Abstract
Objective:
Although major depressive disorder (MDD) and heavy episodic drinking (HED, 4+/5+ drinks in a single sitting for women/men) are common among young adults in college, the relationship between the two remains unclear. This study examined the association between MDD and HED in this population, the effect of gender on this association, and whether comorbid MDD and heavy alcohol use are associated with higher rates of mental health treatment engagement.
Method:
The study comprised 61,561 (65.3% female) undergraduate students who answered an online survey on depression, alcohol use, and treatment engagement in the past year. Hierarchical linear regressions examined the association between MDD and alcohol use (HED and peak blood alcohol concentration [pBAC]) and whether gender moderated these associations. Logistic regressions were then conducted to examine the influence of MDD, heavy alcohol use, and gender on treatment engagement.
Results:
Students with MDD reported more frequent HED and higher pBAC than did students without MDD; this was especially true for female students. Rates of treatment engagement were higher among women than men, among students with MDD than students without MDD, and among female students with HED than women without HED.
Conclusions:
The presence of an association between MDD and heavy alcohol use suggests the need for systematic screenings of both conditions. Low rates of treatment engagement in college students with MDD and heavy alcohol use calls for the development of strategies to engage this high-risk group in treatment.
Approximately 40% of college students report engaging in heavy episodic drinking (HED, defined as 4+/5+ drinks in a single sitting for women/men; Wechsler et al., 2001) at least once in the past 2 weeks, and 23% report engaging in HED at least three times in the previous 2 weeks (Wechsler & Nelson, 2008). Such heavy drinking takes a considerable toll: an estimated 1,800 deaths, 97,000 sexual assaults, and 599,000 injuries are attributable to alcohol use among college students on a yearly basis (Hingson et al., 2005, 2009). Alcohol is also associated with 66% of college suicides (the third leading cause of death for young adults; Barrios et al., 2000). Given that there are approximately 20.6 million college students in the United States (Snyder & Dillow, 2015), it is crucial to determine factors contributing to HED and its sequelae in order to design better prevention and treatment strategies.
Major depressive disorder (MDD) is also common among college students, with prevalence rates ranging between 7% and 9% (Blanco et al., 2008; Eisenberg et al., 2013). In a nationwide survey, 32% of college students reported having felt “so depressed that it was difficult to function” at least once in the past year (American College Health Association, 2014, p. 15). Given the prevalence of heavy alcohol use and symptoms of depression in the college population, a considerable number of students report co-morbid MDD and heavy drinking (Cranford et al., 2009). Despite the common co-occurrence of MDD and alcohol use, it is still unclear whether one condition constitutes a risk factor for the other among young adults in college. The few studies that have examined the relationship between MDD and alcohol use have had mixed results. Dawson et al. (2005) observed an association between MDD and higher risk for alcohol dependence and HED among young adults (ages 18–29) not in college, yet not among young adults in college. Similarly, an investigation of 412 female undergraduate students did not find an association between depression and HED (here defined as consuming five or more drinks; Vickers et al., 2004). Moreover, in a previous study from our group, Cranford et al. (2009) found that, among 2,843 individuals (1,181 undergraduate and 1,662 graduate students), those with MDD had lower risk to engage in frequent HED than those with no depression. Findings regarding the association between nonclinical depressive symptoms and alcohol use are also mixed. Among college students, depressive symptoms have been found to be associated with ever engaging in HED (Valentiner et al., 2004), problematic alcohol use (Dvorak et al., 2013), and higher daily alcohol use (Pedrelli et al., 2011) but not with past-month drinking days (Lamis et al., 2010), drinks per month (Gonzalez et al., 2011), weekly drinks (Kenney et al., 2013), and frequent heavy drinking (Lamis et al., 2010; Vickers et al., 2004).
These mixed findings may be attributable in large part to three factors. First, several studies have combined undergraduate and graduate students (Cranford et al., 2009; Dawson et al., 2005), although heavy drinking is significantly more prevalent among undergraduate students (Cranford et al., 2009). Second, previous studies with college students have exhibited considerable variability in which drinking behaviors they have examined to be associated with depression. For example, some studies have examined presence of any heavy drinking, some frequency of heavy drinking, and some number of weekly drinks. A study of 14,000 individuals from 18 to 76 years old found that the associations between depression and alcohol use varied based on the drinking behavior considered. For example, depression was associated with both past-year typical quantity of alcohol use and frequency of HED but not with past-year frequency of any alcohol consumption or annual volume of alcohol consumed (Graham et al., 2007). Moreover, current definitions of heavy drinking (consumption of 4/5 drinks for women/men in a row or consumption of 4/5 drinks for women/men within 2 hours; National Institute on Alcohol Abuse and Alcoholism, 2004) are limited by not accounting for the individual’s weight, and thus may not accurately measure the actual degree of alcohol intoxication (see Borsari et al., 2001).
Third, and most important, many studies with college students have not examined gender effects in the association between depression and heavy drinking. Compared with female college students, higher numbers of male students meet criteria for alcohol abuse and dependence, engage in HED (Harford et al., 2006; Wechsler et al., 1994), endorse higher alcohol consumption (O’Donnell et al., 2006; Wechsler et al., 1994; White et al., 2006), and report more alcohol-related problems (Geisner et al., 2004; Harrell & Karim, 2008). Furthermore, women and men metabolize alcohol differently, which may lead to different blood alcohol levels even when consuming the same amount of alcohol (Thomasson, 1995). However, depressive symptoms are more common in female than male students (Harford et al., 2006; Weitzman, 2004). Preliminary evidence suggests that gender may moderate the relationship between depressive symptoms and drinking behavior. In college students, men have demonstrated a stronger relationship between psychological distress and weekly alcohol consumption than women (Geisner et al., 2004), and a relationship between weekend elevated sadness and subsequent elevated weekday alcohol use was found in male but not female college students (Hussong et al., 2011). Conversely, Cranford et al. (2009) found that the risk for frequent HED among male students with MDD was lower than that for female students with MDD. These findings highlight the need for more in-depth analysis of the effect of gender on the association between depression and heavy alcohol use in college students.
Engagement in mental health treatment is very relevant for students experiencing depressive symptoms and HED. Heavy alcohol use is associated with significant impairment in functioning, and the presence of co-occurring depressive symptoms is associated with an even higher risk for alcohol-related problems (Camatta & Nagoshi, 1995; Dennhardt & Murphy, 2011; Harrell & Karim, 2008; Weitzman et al., 2004). Although between one third and one half of the students reporting only mood problems are engaged in treatment, very few (5%–13%) students with only HED are in treatment (Blanco et al., 2008; Cranford et al., 2009). However, the proportion of students with both HED and MDD who are in treatment remains unknown. One study found that among heavy drinking students, depressive symptoms are associated with higher informal (talking to a friend) and formal (talking with a counselor or medical provider) help seeking (Buscemi et al., 2010). However, the study examined formal and informal help seeking together. Moreover, although a higher proportion of female than male students seek treatment for any disorder (Eisenberg et al., 2011a), it is unclear whether similar gender differences exist among students with co-occurring depression and HED. Information on the proportion of students with co-occurring MDD and HED receiving mental health treatment may be of importance for outreach programs.
