Abstract
Objective:
In college student samples, the association between depressive symptoms and alcohol-related problems has been found to be mediated by drinking-to-cope motives. Mindfulness-based interventions suggest that mindfulness may attenuate the conditioned response of using substances in response to negative emotional states, and trait mindfulness has been shown to be a protective factor associated with experiencing fewer alcohol-related problems. In the present study, we examined trait mindfulness as a moderator of the indirect associations of depressive symptoms on alcohol-related problems via drinking-to-cope motives.
Method:
Participants were undergraduate students at a large, southeastern university in the United States who drank at least once in the previous month (n = 448). Participants completed an online survey regarding their personal mental health, coping strategies, trait mindfulness, and alcohol use behaviors. The majority of participants were female (n = 302; 67.4%), identified as being either White nonHispanic (n = 213; 47.5%) or African American (n = 119; 26.6%), and reported a mean age of 22.74 (SD = 6.81) years. Further, 110 (25%) participants reported having a previous and/or current experience with mindfulness mediation.
Results:
As hypothesized, the indirect effects from depressive symptoms to alcohol-related problems via drinking-to-cope motives were weaker among individuals reporting higher levels of mindfulness than among individuals reporting lower and average levels of mindfulness.
Conclusions:
The present study suggests a possible mechanism through which mindfulness-based interventions may be efficacious among college students: decoupling the associations between depressive symptoms and drinking-to-cope motives.
Alcohol-related consequences are highly prevalent among college students and range from academic consequences to injuries and death (Hingson et al., 2002, 2009; National Institute on Alcohol Abuse and Alcoholism, 2015; Wechsler et al., 2002). In addition to alcohol misuse, researchers have also found high rates of psychological distress, particularly depression, among college students (Bayram & Bilgel, 2008; Eisenberg et al., 2007). Not surprisingly, college students who experience poor mental health and depression are more likely than their counterparts to report more hazardous drinking-related out-comes and alcohol abuse (Armeli et al., 2010; Dennhardt & Murphy, 2011; Gonzalez et al., 2009; Weitzman, 2004). Not only have drinking-to-cope motives been shown to be a proximal risk factor for alcohol-related problems among college students (Bravo et al., 2016; Kuntsche et al., 2005), but they have also been shown to be one mechanism through which depressive symptoms are associated with alcohol-related problems (Bravo et al., in press; Gonzalez et al., 2011; Kenney et al., 2015). Although the relationship between depression and alcohol-related problems via drinking-to-cope motives has been established, there have yet to be any attempts to identify what factors might moderate this mediated relationship. Finding protective factors that may reduce these associations can have important implications for interventions.
Mindfulness as a protective factor
Several converging lines of research suggest that mindfulness can buffer the effects of risk factors associated with increased substance use. From a clinical trial testing Mindfulness-Based Relapse Prevention (MBRP; Bowen et al., 2009) for reducing substance use, Witkiewitz and Bowen (2010) found that the participants who received MBRP (compared with control) demonstrated an attenuated association between posttreatment depressive symptoms and self-reported alcohol and other drug craving 2 months following treatment, which predicted decreased substance use 4 months posttreatment. Importantly, MBRP did not change overall levels of depressive symptoms; rather, it appeared to change the conditioned response of craving and substance use in response to depressive symptoms. Brief mindfulness training has been shown to reduce the positive associations between implicit alcohol motivation and heavy drinking (Ostafin et al., 2012). Elwafi et al. (2013) showed that mindfulness training significantly reduced the association between self-reported craving for cigarettes and smoking. These at tenuated associations suggest that mindfulness training can reduce the degree to which a highly conditioned pathway from negative states (i.e., depressive symptoms, craving) to substance use is initiated automatically.
