by PCR as described below. To generate dead, intact controls, Tv was counted, and then reconstituted in complete RPMI media, and rendered dead—but intact—by treatment at 65°C for 1 hour, followed by 3 freeze-thaw cycles [46]. Trichomonads were confirmed by microscopy to be immobile and intact and flow cytometry analysis using Zombie Red dead-cell exclusion dye (Biolegend) confirmed that trichomonads were not viable after this treatment.
Primary human cell acquisition and culture
Primary human peripheral blood mononuclear cells (PBMC) were isolated from leukopacks or trima filters using Ficoll gradient. Blood was obtained from 32 de-identified, healthy donors from the UCLA Virology Core using a UCLA Institutional Review Board approved protocol. Monocytes were isolated based on adherence to plastic (for monocytes used in cytotoxicity experiments) or by Rosette Sep © negative isolation (Stem Cell technologies) (for monocytes used in cytokine secretion experiments). PBMC and monocytes were frozen directly after purification and used the day they were thawed. All experiments with PBMC and monocytes were done using RPMI 1640 media supplemented with 10% Fetal Bovine Serum, Pen/Strep, GlutaMAX, and MEM non-essential amino acids, (Life Technologies), and incubated at 37°C with 5% CO2.
In vitro differentiation of human monocyte-derived macrophages (HMDM)
Primary human PBMC were isolated from a trima filters using Ficoll gradient using blood from donors at the UCLA Virology Core. Monocytes were separated based on adherence to plastic and were plated at 2.7 x 105 cells/ml. 20 ng/ml of GM-CSF (Biolegend) was added for 4 days to induce macrophage differentiation. The differentiation was verified by staining with anti- CD14-PE (Invitrogen- MHCD14014) and an increase in forward scatter (size).
Flow-Cytometry based cytotoxicity assay
Brooks et al. demonstrated that Tv- host cell co-cultures are suitable for flow cytometry analysis [47]. As the similar size of Tv and leukocytes confounds cell discernment via size and scatter properties alone, we utilized differential dye staining. PBMC were labeled with Carboxyfluorescein succinimidyl ester (CFSE) (Biolegend) at 1:2000 for 3 minutes according to the manufacturer’s instructions and then washed and plated at 2.5 x 105 cells/well in 100 μl in u-bottom 96 well plates. Tv was labeled with Cell Tracker Blue © (Molecular Probes), according to the manufacturer’s instructions, and then allowed to recover in complete TYM media for 45 minutes- 2 hours. Tv was then reconstituted in complete RPMI media and added directly to wells containing PBMC at the indicated multiplicities of infection (MOI) for the indicated period of time. After incubation, cells were stained with anti-CD3 APC clone HIT3a and anti-CD19 PeCy7 clone HIN19 (both from Biolegend) at 1 μg/ml in FACS buffer (PBS with 5% FBS and 0.1% sodium azide) on ice for 30 minutes. Cells were then washed and resuspended in FACS buffer and analyzed within 2 hours on an LSR Fortessa © (Becton-Dickinson) at the UCLA Broad Stem Cell Research Center Flow Cytometry core facility. Directly before sample acquisition, 5 μl of Bright Count © counting beads (Life Technologies) was added to each sample. Data were analyzed using FlowJo (Treestar), and counts of each population (Tv, T-cell or B-cell) were determined according to the gating strategy is shown in S1 Fig. Cell counts were uniformly normalized to 2,000 beads, and percent death was calculated as ((# of B-cells in PBMC alone condition—# of B-cells in co-culture condition) / # of B-cells in PBMC alone condition) *100, for B-cells (same analysis was done for T-cells) or as ((# of parasites in parasites alone condition—# of parasites in co-culture condition) / # of parasites in parasites alone condition)*100 for Tv. Zombie Red dead-cell exclusion dye (Biolegend) was added to preliminary cytotoxicity experiments to assure that live cell gates based on forward and side scatter did not include dead cells (S2 Fig), and then found to be redundant since dead cells disappear from the live cell scatter plot completely. Zombie Red staining was therefore excluded in subsequent experiments for simplicity. For transwell cytotoxicity experiments, an HTS Transwell—96 well plate (Corning) with 0.4 μm polycarbonate membrane was used. PBMC were placed in the bottom, receiver plate, which was spun down and processed as described above after the co-culture. Two-tailed, unpaired student’s T-test was done to determine statistical significance between conditions, when relevant.
Lactate dehydrogenase-based cytotoxicity assay
Monocytes isolated based on plastic adherence as described above were plated at 5 x 105 cells/ well in 96-well flat-bottom plates. Tv was reconstituted in complete RPMI media as described above and added at the indicated MOI for the indicated period of time. After the co-culture, monocyte death was measured by determining mammalian-specific lactate dehydrogenase (LDH) release using the CytoTox-One © homogeneous membrane integrity assay (Promega) according to the manufacturer’s instructions. Samples were read on a Victor3 1420 plate reader (Perkin-Elmer) to generate mean fluorescence intensity (MFI) values correlating with LDH presence in the supernatants. Percent death was calculated as (MFI from co-culture supernatants- MFI from live monocytes alone supernatants)/ (MFI from detergent solubilized monocytes alone supernatants–MFI from live monocytes alone supernatants) *100. Transwell cytotoxicity experiments were conducted as described above.
Cytokine analysis
Human monocytes isolated by Rosette Sep © negative selection were plated at 5 x 104 cells/ well in 96-well u-bottom plates. Tv was counted, and then reconstituted in complete RPMI media, and rendered dead, but intact as described above. Dead, intact Tv were then added to monocytes, or human monocyte derived macrophages (HMDM) at an MOI (multiplicity of infection) of 1, and allowed to incubate overnight (16 hours). Positive controls were 100 ng/ml LPS (sigma) 10 μg/ml poly (I:C) (Tocris) or 1000 U/ml IFN gamma (Biolegend). Subsequently plates were centrifuged and supernatants were harvested and frozen at -80°C. Supernatants were then thawed on ice and analyzed using Cytometric Bead Array (Becton-Dickenson) for IL-8, IL-6, IL-1β, TNFα, and IL-12 according to the manufacturer’s instructions. IL-6, IL-1β, and IL-12 were multiplexed, and IL-8 was measured separately on supernatants diluted 1:100. Data were analyzed using FlowJo (Treestar) to determine MFI, which was normalized to absolute concentrations according to a standard curve generated using lyophilized protein provided with the kit. IL-23 was measured using Legend Max Human IL-23 (p19/p40) ELISA kit with pre-coated wells (Biolegend) according to the manufacturer’s instructions. Wells were read using a Victor3 1420 plate reader (Perkin-Elmer), and MFI was normalized as described above.
M. hominis analysis in T. vaginalis strains
Dense 15ml cultures of Tv were lysed using a solution of 8M urea, 2% sarkosyl, 0.15M NaCl, 0.001M EDTA, and 0.1M Tris HCL pH7.5, and DNA was extracted using phenol: chloroform: ISA (Amresco), precipitated with isopropanol, and reconstituted in 10mM Tris pH8+ RNase. Then PCR was performed on Tv DNA using the following primer pairs: (1) M. hominis specific primers: 5’ CAA TGG CTA ATG CCG GAT ACG C 3’ and 5’ GGT ACC GTC AGT CTG CAA T 3’ [48] and (2) universal 16S rDNA primers: 5’ AGA GTT TGA TCC TGG CTC AG 3’ and 5’ GGA CTA CCA GGG TAT CTA AT 3’ (Greg James, PCR for Clinical Microbiology, 2010). PCR products were sequenced (Genewiz), and resultant sequences were aligned using NCBI nucleotide BLAST and ApE software and confidence peaks were examined in comparison to M. hominis sequence. These analysis were done on non-clonal Tv strains G3 and MSA1132 either cured of resident M. hominis strains or prior to curing with antibiotic treatment. Identical M. hominis sequences were derived using uncured strains in replicate experiments.