The current study examined two related research questions in a large, multisite sample of undergraduate students. First, we aimed to investigate the association between MDD and heavy alcohol use as well as peak blood alcohol concentration (pBAC) among undergraduate students and the effect of gender on these associations. We also addressed limitations of previous research by measuring both heavy alcohol use and pBAC (a method that accounts for weight and gender; Thomasson, 1995). We hypothesized that students with MDD would drink more (have both more frequent HED and higher pBAC) than those without MDD. Consistent with previous research examining MDD (Cranford et al., 2009), we hypothesized that the association between depression and heavy alcohol use and pBAC would be stronger in women. Second, we examined the effect of MDD, heavy alcohol use, and gender on mental health treatment use among students. As previously noted, this is an important question that, to our knowledge, has not yet been examined. Given previous studies suggesting a higher help-seeking behavior among women and among students with co-occurring heavy drinking and depressive symptoms, we hypothesized that students with comorbid MDD and HED would engage in mental health treatment significantly more than those with only MDD and that this association would be stronger among women.
Method
Study design
This study is a secondary analysis of multiyear cross-sectional data from the Healthy Minds Study (HMS; Eisenberg et al., 2007) for college and university student populations in the United States. HMS is an annual web-based survey that examines mental health and service utilization; data were drawn from six waves of HMS (2007, 2009–2013).
Participants
The current study examines a sample of undergraduate students (N = 61,561) enrolled at more than 100 institutions. In 2007 and 2009, a random sample of 1,000 students at each institution was invited via postal mail (with a $2 incentive) followed by email reminders. Since 2010, recruitment has been conducted entirely by email, with random samples of 4,000 students at larger institutions and full student populations at institutions with fewer than 4,000 students. All students were informed that they were entered into a cash sweepstakes regardless of their participation. To engage nonresponders, up to three reminders were sent over the monthlong data collection period. Response rates ranged from 23.2% to 42.7% over the 7-year span of 2007 to 2013. The survey was administered using DatStat Illume online survey software (DatStat, Inc., Seattle, WA). The study was approved by the Institutional Review Boards at all participating institutions. Students were presented with an online consent form and voluntarily granted consent before entering the survey.
To adjust for potential differences between survey responders and nonresponders, we constructed sample probability weights. For students in the initial random samples, we obtained administrative data from participating institutions, including gender, academic level, race/ethnicity, and grade point average. We then constructed response weights, equal to 1 divided by the predicted probability of survey response, using a logistic regression to estimate the predicted probability of response based on these variables. Thus, weights are larger for respondents with underrepresented characteristics, ensuring that all estimates are representative of the full population in terms of basic demographic and other characteristics. This method follows the approach used in the National Comorbidity Survey Replication to develop a nonresponse adjustment weight (Kessler et al., 2004). Nonresponse weights to adjust for nonresponse bias have been used by other epidemiologic surveys of mental health and substance use (Grant et al., 2004; Substance Abuse and Mental Health Services Administration, 2007).
Measures
Depressive symptoms.
MDD was measured using the Patient Health Questionnaire–9 (PHQ-9), a validated screening instrument based on the core symptoms of a major depressive episode (Spitzer et al., 1999). The instrument yields individual scores ranging from 0 to 27, with higher number indicating more severe depressive symptoms. Validation studies of the PHQ-9 have shown the instrument to be internally consistent and highly correlated with clinical diagnosis of MDD (Diez-Quevedo et al., 2001; Löwe et al., 2004; Manea et al., 2015), and it has shown high internal consistency in previous research (α = .84; Eisenberg et al., 2011b) and in the present sample (α = .87). In the current study, we categorized presence of MDD using the cutoff score of PHQ-9 equal to 10, which has been shown to have adequate sensitivity and specificity for diagnosing MDD (Kroenke et al., 2001; Manea et al., 2015; Manea et al., 2012).
Alcohol use.
HED was measured based on responses to a question inquiring about frequency of consumption of four or five drinks or more in a row during the past 2 weeks for women and men, respectively. Response options included zero, one time, two times, three to five times, six to nine times, and ten or more times. A subsample (n = 13,316 from the 2012 and 2013 HMS) was also asked about the number of drinks they had in a row during the most recent HED episode. The eight response options were 4 or 5 drinks (for women and men, respectively), 5 drinks, 6 drinks, 7 drinks, 8 drinks, 9 drinks, 10–14 drinks, and 15 or more drinks. Because the data set included the specific number of drinks consumed during the most recent heavy drinking episode, gender, the amount of time spent drinking, and the participant’s body weight, we were able to calculate a pBAC using the Matthews and Miller (1979) equation and an average metabolism rate of .017 g/dl per hour. This approach has been used in our previous research (Borsari et al., 2012) and is recommended above other drinking indices when gender differences are being examined (Borsari et al., 2001).
Treatment engagement.
Participant engagement in mental health treatment was measured by the following dichotomous (yes/no) item: “In the past 12 months have you received counseling or therapy for your mental or emotional health from a health professional (such as psychiatrist, psychologist, social worker, or primary care doctor)?”
Data analysis
We first examined the association between MDD and alcohol use by conducting equivalent hierarchical linear ordinary least squares regression models for HED and pBAC. Each model was constructed using three steps. In the first step, the covariates age, race/ethnicity (White vs. non-White), citizenship, maternal education (a proxy for socioeconomic status), and gender were entered. In the second step, we added a binary measure of MDD status (positive/negative screen on PHQ-9). In the third step, we added an interaction term of gender and MDD status. We then conducted a hierarchical logistic regression to examine the associations among MDD, alcohol use, and gender on treatment utilization. The first step included covariates from the ordinary least squares regression models. The second step added measures of MDD status (absence/presence) and any HED (binary variable indicating presence of any HED). The third step added terms of two-way interaction of gender and MDD, gender and HED, and MDD and HED. The fourth step added a three-way interaction of gender, MDD status, and HED. We then conducted post hoc analyses by examining marginal effects. Models were adjusted for survey nonresponse, using the weights described above. All analyses were conducted using Stata 12 (StataCorp LP, College Station, TX). We conducted post hoc analyses and computed marginal effects to examine significant interaction terms.