Even outside the context of mindfulness-based treatment or practices, trait mindfulness is an individual difference variable shown to relate to a wide variety of health-related outcomes, including fewer alcohol-related problems (Fernandez et al., 2010; Murphy & MacKillop, 2012; Pearson et al., 2015; Roos et al., 2015). Given the studies reviewed above, we examined whether naturally occurring levels of trait mindfulness may buffer the associations between depressive symptoms, drinking-to-cope motives, and alcohol-related problems. Higher trait mindfulness may be associated with a reduced conditioned response of drinking to cope in the context of experiencing depressive symptoms.
Purpose
The purpose of the present study is to extend research on the associations between depressive symptoms, drinking to cope, and alcohol-related problems. Specifically, we confirm drinking-to-cope motives as a mediator of the association between depressive symptoms and alcohol-related problems, and we examine trait mindfulness as a moderator of this indirect association. Thus, we tested a moderated mediation model in which we expected that the indirect association between depressive symptoms and alcohol-related problems via drinking-to-cope motives would be attenuated among individuals with high trait mindfulness.
Method
Participants and procedure
Participants were undergraduate students recruited from a psychology department participant pool at a large, southeastern university in the United States. Participants completed an online survey regarding their personal mental health, coping strategies, trait mindfulness, and alcohol use behaviors. For this study, only data from students who consumed alcohol at least one day in the previous month (n = 448) were included in the final analysis from a larger sample (N = 699). Among college student drinkers, the majority of participants identified themselves as being either White non-Hispanic (n = 213, 47.54%) or African American (n = 119, 26.56%), were female (n = 302, 67.41%), and reported a mean age of 22.74 (SD = 6.81) years. Further, among the analytic sample, 110 (25%) participants reported having a “previous and/or current experience with mindfulness mediation.” The study was approved by the institutional review board at the participating institution.
Measures
Mindfulness.
Trait mindfulness was assessed using the 39-item Five Facet Mindfulness Questionnaire (Baer et al., 2006) measured on a 5-point response scale to assess five domains of mindfulness: acting with awareness, nonjudging of inner experience, nonreactivity to inner experience, describing, and observing. However, in line with other studies (Desrosiers et al., 2013; Pepping et al., 2013), we averaged all items to assess an overall measure of trait mindfulness (M = 3.27, SD = 0.47, range: 1.95–4.75; α = .88).
Depressive symptoms.
Depressive symptoms were assessed using the 20-item Center for Epidemiological Studies Depression Scale–Revised (Eaton et al., 2004) measured on a 5-point response scale (0 = not at all or less than 1 day, 1 = 1–2 days, 2 = 3–4 days, 3 = 5–7 days, 4 = nearly every day for 2 weeks). As advised by Van Dam and Earleywine (2011), the “5–7 days” and “nearly every day…” were collapsed into the same value and all items were averaged (M = 0.71, SD = 0.67, range: 0–3; α = .95).
Drinking-to-cope motives.
Drinking-to-cope motives were assessed using the nine-item coping-depression motives subscale from the Modified Drinking Motives Questionnaire–Revised (Grant et al., 2007) measured on a 5-point response scale. These items were averaged (M = 1.80, SD = 1.06, range: 1–5; α = .96).
Alcohol-related problems.
Alcohol-related problems were assessed using a checklist form of the 24-item Brief-Young Adult Alcohol Consequences Questionnaire (Kahler et al., 2005). Items were summed to reflect the number of unique alcohol-related problems experienced in the past 30 days (M = 5.15, SD = 5.24, range: 0–23; α = .91).
Alcohol consumption.
Alcohol consumption was assessed with a modified version of the Daily Drinking Questionnaire (Collins et al., 1985). We summed number of standard drinks consumed on each day of the typical drinking week (M = 7.13, SD = 8.51).