Results
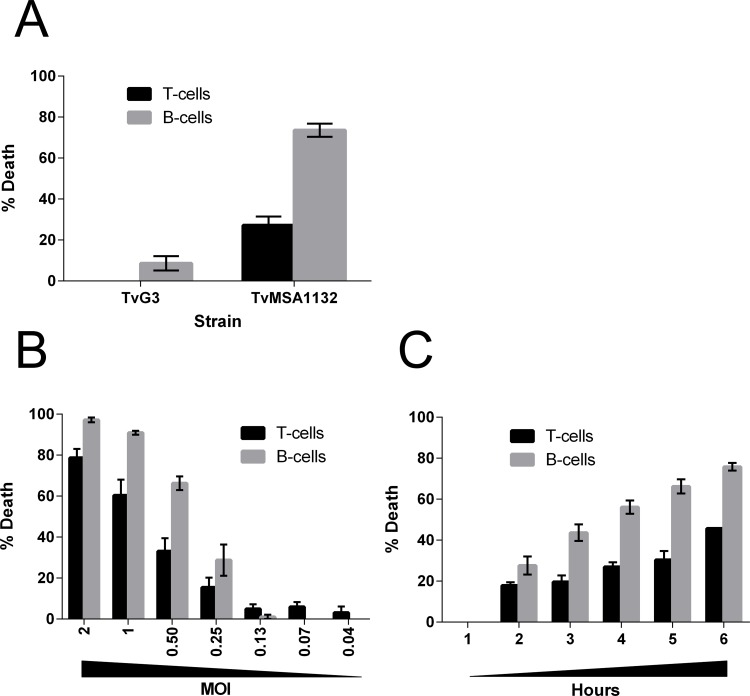
Trichomonas vaginalis (Tv) is known to lyse cervical and prostate epithelial cells [2]. Since leukocytes are present in the genital mucosa [40], and in the lamina propria directly beneath the epithelial layer [41], we asked whether Tv is able to kill leukocytes. To assess this, we set up an in vitro co-culture system of Tv with primary human peripheral blood mononuclear cells (PBMC), and then determined numbers of surviving cells using flow cytometry following the co-culture. Prior to the co-culture, Tv were labeled with Cell Tracker Blue © (CTB), and PBMC were labeled with carboxyfluorescein succinimidyl ester (CFSE). After co-culture, wells were stained with anti-CD3 and anti-CD19 to identify T-cells and B-cells, respectively. Directly before flow cytometry analysis, counting beads were added to wells for sample-to-sample volume normalization. Counts of live CTB+ CFSE- (Tv), CFSE+CD3+ (T-cells) and CFSE+CD19+ (B-cells) events were then determined and normalized to PBMC alone, or Tv alone controls to calculate percent death of each population. Using this system, we first tested a common laboratory adapted strain of Tv (G3) [49] compared to a relatively recent clinical isolate of Tv (MSA1132) [2]. We observed that clinical strain MSA1132 was able to kill ~30% of T cells and ~70% of B-cells in the co-culture, using a multiplicity of infection (MOI) of 0.5 (1:2 Tv: host cell ratio). On the other hand, Tv lab strain G3 did not kill T-cells under these conditions and demonstrated only minimal killing of B-cells (Fig 1A).
Fig 1. Lymphotoxic activity of Tv.
(A) PBMC and Tv strains TvG3 (laboratory adapted) or TvMSA1132 (clinical isolate) were differentially labeled with CFSE or Cell Tracker Blue, respectively and co-cultured at an MOI of 0.5 for 4 hours. Cells were then stained with anti-CD3 and anti-CD19 to detect T-cells or B-cells, respectively, and lymphocyte death was assessed with flow cytometry analysis. (B) Killing of lymphocytes by TvMSA1132 was assessed as in (A) at the indicated MOI for 4 hours. (C) Killing of lymphocytes by TvMSA1132 was assessed as in (A) at an MOI 0.5 for the indicated period of time. All data in (A-C) are averages with standard deviation of triplicate wells and representative of at least 3 donors/ independent experiments.
Having determined that TvMSA1132 is cytotoxic towards lymphocytes, we next addressed the efficiency and kinetics of Tv lymphotoxic activity. The amount of Tv needed to lyse lymphocytes was determined by performing the cytotoxicity assay at various MOI. We found moderate levels of lymphocyte death occurring at MOI of 0.25 (1:4, Tv: host cells), whereas at MOI 2 (2:1, Tv: host cell), we found almost complete killing of B-cells and ~75% killing of T-cells (Fig 1B). Lymphocyte killing requires live parasites, as co-cultures containing dead, intact Tv at the same MOI did not result in any lymphocyte death (S3 Fig). Next, we determined how fast Tv killing of lymphocytes occurs by performing cytotoxicity assays at an intermediate MOI (0.5), and assessing lymphocyte death at various time points during the co-culture. We found that lymphocyte death was not rapid, and required 2 hours to achieve low levels, and 5–6 hours to achieve relatively high levels of death (Fig 1C). Using TvMSA1132 as a model clinical strain, these data indicate that some clinical strains of Tv possess lymphotoxic activity and require several hours and high parasite titers to achieve maximal killing; nevertheless moderate lymphotoxic effects are observed at shorter time points and lower parasite titers. Also, while there was some donor-to-donor variability in susceptibility to Tv cytotoxicity, B-cells were significantly more susceptible (S4A Fig).
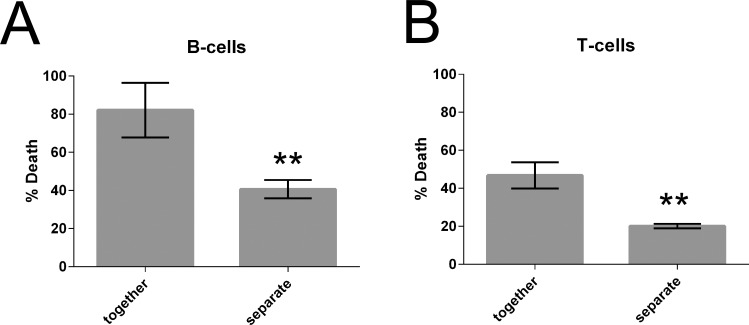
Tv likely comes into direct contact with lymphocytes at the luminal side of the vaginal mucosa and also in the lamina propria after tissue invasion associated with lysis of the epithelial layer. However, Tv killing of lymphocytes could have an extended effect in tissues if it were mediated by soluble factors. We therefore asked whether Tv lymphotoxic activity was contact-dependent, or mediated by soluble factors by performing our cytotoxicity assays utilizing a trans-well insert system with a 0.4 μm porous membrane. As Tv is 7–10 μm in diameter, the parasite cannot pass through [2]. In conditions where PBMC and Tv were cultured together, death of T-cells and B-cells was observed at levels similar to that shown in Fig 1. However, when Tv and PBMC were placed in separate chambers there was an approximately 2-fold decrease in death of T-cells and B-cells (Fig 2A and 2B). The significant difference in lymphotoxic activity observed when parasite and lymphocytes were in the same chamber or separated by a membrane indicates that killing of B-cells and T-cells by Tv is mediated by both contact dependent and soluble factors.
Fig 2. Tv lymphotoxic activity is mediated by contact dependent and soluble factors.
PBMC and TvMSA1132 were co-cultured and lymphocyte death was assessed as described in Fig 1 at an MOI of 0.5 for 4 hours in a transwell apparatus. PBMC were placed in the bottom chamber and TvMSA1132 were placed either with PBMC in the bottom chamber (together) or in a top chamber with shared media, but separated by a 0.4 μm porous membrane (separate). Percent death in the bottom chamber was then assessed for B-cells (A) and T-cells (B). Data shown are averages of triplicate wells with standard deviation, and are representative of 4 donors and 2 independent experiments.
