Supplemental Digital Content is Available in the Text.
Key Words: percutaneous lumbopelvic fixation, unstable sacral fractures, spinopelvic dissociation, lumbopelvic dissociation, spinopelvic dissociation
Summary:
Sacral fractures that result in spinopelvic dissociation are unstable injuries that are often treated surgically, with iliosacral screw fixation and/or lumbopelvic fixation from L4 to the pelvis. Open lumbopelvic fixation allows for direct fracture reduction and immediate postoperative weight bearing, but is associated with a relatively high wound complication rate. Open surgery often takes several hours and can be associated with significant blood loss, and therefore may not be well tolerated physiologically in these patients who often have multiple injuries. We developed a percutaneous lumbopelvic reduction and fixation technique to address these issues.
INTRODUCTION
Bilateral vertical sacral fractures that connect horizontally may form a “U” or “H” pattern and are characterized by complete loss of the bony connection between the spine and pelvis (see Figure, Supplemental Digital Content 1, http://links.lww.com/BOT/A637 showing the fracture patterns). These spinopelvic dissociation patterns are highly unstable and are frequently associated with a traumatic sacral kyphotic deformity (see Figure, Supplemental Digital Content 2, http://links.lww.com/BOT/A638 showing a characteristic sagittal computed tomography image of a spinopelvic dissociation pattern) and may cause sacral nerve root injury to the degree that bladder and/or bowel function are compromised. To treat these fractures, an open midline extensile approach is typically employed, which allows for a sacral laminectomy, fracture reduction, and stabilization from the lumbar spine into the pelvis.1–3 This technique is associated with significant blood loss and a relatively high complication rate.4 To minimize the physiological burden to the patient, we developed a minimally invasive percutaneous lumbopelvic fixation technique to reduce and stabilize these fractures.
TECHNICAL PRINCIPLES AND SURGICAL TECHNIQUE
Initial Treatment of Pelvic Ring Injury
If there is an anterior pelvic ring injury with displacement of more than 2 cm, a binder is variably applied and attempts made to bring the patient to the operating room within a day for anterior stabilization. Depending on the type of injury and the patient's medical status, the anterior pelvic ring injury is treated with internal fixation, external fixation, or with a tunneled subcutaneous rod connecting 2 supraacetabular polyaxial screws. If the patient is medically stable, we will perform lumbopelvic instrumentation at the same setting as the anterior stabilization. We return to surgery at a later date if it is felt that the patient cannot tolerate prone positioning for the posterior component of the procedure. We did not delay surgery due to the extent of soft tissue injury, though this may theoretically be necessary in select patients.
Patient Positioning and Indirect Fracture Reduction
The OSI spine table (Mizuho OSI, Union City, CA) was used in all cases, with the pelvis and thigh pads moved caudal to accommodate an external fixator when present. Pillows placed under the thighs to extend the pelvis relative to the spine may effect postural reduction. In patients with more than 10 degrees of traumatic kyphosis, we use intraoperative reduction maneuvers. Bifemoral skeletal traction is applied with counter-traction through Mayfield head tongs, provided there is no spine or skull fracture. Femoral traction can be set up with the traction bow posterior to the thighs in order to extend the pelvis and reduce a kyphotic deformity (Fig. 1A), or anterior to the thighs if longitudinal traction is desired to reduce a traumatic spondyloptosis (Fig. 1B). Lateral fluoroscopy is used to visualize the sacral fracture, and traction is sequentially applied to reduce the fracture. It is also possible to more directly reduce the fracture using the screws (described later) in cases where indirect reduction is not sufficient.
FIGURE 1.
