Abstract
Background
Non-medical prescription opioid use is increasing globally within high-income countries, particularly the United States. However, little is known about whether it is associated with negative outcomes for children. In this study, we use prescription opioid overdose as a proxy measure for non-medical prescription opioid use and ask the following: Do California communities with greater rates of non-medical prescription opioid use also have higher rates of child maltreatment and unintentional child injury?
Methods
We used longitudinal population data to examine ecological associations between hospital discharges involving overdose of prescription opioids and those for child maltreatment or child injury in California zip codes between 2001–2011 (n = 18,517 zip-code year units) using Bayesian space-time misalignment models.
Results
The percentage of hospital discharges involving prescription opioid overdose was positively associated with the number of hospital discharges for child maltreatment (relative rate=1.089, 95% credible interval (1.004, 1.165)) and child injury (relative rate= 1.055, 95% credible interval (1.012, 1.096)) over the ten-year period, controlling for other substance use and environmental factors.
Conclusions
Increases in community level prescription opioid overdoses between 2001–2011 are associated with a 2.06% increase in child maltreatment discharges and a 1.27% increase in discharges for child injury. Communities with higher rates of non-medical prescription opioid use may experience greater levels of child harms.
Keywords: prescription opioid overdose, child maltreatment, unintentional injury, spatial analysis
1. INTRODUCTION
Parenting behaviors can contribute to both intentional and unintentional harms to children and are important targets for prevention. Child maltreatment, which includes both abusive and neglectful parenting behaviors, remains a substantial problem within high-income countries with yearly estimates of 4–16% of children being physically abused and 10% being neglected or psychologically abused (Gilbert et al., 2009). In the United States, approximately 686,000 children are identified as victims of maltreatment each year (US DHHS, 2013) and as many as 12.5 percent of children are estimated to experience maltreatment before age 18 (Wildeman et al., 2014). In addition to the immediate harms that result from child maltreatment, these children are at risk for life-long emotional, social, and physical health problems such as depression, anxiety, low social support, suicide, serotonergic dysfunction and cardiovascular disease (Berglund et al., 2013; Fuller-Thomson et al., 2011; Marshall et al., 2013; McCauley et al., 1997; Norman et al., 2012; Sperry and Widom, 2013; Springer et al., 2007). As a result of these consequences, just one year of confirmed cases of maltreatment in the United States results in approximately $124 billion dollars of costs to society (Fang et al., 2012).
In addition, many children experience concerning levels of harm through unintentional injuries, which are consistently identied as some of the top 15 causes of death worldwide and within the top 10 causes of death within high income countries (World Health Organization, 2008). It is the number one cause of child mortality in the United States (Center for Disease Control and Prevention, 2012). Children experiencing unintentional injury may be victims of neglectful parenting not captured by current surveillance systems. Many unintentional injuries (excluding motor vehicle accidents) have been associated with insufficient supervision (Ewigman et al., 1993) including some poisonings (Ozanne-Smith et al., 2001), pedestrian injuries (Winn et al., 1991), burns (Cerovac and Roberts, 2000), and injury fatalities (Landen et al., 2003). In fact, children who have been reported to child welfare services for neglect within the United States have higher risk of death due to unintentional injury (Putnam-Hornstein et al., 2013).
Ecological studies conducted within the United States have found that characteristics of the substance use environment, which includes the availability of substances through formal or informal means as well as the geographic concentration of users, are associated with negative outcomes for children. Both on-premise (e.g., bars or restaurants) and off-premise (e.g., liquor stores) alcohol outlets are associated with neighborhood child maltreatment rates (Freisthler et al., 2012; Freisthler and Weiss, 2008; Morton, 2013; Morton et al., 2014), although some of the literature is mixed (Morton et al., 2014). Neighborhood indicators of drug markets, such as drug sales (Freisthler et al., 2012), and drug arrests (Albert and Barth, 1996; Freisthler et al., 2005; Freisthler and Weiss, 2008), have also been associated with referrals to child protective services or maltreatment rates. The mechanisms by which the substance use environment is related to child maltreatment remain primarily unknown. In the case of alcohol, people who live in neighborhoods with greater access to alcohol drink more frequently and in greater quantities (Gruenewald et al., 2014). Thus parents who live in neighborhoods with greater access to substances may use them more and the physiological effects of the substances could result in maltreatment. Recent multi-level research, however, suggests that the substance use environment impacts parenting outside of individual behaviors (Freisthler and Gruenewald, 2013; Friesthler et al., 2014), indicating other unknown social and ecological mechanisms. Neighborhoods with more substance use and access to substances may have lower levels of social control (e.g., people willing to intervene in problematic situations such as maltreatment).