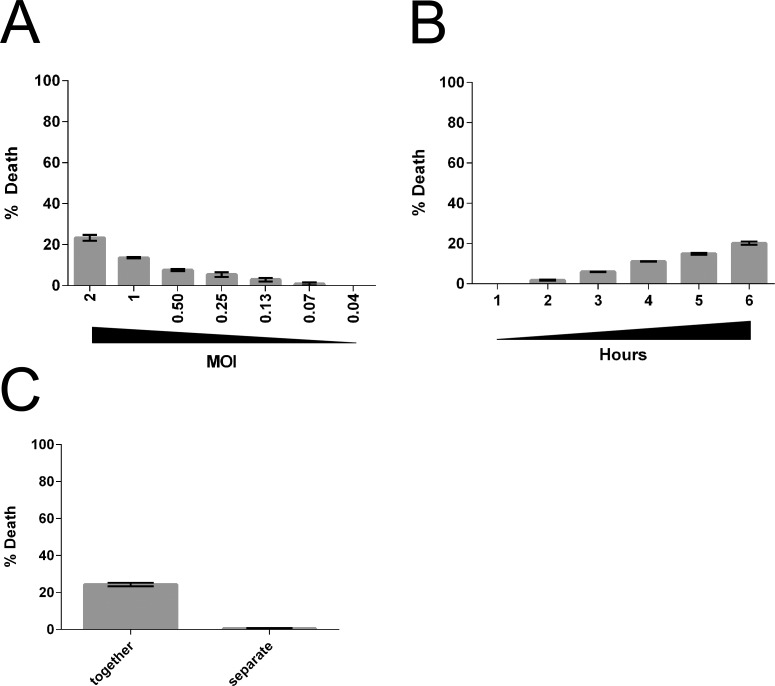
We next asked whether Tv can lyse monocytes. To avoid variability arising from adherence of activated monocytes to plastic, we measured levels of lactate dehydrogenase (LDH) released in the culture supernatants upon lysis of monocytes, instead of using flow cytometry. Tv killing of monocytes was found to be inefficient, with only ~20% death of monocytes observed at an MOI of 2 (2 Tv:1 monocyte) (Fig 3A). A 1–6 hour time course was used to assess the kinetics of killing, and death was found to be linear over 6 hours (Fig 3B). It is notable that prolonged co-incubation did not significantly increase monocyte death even after 24 hour. While there was some donor-to-donor variability, Tv killing of monocytes was always less efficient than that of lymphocytes (S4B Fig). To determine whether Tv lysis of monocytes is contact-dependent, cytotoxicity assays were performed using the transwell system. We found that unlike that observed for killing of lymphocytes (Fig 2), separation of Tv from monocytes almost completely abolished cytotoxic activity (Fig 3C). Together these data indicate that Tv killing of monocytes is inefficient and primarily contact-dependent.
Fig 3. Tv cytotoxicity towards monocytes is inefficient and contact-dependent.
(A) Primary human monocytes were co-cultured with TvMSA1132 at the indicated MOI. Monocyte death was assessed by detecting the release of mammalian lactate dehydrogenase (LDH) into culture supernatants after 4 hours. (B) Primary human monocytes were co-cultured with TvMSA1132 at MOI 0.5 for the indicated times and percent death was determined. (C) Killing of monocytes by TvMSA1132 at an MOI of 2 was determined using a transwell apparatus as described in Figure legend 2, except monocytes were used instead of lymphocytes. LDH was measured in culture supernatants after 4 hours. All data in shown (A-C) are averages of triplicate wells with standard deviation, and are representative of at least 3 donors/independent experiments.
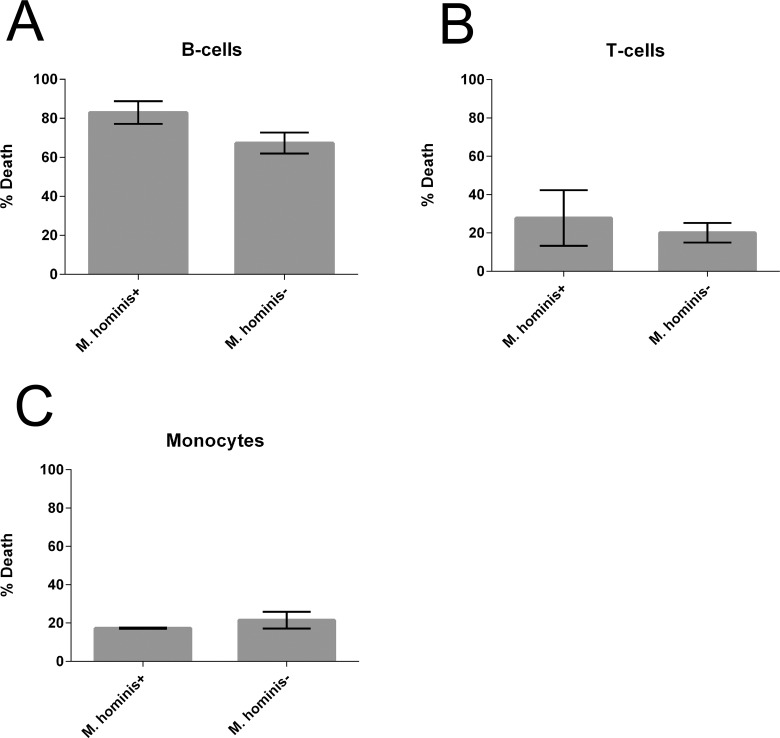
Since symbionts often increase fitness of their hosts, we next asked whether a common symbiont of Tv, M. hominis, affects the ability of Tv to kill leukocytes. TvMSA1132 naturally contains M. hominis, thus to generate isogenic strains that either harbor the symbiont or not, we cultured TvMSA1132 for 1 week either untreated, or in the presence of chloramphenicol and tetracycline. PCR using M. hominis-specific primers was then conducted to confirm that M. hominis was undetectable in the culture treated with additional antibiotics (S5 Fig). Furthermore, sequencing the products generated by PCR using universal 16S bacterial primers on our untreated cultures confirmed that M. hominis is the only bacterial species present in the untreated culture. We then used the untreated (M. hominis+) and antibiotic treated (M. hominis-) strains side-by-side in leukocyte cytotoxicity assays. We found that the ability to kill T-cells, B-cells or monocytes was not significantly different, indicating that M. hominis does not confer greater leukotoxic activity to Tv (Fig 4A–4C).
Fig 4. Tv symbiont Mycoplasma hominis does not affect Tv leukotoxic activity.
Killing of B-cells (A), T-cells (B), or monocytes (C) by TvMSA1132 was determined at an MOI 0.5 for 4 hours. Prior to the cytotoxicity assay, TvMSA1132 was either cultured in the presence (M. hominis -) or absence (M. hominis +) of additional antibiotics. Data shown are average of triplicate wells with standard deviation, and are representative of 3 donors/ independent experiments.