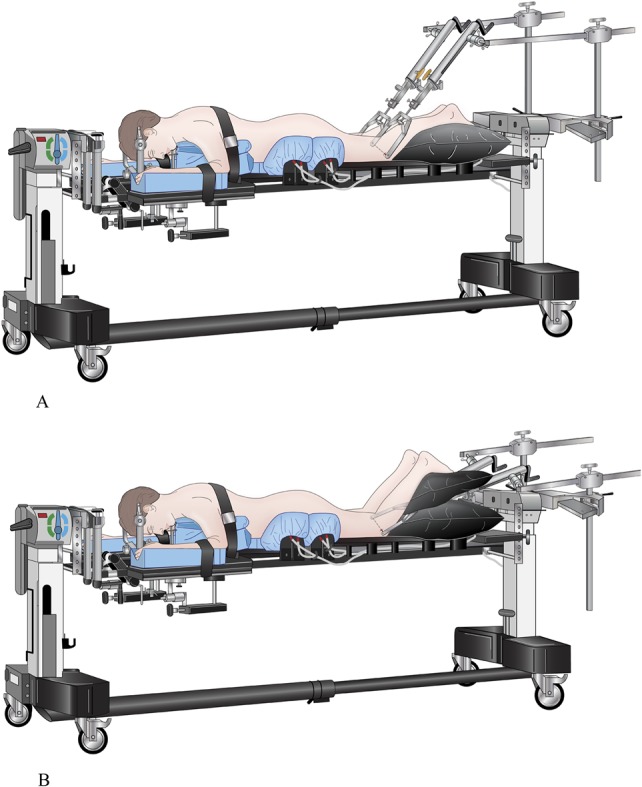
Drawing of patient positioning on the OSI spine table. The head is secured with Mayfield head tongs and the patient is in bifemoral skeletal traction. A, The traction bows are placed posterior to the thighs in order to produce pelvis extension to reduce a sacral fracture kyphotic deformity. B, The traction bows are placed anterior to the thighs in order to produce longitudinal traction to reduce sacral fracture shortening as occurs in traumatic spondyloptosis as seen in Figure 4.
Implants
DePuy Synthes Viper instrumentation (DePuy Synthes Spine, Raynham, MA) was used in all study patients. Both authors have performed paid consulting work for DePuy Synthes Spine, which manufactures the implants used in the reported cases, and therefore a potential conflict of interest exists. The typical construct consisted of bilateral polyaxial cannulated titanium pedicle screws of 6- to 7-mm diameter at L4 and L5 connected to bilateral polyaxial titanium iliac screws of 8- to 9-mm diameter and 80- to 100-mm length, with or without percutaneous iliosacral screws (Fig. 2). It is possible that fixation from L5 to the ilium would be sufficient, but we feel that 4 pedicle screws above the fracture and 2 iliac screws below the fracture create a balanced construct. Consideration could be given to placing S1 screws, but we feel that the fracture pattern often makes these screws of dubious value, and rod passage becomes more difficult. Extended-tab screws, commonly used as reduction screws in scoliosis surgery, are helpful at L4 and L5 but are not necessary with the iliac screws. Tubular extensions are used for the iliac screws (Fig. 3). Rods are 5.5 mm diameter titanium or cobalt-chrome, the latter chosen in young patients with especially strong bone, although we typically use titanium because it is more forgiving and appears to provide sufficient strength. Precontoured lordotic rods work well for L4-pelvis constructs. If longer constructs are necessary, a straight rod is contoured intraoperatively to match the patient's anatomy.
FIGURE 2.
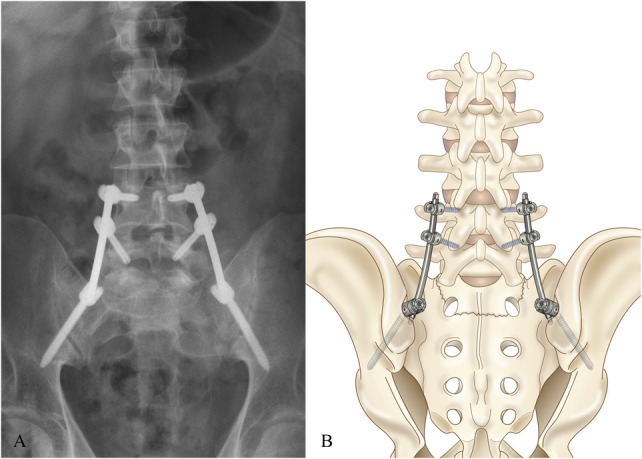
The typical appearance of percutaneous lumbopelvic instrumentation on postoperative AP x-rays (A) and depicted in a drawing (B).