In comparison to other substances, little is known about whether the prescription opioid environment (i.e., availability of prescription opioids and concentration of users) is independently related to child harms, despite the recent and large increase in prescription opioid use world-wide. Since the 1990s, medical use of prescription opioids has tripled with the predominant increase occurring in high income counties (International Narcotics Control Board, 2012). There is some evidence of emerging trends for medical and non-medical prescription opioid use within the European Union; however, the highest rates of increase have been observed within the United States (European Monitoring Centre for Drugs and Drug Addiction, 2011; International Narcotics Control Board, 2012; Shei et al., 2015). Between 1996 and 2011 in the United States, medical use of prescription opioids rose 1,448% while non-medical use (i.e., use without a prescription or in ways other than which it was prescribed) rose 4,680% (Atluri et al., 2014). In addition, United States mortality from prescription opioid overdose increased 200% from 2000 to 2014 (Rudd et al., 2016). In 2007, non-medical prescription opioid use cost U.S. society an estimated $55.7 billion due to lost earnings from premature death or unemployment, health care costs, and criminal incarceration (Birnbaum et al., 2011). In California, there are 596.3 opioid prescriptions per 1,000 residents as of 2013 (Paulozzi et al., 2015).
Emerging research in the United States suggests that non-medical prescription opioid use has a spatial dimension, with rates of abuse or overdose varying between neighborhoods (Brownstein et al., 2010), rural or urban areas (Green et al., 2011; Monnat and Rigg, 2016), and cities (Golub et al., 2013). Compared to other illicit drugs like heroin, prescription opioid overdoses may be more likely to occur in neighborhoods with higher incomes and less family fragmentation (Cerda et al., 2013). This indicates that the spatial patterning of non-medical prescription opioid use may differ from that of other substances. However, a recent cross-sectional study indicates that counties in the United States with high rates of treatment for alcohol and other illicit drug problems may also have greater rates of non-medical prescription opioid use (Wright et al., 2014), suggesting that there may be overlap between the non-medical prescription opioid and other substance use environments. It is unknown whether community level non-medical prescription opioid use contributes independently to rates of child maltreatment or injury. Better understanding of this relationship could allow for more targeted local prevention efforts to reduce non-medical prescription opioid use and subsequent community-level rates of child harm.
Our objective is to examine the relationship between non-medical prescription opioid use and child maltreatment and unintentional child injury in California zip codes between 2001 and 2011. To examine this, we use zip-code level prescription opioid overdose as a proxy for community non-medical prescription opioid use. We ask the following: Is the percentage of hospital discharges involving prescription opioid overdose associated with the number of hospital discharges for child maltreatment or unintentional injury?
2. METHODS
We conducted analyses of all California zip codes in the years 2001–2011, resulting in 18,517 zip code year units. These data were used to examine the ecological associations between prescription opioid overdose, child maltreatment, and child unintentional injury, while controlling for indicators of other substance use and zip-code level environmental characteristics. Bayesian space-time misalignment models (Zhu et al., 2013; Ponicki et al., 2013) were used to account for changes in zip code boundaries over time, while also controlling for spatial autocorrelation.
