Abstract
MicroRNAs (miRs) regulate inflammation and BMP antagonists, thus they have potential uses as therapeutic reagents. However, the molecular function of miR-200c in modulating proinflammatory and bone metabolic mediators and osteogenic differentiation is not known. After miR-200c was transduced into a human embryonic palatal mesenchyme (HEPM) (a cell line of preosteoblasts), using lentiviral vectors, the resulting miR-200c overexpression increased osteogenic differentiation biomarkers, including osteocalcin (OCN) transcripts and calcium content. miR-200c expression also down-regulated interleukin (IL)-6, IL-8, and chemokine (C-C motif) ligand (CCL)-5 under lipopolysaccharide (LPS) stimulation and increased osteoprotegerin (OPG) in these cells. miR-200c directly regulates the expression of IL-6, IL-8 and CCL-5 transcripts by binding to their 3’UTRs. A plasmid-based miR-200c inhibitor effectively reduces their binding activities. Additionally, miR-200c delivered using polyethylenimine (PEI) nanoparticles effectively inhibits IL-6, IL-8 and CCL-5 in primary human periodontal ligament fibroblasts and increases the biomarkers of osteogenic differentiation in human bone marrow mesenchymal stem cells (MSCs), including calcium content, ALP, and Runx2. These data demonstrate that miR-200c represses IL-6, IL-8 and CCL-5 and improves osteogenic differentiation. miR-200c may potentially be used as an effective means to prevent periodontitis-associated bone loss by arresting inflammation and osteoclastogenesis and enhancing bone regeneration.
Introduction
It has been reported that approximately half of American adults aged 30 years and older have periodontitis, and the prevalence of periodontitis further increase in aged populations and in patients with diabetes or who smoke [1, 2]. Approximately 50% of periodontitis patients aged 30 years and older have alveolar bone loss that eventually may lead to tooth loss and osseointegration failure of dental implants, if patients do not receive efficient therapeutics to arrest the progression of this chronic disease [2, 3]. Although anti-resorptive and anabolic agents, including vitamin D, calcium, hormone replacements, and bisphosphonates, are currently used to prevent and treat systemic osteoporosis, their efficacy to arrest periodontal bone loss and improve osseointegration of dental implants has not been confirmed [4–6]. Long-term use of intravenous bisphosphonates has been shown to cause osteonecrosis of the jaw [7].
While bacteria-derived factors initiate periodontitis, there is strong evidence that the majority of periodontitis occurs due to activation of host-derived immune and inflammatory defense mechanisms. Toll-like receptors (TLRs) are the major cell-surface initiators of inflammatory responses to pathogens. TLR-2 and TLR4 play critical roles in recognizing periodontal pathogens and trigger the up-regulation of interleukin (IL)-6, IL-1β, and tumor necrosis factor (TNF)-α in periodontitis [8–10]. TLR-mediated signaling pathways also lead to activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), a key proinflammatory transcription factor [11]. These cytokines and transcription factors in turn further amplify the inflammatory response and lead to production of lytic enzymes and stimulate the production of chemokines, including IL-6, IL-8 and CCL-5 [8–10, 12]. Eventually, a cascade of events leads to osteoclastogenesis and subsequent bone resorption via the receptor activator of nuclear factor kappa-B ligand (RANKL)-osteoprotegerin (OPG) axis. Thus, imbalance and dysregulation of proinflammatory molecules and cytokine networks play essential roles in the process of periodontitis and associated bone resorption [8, 9]. Reducing the expression and activation of proinflammatory and bone metabolic mediators that activate osteoclastogenesis and bone resorption may serve as an effective strategy to prevent and arrest the development of periodontal bone loss. Additionally, proinflammatory mediators have been demonstrated to impair bone formation by reducing differentiation of osteoblasts and their progenitor cells [13–18]. Specifically, TNF-α, and IL-1β have been demonstrated to inhibit osteogenic differentiation of bone marrow stem cells. TNF-α also inhibits Osterix expression and promotes Runx2 degradation. TNF-α and IL-17 activate IκB kinase (IKK)-NF-κB to reduce osteogenic differentiation of MSCs and impair bone formation by promoting β-catenin degradation. Thus, inhibiting proinflammatory mediators may prevent and restore periodontitis-associated bone loss.
MicroRNAs (miRs), non-coding small RNAs, actively participate in inflammation by directly degrading and/or silencing the transcription of targeted genes [19–20]. miRs also regulate osteogenic differentiation and bone homeostasis [21]. miR-200c, a member of the miR-200 family, regulates the mesenchymal-to-epithelial transition (MET) [22] and stem cell proliferation and differentiation [23]. miR-200c is significantly downregulated in gingival tissues of periodontitis patients [24] and has been demonstrated to participate in signal pathways mediated by multiple proinflammatory factors and repress the expression and activity of NF-kB [24–27]. In addition, miR-200c has been found to effectively inhibit Noggin, an antagonist of BMP signals, by directly targeting the 3’UTR of Noggin [28]. This evidence strongly suggests that miR-200c may possess the molecular function to both improve osteogenic differentiation and repress periodontitis-associated proinflammatory cytokines.
In this study, we investigated the molecular effects of overexpressed miR-200c using lentiviral vectors on periodontitis-associated proinflammatory factors and the biomarkers of osteogenic differentiation in human embryonic palatal mesenchyme (HEPM) cells, a cell line of preosteoblasts. We found that overexpression of miR-200c in the human preosteoblast cell line effectively suppresses multiple proinflammatory mediators, including IL-6, IL-8, and CCL-5, and increases OPG (an osteoclastogenesis inhibitor) and osteocalcin (OCN) and calcium content. Additionally, we used polyethylenimine (PEI), a non-viral nanoparticle delivery system, to successfully deliver plasmid DNA containing miR-200c into primary human periodontal ligament fibroblasts and bone marrow MSCs. miR-200c delivered using PEI effectively inhibited IL-6, IL-8, and CCL-5 in periodontal ligament fibroblasts and enhanced osteogenic differentiation of human bone marrow MSCs in vitro. We reported that miR-200c directly targets the 3’UTR of IL-6, IL-8 and CCL-5. These data indicate the usefulness of miR-200c in prevention and restoration for periodontitis-induced bone loss, with the ability to modulate inflammation and bone formation.
Materials and Methods
Materials
Plasmids, including psPAX2, pMD2G, and those carrying miR-200c, scrambled miRs, or the empty vector were purchased from Addgene (Cambridge, MA, USA). HEK 293T and HEPM cells were purchased from ATCC (Manassas, VA, USA). The miR inhibitor plasmids were purchased from NaturemiRI (NaturemiRI.com). Primary human bone marrow MSCs and periodontal ligament fibroblasts were purchased from StemCells (Newark, CA, USA) and ScienCell Research Laboratories (Carlsbad, CA, USA), respectively. Taqmen probe and primers for real-time PCR and Sybre Green primers analysis were purchased from Life Technologies and Invitrogen (ThermoFisher Scientific, Waltham, MA, USA). miRNeasy Mini Kits were purchased from QIAGEN (Valencia, CA, USA). Measurements of ALP and calcium were made using kits purchased from AnaSpec (Fremont, CA, USA) and Cayman Chemical (Ann Arbor, MI, USA). All other chemicals and media were purchased from Invitrogen.
