Abstract
Objective:
Although opioids have substantial efficacy for acute pain management, escalation to opioid misuse and abuse is a persistent concern. This report assesses the current status of the opioid epidemic in Maine using three complementary data sets.
Method:
A representative sample of pharmacists (N = 275) completed an online survey regarding the extent that opioids affected their practice. A county-level analysis of opioid prescriptions (N = 1.22 million) reported to the Maine Prescription Monitoring Program (M-PMP) in 2014 and the agents implicated in arrests as reported to the Maine Diversion Alert Program (DAP, N = 2,700) in 2014/15 also was completed.
Results:
A significantly greater number of pharmacists agreed that opioid misuse (85.9%), rather than diversion (76.8%) or access (54.2%), was a concern. Only half (56.2%) reported use of the M-PMP. Opioids were dispensed to 22.4% of residents (37.7% of women in their 80s). This was enough to supply everyone in Maine with a 16.1-day supply. Buprenorphine accounted for almost half of opioid prescriptions to young adults (46.3% women, 49.3% men). Arrests increased by 13.3% from 2014 to 2015, and the proportion of arrests that involved prescription opioids decreased while those involving stimulants and heroin were elevated.
Conclusions:
Pharmacists are very aware of the potential for opioid misuse, but many do not consistently use the M-PMP. There continues to be substantial legitimate use, as well as criminal activity, involving oxycodone and other prescription opioids. Continued vigilance and use of tools like the PMP and DAP are necessary to minimize nonmedical use of opioids in Maine.
The pronounced increase in overdose deaths involving opioid analgesics (which exceeded those from heroin and cocaine, combined) prompted the U.S. Centers for Disease Control and Prevention to classify prescription drug overdoses as an epidemic (Paulozzi et al., 2012). Unfortunately, Maine (Alexander et al., 2004; Brown et al. 2015; Grau et al., 2007; Heimer et al., 2012; Martin & Rocque, 2011; McCall et al., 2013; Roche, 2000; Rosenberg, 2002; Sorg & Greenwald, 2003) has played a prominent role in this national opioid epidemic (Center for Behavioral Health Statistics and Quality, 2015; Johnston et al., 2015; Maxwell, 2011; Patrick et al., 2015; Paul et al., 2014; Warner et al., 2011). The total daily opioid dose in morphine equivalents in the United States was highest in Maine (798 mg/person), which was approximately fourfold higher than that in the lowest state. Further, there was a strong association between the volume of opioid sales and drug poisoning mortality rates (r = .73) (Paulozzi & Ryan, 2006). Maine was ranked highest in the United States in 2012 for prescribing long-acting/extended-release opioids (Paulozzi et al., 2014). Opioids including heroin, methadone, oxycodone, fentanyl, and hydrocodone accounted for half of the top 10 drugs mentioned on Maine death certificates as a cause of drug-related mortality (Sorg & Greenwald, 2003). Overall, nonmedical use of opioids continues to impose a substantial burden on the health care, economic, and criminal justice systems (Joranson & Gilson, 2005; Maxwell, 2011; Smith et al., 2009).
Many interventions have been implemented nationally or at a state level to limit prescription opioid misuse (Haegerich et al., 2014), including increasing the accessibility to opioid antagonists (Wermeling, 2015), changing clinical guidelines, the development of abuse-resistant opioids (Larochelle et al. 2015), expanding needle-sharing programs, identification of inappropriate prescribing by insurers and pharmacy benefit managers, improved patient and provider education, fining pharmacy chains and revoking the license to dispense controlled substances of stores that failed to prevent diversion (Meier, 2013), passing laws to better regulate so-called pill mills and decrease use of multiple prescribers (i.e., “doctor shopping”), and Prescription (Drug) Monitoring Programs (McCall et al., 2013). The Maine Prescription Monitoring Program (M-PMP) has been recording prescriptions of Schedule II, III, and IV substances since 2004. The majority (>85%) of licensed medical doctors, doctors of osteopathy, dentists, nurse practitioners, and physician assistants had registered to search the M-PMP by December 2013 compared with a minority (39%) of pharmacists. This is unfortunate, as pharmacists also share responsibility for ensuring the safe use of controlled substances.
Maine is currently the only state in the country with a Diversion Alert Program (DAP). The DAP is an electronic resource launched statewide in 2013 that allows health care providers to identify patients charged with drug-related crimes, including illegal possession and diversion of prescription drugs. This informational tool aids prescribers and dispensers in determining if a patient is likely to misuse or divert prescription medications. Unfortunately, less than one third of actively licensed prescribers and dispensers in Maine are registered with the DAP.
Resources like the DAP may be of increasing value because some prescription opioids may be less abuse resistant than was previously thought (Conrad et al., 2015). Importantly, there are commercial websites that collect information from federal, state, and local governments about drug arrests, charging a fee for that data (e.g., publicdata.com). However, DAP has the advantage of being nonproprietary, with a focus on improving patient care, patient outcomes, and communities as a whole. Finally, DAP has established relationships with the Maine Drug Enforcement Agency, state police, and various municipalities, working with law enforcement to provide an effective solution to address prescription drug abuse and diversion.
Given the persistence of nonmedical opioid misuse over the past two decades, the objective of this report was to provide an updated appraisal on this issue in Maine using three complementary sources: a survey of pharmacists, the M-PMP, and the DAP. More specifically, the objectives were to use the mixed-methods approach to (a) describe practicing pharmacists’ beliefs regarding the misuse and diversion of opioids and their use of the M-PMP; (b) characterize the prevalence of opioid use relative to other controlled substance use according to the M-PMP; and (c) evaluate patterns of arrests involving opioids, with an emphasis on Schedule II prescription agents (e.g., oxycodone, hydrocodone, methadone) as well as heroin and other drugs as assessed by the DAP.
Method
Participants
Survey respondents (N = 275, 48.7% female) included 40.5% with a doctor of pharmacy (Pharm.D.) degree. Their primary practice settings varied, with the largest subset working at a large retail chain (41.5%), an inpatient/hospital environment (22.9%), or an independent pharmacy (15.3%). Two fifths (41.0%) had practiced for more than 25 years. All procedures including the consent were approved by the Institutional Review Board of Husson University.
Procedure
All pharmacists with a Maine Board of Pharmacy license (N = 1,262) were emailed a SurveyMonkey link in the fall of 2014. A $5 gas card was offered as an incentive. Participants were asked, “To what extent do you agree or disagree that the following are challenges to your practice?” with specific items including misuse, diversion, store security, and patient access to legitimate use as assessed by a Likert scale (strongly disagree to strongly agree). Similarly, a rating of M-PMP use (In my practice, we use the PMP all the time) and M-PMP favorability (I have a favorable opinion of the PMP) was determined. Results from other (non-opioid) items were presented elsewhere (Martin et al., 2015; Supplemental Materials).