2.1 Data Sources and Variables
2.1.1 Hospital discharge data
We used hospital discharge data obtained from the California Office of Statewide Health Planning and Development (which includes all California hospital discharges of at least 1 overnight stay) to obtain measures for zip code level child maltreatment, child unintentional injury, prescription opioid use (as measured by prescription opioid overdoses), and alcohol or other drug dependence. Each hospital discharge is coded by up to 5 ICD-9 E-codes which identify the causes of the injury, poisoning, or illness leading to hospitalization. Discharges may also be coded by V-codes, which designate other factors associated with the health and well-being of the patient. Discharges are identified by the residential zip code of the patient, and therefore represent hospitalizations for individuals living in a specific zip code in a particular year.
2.1.2 Child maltreatment
We measured child maltreatment as the annual count of hospital discharges for children aged 0–17 with codes of V612.1 (e.g., battering of child, child neglect), E967.0–E967.9 or E995.5 (e.g., assaults due to child abuse).
2.1.3 Child unintentional injury
We calculated the annual count of hospital discharges among children aged 0–17 due to the following unintentional injuries: transport accidents not related to motor vehicles (which may be more likely to occur due to insufficient adult supervision) (E800–E809.9, E826–E848.9), poisonings (E850–869.9), fires or accidental suffocations (E880–929.9), and other accidents (E980–989.9). We excluded injuries due to motor vehicle accidents (which may be less attributable to inadequate supervision) as well as those due to adverse reactions from a medication or medical procedure.
2.1.4 Rate of hospitalization
We controlled for the overall hospitalization rate (rate of hospital discharges per capita/100), in order to account for differing access to health care across zip codes and time periods.
2.1.5 Prescription Drug Overdose
As a community indicator of prescription opioid overdoses, we calculated the percentage of all hospital discharges including an E-Code indicating poisoning from methadone, opiates, or other narcotics (E850.1, E850.2, E935.1, and E935.2). To maintain a specific focus on prescription opioid use, we excluded poisonings from non-narcotics and heroin.
2.1.6 Alcohol and other drug abuse and dependence
We used hospital discharge data to calculate the percentage of hospital discharges with ICD-9 diagnostic codes indicating alcohol abuse or dependence (E303.0, E305.0) and other drug abuse or dependence (E304.2, E304.3, E304.5, E305.2, E305.3, E305.6). We excluded discharges associated with methadone or prescription drug abuse or dependence.
All hospital discharges involving substance use were measured via the percentage of overall discharges in order to avoid collinearity with the overall hospitalization rate and to account for the fact that our substance abuse indicators can only be noted among people whose medical situation required an overnight stay in a hospital.
2.1.7 Intercensal Estimates
We selected covariates based on previous research examining ecological risks for child maltreatment and child injury (Freisthler et al., 2008). The co-variates were calculated with the use of intercensal data projection estimates at the census block group level (GeoLytics, 2013). First, we aggregated these census block estimates to year-specific zip codes. As census block groups do not necessarily align with zip code boundaries, we then used block weights representing the proportion of a census block within each zip code to calculate estimates of annual zip code demographics. Community demographics included age distribution (percentage 20–24, 25–44, 45–64, 65+), the percentage male, retail industries per square mile, population density (per square mile/100,000), and zip code instability (the percent change in local population from the prior year due to changes to a zip code’s boundaries). We also included community-level demographic variables such as percentage of Hispanic, Black, and White population, percentage of families living in poverty, median household income (per $10,000 in 2009 dollars), and the percentage of female headed households as proxies to control for social inequities that have been indicated to contribute to child harm in prior community studies (Coulton et al., 1999; Freisthler et al., 2007).
2.1.8 Alcohol Licensing
We obtained annual lists of active alcohol licenses from the California Department of Alcohol Beverage Control and aggregated geocoded premise addresses to zip codes. These data were used to assess the effects of alcohol outlet densities per square mile for both off- and on-premise locations.
2.2 Data Analysis
We used Bayesian space-time misalignment Poisson models (Zhu et al., 2013) to examine hospital discharges associated with child maltreatment and child injury in the years 2001–2011. These models help correct for changes in zip code boundaries over time (as determined by postal authorities) and account for spatial auto-correlation with year-specific conditional autoregressive (CAR) random effects based on spatial adjacencies.