Preparation of lentiviral vectors carrying miR-200c
Lentiviral vectors carrying plasmid miR-200c or scrambled miRs were produced by transfecting psPAX2, pMD2G, and plasmid carrying miR-200c or scrambled miRs into HEK 293T cells using a standard CaCl2 method. Briefly, 1.8 μg of psPAX2, 1.2 μg of pMD2G, and 4.2 μg of plasmid miR-200c or scrambled miRs were mixed with 14 μl of 2M CaCl2, and 2 μl of 10mg/ml polybrene in HBS buffer (pH 7.05) to constitute the transfection solution. The transfection solution was then applied to culture plates containing HEK 293T cells at 20–30% confluence, and replaced with fresh medium after 24 hours. Supernatant containing the miR-200c lentivirus was then harvested after 72 hours and filtered through a 0.45-μm sterile syringe.
Transduction of HEPM cells with miR-200c using lentivirus
In order to transduce HEPM cells with plasmid miR-200c or scrambled miRs, the lentiviral vector carrying miR-200c (about 108 TU/ml) was added to a suspension of HEPM cells in a 6-well plate and incubated overnight. The medium was replaced each day for 3 days with fresh medium containing the same amount of lentivirus carrying miR-200c or scrambled miRs. The cells were then collected and sorted by flow cytometry for the presence of green fluorescent protein. The positive cells were analyzed for the proliferation, osteogenic capacity, and proinflammatory mediators.
Analysis of proliferative and osteogenic capacity of HEPM cells
HEPM cells infected with miR-200c or scrambled miRs were cultured in Dulbecco's Modified Eagle Medium (DMEM) containing 10% fetal bovine serum (FBS). To determine the proliferation rate, the cells were placed in 6-well plates at 104 cells/per well and collected after 24, 48 and 72 hours. The doubling time of the cells was measured using the equation: Doubling Time = duration * log (2) / log (Final concentration)—log (Initial concentration). To analyze osteogenic capacity, the cells were cultured 6-well plates at 105 cells/per well with osteogenic medium consisting of DMEM supplemented with 1mM β-glycerophosphate and 0.05 mM ascorbic acid-2-phosphate, for up to 2 weeks. The cells transduced with the scrambled miRs served as controls. Transcripts of OCN were quantified using real-time PCR and calcium content was quantified using Calcium Assay Kits (Cayman, Ann Arbor, MI). Primers and probes were designed using the Primer Express software (Applied Biosystems, Foster City, CA, USA). The primers for OCN were forward: 5”-TAG TGA AGA GAC CCA GGC GC-3”, reverse: 5”-CAC AGT CCG GAT TGA GCT CA-3”, and real-time probes: TGT ATC AAT GGC TGG GAG CCC CAG.
Construction of miR expression and inhibitor plasmids
In order to construct an miR expression plasmid, miR genes were PCR amplified that include approximately 100bp upstream and 100bp downstream sequence flanking the approximately 80bp stem loop sequence. The PCR product was ligated into pSilencer 4.1 vector (Ambion) digested by BamHI and HindIII. The miR inhibitor plasmids was purchased from NaturemiRI (NaturemiRI.com). The construction was established according to our previous studies [29]. Briefly, to construct different designs of miR inhibitors for miR-200c and miR-17-18, we annealed and ligated the miR-200c or miR-17-18 binding sites with a central bulge flanked by different sequences into pLL3.7 vector (Addgene) digested with HpaI and XhoI. To construct the miR inhibitor clone vector, we replaced the miR-200c binding site with two BsmBI sites in the most effective inhibitor design. AscI and PmeI sites were inserted between ApaI and XbaI sites before the U6 promoter. An SmaI site was inserted before XhoI after the polIII terminator. This vector is termed PMIS-empty vector (EV) for plasmid of miR inhibitor. After digestion by BsmBI, pmiRi can be used to clone different miR inhibitors into it after annealing and ligation of different miR binding sites with a central bulge.
Transfection of miR-200c using PEI into primary human cells
Plasmid DNA containing miR-200c was incorporated into PEI to form nanoplexes at an N/P ratio of 10:1 {ratio of the total number of end amine groups (N) of PEI and the total number of DNA phosphate groups (P)} according to our previous studies [30]. Briefly, the complexes were prepared by adding 50μl PEI solution to 50μl miR-200c (10μg) solution and mixed for 30 seconds. The mixture was then incubated at room temperature for 30 minutes to allow complex formation between the positively charged PEI and the negatively charged plasmid DNA. The encapsulation efficiency and plasmid miR-200c condensation within the complex were elucidated using spectrophotometry and gel electrophoresis, respectively as in our previous studies [30]. In order to test the transfection efficiency, primary human periodontal ligament fibroblasts and bone marrow MSCs cultured with DMEM medium were seeded in 6-well plates at 105 cells/well. PEI-miR-200c nanoplexes at different doses (1, 2, 5, and 10μg/per well) were added into the medium of cultured cells. The medium was exchanged after 4 hours to remove extra nanoplexes and the cells with different treatment were continuously cultured using DMEM medium. After 48 hours the cells with different treatment were harvested using Trizol. Total RNA was collected using miRNeasy Mini Kit and cDNA was prepared using the TaqMan microRNA reverse transcription kit. miR-200c transcripts were detected using real-time PCR. The primers and probes of miR-200c were purchased from Life Technologies.
Measurement of proinflammatory mediators
The HEPM cells with miR-200c or scrambled miRs were placed in DMEM medium at 106 cells/per 25cm2 tissue culture flask. For periodontal ligament fibroblasts, the cells were placed in DMEM medium at 105 cells/per well and cultured in 6-well plates and subsequently treated with PEI-miR-200c at different concentrations for 4 hours. The cells treated with the same amount of PEI-empty vector severed as controls. The cells were then cultured in DMEM medium for 48 hours. In order to determine the proinflammatory mediators in HEPM cells and periodontal ligament fibroblasts, the cells were cultured using DMEM with or without lipopolysaccharide (LPS) supplement (1μg/ml) (Lonza N-185). To measure the transcript of proinflammatory mediators, the cells with different treatments were collected after 24 hours. Quantitative real-time PCR was used to measure the transcripts of IL-6, IL-8, and CCL-5. The forward and reverse primers for IL-6 were: 5'- CCA TCT TTG GAA GGT TCA GGT TG -3' and 5'- ACT CAC CTC TTC AGA ACG AAT TG -3'. The primers for IL-8 were: 5'- AAC CCT CTG CAC CCA GTT TTC -3' and 5'- ACT GAG GAT TGA GAG TGG AC -3'. The primers for CCL-5: 5'- TGC CCA CAT CAA GGA GTA TTT -3' and 5'- CTT GCT GTC CCT CTC TCT TTG -3'. To measure the proinflammatory mediators in the supernatant of culture medium, a small portion of culture medium (300μl) from different cells with different treatments was collected at different time points up to 32 hours. Chemokine and cytokine concentrations were measured in cell supernatants using Milliplex immunoassays (Millipore, Billerica, MA USA) as previously described [31]. Cell supernatants (25μl) were incubated with anti-human multi-cytokine magnetic beads at 4°C for 18 hours before removing unbound material using a magnetic plate washer (ELx405TS, BioTek, Winooski, VT, USA). Samples were then incubated with anti-human multi-cytokine biotin reporters for IL-6, IL-8, and CCL5 for one hour at room temperature, streptavidin-phycoerythrin was added, and plates were incubated for an additional 30 minutes. Samples were washed and suspended in sheath fluid before analysis using a Luminex 100 (Austin, TX, USA). Standard curves for each cytokine were prepared from 3.20 to 10,000 pg/ml and concentrations of chemokines and cytokines in each sample were interpolated from standard curves (xPonent v3.1, Luminex, Austin, TX USA; MILLIPLEX Analyst v5.1, Millipore, Billerica, MA, USA). Additionally, we measured IL-6 and IL-8 of non-treated HEPM cells and compared to the cells with miR-200c or scrambled miRs to determine the proinflammatory mediators of HEPM cells varied by miR transfection using lentiviral vectors. Non-treated HEPM cells and the cells with scrambled miRs or miR-200c were treated with DMEM medium supplemented with LPS at 0, 1, 5, and 10 μg/mL. The transcripts of IL-6 and IL-8 in different cells were measured using real-time PCR after 24 hours.