The M-PMP is administered by the Maine Department of Health and Human Services and collects Schedule II-IV data for all new and refill prescriptions. Information provided included patient age, sex, county of residence, the agent dispensed, and drug quantity (McCall et al., 2013).
Law enforcement agencies in Maine submit arrest records to DAP. This includes sex, community of residence, drug offense, and drug(s) involved in the offense. De-identified arrest data for the first complete year that DAP was operational (2014), as well as the first quarter of 2015, were analyzed. It is important to note that for marijuana-related drug charges, only nonpossession charges (i.e., trafficking, furnishing) are collected. Marijuana possession is not collected because of the ambiguities associated with medical marijuana.
Statistics
Two complementary analyses were completed on opioid and M-PMP ratings with Systat, Version 13.1 (San Jose, CA): nonparametric with the percent that agreed/strongly agreed combined, and parametric using the mean on the six-point scale. The state of Maine is divided into 16 counties (Supplemental Figure 1). For M-PMP analyses, several prescription endpoints were examined at a county level including percentage prescribed; prescriptions per capita; medication units, which includes pills, capsules, patches, etc.; and the number of days’ supply. As buprenorphine is available in different formulations (buprenorphine hydrochloride vs. buprenorphine with naloxone), these were listed separately.
The data for the population of Maine by age, sex, and county were based on the 2010 census. Age differences in opioid data were expressed two ways—as the number of unique recipients divided by the number of Mainers for each age and sex. An additional analysis was completed with frequencies divided by the total number of each prescription endpoint, by age expressed in decades, in order to facilitate comparison across measures. Drug offenses were categorized as (a) possession, including possession with intent to distribute; (b) trafficking, including aggravated trafficking and trafficking in prison contraband; and (c) other, which includes conspiracy to distribute, furnishing, and stealing. A population-corrected arrest measure was calculated as the percent of all reported arrests minus the percent of the state population in each county. The then-present (May 1, 2015) federal Drug Enforcement Agency Schedule of each drug (i.e., hydrocodone is currently a Schedule II drug) was determined for those reported to the DAP. Variability was expressed as the standard error of the mean.
Results
Survey of pharmacists
Participants (N = 275, a 21.8% response rate; 48.7% female) were representative of licensed pharmacists in the state (46.3%) in terms of gender (p = .46). The majority of pharmacists believed that opioids were a challenge in their practice. As also reported previously (Martin et al., 2015), more respondents strongly agreed or agreed that misuse (85.9%)—rather than diversion (76.8%, p < .01), access (54.2%, p ≤ .0001), or security (53.0%)—was a concern, χ2(1) = 65.63, p ≤ .0001. Diversion was rated less highly by respondents with a Pharm.D. (4.8 + 0.1) than by those with a bachelor’s degree (5.2 + 0.1), t(264) = 2.31, p < .05, d = 0.28. The vast majority of Pharm.D.-educated pharmacists had been practicing for less than 15 years (92.9%), which is very unlike their bachelor’s-level colleagues (7.1%, p ≤ .0005).
More respondents agreed that they have a favorable opinion of the M-PMP (75.3%) than reported using this program (56.2%, p < .0001). Pharmacists with a Pharm.D. had a slightly more favorable rating of the M-PMP (5.1 ± 0.1) than their bachelor’s-educated colleagues (4.8 ± 0.1), t(242) = 1.93, p = .055. Further, Pharm.D.’s (4.6 ± 0.1) were more likely than bachelor’s-level practitioners to use the M-PMP (4.2 ± 0.1), t(259) = 2.23, p < .05, d = 0.28. Pharmacists who worked in a hospital setting were less likely to use the M-PMP (3.7 ± 0.2) than those who were employed in a large retail environment (4.7 ± 0.1), t(80.5) = 4.22, p < .0005, d = 0.74, or private retail environment (4.6 ± 0.2), t(91) = 2.92, p < .005, d = 0.62. Concern about opioid misuse was slightly, albeit significantly, associated with M-PMP use, r(258) = .20, p < .001.