The equation for the models was as follows:
Yi,t represents the count of hospital discharges for either child maltreatment or child injury in zip code i and year t. Ei,t reflects the expected number of hospital discharges for child maltreatment or child injury if these risks were equally distributed among families with children under age 18 in CA zip codes. The relative rate of the outcome for zip code i in year t is therefore exp(μi,t). Areas with relative rates of greater than 1 will have greater number of discharges for child maltreatment or child injury than expected, while those with relative rates of less than 1 have fewer discharges than expected.
The log relative rate (or μi,t,) is modeled as a linear relationship:
In this model, α is the statewide intercept, ρ is a linear time trend, the matrix X′i,t includes space-time covariates, while the vector β includes fixed-effects estimates of the relationship between those covariates and hospital discharges for child maltreatment or child injury. Two random effects, θi,t and φi,t, are included to allow for non-spatial and CAR spatially-autocorrelated variation not explained by other covariates.
We used WinBUGS 1.4.3 software (Lunn et al., 2000) to estimate models and used non-informative priors for all fixed and random effects. We allowed a burn-in period of between 40,000–120,000 Markov Chain Monte Carlo (MCMC) iterations in order for models to fully converge before sampling an additional 40,000 MCMC iterations.
3. RESULTS
Descriptive statistics for California zip codes between 2001 and 2011 are presented in Table 1. The mean number of zip codes per year was 1683.37 (SD=16.75). Averaged across years and zip codes, the mean number of hospital discharges for child maltreatment was 0.66 (SD=1.25), while the average for child injury was 7.69 (SD=11.21). The unweighted mean percentage of hospital discharges for prescription opioid overdose was 0.40% (SD=0.70). The unweighted mean percentages of hospital discharges related to alcohol abuse or dependence or illicit drug use and dependence were 2.11% (SD=2.31) and 1.41% (SD=2.29), respectively.
Table 1.
Descriptive statistics of model variables (n = 18,517 time-space units)
| Mean | SD | |
|---|---|---|
| Number of zip codes per year | 1683.37 | 16.75 |
| Outcome measures | ||
| Number of hospital discharges for child maltreatment | 0.66 | 1.25 |
| Number of hospital discharges for child unintentional injury | 7.69 | 11.21 |
| Substance use measures | ||
| % Hospital discharges for prescription drug overdose | 0.40 | 0.70 |
| % Hospital discharges for alcohol abuse & dependence | 2.11 | 2.31 |
| % Hospital discharges for other drug abuse & dependence | 1.41 | 2.29 |
| Other covariates | ||
| Overall hospitalization rate (/100,000) | 0.22 | 2.38 |
| Retail clutter/mile2 (×10) | 24.72 | 95.98 |
| Zip code instability | 0.01 | 0.33 |
| Population density (10,000/mile2) | 3.32 | 5.49 |
| Off-premise alcohol outlets/mile2 (×10) | 2.67 | 6.77 |
| On-premise alcohol outlets/mile2 (×10) | 5.60 | 23.37 |
| % Hispanic | 26.67 | 22.19 |
| % African American | 4.75 | 8.29 |
| % White | 56.06 | 25.36 |
| % Age 20–24 years | 6.97 | 2.87 |
| % Age 25–44 years | 27.31 | 6.90 |
| % Age 45–64 years | 25.60 | 6.39 |
| % Age 65 or older | 13.86 | 6.87 |
| % families living in poverty | 10.08 | 8.04 |
| Household income ($10,000 US) | 5.82 | 2.51 |
| % Female headed households with children | 2.58 | 2.28 |
| % Male | 50.67 | 4.94 |
time-space units are the unweighted averages of 18,517 annual zip-code observations
The results from our Bayesian spatial models examining hospital discharges for child maltreatment and child injury are presented in Table 2. The median of the MCMC estimates for each parameter was transformed into a relative rate (RR) by exponentiating the raw coefficient. The corresponding 95% credible interval for each estimate represents the 2.5th and 97.5th percentiles of the distribution of the posteriors for each model parameter.