Statistical analysis
After data cleaning and addressing statistical assumptions, predictors were standardized before calculating the interaction term to provide more interpretable findings for researchers (i.e., standard deviation increase compared with one-unit increases). We used Mplus 7.11 (Muthén & Muthén, 1998–2012) to examine the total, direct, and indirect effects of each predictor variable on alcohol-related problems using bias-corrected bootstrapped estimates (Efron & Tibshirani, 1993) based on 10,000 bootstrapped samples. This provides a powerful test of mediation and moderated mediation (Fritz & MacKinnon, 2007; Preacher et al., 2007) and is robust to small departures from normality (Erceg-Hurn & Mirosevich, 2008). Parameters were estimated using maximum likelihood estimation, and missing data were handled using full information maximum likelihood, which is more efficient and has less bias than alternative procedures (Enders, 2001; Enders & Bandalos, 2001). To control for gender, we entered gender as a predictor of all other variables using unweighted effects coding (-.5 = male, .5 = female) so that parameters are interpreted at the unweighted average of men and women. We controlled for alcohol use (standardized) to focus on the associations between predictors and alcohol-related problems beyond differences in overall consumption levels.
Results
Descriptive statistics and bivariate correlations
Depressive symptoms had a moderate negative correlation with mindfulness (r = -.39), a strong positive correlation with drinking-to-cope motives (r = .51), and a weak positive correlation with alcohol-related problems (r = .28). Mindfulness had a moderate negative relationship with drinking-to-cope motives (r = -.35) and a weak negative relationship with alcohol-related problems (r = -.24). Drinking-to-cope motives had a moderate positive relationship with alcohol-related problems (r = .40) and a weak positive correlation with alcohol use (r = .21). Alcohol use had a moderate positive relationship with alcohol-related problems (r = .40). With regard to gender, alcohol use had a weak negative relationship with gender (r = -.23), indicating that men reported more drinks consumed in a typical week. A supplementary table of all correlations is available from the authors on request.
Replication of the mediation model
For the mediation model, depressive symptoms were modeled as the most distal predictor of alcohol-related problems with drinking-to-cope motives (i.e., the mediator) as the more proximal predictor. When we controlled for gender and alcohol consumption, depressive symptoms were significantly associated with higher levels of drinking-to-cope motives for depression (β = .49, 95% CI [.39, .59]) and were uniquely associated with increased alcohol-related problems (β = .12, 95% CI [.01, .22]). Further, drinking-to-cope motives were also significantly associated with higher levels of alcohol-related problems (β = .28, 95% CI [.16, .39]). As could be expected by these direct effects, drinking-to-cope motives mediated the associations between depressive symptoms and alcohol-related problems (indirect β = .14, 95% CI [.07, .20]), accounting for 53.31% of the total effect of depressive symptoms on alcohol-related problems.
Moderated mediation model
Subsequently, we tested for moderated-mediation using a bootstrapping procedure following Preacher et al.’s (2007) Model 2, in which moderation of the path between the predictor and the mediator was evaluated. In other words, we wanted to examine whether the association between depressive symptoms and drinking-to-cope motives is moderated by mindfulness within the mediational path model. We further examined the conditional indirect effect of depressive symptoms to alcohol-related problems via drinking-to-cope motives at various levels of mindfulness. Specifically, we examined these conditional indirect effects at low levels of mindfulness (i.e., 1 SD below the mean), average levels of mindfulness, and high levels of mindfulness (i.e., 1 SD above the mean).