Maine Prescription Monitoring Program
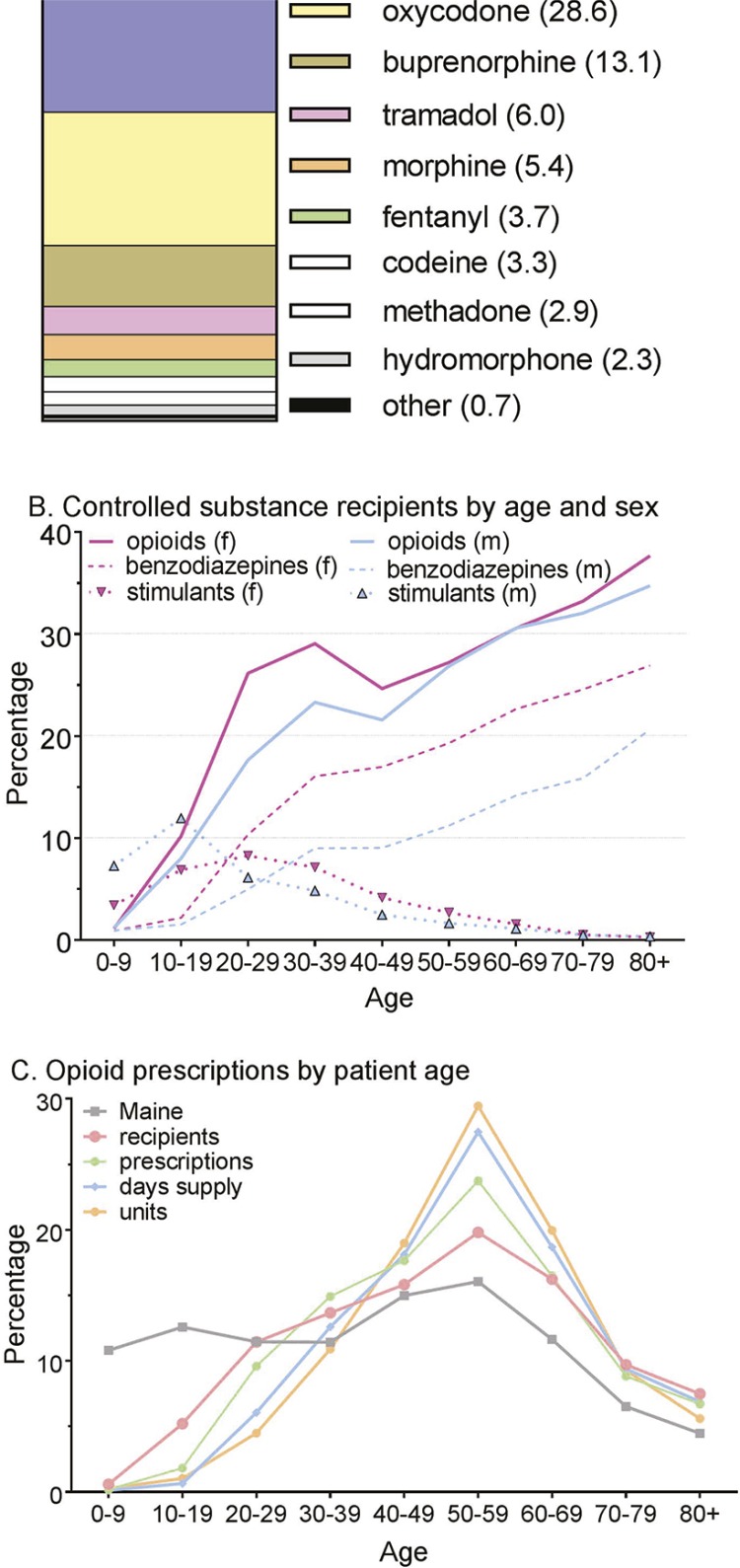
More than three quarters of opioid prescriptions were for Schedule II agents (77.3%), followed by Schedule III (16.6%) and Schedule IV (6.1%) drugs. Figure 1A shows that three agents (hydrocodone, oxycodone, buprenorphine/naloxone) accounted for the preponderance (73.8%) of opioid prescriptions. Within hydrocodone prescriptions, almost all were for hydrocodone/acetaminophen (99.2%), with the remainder for hydrocodone/ibuprofen or hydrocodone bitartrate. Among benzodiazepines, three drugs, lorazepam (33.4%), clonazepam (28.3%), and alprazolam (20.9%), accounted for the vast majority (82.6%) of prescriptions (Supplemental Figure 2A). Among stimulants, almost half were for methylphenidate (45.8%), one third for dextroamphetamine (34.1%), and only one fifth for lisdexamfetamine (20.1%), an abuse-deterrent agent (Supplemental Figure 2B).
Figure 1.
Opioid prescriptions reported to the Maine Prescription Monitoring Program in 2014 by drug. The buprenorphine slice includes buprenorphine/naloxone (11.16%) and buprenorphine hydrochloride (1.95%) (A). Percentage of the Maine population, by age and sex (f = females, m = males), that received a controlled substance (B). Percentage of opioid recipients, prescriptions, days’ supply, and units dispensed by age (C).
There were 1.22 million opioid prescriptions to 291,440 recipients. Therefore, more than one fifth (21.9%) of the state’s population received an opioid in 2014. Benzodiazepine (0.65 million) and stimulant (0.40 million) prescriptions were less common. There were also pronounced age differences. Figure 1B shows the percentage of all Maine residents, by age and sex, who received a prescription within 1 year for opioids, benzodiazepines, and stimulants. Sex differences were most pronounced and consistently observed for benzodiazepines, with women receiving more benzodiazepine prescriptions than men. More male children and adolescents (ages 0–19) received a stimulant, although the reverse pattern was evident at older ages. The percentage of the Maine population that received an opioid from a retail pharmacy increased markedly with age into the eighth and ninth decades.
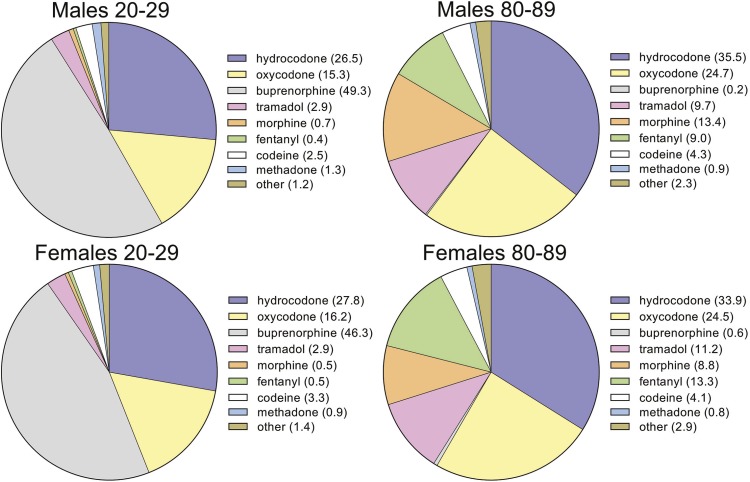
There were also pronounced age differences in the opioid prescribed. Buprenorphine constituted almost half of all opioids prescribed to young adults (ages 20–29), which is quite unlike the pattern for patients in their 80s (Figure 2) or the prescription pattern overall (Figure 1A). More specifically, buprenorphine/naloxone accounted for 39.07% of all opioid prescriptions for individuals in their 20s but was exceedingly uncommon for octogenarians (0.02%, p < .0001). This robust preference for prescribing buprenorphine to young adults was independent of sex.
Figure 2.
Opioid prescriptions reported to the Maine Prescription Monitoring Program in 2014 by age and gender. The percentage of all opioid prescriptions is listed in parentheses. The buprenorphine slice includes buprenorphine hydrochloride/naloxone hydrochloride and buprenorphine hydrochloride.
Additional age analyses were completed within opioid prescriptions (i.e., using the total number of opioid prescriptions, or other parameter, as the denominator). There was evidence for an uncoupling of prescription parameters for persons in their second and sixth decades. More specifically, teenagers account for 10.8% of Maine’s population but only 5.2% of opioid recipients, 1.0% of opioid units, and 0.6% by duration. Conversely, patients in their 50s account for about one sixth (16.1%) of Maine’s population but almost one fifth (19.8%) of all opioid recipients and an even larger portion (29.5%) of the units dispensed (Figure 1C). There was less evidence for uncoupling for benzodiazepines (Supplemental Figure 3A), and this was less pronounced for adolescents (ages 10–19) receiving stimulants (Supplemental Figure 3B).