Results
Sample characteristics
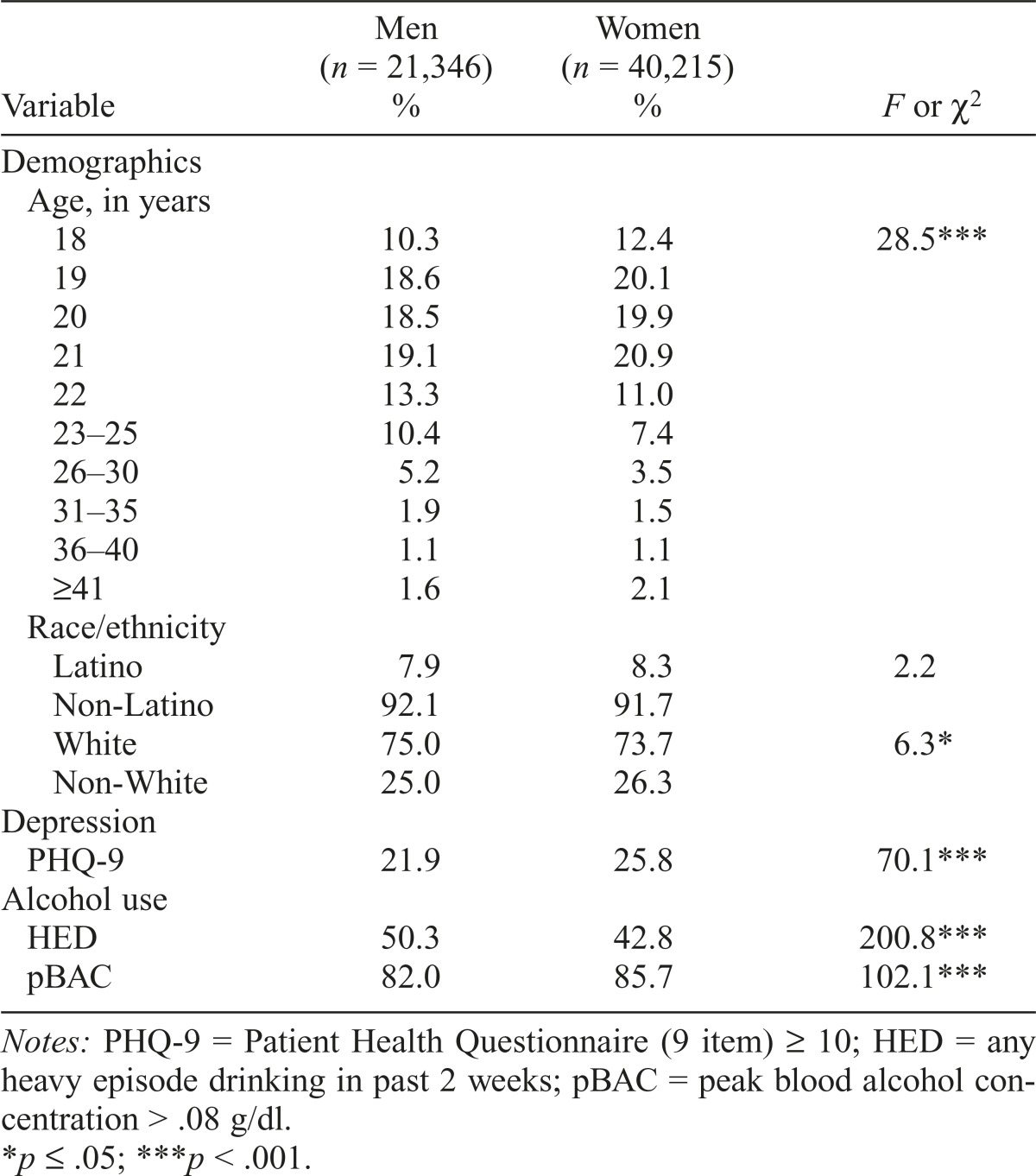
The sample comprised 61,561 undergraduate students (65.3% female; Table 1). The majority of the sample was White (74.3%) and between 18 and 22 years old (82.3%). Overall, 46.0% (50.3% male, 42.8% female) of students reported at least one episode of HED during the past 2 weeks, and 24.1% of the sample screened positive for MDD, with rates significantly higher among women (25.8%) relative to men (21.9%). Co-occurring MDD and HED in the previous two weeks was present in 11.6% of the participants (11.7% of females, 11.4% of males).
Table 1.
Demographic and clinical variables (N = 61,561)
| Variable | Men (n = 21,346) % | Women (n = 40,215) % | F or χ2 |
| Demographics | |||
| Age, in years | |||
| 18 | 10.3 | 12.4 | 28.5*** |
| 19 | 18.6 | 20.1 | |
| 20 | 18.5 | 19.9 | |
| 21 | 19.1 | 20.9 | |
| 22 | 13.3 | 11.0 | |
| 23–25 | 10.4 | 7.4 | |
| 26–30 | 5.2 | 3.5 | |
| 31–35 | 1.9 | 1.5 | |
| 36–40 | 1.1 | 1.1 | |
| ≥41 | 1.6 | 2.1 | |
| Race/ethnicity | |||
| Latino | 7.9 | 8.3 | 2.2 |
| Non-Latino | 92.1 | 91.7 | |
| White | 75.0 | 73.7 | 6.3* |
| Non-White | 25.0 | 26.3 | |
| Depression | |||
| PHQ-9 | 21.9 | 25.8 | 70.1*** |
| Alcohol use | |||
| HED | 50.3 | 42.8 | 200.8*** |
| pBAC | 82.0 | 85.7 | 102.1*** |
Notes: PHQ-9 = Patient Health Questionnaire (9 item) ≥ 10; HED = any heavy episode drinking in past 2 weeks; pBAC = peak blood alcohol concentration > .08 g/dl.
p ≤ .05;
p < .001.
Relationships between heavy episodic drinking, peak blood alcohol concentration, major depressive disorder, and gender
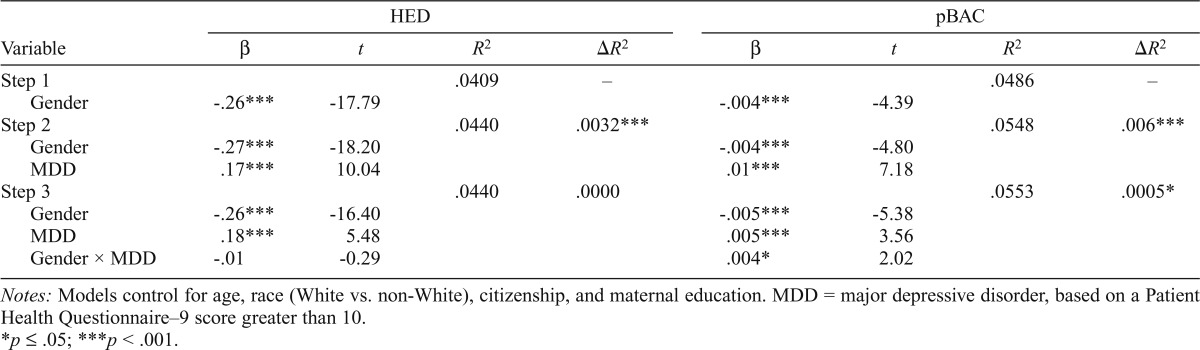
In the hierarchical linear regression models exploring relationships between frequency of HED, MDD, and gender (Table 2, left panel), we found that gender and MDD, but not their interaction, were significant predictors of HED frequency. Significantly more variance was explained when MDD was added along with gender to the model (ΔR2 = .0032).