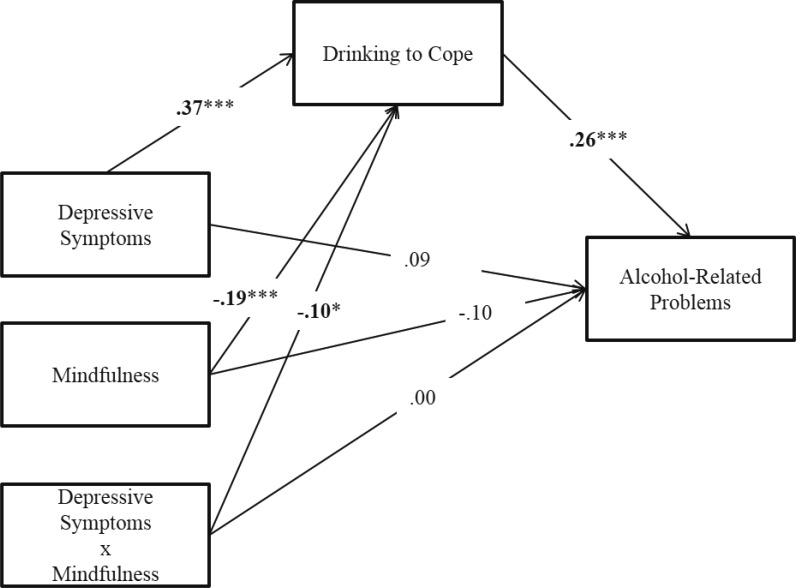
The findings showed that the association between depressive symptoms and drinking-to-cope motives was moderated by mindfulness (β = -.10, 95% CI [-.18, -.01]; Figure 1). Specifically, the indirect effect coefficient for high mindfulness (β = .07) was significantly weaker than the indirect coefficient for average mindfulness (β = .10) (β = -.03, 95% CI [-.06, -.00]), and low mindfulness (β = .12) (β = -.05, 95% CI [-.11, -.01]). The indirect effect coefficient for average mindfulness (β = .10) was significantly weaker than the indirect coefficient for low mindfulness (β = .12) (β = -.03, 95% CI [-.06, -.00]). However, the indirect effects from depressive symptoms to alcohol-related problems via drinking-to-cope motives were still significant at all levels of mindfulness. These findings indicate a statistically significant moderated mediation effect, such that the indirect effects from depressive symptoms to alcohol-related problems via drinking-to-cope motives were weaker among individuals reporting higher levels of mindfulness than among individuals reporting lower levels of mindfulness and average levels of mindfulness.
Figure 1.
Depicts standardized relationships in the moderated-mediation model (n = 448). Gender did not significantly predict to drinking to cope (β = -.08) and alcohol-related problems (β = .07). Alcohol use did significantly predict to drinking to cope (β = .15) and alcohol-related problems (β = .35). These paths are not shown in the figure for reasons of parsimony. *p < .05; ***p < .001.
Discussion
The present study tested a moderated mediation model to examine whether trait mindfulness moderated the associations between depressive symptoms and drinking-to-cope motives, in turn resulting in lower alcohol-related problems. Based on the results of mindfulness-based interventions for substance use (Elwafi et al., 2013; Witkiewitz & Bowen, 2010), we expected that individuals higher in trait mindfulness would demonstrate an attenuated association between depressive symptoms and drinking-to-cope motives. Our results supported our predictions in that the indirect (i.e., mediated) effect of depressive symptoms on alcohol-related problems via drinking-to-cope motives was weakest among individuals with high trait mindfulness and strongest among individuals with low trait mindfulness.
In a sample of college student drinkers (i.e., mostly nondependent drinkers), we were able to demonstrate that naturally occurring variability of mindfulness was related to the strength of associations between the experience of depressive symptoms and reporting the use of alcohol to cope with depressive symptoms. Converging evidence from mindfulness-based intervention studies (Elwafi et al., 2013; Witkiewitz & Bowen, 2010) and the present study suggests that mindfulness is a protective factor that can decouple the conditioned associations between negative emotional states and substance use.
Future directions
Although mindfulness has been generally defined as a state of being aware and nonjudging to present moment experiences, a majority of studies and measurement tools examine mindfulness retrospectively and as a trait (Chiesa, 2013; Sauer et al., 2013; Tanay & Bernstein, 2013). One way to understand the health-promoting effects of mindfulness is to examine psychological and health outcomes after a brief mindfulness induction (i.e., inducing state mindfulness). Thus, to further validate the protective mechanisms of mindfulness on alcohol outcomes, future studies should explore whether being induced into a mindful state decouples the associations between negative mood states and alcohol outcomes even among individuals with higher drinking-to-cope motives. Further, as distinct facets of mindfulness have been shown to be differentially related to alcohol-related outcomes (Brown et al., 2015; Pearson et al., 2015; Reynolds et al., 2015; Roos et al., 2015), future studies should examine whether distinct facets of mindfulness uniquely moderate the mediational relationship between depressive symptoms and alcohol-related problems via drinking-to-cope motives.