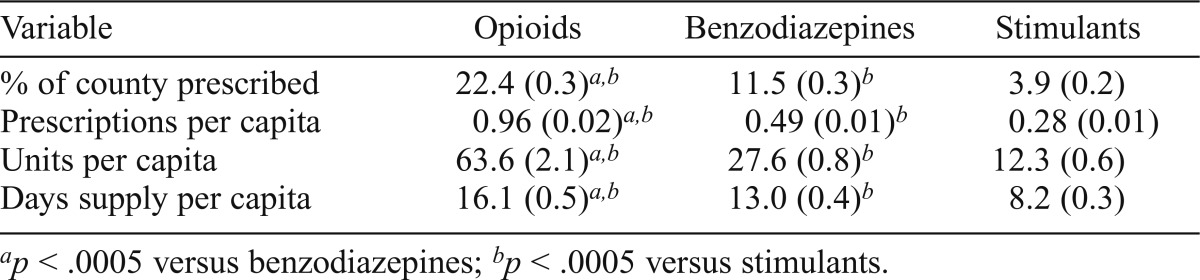
Table 1 extends these statewide results and compares opioid with benzodiazepine and stimulant prescriptions at a county level. Twice as many persons received opioids as benzodiazepines and almost sixfold more than stimulants. Other dispensing parameters showed the same ranking. In contrast, the total days’ supply per person was only twice as high for opioids as stimulants and only 23.8% longer than benzodiazepines, which reflects that prescriptions for non-opioids were typically for only moderately shorter intervals when expressed on a per capita basis.
Table 1.
Comparison of opioid, benzodiazepine, and stimulant prescriptions, per county (N = 16), as reported to the Maine Prescription Monitoring Program in 2014
| Variable | Opioids | Benzodiazepines | Stimulants |
| % of county prescribed | 22.4 (0.3)ab | 11.5 (0.3)b | 3.9 (0.2) |
| Prescriptions per capita | 0.96 (0.02)ab | 0.49 (0.01)b | 0.28 (0.01) |
| Units per capita | 63.6 (2.1)ab | 27.6 (0.8)b | 12.3 (0.6) |
| Days supply per capita | 16.1 (0.5)ab | 13.0 (0.4)b | 8.2 (0.3) |
p < .0005 versus benzodiazepines;
p < .0005 versus stimulants.
Diversion Alert Program
The first set of analyses examined arrests (N = 2,153) in 2014. Men (69.5%) accounted for more than twice the arrests as women (30.5%). Possession accounted for a greater proportion of arrests for women (women = 68.9%, men = 64.1%, p < .05), whereas trafficking accounted for more arrests among men (men = 28.3%, women = 23.5%, p < .05).
More arrests (58.0%) involved Schedule II-IV agents than Schedule I drugs (37.1%). The majority of arrests listed only a single drug (84.1%). Among these, opioids accounted for more than half (50.4%), followed by stimulants (27.7%), benzodiazepines (5.8%), bath salts (4.9%), cannabinoids (4.6%), and others (6.6%). Among opioids, oxycodone (26.3%), buprenorphine/naloxone (15.1%), and hydrocodone (6.4%) together (47.8%) were listed for slightly more arrests than heroin (46.9%). Cocaine and crack cocaine were responsible for more than half of the stimulant arrests (60.2%), followed by methamphetamine (23.6%) and amphetamine (7.3%). For cannabinoids, the preponderance of arrests were for marijuana (77.5%) and hashish (12.7%). Within benzodiazepines, clonazepam (45.4%) and alprazolam (37.1%) accounted for sizable proportions followed by diazepam (8.2%) and lorazepam (8.2%). Among arrests involving two or more drugs, opioids were listed in the majority (71.7%) and specifically heroin in more than one third (34.5%).
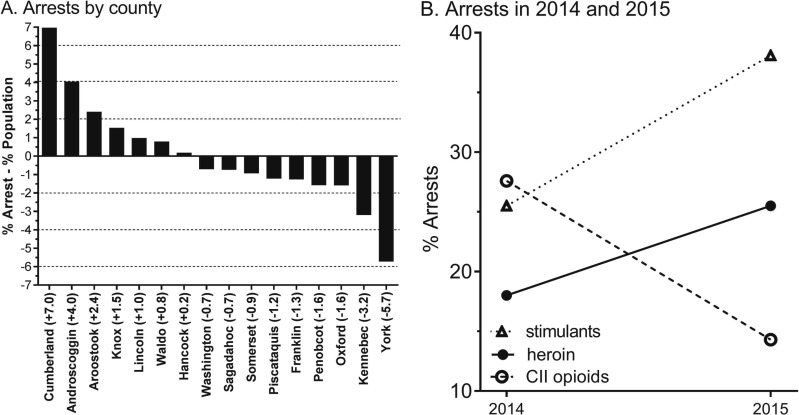
Figure 3A shows that some counties in the southern half of the state (i.e., the more densely populated region) were overrepresented for arrests relative to their population. Southern counties of York and Kennebec also had the lowest number of arrests. Individual counties had pronounced differences in specific drug classes. For example, bath salts accounted for only 0.4% of arrests in Cumberland but 31.4% in Aroostook (p < .0001). The most common single Schedule I agent was heroin in the preponderance (87.5%) of counties. Oxycodone was the most prevalent Schedule II drug in less than half (43.8%) of counties, followed by methamphetamine in one quarter (25.0%, Supplementary Table 1). A map of Schedule II opioid arrests shows highest levels in Augusta, Bangor, Portland, and Rockland (Supplemental Figure 4).
Figure 3.
Percentage of total arrests, corrected for population, as reported by the Maine Diversion Alert Program in 2014 (A). Percentage of arrests involving stimulants, Schedule II (CII) opioids, and heroin during 2014 and 2015. All changes are statistically significant (B).
Associations between the M-PMP and DAP were evaluated at a county level. Counties with more opioid recipients also had more arrests for offenses involving Schedule II drugs, both uncorrected, r(14) = .63, p < .01, and corrected, r(14) = .63, p < .01, for population size. Similarly, counties with a higher volume of opioid prescriptions had more Schedule II drug arrests when the correlation was uncorrected, r(14) = .63, p < .01, and corrected, r(14) = .52, p < .05, for population (Supplemental Figure 5).
The second analyses evaluated whether there were any changes in recent arrests by comparing the first quarter of 2015 with the first quarter of the preceding year. The number of arrests increased by 13.3%, although arrests involving two or more agents decreased (16.5% to 12.0%, p < .05). Figure 3B shows dynamic changes in arrests, with arrests involving heroin (p < .05)—as well as stimulants (p < .0001)—increased whereas those involving Schedule II opioids decreased (p ≤ .0001). Further, benzodiazepine arrests also decreased (8.2% to 4.5%, p < .05), whereas cannabinoid arrests essentially remained stable (2.6% to 2.9%).