FIGURE 3.

These are intraoperative pictures of the patient shown in Supplement Digital Content 3. The head of the patient is to the left side of the picture. A, The surgeon is inserting the left iliac screw. The right iliac screw has already been placed, and the screw extension can be seen as it projects toward the viewer, just above the left iliac screw. The percutaneous pedicle screw guide wires are seen to the left of the image and are held out of the way with a hemostat. Sponges are packed into the wounds to minimize bleeding. B, Close-up intraoperative picture of the same patient after the iliac screws and percutaneous pedicle screws have been placed. The iliac screw extensions are seen to the right of the image and the pedicle screw extended tabs are seen to the left side of the image, with the patient's head to the left.
Pedicle Screw Placement
Percutaneous L4 and L5 screws can usually both be placed through single 2- to 3-cm long incisions because the lordosis in the lower lumbar spine produces convergence of the screw heads. These bilateral incisions are made just big enough to accommodate the screw head extensions and are placed approximately 1–2 cm lateral to the lateral L4 and L5 pedicle walls, which tend to line up longitudinally with the iliac screw incisions. Introducer needles are then placed under fluoroscopic guidance, followed by guide wire placement. The guide wires are held out of the way with hemostats and the iliac screws are then placed.
Iliac Screw Placement
The iliac screw incisions are about 2 cm long, just long enough to place a small Weitlaner retractor superficially and Army-Navy retractors deeply. These incisions are made at the level of, and about ½ to 1 cm medial to, the posterior superior iliac spine (PSIS). The incision is placed medial to the PSIS because this best accommodates the medial-to-lateral oblique angle of screw placement. Sharp dissection is carried down to fascia, and the fascia exposed over the iliac crest (see Figure, Supplemental Digital Content 3, http://links.lww.com/BOT/A639 intraoperative pictures showing the exposure for iliac screw placement). The fascia is then split longitudinally over the iliac crest with electrocautery, halfway between the medial and lateral border, and elevated off the medial side. Digital dissection can then be used to elevate the muscle off the medial side of the iliac crest as it dives deep to the sacrum, and the posterior sacral cortex is palpated. Army-Navy retractors are useful here. In order to recess the screw head deep to the posterior margin of the iliac crest and avoid screw prominence, the distance between the posterior iliac crest and sacrum is palpated, and a starting point chosen where there is approximately 2 cm available. Gouges are then used to remove enough iliac bone, including the medial portion of the dorsal cortex, to place the iliac screw and allow for rod passage.
To place the iliac screws, we prefer to use a blunt curved pedicle gearshift style probe and use the curved tip to navigate between the inner and outer table via tactile feedback, with intermittent AP fluoroscopic views ensuring the trajectory is cephalad to the sciatic notch (see Figures, Supplemental Digital Content 4, http://links.lww.com/BOT/A640 and see Figures, Supplemental Digital Content 5, http://links.lww.com/BOT/A641 showing the curved gearshift creating the iliac screw pathway in the ilium). If there is any doubt about proper screw placement, an outlet-judet oblique “teardrop” view after probe and/or screw placement may be used to confirm appropriate intraosseous screw positioning.5–8 This oblique teardrop view can also be used as the primary imaging technique for probe and iliac screw placement.8 Once the iliac screw pathway is established and tapped, a ball-tipped probe can be used to confirm a bony endpoint. The screw is then placed (Fig. 3A) and advanced until the base of the screw head contacts the sacrum, which will ensure that the screw head is deep to the posterior border of the iliac crest. In order for the rod to be passed when the screw head is recessed in this fashion, sufficient iliac crest bone must be removed proximal and distal to the screw head. Sometimes it is necessary to remove more iliac bone once the screw is placed, and this can be accomplished with a straight osteotome maneuvered both in a caudal and then cephalad direction through the screw head to open a pathway for the rod. The pedicle screws are placed over the guidewires after the iliac screws are inserted (Fig. 3B; and also see Figure, Supplemental Digital Content 6, http://links.lww.com/BOT/A642 intraoperative picture showing the percutaneous pedicle screws and iliac screws with screw extensions).