Analysis of osteogenic differentiation of human bone marrow MSCs
Human bone marrow MSCs were placed in DMEM medium at 105 cells/per well in 6-well plates and subsequently treated with PEI-miR-200c at 1μg/per well for 4 hours. The cells were cultured with DMEM medium supplemented with 1mM β-glycerophosphate and 0.05 mM ascorbic acid-2-phosphate, for up to 2 weeks. After the cells were collected and sonicated, the protein level in the lysate was measured using a protein assay kit (Pierce@BCA Protein Assay Kit, Thermo Scientific, Waltham, MA, USA). Biomarkers of osteogenic differentiation, including ALP and calcium, were quantified using SensoLyte® pNPP Alkaline Phosphatase ELISA Assay Kit *Colorimetric* (AnaSpec Inc) and Calcium Assay Kit (Cayman Chemical). Transcripts of ALP and Runx2 were quantified using real-time PCR. The forward and reverse primers and real-time probes for Runx2 were: 5’-CAA CAA GAC CCT GCC CGT-3’, 5’-TCC CAT CTG GTA CCT CTC CG-3’, and 5’-CTT CAA GGT GGT AGC CC-3’. Primers set for ALP were 5’-AGC TGA ACA GGA ACA ACG TGA-3’ and 5’-CTT CAT GGT GCC CGT GGT C-3’.
Luciferase reporter assays
miR-200c was cloned into pSilenser 4.1(Life Technologies). Luciferase reporters were generated by inserting 3’UTR DNA fragments into pGL3 CXCR4 vector (Addgene). All the cloned constructs were confirmed by DNA sequencing. All plasmids used for transfection were purified by double-banding in CsCL. Luciferase, Bgal and protein concentration assay were done as previously described [28]. HEPM cells were cultured in DMEM supplemented with 5% FBS, 1% penicillin/streptomycin, and transfected by electroporation. Cells were fed and seeded in 60 mm dishes 24 hrs prior to transient transfection. Cells were resuspended in PBS and mixed with 2.5μg of expression plasmid, 5μg of reporter plasmid and 0.2μg of SV-40 β-galactosidase plasmid. Transfection was performed by electroporation at 380v and 950μF (Gene Pulser XL, Bio-Rad, Hercules, CA, USA), or using the Lipofectamine 200 transfection reagent (Life Technologies). Transfected cells were incubated in 60mm culture dishes, for 24 hrs unless otherwise indicated, and fed with 10% FBS and DMEM. Following lysis, assays for reporter activity (Luciferase assay, Promega, Madison, WI, USA) as well as for protein content (Bradford assay, Bio-Rad) were carried out. β-galactosidase was measured using the Galacto-Light Plus reagents (Tropix Inc., Bedford, MA, USA) as an internal normalizer. For each assay, all luciferase activity was normalized to the mean value of the first experimental group.
Statistical Analysis
All quantitative data were calculated as means ± standard deviation. The osteogenic differentiation biomarkers and proinflammatory mediators in HEPM cells, human periodontal ligament fibroblasts, and MSCs with overexpressing miR-200c were analyzed by one-way ANOVA with Fisher's LSD post hoc test, using commercially available statistics software (SPSS Inc., Chicago, IL), and p values fewer than 0.05 were considered significant. Each experiment was performed in triplicate.
Results
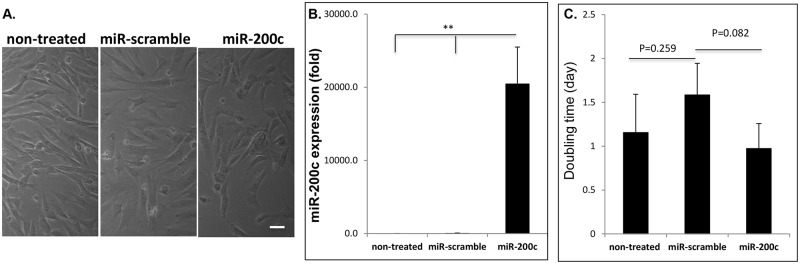
miR-200c expression doesn’t affect cell morphology and proliferation
Lentiviral vectors were used to transfect miR-200c into HEPM cells. The HEPM cells overexpressing miR-200c maintained a fibroblastic morphology compared to the non-treated cells and the cells with scrambled miRs (Fig 1A). The level of miR-200c expression measured using real-time PCR was approximately 2x104-fold higher in HEPM cells infected with miR-200c than in non-treated control cells and the cells transfected with scrambled miRs, while there was limited miR-200c expression in non-treated HEPM cells and the cells with scrambled miRs (Fig 1B). The doubling time for the cells with scrambled miRs was similar to non-treated HEPM cells, and miR-200c-infected HEPM cells did not differ significantly from that in either untreated cells or cells infected with scrambled miRs (Fig 1C).
Fig 1. miR-200c overexpression in HEPM cells and the effects on their proliferation.
A: Microphotographs of HEPM cells and the cells with miR-200c or scrambled miRs under phase-contrast. Bar = 10μm. B: Fold change of miR-200c expression in non-treated HEPM cells and the cells with miR-200c and scrambled miRs. C: The doubling time of non-treated HEPM cells and the cells in the context of miR infection. **: p<0.01.