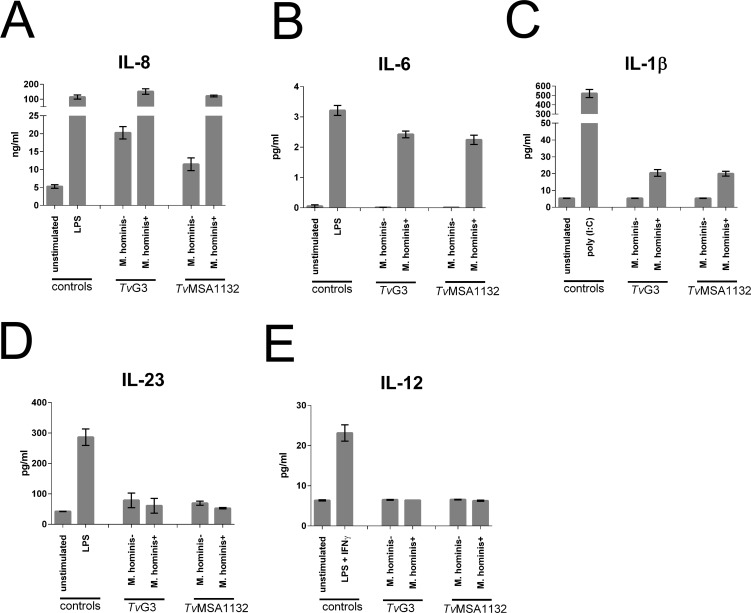
Having observed that Tv is potentially able to modulate immune responses by killing lymphocytes, we next asked the converse question: what type of immune response is mounted against Tv? To address this, we assayed for the presence of several cytokines secreted from primary human monocytes after overnight exposure to Tv. To prevent Tv killing of monocytes from affecting the results, we made dead, intact preparations of Tv before co-culture and confirmed that no monocyte death occurred after incubation with dead Tv. Fiori and colleagues recently showed that M. hominis dramatically increased the amount of pro-inflammatory cytokine induced from a human macrophage-like cell line [38]. We were able to reproduce these results using primary human monocyte derived macrophages (HMDM) (S6 Fig). We therefore compared cytokine responses induced from untreated (M. hominis+) or additional antibiotic treated (M. hominis-) strains using fresh, naïve human monocytes. We also compared the responses against the laboratory adapted (TvG3) versus the clinical (TvMSA1132) strain. Levels of cytokines known to support Th1 responses (IL-12) and Th17 responses (IL-6, IL-1β, and IL-23) were assessed. IL-8, a broadly inflammatory, neutrophil-recruiting chemokine previously reported to be highly secreted following Tv encounter [31,32,37] was also measured. All strains of Tv tested induced IL-8 secretion over background (Fig 5A). Notably, the presence of M. hominis greatly increased IL-8 induction, relative to isogenic strains lacking M. hominis (Fig 5A), and enabled induction of IL-6 and IL-1β which were otherwise not detectable in response to Tv alone (Fig 5B and 5C). In contrast, neither M. hominis positive nor negative parasites induced detectable IL-23 or IL-12 secretion (Fig 5D and 5E). No difference was observed in the immunogenicity of laboratory-adapted strain TvG3 compared to clinical strain TvMSA1132 (Fig 5A–5E). Together these analyses indicate that IL-8 is the dominant cytokine response to Tv, both in the presence and absence of M. hominis. The data also show that the symbiont M. hominis greatly increases the induction of inflammatory cytokines IL-6 and IL-1β, in addition to IL-8. This increased immunogenicity may be instrumental in triggering adaptive immune responses that would not normally be mounted against Tv in the absence of the symbiont.
Fig 5. Induction of cytokine secretion from human monocytes by Tv is largely dependent on the presence of Mycoplasma hominis and is dominated by IL-8 secretion.
Primary human monocytes were cultured with either dead intact TvG3, TvMSA1132, unstimulated, or treated with LPS (A, B, D) or poly (I:C) (C) or LPS and IFNγ (E) for 16 hours. Prior to killing, Tv strains were either untreated (M. hominis+) or treated with additional antibiotic to clear the symbiont (M. hominis-). Supernatants were collected and the indicated cytokines were measured using Cytometric Bead Array (CBA) or ELISA. Data shown are average of triplicate wells with standard deviation, and are representative of 3 donors/ independent experiments.
Discussion
Despite the numerous inflammatory complications associated with Tv infection, how Tv interacts with the cells of the host immune system is not well characterized. Furthermore, partner re-infection after treatment for trichomoniasis indicates a lack of effective adaptive immunity to Tv. Using primary human leukocytes, we have demonstrated that Tv has leukotoxic activity, that IL-8 secretion dominates the primary cytokine response to Tv infection, and that the M. hominis symbiont is likely to play a major role in shaping more robust and diverse inflammatory responses to Tv. These results form a foundation for the dissection of interactions between Tv and the cells of the human immune system. These studies are the first to examine how primary human leukocytes respond to Tv, and to assess Tv leukotoxic activity, with attention to strain specificity, host cell-preference, timing, and dosage. These analyses have also interrogated the contribution of the symbiont M. hominis to the pathogenesis and immunogenicity of Tv using primary immune cells. We found that immune responses against Tv may be modulated by leukotoxic activity of the parasite as well as the presence of M. hominis. These results suggest potential explanations for the considerable variability in Tv clinical presentation, pathogenicity, and inflammatory sequelae.
The leukotoxic activity of Tv reported here may be important in subverting immune responses, or in modulating the leukocyte repertoire in the vaginal mucosa, where leukocytes may control concomitant STIs and commensal micro-organisms [41]. We sought to determine which cells among PBMC are primary targets of the parasite and found that Tv demonstrates a preference for killing B-cells, followed by T-cells, and is very inefficient at killing monocytes. Interestingly, while the cell-type preference was maintained in all donors tested, there was some variability in overall susceptibility of leukocytes to Tv- mediated killing (S4 Fig), which could account for variation in symptoms and sequelae in the clinic. It is interesting that B-cells are the most vulnerable leukocyte in the presence of Tv, as humoral immunity is likely to be important in host defense against Tv: a large extracellular eukaryotic pathogen. Antibodies against Tv can be detected in sera and vaginal washes of infected individuals [1,34,50], indicating that humoral immunity is formed against the parasite. Furthermore, Tv strains that do not harbor the symbiont M. hominis do not induce detectable levels of IL-1β, IL-6 or IL-12 secretion from monocytes (Fig 5B, 5C and 5E), suggesting formation of default Th2 responses to Tv, at least in the absence of symbiont M. hominis. Since ~50% Tv clinical isolates lack M. hominis [27,30], Th2 responses could predominate in these cases. Killing of antibody-producing B-cells (such as those at the mucosa secreting IgA [51] could therefore be a way for the parasite to subvert immune clearance. Interestingly, Tv proteases are reported to cleave IgG and secretory IgA [52] and Tv exhibits antigenic variation [53], both consistent with a model of humoral immunity subversion as an evolved behavior of Tv to survive in its host. We also found that approximately 50% of Tv leukotoxic activity against B-cells was mediated by soluble factors, indicating that the parasite may kill B-cells even if it does not come into direct contact with them, potentially allowing for a broader effect of this anti-B cell activity. Contact dependent killing was also observed, consistent with previous work showing that human PBMC can be phagocytosed by Tv [54].
Moderate cytotoxic activity of Tv against T-cells was also detected, albeit lower than that exhibited towards B-cells, again mediated by both contact-dependent and soluble factors (Figs 1 and 2). Tv-antigen-induced proliferation of PBMC from infected women [36] indicates that T-cell responses are formed against Tv in vivo. Tv killing of T-cells could therefore potentially subvert anti-Tv immune responses as well as affect the T-cell repertoire in the such that control of concomitant STIs or commensals is dysregulated. Indeed, Tv infection is associated with dysbiosis of microbiota in the FRT and bacterial vaginosis [55–57]. Since T-cell polarization is a delicate and multi-factorial process involving both positive and negative feedback, Tv killing of T-cells could have more complex downstream implications in anti-Tv immunity, on other vaginal microflora, and on mucosal inflammation.
We observed both contact-dependent and contact-independent leukotoxic activity for the clinical isolate TvMSA1132. Previously demonstrated phagocytosis of leukocytes [42] could account for or contribute to the contact-dependent leukotoxic activity observed. Alternatively, the cytotoxicity could be mediated almost entirely by soluble factors, but require close proximity; concentrations of pH and secreted effectors being effectively higher in such a microenvironment. Contact-independent killing of leukocytes by Tv has not been previously described. However soluble, extracellular Tv cysteine proteases have been isolated [58,59] and several studies implicate them in Tv cytolytic mechanisms [60–63]. In addition, several genes with homology to known pore-forming toxins are present in the Tv genome [49]. Future work to determine the identity of soluble factors involved in Tv contact-independent killing of lymphocytes will be important to understand the mechanism underlying this mode of host cell cytotoxicity.