Fracture Reduction
Traction is the first maneuver employed, with visualization under fluoroscopy (see Figure, Supplemental Digital Content 7A and B, http://links.lww.com/BOT/A643 intraoperative fluoroscopy images showing the effect of traction on fracture reduction). The lumbar and iliac screws can be used to more directly control the fracture (see Figure, Supplemental Digital Content 7C, http://links.lww.com/BOT/A643 intraoperative fluoroscopy images showing completion of the reduction maneuver using direct manipulation with the iliac screws). To do this, the screw insertion drivers are left in place to serve as rigid handles to manipulate the pelvis with respect to the spine. Longitudinal traction and kyphosis reduction are possible. Once the fracture is reduced, it is held in place manually through the screws on one side of the spine, whereas the screwdrivers on the other side are removed and the rod passed and set screws placed. The set screws are tightened to hold the reduction, and then the contralateral screwdrivers are removed and the second rod is passed and set screws secured.
Rod Passage and Final Tightening
In our experience, the rod is best passed in a caudal to cephalad direction, because the iliac screws are relatively superficial, so the rod starts superficial and dives deep. For constructs extending cephalad to L4, the rod tip has a tendency to tunnel deeper than the most cephalad pedicle screw head, a problem that can be confirmed on lateral fluoroscopy. When this occurs, it is sometimes necessary to extend the screw incision slightly distal and use a low-profile rod holder or Kocher clamp to grasp and guide the rod. For final tightening, the set screws should be sequentially tightened in the lumbar spine first, starting at the lower levels. The polyaxial iliac screw heads will pivot as the rod is seated into the lumbar screws, and then the iliac set screws are tightened last. A lumbar fusion is not performed.
Role of Percutaneous Iliosacral Screws
Percutaneous SI screws add stability to the lumbopelvic construct, but the clinical importance of this is unclear. Generally speaking, we chose to place SI screws as supplementary fixation in those fractures that required major kyphosis reduction maneuvers of more than 10–15 degrees or spondyloptosis reduction.
Wound Closure
The fascia is closed with #1 vicryl or PDS suture. Particular attention should be made to closing the fascia over the iliac screws because this is the most prominent and potentially problematic area. Skin closure is performed with interrupted nylon sutures.
Postoperative Protocol
Immediate mobilization without weight-bearing restriction is allowed. When resting in bed, patients should lay rolled approximately 45 degrees to either side to avoid pressure on the iliac screw wounds.
Instrumentation Removal
We generally recommend removal of the instrumentation 4–6 months after the index surgery because a spinal fusion is not performed. A CT scan may be obtained to confirm the fracture is healed. Removal is performed through the same incisions. Patients should be informed of the recommendation for this planned subsequent surgery during the informed consent process for the initial fracture surgery.
SPECIAL CONSIDERATIONS
Sacral Nerve Root Function
Patients with spinopelvic dissociation injuries often have other injuries and may not be able to participate with a detailed neurological examination. Patients with isolated sacral fractures who can participate in a neurological examination may have difficulty urinating spontaneously because of the pain associated with the injury and the awkwardness of trying to urinate or defecate on a bedpan in the setting of this painful injury. In patients who can participate with a neurological examination, as long as perineal sensation and rectal tone are intact, we do not perform a sacral laminectomy. In patients with diminished perineal sensation, or in patients with obvious sacral canal compromise on CT scan who cannot participate with the neurological examination, we strive to achieve an indirect reduction, and if we feel this is successful, we do not perform a sacral laminectomy. The main indication for a laminectomy would be the patient with bowel or bladder dysfunction and the fracture reduction was incomplete or did not adequately achieve an indirect decompression of the neural elements. We performed a sacral laminectomy in only one patient, who had an obvious cauda equina syndrome. We do not think this is routinely necessary, but the indications for a sacral laminectomy are not clear.