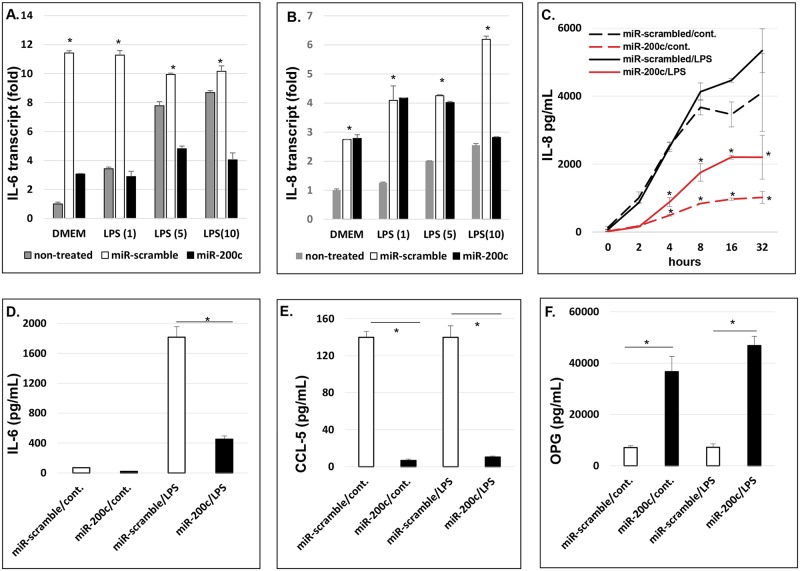
miR-200c modulates proinflammatory mediators and osteogenic differentiation in preosteoblasts
Fig 2A and 2B summarize the transcripts of IL-6 and IL-8 in non-treated HEPM cells, compared to the cells with scrambled miRs or miR-200c. IL-6 and IL-8 in the cells with scrambled miRs were significantly higher than non-treated HEPM cells after LPS treatment at different concentrations (Fig 2A and 2B). This indicates that transfection of miRs using lentiviral vectors may affect the proinflammatory mediators of HEPM cells. Therefore, comparison between HEPM cells transfected with miR-200c to the cells with scrambled miRs would be more reliable and accurate to determine the function of miR-200c overexpression in HEPM cells. We measured the protein concentration of proinflammatory mediators in the supernatant of HEPM cells after HEPM cells transfected with miR-200c or scrambled miRs were cultured with or without LPS supplement (1μg/ml) up to 32 hours. The amounts of IL-8 in the culture medium of the cells with miR-200c overexpression were significantly lower than cells with scrambled miRs at each time point (Fig 2C). Cells were cultured with DMEM containing FBS, which contains cytokines and growth factors; however, we measured relative concentrations of IL-8, IL-6 and CCL-5 compared to controls cells also cultured in FBS. LPS supplement increased the amount of IL-8 in HEPM cells with scrambled miRs starting after 4 hours. However, the cells with miR-200c produced much less IL-8 than that of controls even after they were exposed to LPS (Fig 2C). Similarly, the amount of IL-6 secreted by the cells with miR-200c overexpression in culture medium was lower (3–4 fold) than that of cells with scrambled miRs after 24 hours (Fig 2D). With LPS treatment, IL-6 concentrations in the media are significantly increased, the IL-6 concentration of cells with miR-200c were significantly lower (2–3 fold) than that of cells with scrambled miRs (Fig 2D). In addition, although LPS treatment didn’t effectively increase CCL-5 production in HEPM cells, the cells with overexpression of miR-200c produced significantly lower CCL-5 (approximately 20-fold) than the cells with scrambled miRs (Fig 2E). The amount of OPG secreted by the cells with miR-200c overexpression with or without LPS supplement were higher (6–8 folds) than that of cells with scrambled miRs after 32 hours (Fig 2F). After the non-treated HEPM cells and the cells with miR-200c or scrambled miRs were cultured in DMEM medium supplemented with β-glycerophosphate and ascorbic acid, we observed that OCN transcripts measured using real-time PCR in cells with miR-200c were significantly higher than the non-treated HEPM cells and the cells with scrambled miRs after one week (Fig 3A). The calcium content in miR-200c cells was 3 times higher than that of non-treated cells and the cells with scrambled miRs after two weeks (Fig 3B). There was no difference of OCN and calcium content between non-treated HEPM cells and the cells with scrambled miRs (Fig 3A and 3B).
Fig 2. miR-200c modulates proinflammatory mediators in human preosteoblasts.
A and B: the transcripts of IL-6 (A) and IL-8 (B) in non-treated HEPM cells and the cells with miR-200c or scrambled miRs cultured in DMEM supplemented with LPS at 0, 1, 5 and 10 μg/mL after 24 hours; *:p<0.05 vs non-treated; C: the amounts of IL-8 secreted by HEPM cells with miR-200c or scrambled miRs cultured in DMEM supplemented with or without LPS at different time points; *: p<0.05 vs cells with scrambled miRs; D and E: the amounts of IL-6 (D) and CCL-5 (E) secreted by HEPM cells with miR-200c or scrambled miRs cultured in DMEM supplemented with or without LPS after 24 hrs; F: the amounts of OPG secreted by HEPM cells with different miRs cultured in DMEM supplemented with or without LPS after 32 hours. *: p<0.05.
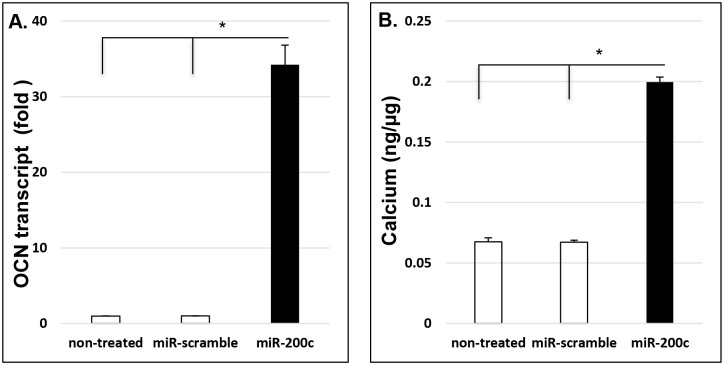
Fig 3. miR-200c increases osteogenic biomarkers in human preosteoblasts.
A and B: the amounts of the transcript of OCN (A) and calcium content (B) in non-treated HEPM cells and the cells with miR-200c or scrambled miRs cultured in DMEM supplemented β-glycerophosphate and ascorbic acid after 1 and 2 weeks, respectively. *: p<0.05.
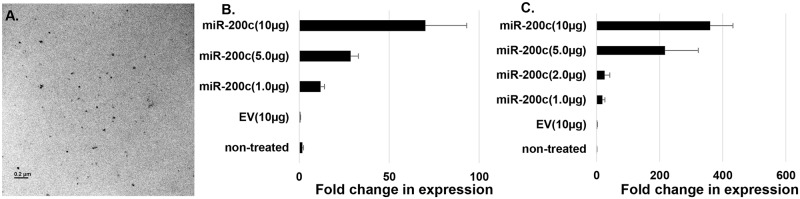
PEI nanoparticles deliver miR-200c to primary human bone marrow MSCs and periodontal ligament fibroblasts
Plasmid miR-200c was incorporated into PEI to form nanoplexes at an N/P ratio of 10:1. PEI-miR-200c nanoplexes were visualized using transmission electron microscope (TEM) (Fig 4A). PEI-miR-200c nanoplexes at 1, 2, 5, and 10 μg/per well were added to the medium of cultured primary human bone marrow MSCs and periodontal ligament fibroblasts in 6-well plates. PEI-empty vector (10 μg/per well) was used as a control. The medium was changed after 4 hours to remove excess nanoplexes and the cells were continuously cultured in DMEM medium. After 2 days miR-200c expression was detected using real-time PCR in periodontal ligament fibroblasts (Fig 4B). miR-200c dose-dependent expression was also observed in human bone marrow MSCs (Fig 4C). The expressions of miR-200c in non-treated periodontal ligament fibroblasts and bone marrow MSCs were similar to that of the cells treated with empty vector.