Table 2.
Relative rates associated with zip code characteristics predicting child maltreatment and unintentional injury
| Model 1 Child maltreatment |
Model 2 Unintentional injury |
|||
|---|---|---|---|---|
| Median RR | (95% Credible Interval) | Median RR | (95% Credible Interval) | |
| Time trend | 1.005 | (0.996, 1.014) | 0.982 | (0.978, 0.986) |
| Substance use measures | ||||
| % Hospital discharges for prescription drug overdose |
1.089 | (1.004, 1.165) | 1.055 | (1.012, 1.096) |
| % Hospital discharges for alcohol abuse & dependence |
1.068 | (1.015, 1.068) | 0.990 | (0.977, 1.002) |
| % Hospital discharges for other drug abuse & dependence |
1.082 | (1.066, 1.096) | 1.056 | (1.044, 1.067) |
| Other covariates | ||||
| Overall hospitalization rate (/100,000) | 1.051 | (1.015, 1.068) | 1.051 | (1.043, 1.058) |
| Retail clutter/mile2 (×10) | 1.000 | (0.999, 1.001) | 0.999 | (0.998, 0.999) |
| Zip code instability | 0.755 | (0.191, 2.680) | 0.316 | (0.175, 0.563) |
| Population density (10,000/mile2) | 0.428 | (0.181, 0.917) | 1.411 | (0.961, 1.998) |
| Off-premise alcohol outlets/mile2 (×10) | 0.996 | (0.987, 1.005) | 1.015 | (1.010, 1.020) |
| On-premise alcohol outlets/mile2 (×10) | 1.002 | (0.999, 1.004) | 0.998 | (0.996, 0.999) |
| % Hispanic | 1.001 | (0.998, 1.003) | 1.007 | (1.006, 1.008) |
| % African American | 1.017 | (1.014, 1.021) | 1.007 | (1.005, 1.009) |
| % White | 0.998 | (0.995, 1.000) | 0.999 | (0.998, 0.999) |
| % Age 20–24 years | 0.941 | (0.925, 0.960) | 0.948 | (0.940, 0.956) |
| % Age 25–44 years | 0.950 | (0.942, 0.960) | 0.943 | (0.939, 0.947) |
| % Age 45–64 years | 0.929 | (0.919, 0.942) | 0.929 | (0.925, 0.934) |
| % Age 65 years or older | 0.963 | (0.957, 0.971) | 0.936 | (0.932, 0.939) |
| % Families living in poverty | 1.003 | (0.998, 1.008) | 1.007 | (1.004, 1.009) |
| Household income ($10,000 US) | 0.912 | (0.895, 0.929) | 1.042 | (1.034, 1.050) |
| % Female headed households with children | 0.943 | (0.919, 0.966) | 0.961 | (0.951, 0.972) |
| % Male | 1.021 | (1.004, 1.029) | 0.989 | (0.985, 0.993) |
Note: Includes 18,517 annual zip code observations
3.1 Child Maltreatment
There was a well-supported positive association between prescription opioid overdoses and child maltreatment at the zip-code level (RR= 1.089, 95% credible interval (1.004, 1.165)). This suggests that an additional percentage point of hospital discharges involving prescription opioid overdose (an increase of 1.43 standard deviations) is associated with an 8.9% increased risk of hospital discharges related to child maltreatment. There were also positive relationships of the percentages of discharges related to both alcohol abuse or dependence (RR=1.068, 95% credible interval (1.015, 1.068)) and illicit drug abuse or dependence (RR=1.082, 95% credible interval (1.066, 1.096)) to the rates of discharges for child maltreatment. The overall rate of hospital discharges, the percentage of Black population, and the percentage of male population were positively associated with discharges for child maltreatment, while higher population density, the percentage of population aged older than 19, and higher median income were negatively associated with discharges for child maltreatment.