Table 2.
Associations of gender and major depressive disorder (MDD) with heavy episodic drinking (HED) and peak blood alcohol concentration (pBAC)
| Variable | HED |
pBAC |
||||||
| β | t | R2 | ΔR2 | β | t | R2 | ΔR2 | |
| Step 1 | .0409 | – | .0486 | – | ||||
| Gender | -.26*** | -17.79 | -.004*** | -4.39 | ||||
| Step 2 | .0440 | .0032*** | .0548 | .006*** | ||||
| Gender | -.27*** | -18.20 | -.004*** | -4.80 | ||||
| MDD | .1 7*** | 10.04 | .01*** | 7.18 | ||||
| Step 3 | .0440 | .0000 | .0553 | .0005* | ||||
| Gender | -.26*** | -16.40 | -.005*** | -5.38 | ||||
| MDD | .1 8*** | 5.48 | .005*** | 3.56 | ||||
| Gender × MDD | -.01 | -0.29 | .004* | 2.02 | ||||
Notes: Models control for age, race (White vs. non-White), citizenship, and maternal education. MDD = major depressive disorder, based on a Patient Health Questionnaire–9 score greater than 10.
p ≤ .05;
p < .001.
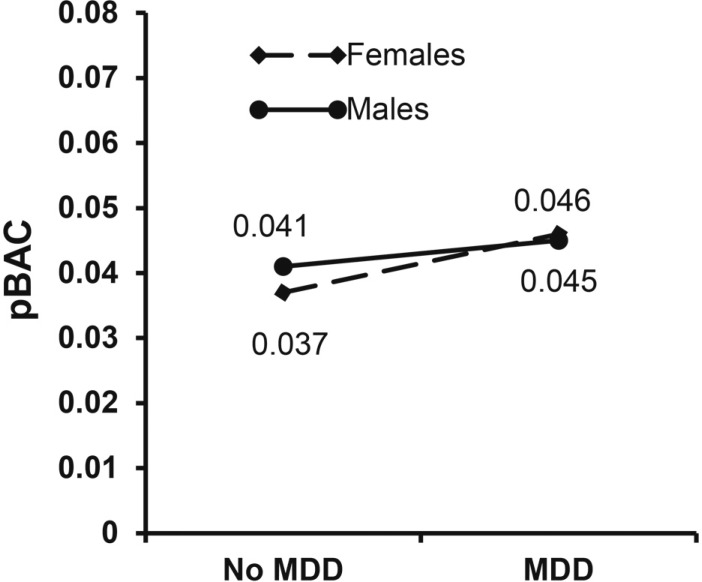
Hierarchical linear regression models exploring the relationships between pBAC, MDD, and gender (Table 2, right panel) indicated that gender, MDD, and their interaction were all significant predictors of pBAC and that each step explained significantly more variance. Post hoc analyses of average marginal effects showed that women with MDD had .009 g/dl higher pBAC than women without MDD (p < .001), compared with a .004 g/dl higher pBAC for men with MDD relative to men without MDD (p < .001; Figure 1).
Figure 1.
Peak blood alcohol concentration (pBAC) and major depressive disorder (MDD) in female and male students
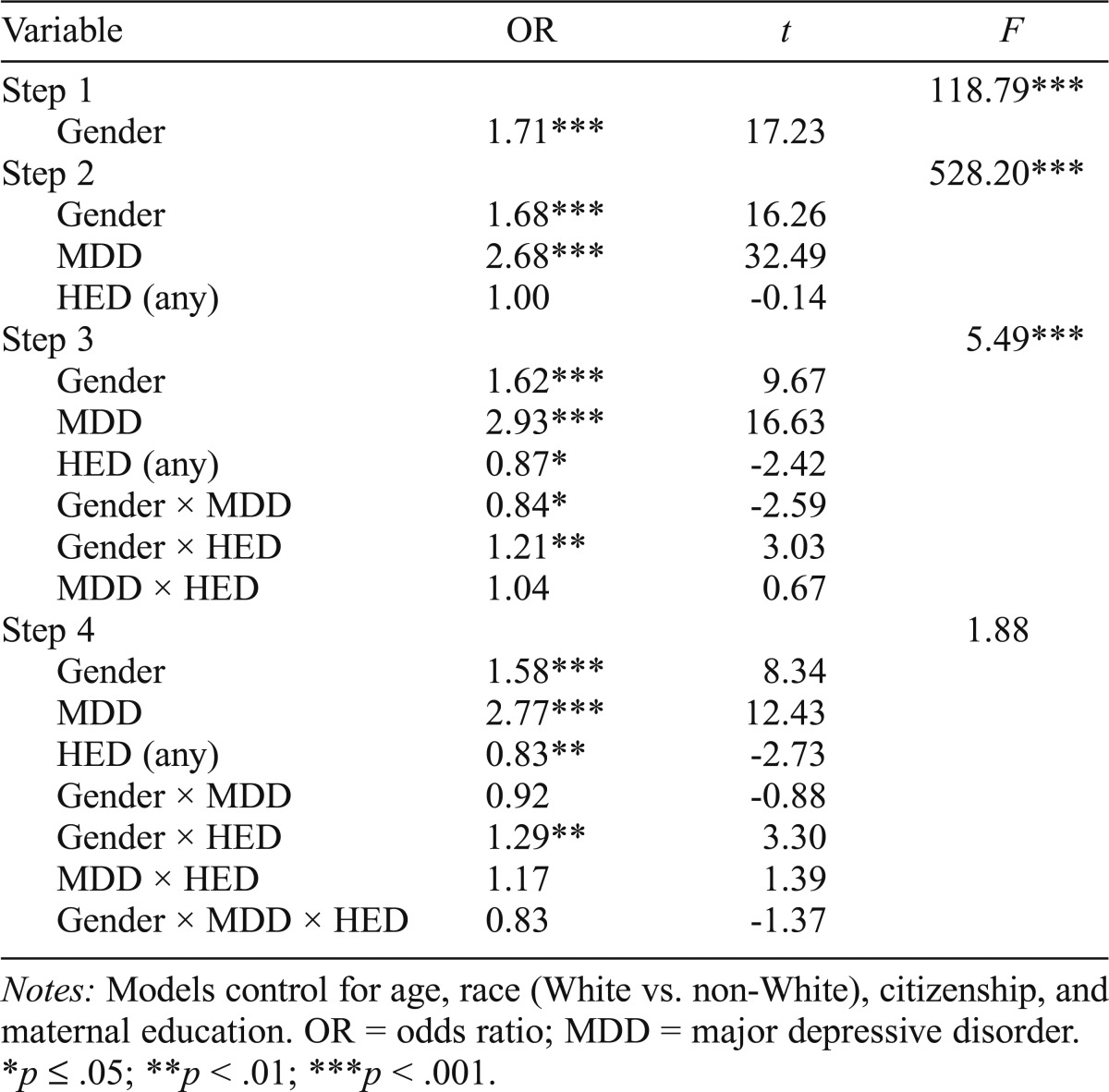
Relationships between treatment utilization, heavy episodic drinking, major depressive disorder, and gender
In the hierarchical logistic regressions examining treatment engagement in the past year (Table 3), women and students with MDD had significantly increased odds of treatment utilization. Post hoc analyses of the significant interaction of gender and HED revealed that the difference in proportion of students with and without MDD having engaged in mental health treatment was higher in women (31.1% vs. 15.8%, p < .001) than in men (23.8% vs. 9.9%, p < .001). Similarly, the difference between students with and without HED who engaged in treatment was higher among women (21.3% vs. 18.6%, p < .001) than among men (12.8% vs. 13.2%, p = .16).