Limitations
Our findings ought to be interpreted with caution given the present study’s limitations. Our cross-sectional survey design prohibited the demonstration of temporal precedence, which is required for making causal inferences. However, our results based on naturally occurring levels of trait mindfulness support the findings from mindfulness-based interventions, providing evidence that the findings from these intervention studies generalize to other populations (i.e., college student drinkers). Further, our reliance on retrospective self-report measures, which is associated with significant recall biases (e.g., with alcohol use, Ekholm, 2004; Gmel & Daeppen, 2007), and use of a convenience sample limits the generalizability of our findings. These limitations can be overcome by the use of ecological momentary assessment (Shiffman, 2009), which has been used to confirm the indirect associations between affect and alcohol-related outcomes via drinking motives (Dvorak et al., 2014).
Conclusions
The present study confirmed our hypotheses that individuals with higher levels of trait mindfulness would demonstrate weaker indirect associations between depressive symptoms and alcohol-related problems via drinking-to-cope motives. Although additional research using experimental and ecological momentary assessment designs is needed to more fully disentangle the associations among these constructs, our results may have important implications for preventative interventions for college student drinkers. A recent study showed that a brief mindfulness-based intervention reduced heavy episodic (“binge”) drinking and alcohol-related problems among college students (Mermelstein & Garske, 2015). The present study suggests a possible mechanism through which mindfulness-based interventions may be efficacious among college students: decoupling the associations between depressive symptoms and alcohol coping motives. Additional work is needed to test whether decoupling the associations between negative emotional states and motivations for drinking to cope may be a broader mechanism through which mindfulness-based interventions can reduce alcohol use.
Footnotes
Matthew R. Pearson is supported by a career development grant K01-AA023233 from the National Institute on Alcohol Abuse and Alcoholism.
References
- Armeli S., Conner T. S., Cullum J., Tennen H. A longitudinal analysis of drinking motives moderating the negative affect-drinking association among college students. Psychology of Addictive Behaviors. 2010;24:38–47. doi: 10.1037/a0017530. doi:10.1037/a0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer R. A., Smith G. T., Hopkins J., Krietemeyer J., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. doi:10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bayram N., Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Social Psychiatry and Psychiatric Epidemiology. 2008;43:667–672. doi: 10.1007/s00127-008-0345-x. doi:10.1007/s00127-008-0345-x. [DOI] [PubMed] [Google Scholar]
- Bowen S., Chawla N., Collins S. E., Witkiewitz K., Hsu S., Grow J., Marlatt A. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. doi:10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo A. J., Henson J. M., Pearson M. R. Understanding the role of alcohol as a coping mechanism among college students: A review of drinking to cope motives. 2016. Manuscript submitted for publication. [Google Scholar]
- Bravo A. J., Pearson M. R., Henson J. M. Drinking to cope with depressive symptoms and ruminative thinking: A multiple mediation model among college students. in press. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown D. B., Bravo A. J., Roos C. R., Pearson M. R. Five facets of mindfulness and psychological health: Evaluating a psychological model of the mechanisms of mindfulness. Mindfulness. 2015;6:1021–1032. doi: 10.1007/s12671-014-0349-4. doi:10.1007/s12671-014-0349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A. The difficulty of defining mindfulness: Current thought and critical issues. Mindfulness. 2013;4:255–268. doi:10.1007/s12671-012-0123-4. [Google Scholar]