Discussion
These three complementary data sets provide a thorough update on the evolving opioid epidemic in Maine. The online survey revealed that practicing pharmacists in Maine are very aware of the potential for opioids to be misused for nonmedical purposes. Similarly, the preponderance (87.5%) of community pharmacists in Tennessee believed that opioid pain reliever abuse was a problem in their practice. Further, the Tennessee sample indicated that less than one fifth of prescribers or dispensers spent adequate time communicating with patients about the abuse potential of opioids (Hagemeier et al., 2014). Although the majority of Maine pharmacists indicated that opioid diversion, access, and security were issues, these were rated significantly lower than misuse. Possibly, given the spate of pharmacy robberies over the past decade (Smith et al., 2009), with a 27-fold increase from 2008 to 2012 in Maine (J. O’Malley, personal communication, May 27, 2015), many pharmacies may have already made improvements in security.
The training of pharmacists in the United States has changed considerably during the last two decades. A 5-year bachelor’s degree was sufficient to enter the field until the late 1990s, when a doctor of pharmacy degree became mandatory. Therefore, it is unclear whether the difference in level of concern about opioid diversion between Pharm.D.’s and bachelor’s-educated pharmacists is the result of less experience as a practitioner (i.e., bachelor’s pharmacists are more attuned to the needs of their communities) or that more Pharm.D.’s received their training in the “pain as the fifth vital sign” era. Conversely, a greater likelihood among Pharm.D.’s of using the M-PMP could reflect that opioid diversion receives greater attention in their education or it could be the result of younger pharmacists having greater technological sophistication with online resources. The finding that hospital pharmacists were less likely than others to use the M-PMP is not completely unexpected, as hospitals are not required to input controlled substances into the M-PMP. This data gap is problematic, as some patients present to the emergency department with lower back pain, claim an allergy to non-opioids, and request specific opioids by name (Weiner et al., 2015).
There were 332,500 M-PMP reports run on potential patients in 2014, of which 14.7% were initiated by pharmacists (J. Lipovsky, personal communication, June 15, 2015). Clearly, as less than half (39%) of Maine pharmacists are even registered to run reports, there is substantial room for improvement in M-PMP use. Insufficient time has been noted by others as a very common barrier to PMP use by community pharmacists in Indiana (Norwood & Wright, 2016). Only a limited number of pharmacy chains have required PMP use. Another contributing factor is that pharmacists’ license renewal, unlike that of prescribers, is not currently linked to PMP registration. There are also technical barriers in that the PMP is Internet based whereas some pharmacy systems rely on intranets because of security concerns. The M-PMP could also be improved by automatically converting the multiple opioids prescribed to single patients into morphine equivalents, which would make this information more useful for pharmacists.
The United States constitutes 4.6% of the world population but consumes 56% of the world’s morphine supply, 83% of the oxycodone supply, and 99% of the hydrocodone supply (Calabresi, 2015; International Narcotics Control Board, 2009). Within Maine, the total number of opioid prescriptions in 2014 was 8.8% higher than in 2006 but 3.5% lower than in 2010 (McCall et al., 2013). However, comparisons over time are complicated by the removal of propoxyphene from the U.S. market in 2010, reclassifying tramadol from unscheduled to Schedule IV in August 2014. Hydrocodone/acetaminophen was the most prescribed agent from retail pharmacies in the United States from 2007 until 2013 when it was overtaken by levothyroxine (Aitken et al., 2015). The present M-PMP findings that more than one fifth of the Maine population received a prescription opioid is consistent with and extends upon prior pharmacoepidemiological investigations (McCall et al., 2013; Paulozzi et al., 2014; Wright et al., 2014b).
Interestingly, this report identified very similar prescription frequencies for hydrocodone and oxycodone, which is very unlike the national preference for hydrocodone (Aitken et al., 2015). For example, hydrocodone was prescribed sixfold more commonly (68.9% vs. 11.7% of all opioid prescriptions) in Indiana (Wright et al., 2014b). Interestingly, individual provinces in Canada also show pronounced differences (Fischer et al., 2011). These substantial regional variations within the United States, as well as pronounced excess in use compared with countries to the north and south (International Narcotics Control Board, 2011), indicates that there are factors beyond nociception responsible for opioid prescription patterns. Because the M-PMP, like others, does not include information about the patient’s diagnose(s), we can only speculate the extent that economic, demographic, or sociocultural factors are responsible for these differences.
Buprenorphine accounted for approximately half of all opioid prescriptions for persons in their 20s relative to a negligible amount for octogenarians. Although this age difference was not unanticipated (Turner et al., 2015), the proportion within both young adult men and women was not. Because of the frequent reference to buprenorphine products in the DAP and because an even cursory Internet search of substance user groups pulls up simple, detailed, and plausible directions on how to convert the buprenorphine/naloxone film strips into an injectable product (see also Cicero et al., 2014b; Lavonas et al., 2014), Suboxone film strips may offer less of a pronounced benefit over the generic Zubsolv tablets than is generally appreciated.
The notion of one recreational agent serving as a “gateway” to another (Kandel & Logan, 1984) has been both influential and controversial. Although there is a temporal sequence that may occur for many users (e.g., cigarettes precede marijuana) who advance from more accessible to more prohibited agents, the view that prescription opioid misuse may lead to (i.e., causes) heroin misuse has only begun to be evaluated (Grau et al., 2007). The quarterly analysis of drug arrests, which identified a decrease in prescription opioids and a corresponding increase in heroin arrests, does fit with a gateway model. However, approximately half of heroin addicts, if given a choice, prefer prescription opioids over heroin (Cicero et al., 2014a), suggesting that opioid preferences are individualistic and may not uniformly escalate. Relative to 2010, there are indications in the M-PMP of a decrease in oxycodone (10.9%) and hydrocodone (21.8%) prescriptions, whereas buprenorphine has undergone a pronounced increase (65.0%, Supplemental Figure 5). Together, we are cautiously optimistic that health care providers, the general public, and policy makers have finally gained a deeper appreciation of the risks versus benefits of Schedule II opioids.
Some characteristics of Maine are important to contextualize the M-PMP and DAP findings. Maine is ranked first for highest median age (42.2 years), first for highest percentage of the population residing in rural areas (61.3%), the fourth lowest state for proportion of African Americans (1.0%), and first for fewest violent crimes (116/100K) in the country (Jones, 2010; U.S. Census Bureau, 2010, 2012). When Purdue Pharma (Stamford, CT) began aggressively promoting OxyContin to primary care physicians (Van Zee, 2009), these demographics may have conferred a false sense of immunity that resulted in Maine assuming such a prominent role in opioid use and misuse. The number of pharmacy robberies statewide decreased by 67.9% from 2012 to 2014 (J. O’Malley, personal communication, May 27, 2015).