Table 3.
Multiple logistic regressions testing the associations of gender, depression, and heavy episodic drinking (HED) with treatment engagement
| Variable | OR | t | F |
| Step 1 | 118.79*** | ||
| Gender | 1.71 *** | 17.23 | |
| Step 2 | 528.20*** | ||
| Gender | 1.68*** | 16.26 | |
| MDD | 2.68*** | 32.49 | |
| HED (any) | 1.00 | -0.14 | |
| Step 3 | 5.49*** | ||
| Gender | 1.62*** | 9.67 | |
| MDD | 2.93*** | 16.63 | |
| HED (any) | 0.87* | -2.42 | |
| Gender × MDD | 0.84* | -2.59 | |
| Gender × HED | 1.21** | 3.03 | |
| MDD × HED | 1.04 | 0.67 | |
| Step 4 | 1.88 | ||
| Gender | 1.58*** | 8.34 | |
| MDD | 2 77*** | 12.43 | |
| HED (any) | 0.83** | -2.73 | |
| Gender × MDD | 0.92 | -0.88 | |
| Gender × HED | 1.29** | 3.30 | |
| MDD × HED | 1.17 | 1.39 | |
| Gender × MDD × HED | 0.83 | -1.37 |
Notes: Models control for age, race (White vs. non-White), citizenship, and maternal education. OR = odds ratio; MDD = major depressive disorder.
p ≤ .05;
p < .01;
p < .001.
Discussion
The current study revealed several unique and important associations among gender, MDD, HED, and mental health treatment utilization among college students. First, college students with MDD reported higher frequency of HED and higher levels of alcohol intoxication. Second, the association between MDD and higher alcohol intoxication during a heavy drinking episode was stronger in female than male students; in contrast, both men and women reported a similar degree of association between MDD and frequency of HED. Third, although there was no difference in rates of treatment utilization between depressed students with and without HED, we found that students with MDD were more likely to be engaged in mental health treatment, especially women. Last, we also observed that a higher proportion of female students with HED than female students without HED were engaged in treatment. Of interest, the opposite association was evident in male students. To our knowledge, this is the first time the prevalence of treatment engagement among female and male students reporting HED has been reported. Together, these findings have significant theoretical, clinical, and research implications.
The link between depression and alcohol use (both HED and pBAC) is particularly concerning given that HED is associated with severe consequences, and a higher frequency of this behavior increases the risk of problems (Mundt et al., 2009). Although our study found small effects for the associations between MDD and HED, MDD and pBAC, and the gender interaction, when considering that there are 20.6 million college students in the United States (Snyder & Dillow, 2015), even a small increase in frequency of HED or alcohol intoxication has significant public health implications. Indeed, a number of studies have established that even small differences in HED frequency or in pBAC may increase the risk for alcohol-related problems in meaningful ways. Students with frequent heavy drinking (three or more occasions per week) report experiencing more than twice as many alcohol-related problems than nonfrequent heavy drinking students on average over the course of a year (27.7 + 5.9 vs. 11.8 + 12.9, respectively; Presley & Pimentel, 2006) and are five times as likely to experience five or more alcohol-related problems (Wechsler et al., 1994). Female students are 10% more likely to suffer an alcohol-related injury with each additional day consuming five or more drinks, and male students are 19% more likely to suffer an alcohol-related injury with each additional day consuming eight or more drinks (Mundt et al., 2009). Students who consume just two more drinks over what is considered heavy drinking (6/7 women/men) experience an average of more than three additional unique types of consequences in a year relative to those who consume the exact amount considered HED (using 4/5 definition for women/men; Read et al., 2008).
Similarly, higher BAC has been associated with higher risk for alcohol-related problems (Carey & DeMartini, 2010), and an increase of just .01 g/dl of daily blood alcohol level is associated with a 2% increase in the odds of aggressive behavior (Quinn & Fromme, 2011). We conducted follow-up analyses to better interpret our findings among female students and found that during a heavy drinking episode, 22.9% of those with MDD relative to 16.5% of those without MDD had pBAC higher than .08 g/dl (considered the legal limit to drive in many U.S. states) and that 7.5% of those with MDD relative to 4% of those without MDD had a pBAC higher than .13 g/dl (corresponding to significant impairment).
The association of MDD and HED in both men and women contrasts previous research that reported that college students with MDD, especially men, had lower odds of frequent HED (Cranford and al., 2009). This discrepancy could be because Cranford and colleagues (2009) used a binary variable and examined the odds of the presence of frequent HED (HED at least three times in the past 2 weeks), whereas we examined frequency of HED in the past 2 weeks with the possibility of six responses (0, 1 time, 2 times, 3–5 times, 6–9 times, and 10 or more times). This possibility, combined with our previous research indicating that depressive symptoms are associated with daily drinking more in men than in women (Pedrelli et al., 2011), highlights the need for conducting systematic and detailed (not dichotomous yes/no) assessments of heavy alcohol use among students with MDD who may present at health centers or counseling centers. Only a minority of colleges conducts screenings for alcohol misuse (Winters et al., 2011), indicating a need for universities to increase their efforts to identify this risky behavior. Furthermore, on the basis of this study’s findings, counselors may educate students who have MDD about their increased risk for HED and, similarly, inform students with HED about their risk of developing MDD. Future studies may investigate the direction of the association between MDD and HED and evaluate whether stopping HED may reduce MDD.