Fig 4. Intracellular delivery of miR-200c using PEI nanoparticles to human primary periodontal ligament fibroblasts and bone marrow MSCs.
A: TEM image of PEI-miR-200c nanoplexes. B and C: Fold change of the transcript of miR-200c in non-treated human periodontal ligament fibroblasts (B) and bone marrow MSCs (C) and the cells transfected with empty vector (EV) (10μg/per well) and miR-200c (1, 5, 10μg/per well).
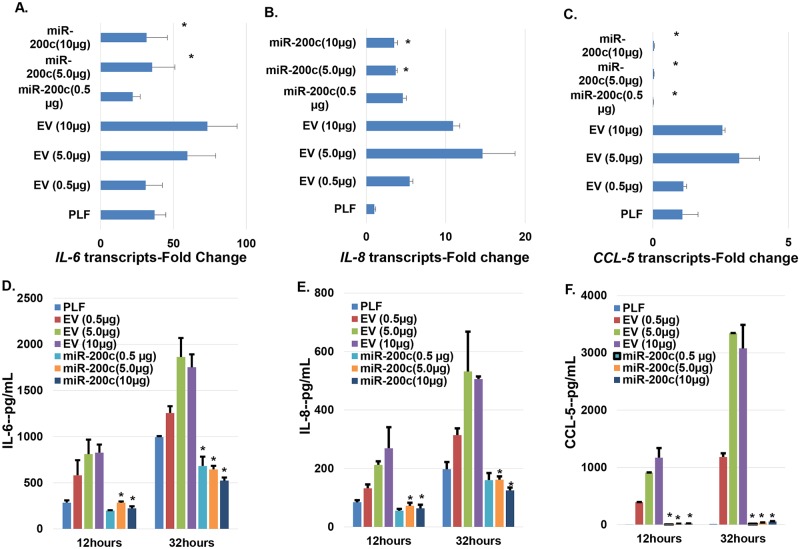
miR-200c delivered using PEI nanoparticles inhibits IL-6, IL-8, and CCL-5 in periodontal ligament cells
After primary human periodontal ligament fibroblasts were treated with PEI-miR-200c at different concentrations, the cells were cultured using DMEM with LPS supplement (1μg/ml) for up to 32 hours. The transcripts levels of IL-8, IL-6 with PEI-miR-200c nanoplex treatment at 5 and 10μg/per well, and CCL-5 at all concentrations in human periodontal ligament cells were lower than that of controls with treatment using the empty vectors at the same concentrations after 24 hours (Fig 5A, 5B and 5C). Furthermore, the concentrations of IL-6, IL-8, and CCL-5 in the supernatant of cells with different treatments after 12 and 32 hours were also decreased after miR-200c nanoplex treatments (Fig 5D, 5E and 5F). Similar to the transcript quantitation, the cell receiving PEI-empty vector at 5 and 10 μg produced higher concentrations of IL-6, IL-8, and CCL-5 compared to control cells without transfection and the increase was statistically significant after 32 hours. However, the protein levels of these mediators in cells treated with PEI-miR-200c were significantly lower than that of cells treated with same concentration of empty vectors. Also, the miR-200c cells had lower levels of IL-6 and IL-8 than control cells without transfection after 32 hours.
Fig 5. miR-200c delivered using PEI nanoparticles inhibits IL-6, IL-8, and CCL-5 in primary human periodontal ligament fibroblasts.
A-C: The transcripts of IL-6 (A), IL-8 (B), and CCL-5 (C) in the cells with miR-200c or empty vector cultured in DMEM supplemented with LPS after 24 hours; D and E: the amounts of IL-6 (D), IL-8 (E), and CCL-5 (F) secreted by the cells with miR-200c or empty vector cultured in DMEM supplemented with LPS after 12 and 32 hrs, respectively. *: p<0.05 vs empty vector with the same amount.
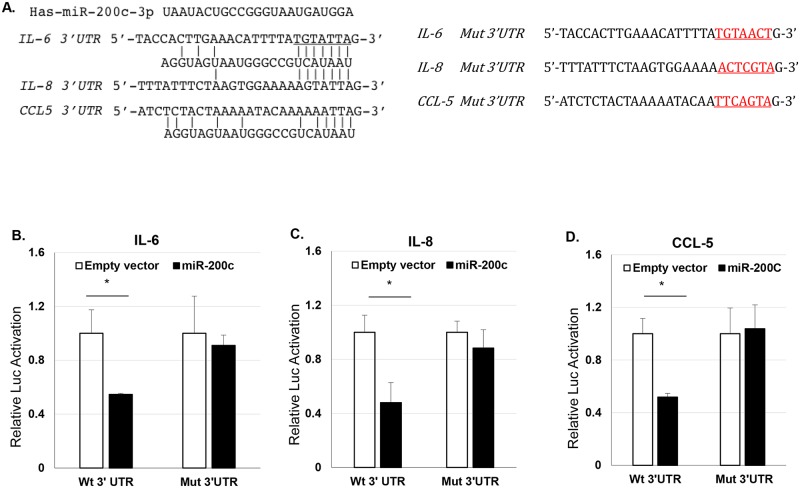
miR-200c directly targets the 3’UTR of IL-6, IL-8, and CCL-5
To test if miR-200c directly targets these mediators the 3’UTR sequence was cloned after the luciferase gene and luciferase activity was determined with and without miR-200c present. The sequence and miR-200c binding region located in the 3’UTR of each mediator is shown in Fig 6A. miR-200c repressed luciferase activity from the IL-6, IL-8 and CCL-5 reporter constructs co-transfected in cells (Fig 6B, 6C and 6D). Normalized luciferase activity of the luciferase reporter with 3’ UTR of IL-6, IL-8, and CCL-5 showed significantly lower with expression of miR-200c compared with the empty plasmid vector. However, there was no loss of luciferase activity when the miR-200c binding sequence was mutated in the 3’UTR of IL-6, IL-8 and CCL-5 (Fig 6).
Fig 6. miR-200c directly targets the 3’UTR of IL-6, IL-8, and CCL-5.
A: The sequence and miR-200c binding region located in the 3’UTR and mutated 3’UTR of IL-6, IL-8, and CCL-5. B-D: Normalized luciferase activities of the 3’ UTR IL-6, IL-8, and CCL-5-luciferase reporters and their 3’UTR-mutated-luciferase reporters treated with empty vector or miR-200c. *: p<0.05.