3.2 Child Injury
We also found a positive association between zip-code rates of prescription opioid overdose and child injury (RR=1.055, 95% credible interval (1.012, 1.096)), indicating that an additional percentage point of hospital discharges involving prescription opioid overdose is correlated with a 5.5% increased risk of hospital discharges related to child injury. Additionally, the percentage of discharges associated with illicit drug abuse or dependence was positively associated with child injury (RR=1.56, 95% credible interval (1.044, 1.067)). There was no well supported association between alcohol abuse or dependence and child injury. Other co-variates positively associated with child injury included the overall hospital discharge rate, the percentage of Black population, the percentage of Hispanic population, higher median income, the percentage of families living in poverty, and density of off-premise alcohol outlets. Having greater percentages of the populations older than 19, having more retail clutter, a higher percentage of male population, and having greater percentage of female-headed households were all negatively associated with hospital discharges for child injury.
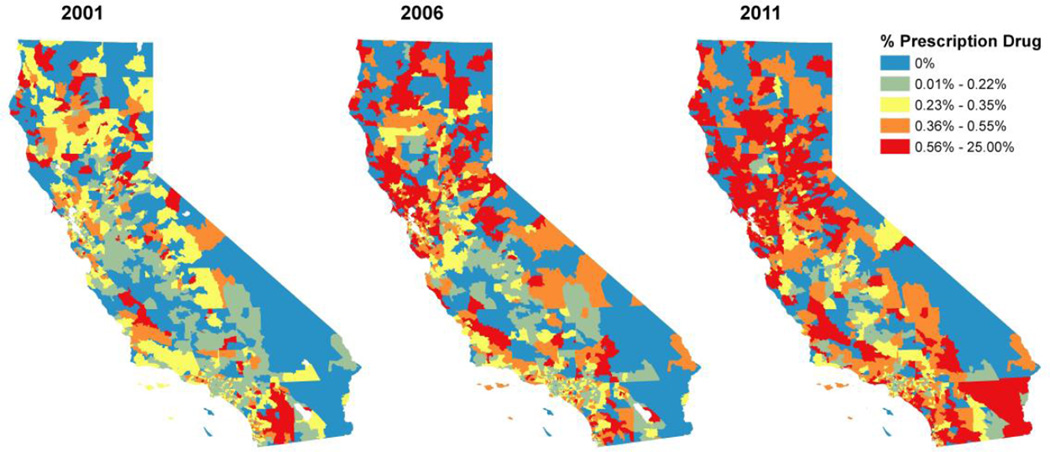
Figure 1 displays a map of the rates of prescription opioid overdose diagnoses among all hospital discharges within the first, middle, and last years analyzed. The figure shows prescription opioid overdose rates generally growing, but also differing across zip codes. The average statewide rate nearly doubled from 0.27% in 2001 to 0.50% in 2011, and this growth in prescription opioid overdoses is associated with increases of 2.06% in child abuse and 1.27% in child injury risks. Looking across zip codes within 2011, a zip code with prescription opioid overdose rates at the 80th percentile statewide would be expected to have 5.95% more child abuse and 3.77% more child injury than would an otherwise equivalent zip code at the 20th percentile of prescription opioid overdose rates.
Figure 1.
The % of hospital discharges involving prescription opioid overdoses by zip code, selected years
4. DISCUSSION
The rise in the number of deaths due to prescription opioid overdoses in high-income countries has led to increased attention towards non-medical prescription opioid use and efforts to prevent overdose. Little is known however, about whether communities with higher rates of overdose may also have greater risk of child harms. Our results suggest that prescription opioid overdoses are associated with both child maltreatment and child injury in California zip codes between the years 2001–2011. Increases in community level prescription opioid overdoses between 2001–2011 were associated with a 2.06% increase in child maltreatment discharges and a 1.27% increase in discharges for child injury. That communities with higher rates of non-medical prescription opioid use appear to experience greater levels of child harms suggests a need for interventions designed to alter the prescription opioid use environment in an effort to improve child well-being. For example, prescription monitoring programs (which have been implemented in most states), and policies regulating pain management clinics may lessen the availability of prescription opioids (Reiffler et al. 2012; Rutkow et al., 2015), potentially reducing non-medical use. Our findings also indicate that interventions designed to reduce the concentration of non-medical prescription opioid users in a community could be beneficial. Existing ecological research suggests that neighborhoods with more substance abuse treatment services have lower rates of child maltreatment (Morton, 2013). Finally, although our findings are ecological and cannot determine if parents who maltreat their children are non-medical prescription opioid users, limited research suggests that interventions pairing substance abuse treatment and parenting skills services can be effective (Berlin et al., 2014).