Soft-Tissue Degloving Injury
Extensive soft tissue degloving injuries may be present in the more severe fracture patterns. We operated through this compromised soft tissue envelope, but the one infection occurred in a patient who had severe soft tissue degloving.
Long-Term Consequences of Instrumentation Into the Spine
Percutaneous instrumentation for fusion-less spine fracture treatment is increasingly accepted, but the long-term consequences are unknown. This issue should be discussed with patients. The other option is to fuse the L4/5 and L5/S1 segments, but we feel the chance of late problems because of facet deterioration after instrumentation removal is preferred to undergoing a primary spinal fusion.
CLINICAL SERIES
Methods
Patients with sacral fracture patterns resulting in spinopelvic dissociation were included in the study. Data were gathered prospectively. Institutional review board approval was obtained. Seventeen consecutive patients who presented with spinopelvic dissociation fracture patterns were treated with percutaneous lumbopelvic fixation. No open lumbopelvic fixations were performed during this time. We identified the accuracy of screw placement on postoperative CT scans, operative time, blood loss, fluoroscopy time, and assessed bowel and bladder function and extremity neurological function. Fracture kyphosis and displacement was measured on preoperative and postoperative CT scans (see Table, Supplemental Digital Content 8, http://links.lww.com/BOT/A644 kyphosis and displacement measurements), and fracture healing was determined with CT scan or x-ray.
RESULTS
Seventeen patients had spinopelvic dissociation pattern injuries with bilateral longitudinal and transverse sacral fracture patterns, commonly referred to as “U- or H-type” sacral fractures.9–11 Clinical follow-up averaged 21 months, with one patient lost to follow-up after 4 months. Operative time was recorded in all 17 patients, and fluoroscopy time was recorded in all patients except for one. Operative time averaged 2 hours 24 minutes (range 105–210 minutes), fluoroscopy time averaged 2 minutes 15 seconds (range 68–220 seconds), and blood loss averaged 202 mL (range 75–400 mL). A total of 79 pedicle screws and 36 iliac screws (4 iliac screws in 1 patient) were placed. Fifteen patients underwent postoperative CT scans, which detected a single 3 mm lateral pedicle breach and a 2 mm iliac screw cortical breach, with all other CT-imaged screws (100 of 102, or 98%) entirely intraosseous. Breaches were not symptomatic or consequential and did not require revision.
Reduction was attempted in 5 fractures with sacral kyphosis greater than 10 degrees and 1 fracture with more than 100% displacement and 1 cm of shortening (traumatic spondyloptosis). These fractures had an average preoperative kyphosis of 16 degrees, which improved to 4 degrees postoperatively, and the traumatic spondyloptosis was anatomically reduced (Figs. 4 and 5; and also see Figure, Supplemental Digital Content 9, http://links.lww.com/BOT/A645 lateral sacral x-ray showing the healed fracture after lumbopelvic instrumentation removal).
FIGURE 4.
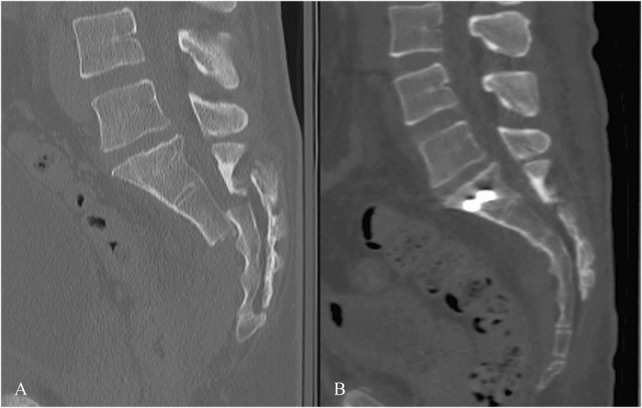
These are images from the patient shown in Supplemental Digital Content 7 with traumatic spondyloptosis. A, Shows the preoperative sagittal CT scan, with complete dorsal displacement and shortening. B, Immediate postoperative CT scan showing anatomic reduction of the fracture. The iliosacral screws are seen in the S1 body. The percutaneous lumbopelvic fixation is in place but is not seen because the implants are all out of the plane of the image.