The presence of a quantifiable level of crimes involving medical/recreational drugs should not be used to stigmatize the state. Over the past half-century, the first opioid used by heroin addicts has changed from heroin to a prescription opioid. Further, Whites and females outside of large urban areas now account for a greater proportion of heroin addicts (Cicero et al., 2014a), which is important considering the limited racial diversity of Maine. A contributing factor to our finding that arrests for Schedule II-IV drugs exceeded those for Schedule I agents is that marijuana appears to be a low priority among law enforcement. Because of the recently documented HIV outbreak among individuals in southeastern Indiana sharing needles to inject prescription opioids (Calabresi, 2015; Conrad et al. 2015), it is noteworthy that oxymorphone was relatively uncommon and pharmacies in Maine can distribute syringes (Ginley et al., 2002). Maine is divided into relatively few (16) counties. The finding that areas with more opioid prescriptions also had more arrests involving Schedule II opioids is important but should be verified in other, more populous states.
Our findings from the M-PMP and DAP have implications for patient care. Information provided by the DAP (which is an especially underused resource) and M-PMP could result in initiation and modification of pain contracts between patients and providers; increased monitoring via “pop” pill counts, urine screens, and more frequent PMP queries; and, in extreme cases, discontinuation of the prescribing of some medications or dismissal of the patient from practice. The age profile of opioid use in Maine may encourage increased vigilance of young adults prescribed buprenorphine and also older adults receiving other opioids.
Some limitations of these data sets and future directions are worthy of consideration. First, the online survey participants were representative of pharmacists statewide in terms of gender. The Maine Board of Pharmacy has not consistently obtained other demographics, which precludes further examination of the representativeness of this sample. These findings may be less generalizable to pharmacists in more urban states. Second, the M-PMP depends entirely on pharmacies—and the DAP is reliant on law enforcement—to submit accurate and complete information. Third, as noted earlier, the M-PMP data set does not contain information about diagnoses, which limits any inferences about the appropriateness of pharmacotherapy. Other efforts to characterize these have determined that back pain, extremity pain, and osteoarthritis patients account for more than half of chronic noncancer pain patients (Boudreau et al., 2009).
Finally, the findings from the M-PMP including that more than one fifth of the residents in each county received an opioid prescription in 2014 are likely an underestimate of the true level of prescription opioids and other agents. Long-term care facilities do not relay prescription information to the M-PMP. Tramadol only became a scheduled substance in the last half of 2014; therefore, Figures 1A and 2 should be interpreted in light of this caveat. International mail order pharmacies (Russell et al., 2015) may not have fully contributed to the M-PMP, and the Department of Veterans Affairs, which serves more than 4,000 patients, only provided data during the last quarter of 2014. Further, the M-PMP is legally prohibited from obtaining information from the nine methadone clinics, which serve 4,500 patients (Lawlor, 2015). As the track record of medical chemists to develop abuse-proof opioids has been underwhelming thus far (Conrad et al., 2015; Lavonas et al., 2014; Sansone & Sansone, 2015), future updates from the M-PMP and DAP with a focus on particular agents will be necessary.
Conclusions
Based on the three data sets, we are very conflicted about the opioid prescription epidemic being referred to as “iatrogenic” (Wright et al., 2014b). Prescribers and dispensers are providing the best care they can for patients where opioids are appropriate (Manchikanti et al., 2010). However, frequent reference to specific Schedule II opioids in the DAP, particularly oxycodone, and that Schedule II–IV substances were more common than Schedule I, as well as the substantial volume of opioid prescriptions in the M-PMP, indicate that the iatrogenic label may, unfortunately, be warranted. Pharmaceutical companies, patients, providers, and pharmacies have contributed to opioid misuse (Calabresi, 2015; Dyer, 2014; Manchikanti et al. 2010; Meier, 2013), and their concerted efforts, in conjunction with law enforcement, will be necessary to remediate the opioid misuse and diversion problem in Maine and nationally.
Acknowledgments
We gratefully acknowledge the pharmacists who responded to the online survey. Jane Jarvi, Ed.D., provided feedback on an earlier version of this manuscript. This article reflects the views of the authors and not the official policy of the Maine Office of Mental Health and Substance Abuse Services or the Maine Diversion Alert Program.
Conflict of Interest Statement
Brian J. Piper, John Lipovsky, Matthew A. Rodney, Robert P. Baker, Kenneth L. McCall, Stephanie D. Nichols, and Sarah L. Martin have no conflicts of interest. Clare E. Desrosiers is employed by the Maine Diversion Alert Program.
Footnotes
Data analysis for this manuscript was conducted using software provided by the National Institute of Environmental Health Sciences (T32 ES007060-31A1). This research was generously supported by internal grants to Sarah L. Martin and Brian J. Piper from the Husson University School of Pharmacy. Funders had no role in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the article for publication.
References
- Aitken M., Kleinrock M., Lyle J., Nass D., Caskey L. Medicines use and spending shifts: A review of the use of medicines in the U.S. in 2014. Parsippany, NJ: IMS Institute for Healthcare Informatics; 2015. Retrieved from http://www.redaccionmedica.com/contenido/images/IIHI_Use_of_Medicines_Report_2015.pdf. [Google Scholar]
- Alexander J. L., Burton J. H., Bradshaw J. R., Colin F. Suspected opioid-related emergency medical services encounters in a rural state, 1997-2002. Prehospital Emergency Care. 2004;8:427–430. doi: 10.1016/j.prehos.2004.06.019. doi:10.1080/312704001133. [DOI] [PubMed] [Google Scholar]
- Boudreau D., Von Korff M., Rutter C. M., Saunders K., Ray G. T., Sullivan M. D., Weisner C. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiology & Drug Safety. 2009;18:1166–1175. doi: 10.1002/pds.1833. doi:10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M. S., Hayes M. J., Thornton L. M. Methadone versus morphine for treatment of neonatal abstinence syndrome: A prospective randomized clinical trial. Journal of Perinatology. 2015;35:278–283. doi: 10.1038/jp.2014.194. doi:10.1038/jp.2014.194. [DOI] [PubMed] [Google Scholar]
- Calabresi M. Why America can’t kick its painkiller problem. Time. 2015, June 4 Retrieved from http://time.com/3908648/why-america-cant-kick-its-painkiller-problem. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50) 2015 Retrieved from http://www.samhsa.gov/data.