The observation that the recent clinical isolate TvMSA1132 demonstrated dramatically enhanced lymphotoxic activity compared to the common laboratory adapted strain TvG3 (Fig 1A) is notable. We have previously shown that Tv lysis of prostate and vaginal epithelial cells, which is strictly contact-dependent, is highly variable among different Tv strains [2]. Strain differences in contact-independent modes of lysis, as demonstrated here, reveal an added layer of strain variation in pathogenic behavior, underscoring the value of using clinical strains for studies of Tv molecular pathogenesis, and highlighting a likely reason for the considerable clinical variability in trichomoniasis presentation and outcomes. Unfortunately, the clinical symptoms of the patient from which TvMSA1132 was isolated are not available to allow direct comparison of host cell toxicity in vitro with clinical outcomes. Variability between Tv and M. hominis strains and their host cell-specific interactions may also explain why in this study we did not find differences between M. hominis positive and negative Tv cultures in their ability to kill leukocytes (Fig 4), in contrast to the enhancement of epithelial cell lysis conferred to Tv by M. hominis observed by Vancini and colleagues [64]. This further supports a model of diverse mechanisms underlying Tv cytotoxicity that may be strain and host cell type dependent.
In contrast to the efficient killing of lymphocytes by TvMSA1132, monocytes were refractory to killing and the cytotoxicity that was observed was almost exclusively contact-dependent (Fig 3). Variation in the ability of Tv to kill host cells may be dependent on specific host-cell factors that are enriched on epithelial cells [2] and B-cells, and are present at lower levels on T-cells and monocytes. Only one host-cell receptor for mediating Tv interaction with host cells, galectin-1, has been identified. However, knock-down of galectin-1 expression in epithelial cells abrogated only ~20% of Tv adherence, indicating that adherence and contact-dependent cytolysis is a multi-factorial process [44]. Future studies aimed at identifying novel host molecules that confer vulnerability to contact-independent Tv killing will be important to understanding mechanisms of Tv leukotoxic activity.
A lack of robust cytotoxic activity towards monocytes (Fig 3) indicates that Tv does not subvert cytokine secretion from myeloid cells by killing the producers. Rather, cytokine secretion by monocytes is likely to proceed even in the presence of live, active parasites. In agreement with Fiori and colleagues [38] we found cytokine secretion by monocytes to be remarkably affected by the presence of the symbiont M. hominis (Fig 5). The absence of inflammatory cytokine production stimulated from monocytes in the presence of M. hominis-free Tv strains suggests that Th2 responses may be formed in cases where Tv strains are M. hominis negative. As Tv is an extracellular pathogen, and no IL-12 was induced in response to any Tv strain tested, it seems unlikely that Th1 responses are formed against the parasite. However, in the presence of M. hominis or other bacterial or viral antigens to provide co-stimulation in the milieu in vivo, Th17 responses specific to Tv may form. In humans, IL-1β, IL-6, and IL-23 support the formation or persistence of Th17 cells [65]. We saw that IL-1β and IL-6 were stimulated by M. hominis-infected Tv. In contrast to that observed by Fiori et al., we did not detect significantly high amounts of IL-23 in response to M. hominis + Tv, which potentially highlights a difference between the THP-1 macrophage cell line that Fiori et al. used and our primary human monocyte system, or that Fiori et al. used live trichomonads as opposed to our use of dead-intact trichomonads as stimulant. Regardless, IL-23 could be present in in vivo milieus as a result of other commensals or concomitant STIs. Indeed, IL-17 has been shown to be a major player in the immune response against the related parasite Giardia lamblia [66–68], and IL-22, a common cytokine associated with Th17 responses has been detected in vaginal secretions from Tv infected patients [69]. Th17 responses are common in the mucosa, where they respond to extracellular pathogens by recruiting neutrophils and repairing damaged epithelia [70,71], consistent with FRT neutrophilia and epithelial damage associated with Tv infection.
The commensal lactobacilli, dominant in ~75% of women’s vaginal microbiomes, have been shown to modulate Tv pathogenic properties in vitro [72]; it is conceivable that moieties present on commensal bacteria sharing a niche with Tv could additionally affect cytokine responses during Tv infection. Recently, additional Mycoplasma species associated with clinical strains of Tv have been discovered [73]. Known symbionts, commensals, and concomitant STIs are likely only the “tip-of-the-iceberg;” many other yet undefined organisms may contribute to the complex ecosystem with which Tv co-operates and contends. Meta-analysis of the FRT microbiome in the context of Tv infection, as well as development of suitable in vivo models will be instrumental to more fully appreciate this diversity and test hypotheses about Tv clearance and inflammation with a more holistic approach.
We found that both Tv strains examined, regardless of M. hominis status, induce IL-8 secretion (Fig 5) [1,31,32,37]. IL-8 is a pleiotropic cytokine [74], with a main function of recruiting neutrophils, consistent with that observed in trichomoniasis in the clinic. Furthermore, work in mouse models has shown that prevention of neutrophil influx is needed to establish infection [43], and primary human neutrophils were shown to swarm and attack Tv in vitro [32] suggesting that neutrophils are crucial for control of Tv infection. However, the molecular determinants of neutrophil-Tv interactions are not characterized. Neutrophils have a range of highly inflammatory and destructive behaviors [75], and can even contribute to cancer microenvironments [74]. It is possible that neutrophils may contribute to the associations of reproductive complications, inflammatory pathologies, and cancers of the reproductive tract with Tv.
These studies shed light on potential reasons for variability in Tv clinical presentation and associated complications, suggest potential immune subversion strategies of the parasite, and may help to inform future immunotherapy interventions. A better understanding of how Tv interacts with the immune system will also potentiate the design of immunotherapies to aid in scenarios of antibiotic resistance or to mitigate damaging inflammatory processes induced by Tv infections.
Supporting Information
(Top panels) Total wells were analyzed for forward scatter vs. side scatter and beads, and live cells were gated on. Beads were further gated based on A-405 positivity to more accurately ensure their identity. (Middle panels) Live cells were further sub-gated based on CFSE+ to gate on leukocytes only (Tv excluded). (Bottom panels) Leukocytes were then further gated based on CD19 and CD3 positivity to identity B-cells and T-cells, respectively.
(TIF)
Total PBMC from live cell gates (shown in S1 Fig) were analysed for Zombie Red expression to rule out that significant T-cells or B-cells occurring in live cell gates had compromised membranes.
(TIF)
To assure that PBMC death observed after co-cultures with Tv was specific to live Tv-mediated mechanisms, we co-cultured PBMC with dead, intact Tv as a control. We did not observe any decrease in counts of viable PBMC after co-culture with dead, intact Tv. Data shown are from Tv co-culture with PBMC at MOI 0.5 for 4 hours and representative of multiple experiments.
(TIF)
% death is shown for all donors used in the study, at MOI 0.5 TvMSA1132 for 4 hours. B-cell versus T-cell susceptibility was compared using paired (donor-matched), student’s T-test.