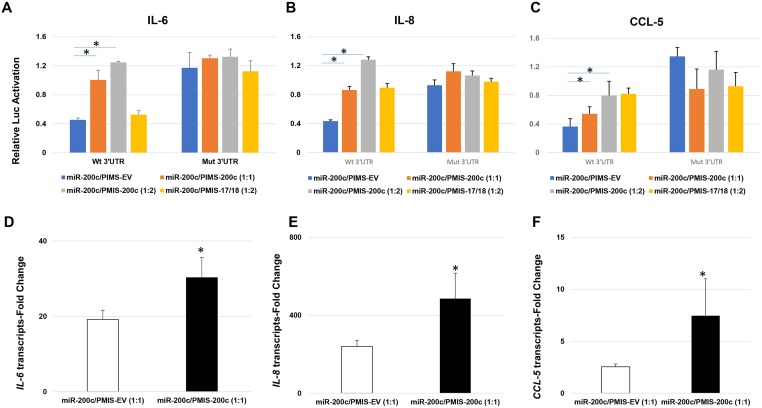
The miR-200c inhibitor restore the activity of miR-200c to IL-6, IL-8, and CCL-5
To further confirm if miR-200c directly targets 3’UTR of these mediators, the luciferase activity inhibited by miR-200c was determined after treatment with a plasmid-base miR inhibitor system (PMIS) designed to bind miR-200c (PMIS-200c). PMIS-200c significantly increased luciferase activity from the luciferase reporter containing the 3’ UTR of IL-6, IL-8, and CCL-5 treated with miR-200c, compared to PMIS designed to bind empty vector (PMIS-EV) or miR-17/18 (PMIS-17/18). However, there was less change of luciferase activity when the mutated sequence in the 3’UTR of IL-6, IL-8 and CCL-6 was used (Fig 7A, 7B and 7C). In addition, PMIS-200c also significantly increased the transcripts of IL-6, IL-8 and CCL-5 in human periodontal ligament fibroblasts with overexpression of miR-200c after LPS stimulation compared to PMIS-EV. These results further indicated the inhibitory effects of IL-6, IL-8 and CCL-5 mediated by miR-200c by targeting their 3’ UTRs.
Fig 7. PMIS-200c reduces binding activity of miR-200c to the 3’UTR of IL-6, IL-8, and CCL-5 and the function of miR-200c.
A-C: Normalized luciferase activities of the 3’ UTR IL-6, IL-8, and CCL-5-luciferase reporters and their 3’UTR-mutated-luciferase reporters co-treated with miR-200c and PMIS-EV or PMIS-200c at different ratios of concentration. D-F: the transcripts of IL-6 (D), IL-8 (E), and CCL-5 (F) in the cells co-treated with miR-200c and PMIS-EV or PMIS-200c cultured in DMEM supplemented with LPS after 24 hours; *: p<0.05.
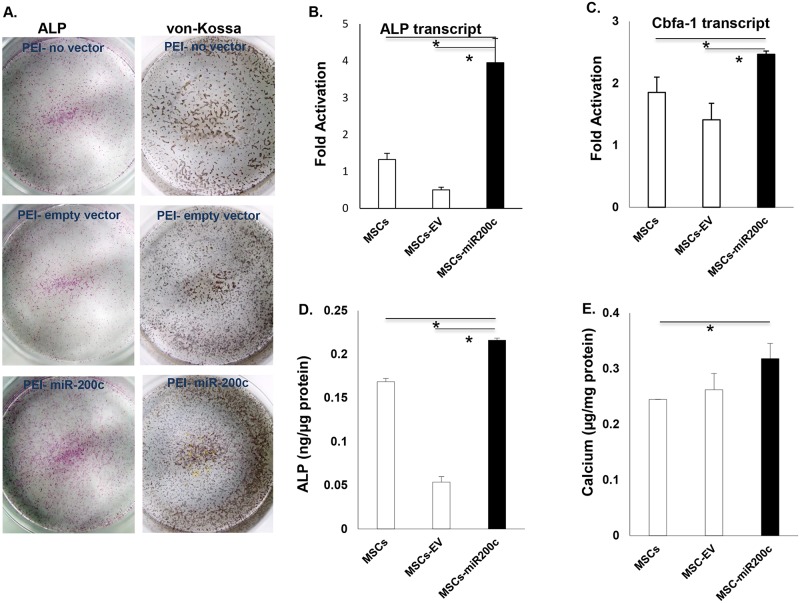
miR-200c delivered using PEI improves osteogenic differentiation of human MSCs
Human bone marrow MSCs were transfected using PEI-miR-200c or PEI-empty vector at 1.0 μg/per well, then the cells were subsequently cultured using DMEM supplemented with ascorbic acid and β-glycerophosphate for up to 2 weeks. ALP staining of MSCs showed mineralization effects with different treatment in culture dishes, 1 week after culture in osteogenic medium (Fig 8A). Staining was observed in both controls, including MSCs with and without treatment with the PEI-empty vector. PEI-miR-200c transfected cells showed stronger ALP staining than that in controls. von-Kossa staining was observed in MSCs with and without treatment with the PEI-empty vector. The von-Kossa staining was darker in the MSCs transfected with miR-200c. Quantitatively, the transcripts of ALP (Fig 8B) and Runx2 (Fig 8C) were significantly increased in the cells treated with PEI-miR-200c, compared to controls including MSCs treated with PEI, with or without empty vector. In addition, the ALP concentration (Fig 8D) and calcium content (Fig 8E) in the MSCs transfected with miR-200c were increased after 2 weeks in culture.
Fig 8. Enhancement of osteogenic differentiation of human bone marrow MSCs with overexpression of miR-200c using PEI nanoparticles.
A: Images of ALP and von-Kossa staining in MSCs overexpressing miR-200c, one and two weeks after treatment with osteogenic medium. B and C: the transcripts of ALP (B) and Runx2 (C) in MSCs overexpressing miR-200c, one week after treatment with osteogenic medium. D and E: Quantitative measurement of ALP levels (D) and calcium content (E) in MSCs overexpressing miR-200c, one and two week after treatment with osteogenic medium. Each measurement was made in triplicate. *: p<0.05.
Discussion
In this study we observed that, for the first time, overexpression of miR-200c effectively represses multiple proinflammatory mediators, including IL-6, IL-8 and CCL-5, in a human preosteoblast cell line. Our Gene analysis indicated that miR-200c may directly target the 3’UTR of these mediators. Overexpression of miR-200c may also promote OPG and improve osteogenic differentiation in this cell line. Furthermore, our studies demonstrated that plasmid DNA containing miR-200c can be effectively delivered using a non-viral delivery system. miR-200c delivered using PEI nanoparticles inhibited IL-6, IL-8, and CCL-5 in primary human periodontal ligament fibroblasts and improved osteogenic differentiation of primary human bone marrow MSCs. These data strongly suggest that miR-200c may potentially be used to repress periodontitis-associated bone resorption and restore the periodontal bone defects by improving bone formation and modulating imbalance and dysregulation of proinflammatory mediators.