Regarding mental health treatment engagement, our findings replicate previous research indicating that female students were more likely than male students to be engaged in mental health treatment and that the association between MDD and treatment engagement was stronger in female than male students (Eisenberg et al., 2011a, 2013; Hasin et al., 2005). Perhaps the most compelling finding was that a higher proportion of female students with HED were engaged in treatment than female students without HED, a pattern that was not present in male students. One possible explanation for this pattern of findings is that female students who engage in HED may find alcohol-related incidents more aversive than men, and thus they may be more likely to engage in treatment to prevent these problems from happening. Among students who receive a sanction for an alcohol violation, avoiding another sanction is more important for females than for males, and females are more confident in their ability to do so than their male peers (Carey & DeMartini, 2010). Moreover, women perceive their friends as less approving of an alcohol violation than do men (Carey & DeMartini, 2010).
Degree of aversiveness to an alcohol-related problem also predicts change in alcohol behaviors (Barnett et al., 2006; Qi et al., 2014); women rate alcohol-related problems as more aversive than men (Qi et al., 2014) and following an alcohol-related incident may have higher motivation to change drinking behaviors than men. Conversely, male students with HED may not experience alcohol-related problems as aversive and thus may not be interested in treatment. Unexpectedly, students with MDD and HED did not have higher rates of mental health treatment utilization than students with MDD alone. Our results, together with a previous report that found that students with HED and depressive symptoms sought higher formal and informal help-seeking behaviors than their peers with only depression (Buscemi, 2010), suggest that college students with MDD and HED may engage in more informal help seeking than students with MDD alone but not in more formal treatment.
Given the cross-sectional nature of the presented findings, the temporal relationships between MDD and alcohol use can be interpreted in two ways. On the one hand, among undergraduate students, heavy drinking may lead to MDD. Indeed, alcohol is a depressant, and it has been shown that in some people depression can be induced by heavy alcohol use (Schuckit et al., 2013). Moreover, students who consume more alcohol and engage in more frequent heavy drinking are at higher risk for experiencing alcohol-related consequences (e.g., academic or relationship difficulties) that may lead to MDD. Heavy alcohol use may lead to difficulties with sleep (Chan et al., 2015) that, in turn, may lead to depression (Hershner & Chervin, 2014; Kenney, 2013). The gender effect of MDD on pBAC may be the result of women and men metabolizing alcohol differently, which may contribute to the higher prevalence of depression in women.
On the other hand, it is possible that, consistent with the “self-medication” model (Khantzian, 2003), students with MDD may consume more alcohol and consume it more often to cope with their negative affect. Our finding of high pBAC among students with MDD suggests that students with MDD may consume more alcohol to reach a higher level of intoxication to cope with negative affect. The college years are characterized by numerous difficulties, as young adults attending college find themselves taking on more adult-like responsibilities and tasks without having yet mastered the skills and cognitive maturity of adulthood (Arnett, 2000). In this context, some develop MDD and may drink heavily because they lack alternative, healthy skills to cope with their depressed mood. In support of this hypothesis, it has been consistently shown that drinking to cope is associated with higher alcohol consumption during sad days (Grant et al., 2009). This self-medication model has received support in the context of posttraumatic stress disorder and alcohol use among college students (e.g., Read et al., 2014) and it may also explain HED in undergraduate students with depression. Future studies should seek to discern which of the above scenarios might explain the association we observed in this study.
Limitations
The findings of this study should be considered in the context of some limitations. First, self-report assessments may be associated with biases; however, there is little indication that college students misrepresent alcohol use or other problems as long as confidentiality is clearly explained (Borsari & Muellerleile, 2009). Second, our computation of pBAC may have led to imprecise estimates because there may be individual variation in metabolism and because the response options for number of drinks consumed during a heavy drinking episode included both precise numbers and ranges of numbers. In addition, we used a cutoff score of 10 on the PHQ-9 to indicate MDD, whereas others have used a different algorithm. In our study, approximately 25% of the women and 21% of the men met criteria for MDD. These rates are higher than those found in previous studies that have reported that MDD was present in approximately 10% of students (Blanco et al., 2008; Eisenberg et al., 2013). However, Eisenberg and colleagues (2013) found that 17% of college students had MDD or minor depression (dysthymia or depression not otherwise specified). Moreover, a nationwide survey on college students found that 32% of college students reported having felt “so depressed that it was difficult to function” at least once in the past year (American College Health Association, 2014). It is possible that our cutoff score of PHQ-9 equal to 10 may have included students with MDD as well as with minor depression. We opted to use this cutoff score because it has shown to be more sensitive to MDD diagnoses than other methods (e.g., the PHQ-9 algorithm; Manea et al., 2015). Third, a response rate of approximately 25% of potential students who answered the survey may have introduced biases into the data. In an attempt to address survey nonresponse, we have constructed sample probability weight that would account for demographic differences between responders and nonresponders. However, the probability weight may have not addressed other possible sampling biases. Last, we did not ask which condition students received mental health treatment for, and thus it is not possible to determine whether students were in treatment for heavy alcohol use or for other problems.
Summary
These findings significantly increase our knowledge regarding the intersection of gender, MDD, heavy alcohol use, alcohol intoxication, and engagement in mental health treatment in college students. Specifically, depression and alcohol use differ in male and female college students, indicating the importance of continuing to consider gender when constructing and interpreting models of alcohol consumption. Of particular concern, only 29.5% of students with both MDD and HED received mental health treatment in the previous year, suggesting that there may be a large proportion of students at high risk who are not receiving formal help. Such low rates of engagement in mental health treatment highlight the need to increase screening and outreach efforts in college students.
Footnotes
This study was supported by National Institute on Alcohol Abuse and Alcoholism Grants K23AA020064 (to Paola Pedrelli) and R01AA017427 (to Brian Borsari), and VISN1 Career Development Award V1CDA2012-18 (to Brian Borsari). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism, the National Institutes of Health, the Department of Veterans Affairs, or the United States Government.