- Collins R. L., Parks G. A., Marlatt G. A. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. doi:10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Dennhardt A. A., Murphy J. G. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25:595–604. doi: 10.1037/a0025807. doi:10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Desrosiers A., Klemanski D. H., Nolen-Hoeksema S. Mapping mindfulness facets onto dimensions of anxiety and depression. Behavior Therapy. 2013;44:373–384. doi: 10.1016/j.beth.2013.02.001. doi:10.1016/j.beth.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak R. D., Pearson M. R., Day A. M. Ecological momentary assessment of acute alcohol use disorder symptoms: Associations with mood, motives, and use on planned drinking days. Experimental and Clinical Psychopharmacology. 2014;22:285–297. doi: 10.1037/a0037157. doi:10.1037/a0037157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton W. W., Muntaner C., Smith C., Tien A., Ybarra M. Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R) In: Maruish M. E., editor. The use of psychological testing for treatment planning and outcomes assessment. 3rd ed. Mahwah, NJ: Lawrence Erlbaum; 2004. pp. 363–377. [Google Scholar]
- Efron B., Tibshirani R. J. An introduction to the bootstrap. Boca Raton, FL: CRC Press; 1993. [Google Scholar]
- Eisenberg D., Gollust S. E., Golberstein E., Hefner J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. American Journal of Orthopsychiatry. 2007;77:534–542. doi: 10.1037/0002-9432.77.4.534. doi:10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- Ekholm O. Influence of the recall period on self-reported alcohol intake. European Journal of Clinical Nutrition. 2004;58:60–63. doi: 10.1038/sj.ejcn.1601746. doi:10.1038/sj.ejcn.1601746. [DOI] [PubMed] [Google Scholar]
- Elwafi H. M., Witkiewitz K., Mallik S., Thornhill T. A., IV, Brewer J. A. Mindfulness training for smoking cessation: Moderation of the relationship between craving and cigarette use. Drug and Alcohol Dependence. 2013;130:222–229. doi: 10.1016/j.drugalcdep.2012.11.015. doi:10.1016/j.drugalcdep.2012.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C. K. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychological Methods. 2001;6:352–370. doi:10.1037/1082-989X.6.4.352. [PubMed] [Google Scholar]
- Enders C. K., Bandalos D. L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2001;8:430–457. doi:10.1207/S15328007SEM0803_5. [Google Scholar]
- Erceg-Hurn D. M., Mirosevich V. M. Modern robust statistical methods: An easy way to maximize the accuracy and power of your research. American Psychologist. 2008;63:591–601. doi: 10.1037/0003-066X.63.7.591. doi:10.1037/0003-066X.63.7.591. [DOI] [PubMed] [Google Scholar]
- Fernandez A. C., Wood M. D., Stein L. A. R., Rossi J. S. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24:608–616. doi: 10.1037/a0021742. doi:10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz M. S., Mackinnon D. P. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. doi:10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gmel G., Daeppen J.-B. Recall bias for seven-day recall measurement of alcohol consumption among emergency department patients: Implications for case-crossover designs. Journal of Studies on Alcohol and Drugs. 2007;68:303–310. doi: 10.15288/jsad.2007.68.303. doi:10.15288/jsad.2007.68.303. [DOI] [PubMed] [Google Scholar]
- Gonzalez V. M., Reynolds B., Skewes M. C. Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacology. 2011;19:303–313. doi: 10.1037/a0022720. doi:10.1037/a0022720. [DOI] [PubMed] [Google Scholar]
- Gonzalez V. M., Bradizza C. M., Collins R. L. Drinking to cope as a statistical mediator in the relationship between suicidal ideation and alcohol outcomes among underage college drinkers. Psychology of Addictive Behaviors. 2009;23:443–451. doi: 10.1037/a0015543. doi:10.1037/a0015543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant V. V., Stewart S. H., O’Connor R. M., Blackwell E., Conrod P. J. Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire—Revised in undergraduates. Addictive Behaviors. 2007;32:2611–2632. doi: 10.1016/j.addbeh.2007.07.004. doi:10.1016/j.addbeh.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Hingson R. W., Heeren T., Zakocs R. C., Kopstein A., Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24. Journal of Studies on Alcohol. 2002;63:136–144. doi: 10.15288/jsa.2002.63.136. doi:10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Hingson R. W., Zha W., Weitzman E. R. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs, Supplement. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. doi:10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler C. W., Strong D. R., Read J. P. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29:1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. doi:10.1097/01.ALC.0000171940.95813.A5. [DOI] [PubMed] [Google Scholar]