While miR-200c is downregulated in gingival tissues of periodontitis patient, its function and underlying mechanism(s) in this chronic inflammatory disease are less understood. Several publications have suggested that miR-200c may participate in the regulation of inflammation. Rokavec et al. reported that miR-200c suppression may direct the constitutive activation of inflammatory signaling circuit in transformation and tumorigenesis [25]. Wendlandt et al. demonstrated that miR-200c may reduce NF-kB activation by modifying TLR-4 signaling through the MyD88-dependent pathway [26]. miR-200c may also reduce IL-8 expression by targeting IKBKB in NF-kB signal pathway [32]. Another report indicated that miR-200c may target an NF-κB up-regulated TrkB/NTF3 autocrine signaling loop in breast tumors [27]. However, this is the first study to investigate the anti-inflammatory activity of miR-200c in periodontitis and related bone metabolism. In this study, although the effect mediated by miR-200c on the regulation of the p65/p50 subunits of NF-kB was not observed (data not shown), we have shown that, miR-200c effectively inhibits IL-8 expression in human preosteoblasts and periodontal ligament fibroblast under the stimulation of a bacterial endotoxin by binding to the IL-8 3’UTR. Moreover, we demonstrated that miR-200c effectively reduces IL-6 and CCL-5 expression in human preosteoblasts and periodontal ligament fibroblasts. The reporter gene analysis also demonstrated that miR-200c effectively targets the 3’UTR of IL-6 and CCL-5. As IL-6, IL-8 and CCL-5 major proinflammatory mediators having critical roles in inflammation, these results strongly suggest that miR-200c possesses a powerful capacity to reduce inflammation via post-transcriptional regulation of these proinflammatory mediators.
We observed that overexpression of miR-200c upregulated OCN and calcium content in human preosteoblast cells. Furthermore, we demonstrated that miR-200c delivered using PEI nanoparticles promotes increased ALP, Runx2, and calcium content in primary human MSCs. While miR-200c can participate in stem cell proliferation and differentiation [24], this is the first study that demonstrates the potential function of miR-200c to improve osteogenic differentiation and bone regeneration. This function may be accomplished by inhibiting Noggin, an antagonist of BMP signals. We have previously reported that miR-200c targets Noggin 3’UTR and down-regulates Noggin expression in dental epithelial cells [28]. Noggin is a secreted protein that binds and inactivates a number of BMPs, including BMP-2, 7. Noggin suppression has been demonstrated to promote BMP-induced bone regeneration in vitro and in vivo [33, 34]. In this study, we also observed miR-200c inhibition of Noggin expression in human bone marrow MSCs (data not shown). Additionally, proinflammatory mediators have been demonstrated to impair bone formation by reducing differentiation of osteoblasts and their progenitor cells [17, 18]. Inhibition of proinflammatory mediators also partially explains the function of miR-200c on enhancing bone formation.
Although non-viral gene delivery systems have shown promise as alternative approaches of recombinant viral vectors, nanoparticles are the only non-viral vectors that can provide a targeted intracellular delivery with controlled release properties. Nanoparticles can serve as a local drug delivery system to oral mucosa [35]. PEI nanoparticles have been used as a non-viral vector for gene delivery due to their “proton-sponge” effect and high transfection efficiency. Our previous studies have successfully delivered plasmid DNA using PEI nanoparticles. We demonstrated that N/P ratios significantly influence the size, surface charge, transfection efficiency, and cytotoxicity of PEI nanoplexes. Our previous studies have also shown that PEI-pDNA {encoding for platelet derived growth factor-B (PDGF-B)} nanoplexes can induce significantly higher bone regeneration in calvarial rat defects [30]. In this study we showed that PEI can effectively deliver miR-200c into primary human periodontal ligament fibroblasts and bone marrow MSCs, demonstrating the feasibility of transfecting miR-200c using PEI nanoparticles. These results, along with our previous in vivo studies, strongly suggest that PEI nanoparticles may potentially be used as a delivery system to transfect miR-200c for clinical application purposes. In addition, we observed that the up-regulated content of miR-200c expression is dose-dependent according to PEI-miR-200c nanoplex treatment. Thus, we can maximize the effects of miR-200c by optimizing the PEI-miR-200c nanoplex concentration and its expression level.
In this study, we observed that the secreted amounts of IL-6, IL-8, and CCL-5 increased with the dose of transfection of plasmid DNA, which indicates that the cellular inflammation response and inhibitory effects can be mediated by miR-200c in response to the stimulation by bacterial endotoxin. This is probably caused by the innate immune system of the cells that can recognize nucleic acids after transfection. It has been demonstrated that after plasmid DNA is detected by endosomal toll-like receptors, including TLR3, TLR7, and TLR8, and cytoplasmic RIG-I and MDA5, endosomal TLR9 and cytoplasmic DAI may bind the DNA, resulting in the activation of NF-kB and interferon regulatory factor transcription factors [36]. Therefore, in order to develop a plasmid miR-200c based approach for anti-inflammation, an optimal transfection of miR-200c to limit plasmid DNA-induced innate immune response is necessary. Besides periodontitis, IL-6, IL-8, and CCL-5 as major proinflammatory mediators they also play critical roles in many inflammation-related diseases, including osteoarthritis and Parkinson’s disease. Thus, the inhibitory effects mediated by miR-200c indicate that this miR may be potentially developed into a therapeutic tool for these diseases.
Acknowledgments
We thank members of the Hong and Amendt laboratories for helpful discussions and technical work.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1.Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. CDC Periodontal Disease Surveillance workgroup: James Beck (University of North Carolina, Chapel Hill, USA), Gordon Douglass (Past President, American Academy of Periodontology), Roy Page (University of Washin. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012; 91: 914–1920. [DOI] [PubMed] [Google Scholar]
- 2.Papapanou PN, Tonetti MS. Diagnosis and epidemiology of periodontal osseous lesions. Periodontol. 2000; 22: 8–21. [DOI] [PubMed] [Google Scholar]
- 3.Müller HP, Ulbrich M. Alveolar bone levels in adults as assessed on panoramic radiographs. (I) Prevalence, extent, and severity of even and angular bone loss. Clin Oral Investig. 2005; 9: 98–104 [DOI] [PubMed] [Google Scholar]
- 4.Armas J, Culshaw S, Savarrio L. Treatment of peri-implant diseases: a review of the literature and protocol proposal. Dent Update. 2013; 40:472–480. [DOI] [PubMed] [Google Scholar]
- 5.Jeffcoat MK. Osteoporosis: a possible modifying factor in oral bone loss. Ann Periodontol. 1998; 3: 312–321 [DOI] [PubMed] [Google Scholar]
- 6.Sidiropoulou-Chatzigiannis S, Kourtidou M, Tsalikis L. The effect of osteoporosis on periodontal status, alveolar bone and orthodontic tooth movement. A literature review. J Int Acad Periodontol. 2007; 9: 77–84 [PubMed] [Google Scholar]