References
- American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. Hanover, MD: Author; 2014. [Google Scholar]
- Arnett J. J. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. doi:10.1037/0003-066X.55.5.469. [PubMed] [Google Scholar]
- Barnett N. P., Goldstein A. L., Murphy J. G., Colby S. M., Monti P. M. “I’ll never drink like that again”: Characteristics of alcohol-related incidents and predictors of motivation to change in college students. Journal of Studies on Alcohol. 2006;67:754–763. doi: 10.15288/jsa.2006.67.754. doi:10.15288/ jsa.2006.67.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrios L. C., Everett S. A., Simon T. R., Brener N. D. Suicide ideation among US college students. Associations with other injury risk behaviors. Journal of American College Health. 2000;48:229–233. doi: 10.1080/07448480009599309. doi:10.1080/07448480009599309. [DOI] [PubMed] [Google Scholar]
- Blanco C., Okuda M., Wright C., Hasin D. S., Grant B. F., Liu S. M., Olfson M. Mental health of college students and their noncollege-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65:1429–1437. doi: 10.1001/archpsyc.65.12.1429. doi:10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Hustad J. T. P., Mastroleo N. R., Tevyaw T. O. L., Barnett N. P., Kahler C. W., … Monti P. M. Addressing alcohol use and problems in mandated college students: a randomized clinical trial using stepped care. Journal of Consulting and Clinical Psychology. 2012;80:1062–1074. doi: 10.1037/a0029902. doi:10.1037/a0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Muellerleile P. Collateral reports in the college setting: A meta-analytic integration. Alcoholism: Clinical and Experimental Research. 2009;33:826–838. doi: 10.1111/j.1530-0277.2009.00902.x. doi:10.1111/j.1530-0277.2009.00902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B., Neal D. J., Collins S. E., Carey K. B. Differential utility of three indexes of risky drinking for predicting alcohol problems in college students. Psychology of Addictive Behaviors. 2001;15:321–324. doi: 10.1037//0893-164x.15.4.321. doi:10.1037/0893-164X.15.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscemi J., Murphy J. G., Martens M. P., McDevitt-Murphy M. E., Dennhardt A. A., Skidmore J. R. Help-seeking for alcohol-related problems in college students: Correlates and preferred resources. Psychology of Addictive Behaviors. 2010;24:571–580. doi: 10.1037/a0021122. doi:10.1037/a0021122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camatta C. D., Nagoshi C. T. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcoholism: Clinical and Experimental Research. 1995;19:142–146. doi: 10.1111/j.1530-0277.1995.tb01482.x. doi:10.1111/j.1530-0277.1995.tb01482.x. [DOI] [PubMed] [Google Scholar]
- Carey K. B., DeMartini K. S. The motivational context for mandated alcohol interventions for college students by gender and family history. Addictive Behaviors. 2010;35:218–223. doi: 10.1016/j.addbeh.2009.10.011. doi:10.1016/j. addbeh.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J. K., Trinder J., Colrain I. M., Nicholas C. L. The acute effects of alcohol on sleep electroencephalogram power spectra in late adolescence. Alcoholism: Clinical and Experimental Research. 2015;39:291–299. doi: 10.1111/acer.12621. doi:10.1111/acer.12621. [DOI] [PubMed] [Google Scholar]
- Cranford J. A., Eisenberg D., Serras A. M. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors. 2009;34:134–145. doi: 10.1016/j.addbeh.2008.09.004. doi:10.1016/j.addbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Dawson D. A., Grant B. F., Stinson F. S., Chou P. S. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug and Alcohol Dependence. 2005;77:139–150. doi: 10.1016/j.drugalcdep.2004.07.012. doi:10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Dennhardt A. A., Murphy J. G. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25:595–604. doi: 10.1037/a0025807. doi:10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Diez-Quevedo C., Rangil T., Sanchez-Planell L., Kroenke K., Spitzer R. L. Validation and utility of the Patient Health Questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic Medicine. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. doi:10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- Dvorak R. D., Lamis D. A., Malone P. S. Alcohol use, depressive symptoms, and impulsivity as risk factors for suicide proneness among college students. Journal of Affective Disorders. 2013;149:326–334. doi: 10.1016/j.jad.2013.01.046. doi:10.1016/j.jad.2013.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D., Gollust S. E., Golberstein E., Hefner J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77:534–542. doi: 10.1037/0002-9432.77.4.534. doi:10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- Eisenberg D., Hunt J., Speer N. Mental health in American colleges and universities: Variation across student subgroups and across campuses. Journal of Nervous and Mental Disease. 2013;201:60–67. doi: 10.1097/NMD.0b013e31827ab077. doi:10.1097/NMD.0b013e31827ab077. [DOI] [PubMed] [Google Scholar]
- Eisenberg D., Hunt J., Speer N., Zivin K. Mental health service utilization among college students in the United States. Journal of Nervous and Mental Disease. 2011a;199:301–308. doi: 10.1097/NMD.0b013e3182175123. doi:10.1097/ NMD.0b013e3182175123. [DOI] [PubMed] [Google Scholar]
- Eisenberg D., Nicklett E. J., Roeder K., Kirz N. E. Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. Journal of American College Health. 2011b;59:700–707. doi: 10.1080/07448481.2010.546461. doi:10.1080/07448481.2010.546461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez V., Reynolds B., Skewes M. Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacology. 2011;19:303–313. doi: 10.1037/a0022720. [DOI] [PubMed] [Google Scholar]
- Geisner I. M., Larimer M. E., Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. doi:10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Graham K., Massak A., Demers A., Rehm J. Does the association between alcohol consumption and depression depend on how they are measured? Alcoholism: Clinical and Experimental Research. 2007;31:78–88. doi: 10.1111/j.1530-0277.2006.00274.x. doi:10.1111/j.1530-0277.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Hasin D. S., Chou S. P., Stinson F. S., Dawson D. A. Nicotine dependence and psychiatric disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. doi:10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grant V. V., Stewart S. H., Mohr C. D. Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychology of Addictive Behaviors. 2009;23:226–237. doi: 10.1037/a0015006. doi:10.1037/ a0015006. [DOI] [PubMed] [Google Scholar]
- Harford T. C., Yi H.-Y., Hilton M. E. Alcohol abuse and dependence in college and noncollege samples: A ten-year prospective followup in a national survey. Journal of Studies on Alcohol. 2006;67:803–809. doi: 10.15288/jsa.2006.67.803. doi:10.15288/jsa.2006.67.803. [DOI] [PubMed] [Google Scholar]