- Kenney S., Jones R. N., Barnett N. P. Gender differences in the effect of depressive symptoms on prospective alcohol expectancies, coping motives, and alcohol outcomes in the first year of college. Journal of Youth and Adolescence. 2015;44:1884–1897. doi: 10.1007/s10964-015-0311-3. doi:10.1007/s10964-015-0311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E., Knibbe R., Gmel G., Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. doi:10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Mermelstein L. C., Garske J. P. A brief mindfulness intervention for college student binge drinkers: A pilot study. Psychology of Addictive Behaviors. 2015;29:259–269. doi: 10.1037/adb0000040. doi:10.1037/adb0000040. [DOI] [PubMed] [Google Scholar]
- Murphy C., MacKillop J. Living in the here and now: Interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology. 2012;219:527–536. doi: 10.1007/s00213-011-2573-0. doi:10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. Mplus user's guide. 7th ed. Los Angeles, CA: Authors; 1998–2012. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. College drinking. 2015. Retrieved from http://pubs.niaaa.nih.gov/publications/CollegeFact-Sheet/CollegeFactSheet.pdf. [Google Scholar]
- Ostafin B. D., Bauer C., Myxter P. Mindfulness decouples the relation between automatic alcohol motivation and heavy drinking. Journal of Social and Clinical Psychology. 2012;31:729–745. doi:10.1521/jscp.2012.31.7.729. [Google Scholar]
- Pearson M. R., Brown D. B., Bravo A. J., Witkiewitz K. Staying in the moment and finding purpose: The associations of trait mindfulness, decentering, and purpose in life with depressive symptoms, anxiety symptoms, and alcohol-related problems. Mindfulness. 2015;6:645–653. doi:10.1007/s12671-014-0300-8. [Google Scholar]
- Pepping C. A., Davis P. J., O’Donovan A. Individual differences in attachment and dispositional mindfulness: The mediating role of emotion regulation. Personality and Individual Differences. 2013;54:453–456. doi:10.1016/j.paid.2012.10.006. [Google Scholar]
- Preacher K. J., Rucker D. D., Hayes A. F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. doi:10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Reynolds L. M., Lin Y. S., Zhou E., Consedine N. S. Does a brief state mindfulness induction moderate disgust-driven social avoidance and decision-making? An experimental investigation. Journal of Behavioral Medicine. 2015;38:98–109. doi: 10.1007/s10865-014-9582-5. doi:10.1007/s10865-014-9582-5. [DOI] [PubMed] [Google Scholar]
- Roos C. R., Pearson M. R., Brown D. B. Drinking motives mediate the negative associations between mindfulness facets and alcohol outcomes among college students. Psychology of Addictive Behaviors. 2015;29:176–183. doi: 10.1037/a0038529. doi:10.1037/a0038529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer S., Walach H., Schmidt S., Hinterberger T., Lynch S., Büssing A., Kohls N. Assessment of mindfulness: Review on state of the art. Mindfulness. 2013;4:3–17. doi:10.1007/s12671-012-0122-5. [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21:486–497. doi: 10.1037/a0017074. doi:10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanay G., Bernstein A. State Mindfulness Scale (SMS): Development and initial validation. Psychological Assessment. 2013;25:1286–1299. doi: 10.1037/a0034044. doi:10.1037/a0034044. [DOI] [PubMed] [Google Scholar]
- Van Dam N. T., Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale—Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Research. 2011;186:128–132. doi: 10.1016/j.psychres.2010.08.018. doi:10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]
- Wechsler H., Lee J. E., Kuo M., Seibring M., Nelson T. F., Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. doi:10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Weitzman E. R. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. doi:10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K., Bowen S. Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology. 2010;78:362–374. doi: 10.1037/a0019172. doi:10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]