FIGURE 5.
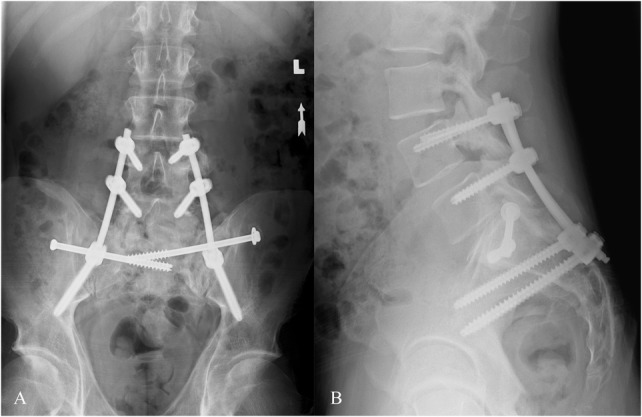
A and B, AP and lateral x-rays, respectively, showing maintenance of the fracture reduction, intact implants without evidence of loosening, and a healed fracture 6 months after surgery. These films were taken shortly before the lumbopelvic implants were removed.
One patient developed a deep wound infection requiring serial debridements. Instrumentation was retained, and the wounds healed. There were no other wound problems. Bowel and bladder function was not assessed preoperatively, though 11 of 14 patients who were alert and cooperative with the examination had intact perineal sensation and normal rectal tone before surgery (see Table, Supplemental Digital Content 10, http://links.lww.com/BOT/A646 patient neurological status before and after surgery). One patient with preoperative unilateral tibialis anterior weakness developed bilateral tibialis anterior weakness after surgery, determined to be secondary to stretch neurapaxia after imaging studies and nerve conduction studies were completed. Full strength was later regained. One patient with reportedly normal bowel and bladder function prior to the injury lost normal function, though this patient also had severe lumbar burst fractures with greater than 75% canal compromise, perineal sensation and rectal tone were not assessable preoperatively owing to a head injury, and this patient was transported back to his home country and was lost to follow-up after 135 days. Two elderly patients with ground-level falls presented more than a week after their injury with bladder incontinence, and despite a laminectomy being performed in one, bladder function was not regained. All 14 other patients regained normal bladder function. There were no other perioperative complications.
DISCUSSION
Sacral fractures with spinopelvic dissociation patterns are highly unstable injuries. Open lumbopelvic fixation has been associated with a relatively high wound complication and infection rate.3,4 We have demonstrated a percutaneous technique that is effective in both reducing and stabilizing these fractures, with minimal blood loss (averaging approximately 200 mL) in a reasonable surgical duration of 1½–3 hours. Early in the series, we had difficulty-reducing fractures because we relied primarily on postural reduction maneuvers. Once we began using bifemoral skeletal traction combined with direct reduction maneuvers using the screws as levers, we were able to more reliably reduce the fractures, including in a patient with traumatic sacral spondyloptosis. Wound breakdown and infection are still concerns. The percutaneous technique does not completely solve this problem. Efforts should be made to close fascia and avoid direct pressure on the wound postoperatively. In cases where a safe SI screw corridor is available and a kyphotic deformity is reduced, we are inclined to perform percutaneous SI screw fixation, which provides a biomechanical advantage though the clinical importance of this is unknown.12
The advantages to percutaneous lumbopelvic fixation include the ability to immediately weight-bear without restriction, reasonable blood loss and surgical time, a relatively low wound complication rate, and avoidance of a lower lumbar spine fusion. A primary criticism of lumbopelvic fixation is the choice of this technique over percutaneous SI screw placement. In our series, there were several patients with minimal kyphosis and displacement that arguably could have been treated with SI screw fixation alone. However, SI screw fixation alone does not allow for immediate unprotected weight bearing and may not provide for sufficient stabilization in fractures with extensive comminution. We do believe that SI screw fixation alone may be sufficient in some of these injuries, but percutaneous lumbopelvic fixation is an option that should be considered.