(TIF)
Chloramphenicol/ tetracycline treated (TvMSA1132 Cm/Tet) parasites were analyzed for the presence of bacterial symbionts using universal 16S primers designed to amplify a conserved region of bacterial 16S rDNA. The designed primers amplify a fragment of 834 bp. (Cm: chloramphenicol; Tet: tetracycline) specifically in TvMSA1132 untreated parasites. DNA sequencing of the uncloned, amplified 16S bacterial rDNA fragment from untreated TvMSA1132 was analyzed by BLAST analyses of Genbank. Only one sequence, with 100% homology to 16S region of M. hominis was detected. The sequence matched the following accession numbers with 100% identity: (all strains of M. hominis) CP009652.1, JN935871.1, NR113679.1, NR041881.1, FP236530.1, AF443616.3, AF443617.3, AJ002268.1, AJ002267.1, AJ002266.1, and AJ002265.1.
(TIF)
(A) Differentiation of human monocytes to macrophages (HMDM) was verified by the expression of CD14 and the increase in size. (B) HMDM were either unstimulated, treated with LPS, or cultured with heat-inactivated TvG3 for 16 hours. Supernatants were collected and the indicated cytokines were measured using CBA. Data shown are average of triplicate wells with standard deviation, and are representative of 3 donors/ independent experiments.
(TIF)
Acknowledgments
We would like to thank Deborah Anisman-Posner and Irene Kim at the UCLA virology core for recruiting blood donors and processing buffy coats. We also thank Felicia Codrea and Jessica Scholes at the Eli and Edith Broad Flow Cytometry Core facility at UCLA for training and technical expertise. We thank our colleagues Drs. Brian Janssen, Angelica Riestra, Olivia Twu, and Sharon Alterzon for helpful comments and discussions, Drs. Melissa Conrad and Jane Carlton for sharing information about Mycoplasma hominis status of their T. vaginalis isolates and Drs. Linda Baum and Dusan Bogunovic for advice on HMDM differentiation. We also thank Dr. Stephen Rawlings for comments on the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by National Institutes of Health Grant R01AI103182 (PJJ) and F32AI122643 (FM). FGID and YPC were supported by the Microbial Pathogenesis Training Grant (T32-AI07323), and BMM was supported by the Cellular & Molecular Training Grant (T32GM007185). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Schwebke JR, Burgess D (2004) Trichomoniasis. Clin Microbiol Rev 17: 794–803, table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lustig G, Ryan CM, Secor WE, Johnson PJ (2013) Trichomonas vaginalis contact-dependent cytolysis of epithelial cells. Infect Immun 81: 1411–1419. 10.1128/IAI.01244-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Midlej V, Benchimol M (2010) Trichomonas vaginalis kills and eats—evidence for phagocytic activity as a cytopathic effect. Parasitology 137: 65–76. 10.1017/S0031182009991041 [DOI] [PubMed] [Google Scholar]
- 4.Meade JC, Carlton JM (2013) Genetic diversity in Trichomonas vaginalis. Sex Transm Infect 89: 444–448. 10.1136/sextrans-2013-051098 [DOI] [PubMed] [Google Scholar]
- 5.McClelland RS (2008) Trichomonas vaginalis infection: can we afford to do nothing? J Infect Dis 197: 487–489. 10.1086/526498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fichorova RN (2009) Impact of T. vaginalis infection on innate immune responses and reproductive outcome. J Reprod Immunol 83: 185–189. 10.1016/j.jri.2009.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shafir SC, Sorvillo FJ, Smith L (2009) Current issues and considerations regarding trichomoniasis and human immunodeficiency virus in African-Americans. Clin Microbiol Rev 22: 37–45, Table of Contents. 10.1128/CMR.00002-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grossman JH 3rd, Galask RP (1990) Persistent vaginitis caused by metronidazole-resistant trichomonas. Obstet Gynecol 76: 521–522. [PubMed] [Google Scholar]
- 9.Dunne RL, Dunn LA, Upcroft P, O'Donoghue PJ, Upcroft JA (2003) Drug resistance in the sexually transmitted protozoan Trichomonas vaginalis. Cell Res 13: 239–249. [DOI] [PubMed] [Google Scholar]
- 10.Land KM, Johnson PJ (1999) Molecular basis of metronidazole resistance in pathogenic bacteria and protozoa. Drug Resist Updat 2: 289–294. [DOI] [PubMed] [Google Scholar]
- 11.Upcroft JA, Dunn LA, Wal T, Tabrizi S, Delgadillo-Correa MG, et al. (2009) Metronidazole resistance in Trichomonas vaginalis from highland women in Papua New Guinea. Sex Health 6: 334–338. 10.1071/SH09011 [DOI] [PubMed] [Google Scholar]
- 12.Leitsch D, Janssen BD, Kolarich D, Johnson PJ, Duchene M (2014) Trichomonas vaginalis flavin reductase 1 and its role in metronidazole resistance. Mol Microbiol 91: 198–208. 10.1111/mmi.12455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gulmezoglu AM, Azhar M (2011) Interventions for trichomoniasis in pregnancy. Cochrane Database Syst Rev: CD000220 10.1002/14651858.CD000220.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okun N, Gronau KA, Hannah ME (2005) Antibiotics for bacterial vaginosis or Trichomonas vaginalis in pregnancy: a systematic review. Obstet Gynecol 105: 857–868. [DOI] [PubMed] [Google Scholar]
- 15.Hirt RP, Sherrard J (2015) Trichomonas vaginalis origins, molecular pathobiology and clinical considerations. Curr Opin Infect Dis 28: 72–79. 10.1097/QCO.0000000000000128 [DOI] [PubMed] [Google Scholar]
- 16.Gram IT, Macaluso M, Churchill J, Stalsberg H (1992) Trichomonas vaginalis (TV) and human papillomavirus (HPV) infection and the incidence of cervical intraepithelial neoplasia (CIN) grade III. Cancer Causes Control 3: 231–236. [DOI] [PubMed] [Google Scholar]
- 17.Boyle DC, Smith JR (1999) Infection and cervical intraepithelial neoplasia. Int J Gynecol Cancer 9: 177–186. [DOI] [PubMed] [Google Scholar]
- 18.Yap EH, Ho TH, Chan YC, Thong TW, Ng GC, et al. (1995) Serum antibodies to Trichomonas vaginalis in invasive cervical cancer patients. Genitourin Med 71: 402–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayed el-Ahl SA, el-Wakil HS, Kamel NM, Mahmoud MS (2002) A preliminary study on the relationship between Trichomonas vaginalis and cervical cancer in Egyptian women. J Egypt Soc Parasitol 32: 167–178. [PubMed] [Google Scholar]
- 20.Zhang ZF, Graham S, Yu SZ, Marshall J, Zielezny M, et al. (1995) Trichomonas vaginalis and cervical cancer. A prospective study in China. Ann Epidemiol 5: 325–332. [DOI] [PubMed] [Google Scholar]
- 21.Sena AC, Miller WC, Hobbs MM, Schwebke JR, Leone PA, et al. (2007) Trichomonas vaginalis infection in male sexual partners: implications for diagnosis, treatment, and prevention. Clin Infect Dis 44: 13–22. [DOI] [PubMed] [Google Scholar]
- 22.Mitteregger D, Aberle SW, Makristathis A, Walochnik J, Brozek W, et al. (2012) High detection rate of Trichomonas vaginalis in benign hyperplastic prostatic tissue. Med Microbiol Immunol 201: 113–116. 10.1007/s00430-011-0205-2 [DOI] [PubMed] [Google Scholar]
- 23.Stark JR, Judson G, Alderete JF, Mundodi V, Kucknoor AS, et al. (2009) Prospective study of Trichomonas vaginalis infection and prostate cancer incidence and mortality: Physicians' Health Study. J Natl Cancer Inst 101: 1406–1411. 10.1093/jnci/djp306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benchimol M, Rosa ID, Fontes RD, Dias AJB (2008) Trichomonas adhere and phagocytose sperm cells: adhesion seems to be a prominent stage during interaction. Parasitology Research 102: 597–604. [DOI] [PubMed] [Google Scholar]