- Harrell Z. A., Karim N. M. Is gender relevant only for problem alcohol behaviors? An examination of correlates of alcohol use among college students. Addictive Behaviors. 2008;33:359–365. doi: 10.1016/j.addbeh.2007.09.014. doi:10.1016/j. addbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Goodwin R. D., Stinson F. S., Grant B. F. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. doi:10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hershner S. D., Chervin R. D. Causes and consequences of sleepiness among college students. Nature and Science of Sleep. 2014;6:73–84. doi: 10.2147/NSS.S62907. doi:10.2147/NSS.S62907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R., Heeren T., Winter M., Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. doi:10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hingson R. W., Zha W., Weitzman E. R. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs, Supplement. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. doi:10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong A. M., Jones D. J., Stein G. L., Baucom D. H., Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. doi:10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney S. R., Lac A., LaBrie J. W., Hummer J. F., Pham A. Mental health, sleep quality, drinking motives, and alcohol-related consequences: A path-analytic model. Journal of Studies on Alcohol and Drugs. 2013;74:841–851. doi: 10.15288/jsad.2013.74.841. doi:10.15288/jsad.2013.74.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Chiu W. T., Demler O., Heeringa S., Hiripi E., Zheng H. The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. doi:10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian E. J. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10:47–54. [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. doi:10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamis D. A., Malone P. S., Langhinrichsen-Rohling J., Ellis T. E. Body investment, depression, and alcohol use as risk factors for suicide proneness in college students. Crisis. 2010;31:118–127. doi: 10.1027/0227-5910/a000012. doi:10.1027/0227-5910/a000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Herzog W., Grafe K. Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9) Journal of Affective Disorders. 2004;81:61–66. doi: 10.1016/S0165-0327(03)00198-8. doi:10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Canadian Medical Association Journal. 2012;184:E191–E196. doi: 10.1503/cmaj.110829. doi:10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. General Hospital Psychiatry. 2015;37:67–75. doi: 10.1016/j.genhosppsych.2014.09.009. doi:10.1016/j.genhosppsych.2014.09.009. [DOI] [PubMed] [Google Scholar]
- Matthews D. B., Miller W. R. Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Addictive Behaviors. 1979;4:55–60. doi: 10.1016/0306-4603(79)90021-2. doi:10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- Mundt M. P., Zakletskaia L. I., Fleming M. F. Extreme college drinking and alcohol-related injury risk. Alcoholism: Clinical and Experimental Research. 2009;33:1532–1538. doi: 10.1111/j.1530-0277.2009.00981.x. doi:10.1111/j.1530-0277.2009.00981.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3. http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf Retrieved from. [Google Scholar]
- O’Donnell K., Wardle J., Dantzer C., Steptoe A. Alcohol consumption and symptoms of depression in young adults from 20 countries. Journal of Studies on Alcohol. 2006;67:837–840. doi: 10.15288/jsa.2006.67.837. doi:10.15288/ jsa.2006.67.837. [DOI] [PubMed] [Google Scholar]
- Pedrelli P., Farabaugh A. H., Zisook S., Tucker D., Rooney K., Katz J., Fava M. Gender, depressive symptoms and patterns of alcohol use among college students. Psychopathology. 2011;44:27–33. doi: 10.1159/000315358. doi:10.1159/000315358. [DOI] [PubMed] [Google Scholar]
- Presley C. A., Pimentel E. R. The introduction of the heavy and frequent drinker: A proposed classification to increase accuracy of alcohol assessments in postsecondary educational settings. Journal of Studies on Alcohol. 2006;67:324–331. doi: 10.15288/jsa.2006.67.324. doi:10.15288/jsa.2006.67.324. [DOI] [PubMed] [Google Scholar]
- Qi D., Pearson M. R., Hustad J. T. Predictors of motivation to change in mandated college students following a referral incident. Psychology of Addictive Behaviors. 2014;28:524–531. doi: 10.1037/a0035910. doi:10.1037/a0035910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn P. D., Fromme K. Predictors and outcomes of variability in subjective alcohol intoxication among college students: An event-level analysis across 4 years. Alcoholism: Clinical and Experimental Research. 2011;35:484–95. doi: 10.1111/j.1530-0277.2010.01365.x. doi:10.1111/j.1530-0277.2010.01365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J. P., Beattie M., Chamberlain R., Merrill J. E. Beyond the “Binge” threshold: Heavy drinking patterns and their association with alcohol involvement indices in college students. Addictive Behaviors. 2008;33:225–234. doi: 10.1016/j.addbeh.2007.09.001. doi:10.1016/j.addbeh.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Read J. P., Griffin M. J., Wardell J. D., Ouimette P. Coping, PTSD symptoms, and alcohol involvement in trauma-exposed college students in the first three years of college. Psychology of Addictive Behaviors. 2014;28:1052–1064. doi: 10.1037/a0038348. doi:10.1037/a0038348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit M. A., Smith T. L., Kalmijn J. Relationships among independent major depressions, alcohol use, and other substance use and related problems over 30 years in 397 families. Journal of Studies on Alcohol and Drugs. 2013;74:271–279. doi: 10.15288/jsad.2013.74.271. doi:10.15288/jsad.2013.74.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder T. D., Dillow S. A. Digest of Education Statistics 2013 (NCES 2015-011). Chapter 3: “Postsecondary education” (pp. 377–674) Washington, DC: National Center for Education Statistics; 2015. Retrieved from http://nces.ed.gov/pubs2015/2015011.pdf. [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B. W. the Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. doi:10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07–4293) Rockville, MD: Author; 2007. [Google Scholar]
- Thomasson H. R. Gender differences in alcohol metabolism. Physiological responses to ethanol. Recent Developments in Alcoholism. 1995;12:163–179. doi: 10.1007/0-306-47138-8_9. [DOI] [PubMed] [Google Scholar]
- Valentiner D. P., Mounts N. S., Deacon B. J. Panic attacks, depression and anxiety symptoms, and substance use behaviors during late adolescence. Journal of Anxiety Disorders. 2004;18:573–585. doi: 10.1016/j.janxdis.2003.04.001. doi:10.1016/j. janxdis.2003.04.001. [DOI] [PubMed] [Google Scholar]
- Vickers K. S., Patten C. A., Bronars C., Lane K., Stevens S. R., Croghan I. T., Clark M. M. Binge drinking in female college students: The association of physical activity, weight concern, and depressive symptoms. Journal of American College Health. 2004;53:133–140. doi: 10.3200/JACH.53.3.133-140. doi:10.3200/JACH.53.3.133-140. [DOI] [PubMed] [Google Scholar]
- Wechsler H., Davenport A., Dowdall G., Moeykens B., Castillo S. Health and behavioral consequences of binge drinking in college. A national survey of students at 140 campuses. JAMA. 1994;272:1672–1677. doi:10.1001/jama.1994.03520210056032. [PubMed] [Google Scholar]
- Wechsler H., Nelson T. F. Binge drinking and the American college student: What’s five drinks? Psychology of Addictive Behaviors. 2001;15:287–291. doi: 10.1037//0893-164x.15.4.287. doi:10.1037/0893-164X.15.4.287. [DOI] [PubMed] [Google Scholar]
- Wechsler H., Nelson T. F. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69:481–490. doi: 10.15288/jsad.2008.69.481. doi:10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Weitzman E. R. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. doi:10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- White A. M., Kraus C. L., Swartzwelder H. Many college freshmen drink at levels far beyond the binge threshold. Alcoholism: Clinical and Experimental Research. 2006;30:1006–1010. doi: 10.1111/j.1530-0277.2006.00122.x. doi:10.1111/j.1530-0277.2006.00122.x. [DOI] [PubMed] [Google Scholar]
- Winters K. C., Toomey T., Nelson T. F., Erickson D., Lenk K., Miazga M. Screening for alcohol problems among 4-year colleges and universities. Journal of American College Health. 2011;59:350–357. doi: 10.1080/07448481.2010.509380. doi:10. 1080/07448481.2010.509380. [DOI] [PMC free article] [PubMed] [Google Scholar]