The main drawbacks to percutaneous lumbopelvic fixation are the need for a separate incision for a sacral laminectomy when thought to be necessary, the potential need for a second surgery to remove the instrumentation, the reliance on fluoroscopy for pedicle screw placement, and the potential long-term deleterious effects of instrumenting into the mobile spine. Our patients did not have any issues with instrumentation prominence or failure, and removal was uneventful and well tolerated. Reduction and instrumentation requires more preoperative planning and intraoperative setup than in open cases, but surgery once started is expeditious and is likely associated with less physiological burden to the patient compared to open surgery. The need for a sacral laminectomy is not clear. This percutaneous technique is particularly appealing in patients with intact perineal sensation and no obvious sacral nerve dysfunction.
Footnotes
This material was presented in part at the Annual Meeting of the AAOS, New Orleans, LA, April 13, 2014, at the Annual Meeting of the Lumbar Spine Research Society, Chicago, IL, May 2, 2014, at the 2015 Orthopaedic Trauma Association Annual Meeting, San Diego, California, October 7–10, 2015, and at the Annual Meeting of the North American Spine Society, Chicago, IL, October 14–17, 2015.
Dr. Williams is a paid consultant for DePuy Synthes Spine and Titan Spine. Dr. Quinnan is a paid consultant for DePuy Synthes, Smith & Nephew, and Orthofix. Dr. Williams and Dr. Quinnan are AOTrauma faculty members and have received honoraria for participating in AOTrauma courses.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
This study was conducted at Jackson Memorial Hospital and the University of Miami Hospital in Miami, Florida, and at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin. The respective institutional review boards approved the study.
REFERENCES
- 1.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 2006;20:S44–S51. [PubMed] [Google Scholar]
- 2.Schildhauer TA, Bellabarba C, Nork SE, et al. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–457. [DOI] [PubMed] [Google Scholar]
- 3.Konig MA, Jehan S, Boszczyk AA, et al. Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J. 2012;21:829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellabarba C, Schildhauer TA, Vaccaro AR, et al. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976). 2006;31:S80–S88; discussion S104. [DOI] [PubMed] [Google Scholar]
- 5.Schildhauer TA, McCulloch P, Chapman JR, et al. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002;15:199–205; discussion 205. [DOI] [PubMed] [Google Scholar]
- 6.Wang MY. Percutaneous iliac screws for minimally invasive spinal deformity surgery. Minim Invasive Surg. 2012;2012:173685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang MY, Williams S, Mummaneni PV, et al. Minimally invasive percutaneous iliac screws: initial 24 case experience with CT confirmation. J Spinal Disord Tech. 2012. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 8.Wang MY, Ludwig SC, Anderson DG, et al. Percutaneous iliac screw placement: description of a new minimally invasive technique. Neurosurg Focus. 2008;25:E17. [DOI] [PubMed] [Google Scholar]
- 9.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 10.Roy-Camille R, Saillant G, Gagna G, et al. Transverse fracture of the upper sacrum. Suicidal jumper's fracture. Spine (Phila Pa 1976). 1985;10:838–845. [DOI] [PubMed] [Google Scholar]
- 11.Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5:200–203. [DOI] [PubMed] [Google Scholar]
- 12.Schildhauer TA, Ledoux WR, Chapman JR, et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. [DOI] [PubMed] [Google Scholar]