- 25.Sutcliffe S, Neace C, Magnuson NS, Reeves R, Alderete JF (2012) Trichomonosis, a common curable STI, and prostate carcinogenesis—a proposed molecular mechanism. PLoS Pathog 8: e1002801 10.1371/journal.ppat.1002801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144: 646–674. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 27.Rappelli P, Addis MF, Carta F, Fiori PL (1998) Mycoplasma hominis parasitism of Trichomonas vaginalis. Lancet 352: 1286 [DOI] [PubMed] [Google Scholar]
- 28.Vancini RG, Benchimol M (2008) Entry and intracellular location of Mycoplasma hominis in Trichomonas vaginalis. Arch Microbiol 189: 7–18. [DOI] [PubMed] [Google Scholar]
- 29.Dessi D, Delogu G, Emonte E, Catania MR, Fiori PL, et al. (2005) Long-term survival and intracellular replication of Mycoplasma hominis in Trichomonas vaginalis cells: potential role of the protozoon in transmitting bacterial infection. Infect Immun 73: 1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.da Luz Becker D, Dos Santos O, Frasson AP, de Vargas Rigo G, Macedo AJ, et al. (2015) High rates of double-stranded RNA viruses and Mycoplasma hominis in Trichomonas vaginalis clinical isolates in South Brazil. Infect Genet Evol 34: 181–187. 10.1016/j.meegid.2015.07.005 [DOI] [PubMed] [Google Scholar]
- 31.Shaio MF, Lin PR, Liu JY, Tang KD (1994) Monocyte-derived interleukin-8 involved in the recruitment of neutrophils induced by Trichomonas vaginalis infection. J Infect Dis 170: 1638–1640. [DOI] [PubMed] [Google Scholar]
- 32.Rein MF, Sullivan JA, Mandell GL (1980) Trichomonacidal activity of human polymorphonuclear neutrophils: killing by disruption and fragmentation. J Infect Dis 142: 575–585. [DOI] [PubMed] [Google Scholar]
- 33.Twu O, Dessi D, Vu A, Mercer F, Stevens GC, et al. (2014) Trichomonas vaginalis homolog of macrophage migration inhibitory factor induces prostate cell growth, invasiveness, and inflammatory responses. Proc Natl Acad Sci U S A 111: 8179–8184. 10.1073/pnas.1321884111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ton Nu PA, Rappelli P, Dessi D, Nguyen VQ, Fiori PL (2015) Kinetics of circulating antibody response to Trichomonas vaginalis: clinical and diagnostic implications. Sex Transm Infect. [DOI] [PubMed] [Google Scholar]
- 35.Smith JD, Garber GE (2015) Trichomonas vaginalis Infection Induces Vaginal CD4+ T-Cell Infiltration in a Mouse Model: A Vaccine Strategy to Reduce Vaginal Infection and HIV Transmission. J Infect Dis 212: 285–293. 10.1093/infdis/jiv036 [DOI] [PubMed] [Google Scholar]
- 36.Mason PR, Patterson BA (1985) Proliferative response of human lymphocytes to secretory and cellular antigens of Trichomonas vaginalis. J Parasitol 71: 265–268. [PubMed] [Google Scholar]
- 37.Shaio MF, Lin PR, Liu JY, Yang KD (1995) Generation of interleukin-8 from human monocytes in response to Trichomonas vaginalis stimulation. Infect Immun 63: 3864–3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiori PL, Diaz N, Cocco AR, Rappelli P, Dessi D (2013) Association of Trichomonas vaginalis with its symbiont Mycoplasma hominis synergistically upregulates the in vitro proinflammatory response of human monocytes. Sex Transm Infect 89: 449–454. 10.1136/sextrans-2012-051006 [DOI] [PubMed] [Google Scholar]
- 39.Brotman RM, Ravel J, Bavoil PM, Gravitt PE, Ghanem KG (2014) Microbiome, sex hormones, and immune responses in the reproductive tract: challenges for vaccine development against sexually transmitted infections. Vaccine 32: 1543–1552. 10.1016/j.vaccine.2013.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Givan AL, White HD, Stern JE, Colby E, Gosselin EJ, et al. (1997) Flow cytometric analysis of leukocytes in the human female reproductive tract: comparison of fallopian tube, uterus, cervix, and vagina. Am J Reprod Immunol 38: 350–359. [DOI] [PubMed] [Google Scholar]
- 41.Wira CR, Fahey JV, Sentman CL, Pioli PA, Shen L (2005) Innate and adaptive immunity in female genital tract: cellular responses and interactions. Immunol Rev 206: 306–335. [DOI] [PubMed] [Google Scholar]
- 42.Rendon-Maldonado JG, Espinosa-Cantellano M, Gonzalez-Robles A, Martinez-Palomo A (1998) Trichomonas vaginalis: in vitro phagocytosis of lactobacilli, vaginal epithelial cells, leukocytes, and erythrocytes. Exp Parasitol 89: 241–250. [DOI] [PubMed] [Google Scholar]
- 43.Cobo ER, Eckmann L, Corbeil LB (2011) Murine models of vaginal trichomonad infections. Am J Trop Med Hyg 85: 667–673. 10.4269/ajtmh.2011.11-0123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okumura CY, Baum LG, Johnson PJ (2008) Galectin-1 on cervical epithelial cells is a receptor for the sexually transmitted human parasite Trichomonas vaginalis. Cell Microbiol 10: 2078–2090. 10.1111/j.1462-5822.2008.01190.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark CG, Diamond LS (2002) Methods for cultivation of luminal parasitic protists of clinical importance. Clin Microbiol Rev 15: 329–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zielinski CE, Mele F, Aschenbrenner D, Jarrossay D, Ronchi F, et al. (2012) Pathogen-induced human TH17 cells produce IFN-gamma or IL-10 and are regulated by IL-1beta. Nature 484: 514–518. 10.1038/nature10957 [DOI] [PubMed] [Google Scholar]
- 47.Brooks AE, Parsamand T, Kelly RW, Simoes-Barbosa A (2013) An improved quantitative method to assess adhesive properties of Trichomonas vaginalis to host vaginal ectocervical cells using flow cytometry. J Microbiol Methods 92: 73–78. 10.1016/j.mimet.2012.10.011 [DOI] [PubMed] [Google Scholar]
- 48.Blanchard A, Yanez A, Dybvig K, Watson HL, Griffiths G, et al. (1993) Evaluation of intraspecies genetic variation within the 16S rRNA gene of Mycoplasma hominis and detection by polymerase chain reaction. J Clin Microbiol 31: 1358–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carlton JM, Hirt RP, Silva JC, Delcher AL, Schatz M, et al. (2007) Draft genome sequence of the sexually transmitted pathogen Trichomonas vaginalis. Science 315: 207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaur S, Khurana S, Bagga R, Wanchu A, Malla N (2008) Antitrichomonas IgG, IgM, IgA, and IgG subclass responses in human intravaginal trichomoniasis. Parasitol Res 103: 305–312. 10.1007/s00436-008-0971-y [DOI] [PubMed] [Google Scholar]
- 51.Corthesy B (2013) Multi-faceted functions of secretory IgA at mucosal surfaces. Front Immunol 4: 185 10.3389/fimmu.2013.00185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Provenzano D, Alderete JF (1995) Analysis of human immunoglobulin-degrading cysteine proteinases of Trichomonas vaginalis. Infect Immun 63: 3388–3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alderete JF (1988) Alternating phenotypic expression of two classes of Trichomonas vaginalis surface markers. Rev Infect Dis 10 Suppl 2: S408–412. [DOI] [PubMed] [Google Scholar]
- 54.Pereira-Neves A, Benchimol M (2007) Phagocytosis by Trichomonas vaginalis: new insights. Biol Cell 99: 87–101. [DOI] [PubMed] [Google Scholar]