- Cicero T. J., Ellis M. S., Surratt H. L., Kurtz S. P. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014a;71:821–826. doi: 10.1001/jamapsychiatry.2014.366. doi:10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Cicero T. J., Ellis M. S., Surratt H. L., Kurtz S. P. Factors contributing to the rise of buprenorphine misuse: 2008-2013. Drug and Alcohol Dependence. 2014b;142:98–104. doi: 10.1016/j.drugalcdep.2014.06.005. doi:10.1016/j.drugalcdep.2014.06.005. [DOI] [PubMed] [Google Scholar]
- Conrad C., Bradley H. M., Broz D., Buddha S., Chapman E. L., Galang R. R., Duwve J. M. the Centers for Disease Control and Prevention (CDC) Community outbreak of HIV infection linked to injection drug use of oxymorphone — Indiana, 2015. Morbidity and Mortality Weekly Report. 2015;64:443–444. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6416a4.htm. [PMC free article] [PubMed] [Google Scholar]
- Dyer O. Kentucky seeks $1bn from Purdue Pharma for misrepresenting addictive potential of oxycodone. BMJ. 2014;349:g6605. doi: 10.1136/bmj.g6605. doi:10.1136/bmj.g6605. [DOI] [PubMed] [Google Scholar]
- Fischer B., Jones W., Krahn M., Rehm J. Differences and over-time changes in levels of prescription opioid analgesic dispensing from retail pharmacies in Canada, 2005-2010. Pharmacoepidemiology & Drug Safety. 2011;20:1269–1277. doi: 10.1002/pds.2190. doi:10.1002/pds.2190. [DOI] [PubMed] [Google Scholar]
- Ginley B., Patterson S. L., Nickerson N., Bruno J., Grotton J. Maine Board of Pharmacy strongly supports unrestricted sale of sterile syringes. Journal of the American Pharmaceutical Association. 2002;42(Supplement 2):S24–S25. doi: 10.1331/1086-5802.42.0.s24.ginley. doi:10.1331/1086-5802.42.0.S24.Ginley. [DOI] [PubMed] [Google Scholar]
- Grau L. E., Dasgupta N., Harvey A. P., Irwin K., Givens A., Kinzly M. L., Heimer R. Illicit use of opioids: Is OxyContin a “gateway drug”? American Journal on Addictions. 2007;16:166–173. doi: 10.1080/10550490701375293. doi:10.1080/10550490701375293. [DOI] [PubMed] [Google Scholar]
- Haegerich T. M., Paulozzi L. J., Manns B. J., Jones C. M. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug and Alcohol Dependence. 2014;145:34–47. doi: 10.1016/j.drugalcdep.2014.10.001. doi:10.1016/j.drugalcdep.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagemeier N. E., Murawski M. M., Lopez N. C., Alamian A., Pack R. P. Theoretical exploration of Tennessee community pharmacists’ perceptions regarding opioid pain reliever abuse communication. Research in Social & Administrative Pharmacy. 2014;10:562–575. doi: 10.1016/j.sapharm.2013.07.004. doi:10.1016/j.sapharm.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Heimer R., Dasgupta N., Irwin K. S., Kinzly M., Harvey A. P., Givens A., Grau L. E. Chronic pain, addiction severity, and misuse of opioids in Cumberland County, Maine. Addictive Behaviors. 2012;37:346–349. doi: 10.1016/j.addbeh.2011.11.017. doi:10.1016/j.addbeh.2011.11.017. [DOI] [PubMed] [Google Scholar]
- International Narcotics Control Board. Report of the International Narcotics Control Board for 2008 (p. 20) New York, NY: United Nations; 2009. Retrieved from https://www.incb.org/documents/Publications/AnnualReports/AR2008/AR_08_English.pdf. [Google Scholar]
- International Narcotics Control Board. Report of the International Narcotics Control Board on the Availability of Internationally Controlled Drugs: Ensuring Adequate Access for Medical and Scientific Purposes. New York, NY: United Nations; 2011. Retrieved from http://www.unodc.org/documents/lpo-brazil/noticias/2011/03-marco/Jife/Report_of_the_Board_on_the_availability_of_controlled_substances.pdf. [Google Scholar]
- Johnston L. D., O’Malley P. M., Miech R. A., Bachman J. G., Schulenberg J. E. Monitoring the Future national survey results on drug use: 1975-2014: Overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- Jones B. Median age by state. USA Today. 2010 Retrieved from http://usatoday30.usatoday.com/news/nation/census/median-age-by-state.htm. [Google Scholar]
- Joranson D. E., Gilson A. M. Drug crime is a source of abused pain medications in the United States. Journal of Pain and Symptom Management. 2005;30:299–301. doi: 10.1016/j.jpainsymman.2005.09.001. doi:10.1016/j.jpainsymman.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Kandel D. B., Logan J. A. Patterns of drug use from adolescence to young adulthood: I. Periods of risk for initiation, continued use, and discontinuation. American Journal of Public Health. 1984;74:660–666. doi: 10.2105/ajph.74.7.660. doi:10.2105/AJPH.74.7.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle M. R., Zhang F., Ross-Degnan D., Wharam J. F. Rates of opioid dispensing and overdose after introduction of abuse-deterrent extended-release oxycodone and withdrawal of propoxyphene. JAMA Internal Medicine. 2015;175:978–987. doi: 10.1001/jamainternmed.2015.0914. doi:10.1001/jamainternmed.2015.0914. [DOI] [PubMed] [Google Scholar]
- Lavonas E. J., Severtson S. G., Martinez E. M., Bucher-Bartelson B., Le Lait M.-C., Green J. L., Dart R. C. Abuse and diversion of buprenorphine sublingual tablets and film. Journal of Substance Abuse Treatment. 2014;47:27–34. doi: 10.1016/j.jsat.2014.02.003. doi:10.1016/j.jsat.2014.02.003. [DOI] [PubMed] [Google Scholar]
- Lawlor J. Thousands of patients lose if state cuts methadone benefit. Portland Press Herald. 2015, January 23 Retrieved from http://www.pressherald.com/2015/01/23/thousands-of-patients-lose-if-state-cuts-methadone-benefit. [Google Scholar]
- Manchikanti L., Fellows B., Ailinani H., Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: A ten-year perspective. Pain Physician. 2010;13:401–435. [PubMed] [Google Scholar]
- Martin S. L., Baker R. P., Piper B. J. Evaluation of urban-rural differences in pharmacy practice needs in Maine with the MaPPNA. Pharmacy Practice. 2015;13:669. doi: 10.18549/PharmPract.2015.04.669. doi:10.18549/PharmPract.2015.04.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin T. C., Rocque M. Accidental and non-accidental ingestion of methadone and buprenorphine in childhood: A single center experience, 1999-2009. Current Drug Safety. 2011;6:12–16. doi: 10.2174/157488611794480034. doi:10.2174/157488611794480034. [DOI] [PubMed] [Google Scholar]