- 7.Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, et al. Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab. 2012; 97: 2272–82. 10.1210/jc.2012-1027 [DOI] [PubMed] [Google Scholar]
- 8.Darveau RP. (2010) Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol. 2010; 8: 481–490. 10.1038/nrmicro2337 [DOI] [PubMed] [Google Scholar]
- 9.Di Benedetto A, Gigante I, Colucci S, Grano M. Periodontal disease: linking the primary inflammation to bone loss. Clin Dev Immunol. 2013; 2013:503754 10.1155/2013/503754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hajishengallis G, Krauss JL, Liang S, McIntosh ML, Lambris JD. Pathogenic microbes and community service through manipulation of innate immunity. Adv Exp Med Biol. 2012: 946: 69–85. 10.1007/978-1-4614-0106-3_5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herath TD, Darveau RP, Seneviratne CJ, Wang CY, Wang Y, Jin L. Tetra- and penta-acylated lipid A structures of Porphyromonas gingivalis LPS differentially activate TLR4-mediated NF-κB signal transduction cascade and immuno-inflammatory response in human gingival fibroblasts. PLoS One. 2013; 8:e58496 10.1371/journal.pone.0058496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graves DT, Oates T, Garlet GP. Review of osteoimmunology and the host response in endodontic and periodontal lesions. J Oral Microbiol. 2011; 17:3 10.3402/jom.v3i0.5304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang N, Wang G, Hu C, Shi Y, Liao L, Shi S, et al. Tumor necrosis factor α suppresses the mesenchymal stem cell osteogenesis promoter miR-21 in estrogen deficiency-induced osteoporosis. J Bone Miner Res. 2013; 28: 559–573. 10.1002/jbmr.1798 [DOI] [PubMed] [Google Scholar]
- 14.Lacey DC, Simmons PJ, Graves SE, Hamilton JA. Proinflammatory cytokines inhibit osteogenic differentiation from stem cells: implications for bone repair during inflammation. Osteoarthritis Cartilage. 2009; 17: 735–742. 10.1016/j.joca.2008.11.011 [DOI] [PubMed] [Google Scholar]
- 15.Hikiji H, Shin WS, Koizumi T, Takato T, Susami T, Koizumi Y, et al. Peroxynitrite production by TNF-alpha and IL-1beta: implication for suppression of osteoblastic differentiation. Am J Physiol Endocrinol Metab. 2000; 278: E1031–1037. [DOI] [PubMed] [Google Scholar]
- 16.Wang L, Zhao Y, Shi S. Interplay between mesenchymal stem cells and lymphocytes: implications for immunotherapy and tissue regeneration. J Dent Res. 2012; 91: 1003–1010 10.1177/0022034512460404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang J, Wang Z, Tang E, Fan Z, McCauley L, Franceschi R, et al. Inhibition of osteoblastic bone formation by nuclear factor-kappaB. Nat Med. 2009; 15: 682–689 10.1038/nm.1954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang J, Liu F, Lee M, Wu B, Ting K, Zara JN, et al. NF-κB inhibits osteogenic differentiation of mesenchymal stem cells by promoting β-catenin degradation. Proc Natl Acad Sci U S A. 2013; 110: 9469–9474. 10.1073/pnas.1300532110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh RP, Massachi I, Manickavel S, Singh S, Rao NP, Hasan S, et al. The role of miRNA in inflammation and autoimmunity. Autoimmun Rev. 2013; 12: 1160–1165. 10.1016/j.autrev.2013.07.003 [DOI] [PubMed] [Google Scholar]
- 20.Plank M, Maltby S, Mattes J, Foster PS. Targeting translational control as a novel way to treat inflammatory disease: the emerging role of microRNAs. Clin Exp Allergy. 2013; 43: 981–999. 10.1111/cea.12170 [DOI] [PubMed] [Google Scholar]
- 21.Lian JB, Stein GS, van Wijnen AJ, Stein JL, Hassan MQ, Gaur T, et al. MicroRNA control of bone formation and homeostasis. Nat Rev Endocrinol. 2012; 8: 212–227. 10.1038/nrendo.2011.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katoh Y, Katoh M. Hedgehog signaling, epithelial-to-mesenchymal transition and miRNA (review). Int J Mol Med. 2008; 22: 271–275. [PubMed] [Google Scholar]
- 23.Huang HN, Chen SY, Hwang SM, Yu CC, Su MW, Mai W, et al. miR-200c and GATA binding protein 4 regulate human embryonic stem cell renewal and differentiation. Stem Cell Res. 2014; 12: 338–353. 10.1016/j.scr.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 24.Stoecklin-Wasmer C, Guarnieri P, Celenti R, Demmer RT, Kebschull M, Papapanou PN. MicroRNAs and their target genes in gingival tissues. J Dent Res. 2012; 91: 934–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rokavec M, Wu W, Luo JL. IL6-mediated suppression of miR-200c directs constitutive activation of inflammatory signaling circuit driving transformation and tumorigenesis. Mol Cell. 2012; 45: 777–789. 10.1016/j.molcel.2012.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wendlandt EB, Graff JW, Gioannini TL, McCaffrey AP, Wilson ME. The role of microRNAs miR-200b and miR-200c in TLR4 signaling and NF-κB activation. Innate Immun. 2012; 18: 846–855. 10.1177/1753425912443903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howe EN, Cochrane DR, Cittelly DM, Richer JK. miR-200c targets a NF-κB up-regulated TrkB/NTF3 autocrine signaling loop to enhance anoikis sensitivity in triple negative breast cancer. PLoS One. 2012; 7:e49987 10.1371/journal.pone.0049987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao H, Jheon A, Li X, Sun Z, Wang J, Florez S, et al. The Pitx2:miR-200c/141:noggin pathway regulates Bmp signaling and ameloblast differentiation. Development. 2013; 140: 3348–3359. 10.1242/dev.089193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao H, Yu W, Li X, Wang J, Gao S, Holton NE, et al. A new plasmid-based microRNA inhibitor system that inhibits microRNA families in transgenic mice and cells: A potential new therapeutic reagent. Gene Ther. 2016; March 2 10.1038/gt.2016.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elangovan S., D'Mello S.R., Hong L., Ross R.D., Allamargot C., Dawson D.V., et al. The enhancement of bone regeneration by gene activated matrix encoding for platelet derived growth factor. Biomaterials 2014; 35: 737–747 10.1016/j.biomaterials.2013.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borgwardt DS, Martin AD, Van Hemert JR, Yang J, Fischer CL, Recker EN, et al. Histatin 5 binds to Porphyromonas gingivalis hemagglutinin B (HagB) and alters HagB-induced chemokine responses. Sci Rep. 2014; 4: 3904 10.1038/srep03904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chuang TD, Khorram O. miR-200c regulates IL8 expression by targeting IKBKB: a potential mediator of inflammation in leiomyoma pathogenesis. PLoS One. 2014; e95370 10.1371/journal.pone.0095370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stottmann RW, Anderson RM, Klingensmith J. The BMP antagonists Chordin and Noggin have essential but redundant roles in mouse mandibular outgrowth. Dev Biol. 2001; 240: 457–273. [DOI] [PubMed] [Google Scholar]
- 34.Heliotis M, Tsiridis E. Suppression of bone morphogenetic protein inhibitors promotes osteogenic differentiation: therapeutic implications. Arthritis Res Ther. 2008; 10: 115 10.1186/ar2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holpuch AS, Hummel GJ, Tong M, Seghi GA, Pei P, Ma P, et al. Nanoparticles for local drug delivery to the oral mucosa: proof of principle studies. Pharm Res. 2010: 27: 1224–1236. 10.1007/s11095-010-0121-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin Microbiol Rev. 2009; 22: 240–273 10.1128/CMR.00046-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.