- 55.Bar AK, Phukan N, Pinheiro J, Simoes-Barbosa A (2015) The Interplay of Host Microbiota and Parasitic Protozoans at Mucosal Interfaces: Implications for the Outcomes of Infections and Diseases. PLoS Negl Trop Dis 9: e0004176 10.1371/journal.pntd.0004176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martin DH, Zozaya M, Lillis RA, Myers L, Nsuami MJ, et al. (2013) Unique vaginal microbiota that includes an unknown Mycoplasma-like organism is associated with Trichomonas vaginalis infection. J Infect Dis 207: 1922–1931. 10.1093/infdis/jit100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.El Sayed Zaki M, Raafat D, El Emshaty W, Azab MS, Goda H (2010) Correlation of Trichomonas vaginalis to bacterial vaginosis: a laboratory-based study. J Infect Dev Ctries 4: 156–163. [DOI] [PubMed] [Google Scholar]
- 58.Garber GE, Lemchuk-Favel LT (1989) Characterization and purification of extracellular proteases of Trichomonas vaginalis. Can J Microbiol 35: 903–909. [DOI] [PubMed] [Google Scholar]
- 59.Garber GE, Lemchuk-Favel LT (1994) Analysis of the extracellular proteases of Trichomonas vaginalis. Parasitol Res 80: 361–365. [DOI] [PubMed] [Google Scholar]
- 60.Alvarez-Sanchez ME, Avila-Gonzalez L, Becerril-Garcia C, Fattel-Facenda LV, Ortega-Lopez J, et al. (2000) A novel cysteine proteinase (CP65) of Trichomonas vaginalis involved in cytotoxicity. Microb Pathog 28: 193–202. [DOI] [PubMed] [Google Scholar]
- 61.Mendoza-Lopez MR, Becerril-Garcia C, Fattel-Facenda LV, Avila-Gonzalez L, Ruiz-Tachiquin ME, et al. (2000) CP30, a cysteine proteinase involved in Trichomonas vaginalis cytoadherence. Infect Immun 68: 4907–4912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Arroyo R, Alderete JF (1989) Trichomonas vaginalis surface proteinase activity is necessary for parasite adherence to epithelial cells. Infect Immun 57: 2991–2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kummer S, Hayes GR, Gilbert RO, Beach DH, Lucas JJ, et al. (2008) Induction of human host cell apoptosis by Trichomonas vaginalis cysteine proteases is modulated by parasite exposure to iron. Microb Pathog 44: 197–203. [DOI] [PubMed] [Google Scholar]
- 64.Vancini RG, Pereira-Neves A, Borojevic R, Benchimol M (2008) Trichomonas vaginalis harboring Mycoplasma hominis increases cytopathogenicity in vitro. Eur J Clin Microbiol Infect Dis 27: 259–267. [DOI] [PubMed] [Google Scholar]
- 65.Schmitt N, Ueno H (2015) Regulation of human helper T cell subset differentiation by cytokines. Curr Opin Immunol 34: 130–136. 10.1016/j.coi.2015.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lopez-Romero GC, Quintero J, Astiazaran-Garcia H, Velazquez C (2015) Host Defences Against Giardia Lamblia. Parasite Immunol. [DOI] [PubMed] [Google Scholar]
- 67.Dann SM, Manthey CF, Le C, Miyamoto Y, Gima L, et al. (2015) IL-17A promotes protective IgA responses and expression of other potential effectors against the lumen-dwelling enteric parasite Giardia. Exp Parasitol 156: 68–78. 10.1016/j.exppara.2015.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dreesen L, De Bosscher K, Grit G, Staels B, Lubberts E, et al. (2014) Giardia muris infection in mice is associated with a protective interleukin 17A response and induction of peroxisome proliferator-activated receptor alpha. Infect Immun 82: 3333–3340. 10.1128/IAI.01536-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Makinde HM, Zariffard R, Mirmonsef P, Novak RM, Jarrett O, et al. (2013) IL-22 levels are associated with Trichomonas vaginalis infection in the lower genital tract. Am J Reprod Immunol 70: 38–44. 10.1111/aji.12100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Littman DR, Rudensky AY (2010) Th17 and regulatory T cells in mediating and restraining inflammation. Cell 140: 845–858. 10.1016/j.cell.2010.02.021 [DOI] [PubMed] [Google Scholar]
- 71.Zenewicz LA, Flavell RA (2011) Recent advances in IL-22 biology. Int Immunol 23: 159–163. 10.1093/intimm/dxr001 [DOI] [PubMed] [Google Scholar]
- 72.Phukan N, Parsamand T, Brooks AE, Nguyen TN, Simoes-Barbosa A (2013) The adherence of Trichomonas vaginalis to host ectocervical cells is influenced by lactobacilli. Sex Transm Infect 89: 455–459. 10.1136/sextrans-2013-051039 [DOI] [PubMed] [Google Scholar]
- 73.Fettweis JM, Serrano MG, Huang B, Brooks JP, Glascock AL, et al. (2014) An emerging mycoplasma associated with trichomoniasis, vaginal infection and disease. PLoS ONE 9: e110943 10.1371/journal.pone.0110943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Waugh DJ, Wilson C (2008) The interleukin-8 pathway in cancer. Clin Cancer Res 14: 6735–6741. 10.1158/1078-0432.CCR-07-4843 [DOI] [PubMed] [Google Scholar]
- 75.Kolaczkowska E, Kubes P (2013) Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 13: 159–175. 10.1038/nri3399 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(Top panels) Total wells were analyzed for forward scatter vs. side scatter and beads, and live cells were gated on. Beads were further gated based on A-405 positivity to more accurately ensure their identity. (Middle panels) Live cells were further sub-gated based on CFSE+ to gate on leukocytes only (Tv excluded). (Bottom panels) Leukocytes were then further gated based on CD19 and CD3 positivity to identity B-cells and T-cells, respectively.
(TIF)
Total PBMC from live cell gates (shown in S1 Fig) were analysed for Zombie Red expression to rule out that significant T-cells or B-cells occurring in live cell gates had compromised membranes.
(TIF)
To assure that PBMC death observed after co-cultures with Tv was specific to live Tv-mediated mechanisms, we co-cultured PBMC with dead, intact Tv as a control. We did not observe any decrease in counts of viable PBMC after co-culture with dead, intact Tv. Data shown are from Tv co-culture with PBMC at MOI 0.5 for 4 hours and representative of multiple experiments.
(TIF)
% death is shown for all donors used in the study, at MOI 0.5 TvMSA1132 for 4 hours. B-cell versus T-cell susceptibility was compared using paired (donor-matched), student’s T-test.
(TIF)
Chloramphenicol/ tetracycline treated (TvMSA1132 Cm/Tet) parasites were analyzed for the presence of bacterial symbionts using universal 16S primers designed to amplify a conserved region of bacterial 16S rDNA. The designed primers amplify a fragment of 834 bp. (Cm: chloramphenicol; Tet: tetracycline) specifically in TvMSA1132 untreated parasites. DNA sequencing of the uncloned, amplified 16S bacterial rDNA fragment from untreated TvMSA1132 was analyzed by BLAST analyses of Genbank. Only one sequence, with 100% homology to 16S region of M. hominis was detected. The sequence matched the following accession numbers with 100% identity: (all strains of M. hominis) CP009652.1, JN935871.1, NR113679.1, NR041881.1, FP236530.1, AF443616.3, AF443617.3, AJ002268.1, AJ002267.1, AJ002266.1, and AJ002265.1.
(TIF)
(A) Differentiation of human monocytes to macrophages (HMDM) was verified by the expression of CD14 and the increase in size. (B) HMDM were either unstimulated, treated with LPS, or cultured with heat-inactivated TvG3 for 16 hours. Supernatants were collected and the indicated cytokines were measured using CBA. Data shown are average of triplicate wells with standard deviation, and are representative of 3 donors/ independent experiments.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.