- Maxwell J. C. The prescription drug epidemic in the United States: A perfect storm. Drug and Alcohol Review. 2011;30:264–270. doi: 10.1111/j.1465-3362.2011.00291.x. doi:10.1111/j.1465-3362.2011.00291.x. [DOI] [PubMed] [Google Scholar]
- McCall K. L., III, Tu C., Lacroix M., Holt C., Wallace K. L., Balk J. Controlled substance prescribing trends and physician and pharmacy utilization patterns: Epidemiological analysis of the Maine Prescription Monitoring Program from 2006 to 2010. Journal of Substance Use. 2013;18:467–475. doi:10.3109/14659891.2012.685794. [Google Scholar]
- Meier B. Walgreen to pay 80 million fine in D.E.A. inquiry. The New York Times. 2013, June 11 Retrieved from http://www.nytimes.com/2013/06/12/business/walgreen-to-pay-80-million-settlement-over-painkiller-sales.html?_r=0. [Google Scholar]
- Norwood C. W., Wright E. R. Promoting consistent use of prescription drug monitoring programs (PDMP) in outpatient pharmacies: Removing administrative barriers and increasing awareness of Rx drug abuse. Research in Social and Administrative Pharmacy. 2016;12:509–514. doi: 10.1016/j.sapharm.2015.07.008. doi:10.1016/j.sapharm.2015.07.008. [DOI] [PubMed] [Google Scholar]
- Patrick S. W., Davis M. M., Lehman C. U., Cooper W. O. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. Journal of Perinatology. 2015;35:650–655. doi: 10.1038/jp.2015.36. doi: 10.1038/jp.2015.36. Erratum in Journal of Perinatology, 35, 667. doi:10.1038/jp.2015.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul J. A., Logan B. A., Krishnan R., Heller N. A., Morrison D. G., Pritham U. A., Hayes M. J. Development of auditory event-related potentials in infants prenatally exposed to methadone. Developmental Psychobiology. 2014;56:1119–1128. doi: 10.1002/dev.21160. doi:10.1002/dev.21160. [DOI] [PubMed] [Google Scholar]
- Paulozzi L., Baldwin G. the Centers for Disease Control and Prevention (CDC) CDC grand rounds: Prescription drug overdoses – a U.S. epidemic. Morbidity and Mortality Weekly Report. 2012;61:10–13. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6101a3.htm. [PubMed] [Google Scholar]
- Paulozzi L. J., Mack K. A., Hockenberry J. M. Vital signs: Variation among states in prescribing opioid pain relievers and benzodiazepines – United States, 2012. Morbidity and Mortality Weekly Report. 2014;63:563–568. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6326a2.htm. [PMC free article] [PubMed] [Google Scholar]
- Paulozzi L. J., Ryan G. W. Opioid analgesics and rates of fatal drug poisoning in the United States. American Journal of Preventive Medicine. 2006;31:506–511. doi: 10.1016/j.amepre.2006.08.017. doi:10.1016/j.amepre.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Roche T. The potent perils of a miracle drug. Time. 2000, December 31 Retrieved from http://content.time.com/time/magazine/article/0,9171,93319,00.html. [PubMed] [Google Scholar]
- Rosenberg D.2002, April 21Oxy’s offspring NewsweekRetrieved from http://www.newsweek.com/oxys-offspring-142923 [PubMed] [Google Scholar]
- Russell E. Judge strikes down Maine law allowing residents to buy drugs from foreign pharmacies. Portland Press Herald. 2015, February 24 Retrieved from http://www.pressherald.com/2015/02/24/maine-residents-cant-order-drugs-from-foreign-pharmacies-judge-rules/ [Google Scholar]
- Sansone R. A., Sansone L. A. Buprenorphine treatment for narcotic addiction: Not without risks. Innovations in Clinical Neuroscience. 2015;12:32–36. [PMC free article] [PubMed] [Google Scholar]
- Smith M. Y., Graham J. A., Haddox J. D., Steffey A. RxPATROL: A Web-based tool for combating pharmacy theft. Journal of the American Pharmacists Association. 2009;49:599–603. doi: 10.1331/JAPhA.2009.08028. doi: 10.1331/JAPhA.2009.08028. [DOI] [PubMed] [Google Scholar]
- Sorg M. H., Greenwald M. Patterns of drug-related mortality in Maine, 1997-2002. Maine Policy Review. 2003;12:84–96. [Google Scholar]
- Turner L., Kruszewski S. P., Alexander G. C. Trends in the use of buprenorphine by office-based physicians in the United States, 2003-2013. American Journal on Addictions. 2015;24:24–29. doi: 10.1111/ajad.12174. doi:10.1111/ajad.12174. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Violent crime rate, 2007. 2010 Retrieved from https://www.census.gov/library/publications/2009/compendia/statab/129ed/rankings.html.
- U.S. Census Bureau. Growth in urban population outpaces rest of nation, Census Bureau reports. 2012, March 26 Retrieved from http://www.census.gov/newsroom/releases/archives/2010_census/cb12-50.html.
- Van Zee A. The promotion and marketing of Oxycontin: Commercial triumph, public health tragedy. American Journal of Public Health. 2009;99:221–227. doi: 10.2105/AJPH.2007.131714. doi:10.2105/AJPH.2007.131714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner M., Chen L. H., Makuc D. M., Anderson R. N., Miniño A. M. NCHS data brief, no 81. Hyattsville, MD: National Center for Health Statistics; 2011. Drug poisoning deaths in the United States, 1980–2008. [PubMed] [Google Scholar]
- Weiner S. G., Griggs C. A., Langlois B. K., Mitchell P. M., Nelson K. P., Friedman F. D., Feldman J. A. Characteristics of emergency department “doctor shoppers.”. The Journal of Emergency Medicine. 2015;48:424–431. doi: 10.1016/j.jemermed.2014.11.008. e1. doi:10.1016/j.jemermed.2014.11.008. [DOI] [PubMed] [Google Scholar]
- Wermeling D. P. Review of naloxone safety for opioid overdose: Practical considerations for new technology and expanded public access. Therapeutic Advances in Drug Safety. 2015;6:20–31. doi: 10.1177/2042098614564776. doi:10.1177/2042098614564776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright E. R., Kooreman H. E., Greene M. S., Chambers R. A., Banerjee A., Wilson J. The iatrogenic epidemic of prescription drug abuse: County-level determinants of opioid availability and abuse. Drug and Alcohol Dependence. 2014b;138:209–215. doi: 10.1016/j.drugalcdep.2014.03.002. doi:10.1016/j. drugalcdep.2014.03.002. [DOI] [PubMed] [Google Scholar]