One strength of our study is that we investigate the non-medical prescription opioid use environment (as measured by prescription opioid overdoses) separately from that of the alcohol and illicit drug environments. Zip-code level prescription opioid overdose, alcohol abuse or dependence, and illicit drug abuse or dependence were all associated with child maltreatment. Prescription opioid overdose and illicit drug use or dependence were both associated with child injury. This suggests that community-level prescription opioid overdose is independently associated with community-level outcomes for children during this time period and should be considered in further studies in other parts of the United States [where prescription opioid rates can be approximately twice as high as California’s (Paulozzi et al., 2015)] and other high-income countries where non-medical prescription opioid use is less predominant but remains a public health concern (Shei et al., 2015).
Our results also suggest that large spatial differences in prescription opioid overdose across California are associated with substantial regional inequality in both child maltreatment and unintentional injury. Thus particular zip codes may be more in need of prevention strategies than others. Zip codes are crude approximations of communities, however, and more nuanced information is needed to better identify true “hot spots” of risk. Our findings do indicate, however, that understanding of how unique substance-related risks are distributed across places and communities could help inform which geographic regions might receive greater benefit from interventions designed to reduce the availability of prescription opioids and the concentration of non-medical prescription opioid users.
4.1 Alcohol and Other Illicit Drug Use Environments
To our knowledge, there are no other examinations of ecological relationships between prescription opioid overdose and child harms. However, several studies have investigated whether alcohol and drug environments are associated with these outcomes. For the most part our findings are similar to existing literature. Both alcohol availability (specifically the density of off-premise outlets) and indicators of illicit drug markets at the community level have been associated with child maltreatment (Albert and Barth, 1996; Freisthler et al., 2012, 2005; Freisthler and Weiss, 2008) and off-premise outlets have been associated with higher rates of child injury (Freisthler et al., 2008). Our finding that on-premise alcohol outlets are negatively associated with child injury is novel and warrants further investigation. Our observed effects suggest that having a greater percentage of population suffering from alcohol or illicit drug abuse or dependence is associated with greater rates of child maltreatment and that larger populations with illicit drug abuse or dependence and greater densities of off-premise alcohol outlets are associated with more child injuries in California.
4.2 Limitations
Hospital discharge data capture only the most severe cases of non-medical prescription opioid use. As a result, relationships between community-level rates of less severe non-medical prescription opioid use (i.e., instances not leading to overdose or hospitalization) and rates of child maltreatment or injury may be different than those described here. While hospital discharge codes have been found to be valid indicators of maltreatment, they do not represent legal definitions of maltreatment and do not identify all victims of maltreatment (Schnitzer et al., 2004). Ecological studies examine complex phenomena that are linked though a potentially long causal chain. As a result, our findings suggest that while an association exists between prescription opioid overdose and child maltreatment and child injury, the mechanisms for these associations may be mediated through untested and unknown variables. For example, results demonstrating community-level racial/ethnic and economic concentrations are related to child harm may be more of a consequence of residential segregation prevalent within California and its associated social inequities rather than individual racial/ethnic or economic identities (Coulton et al., 2007; Lee et al., 2008). As our models controlled for a variety of characteristics that are known to be associated with child maltreatment and child injury, it may be that more thorough knowledge of the ecological correlates of prescription opioid overdose and their potential relationship to child maltreatment or child injury could help us better refine estimates of the independent association of prescription opioid overdose. Ideally, complex analyses with multi-level data would assist with developing a thorough understanding of the mechanisms linking non-medical prescription opioid use to child maltreatment and injury.
4.3 Conclusion
Communities with higher rates of non-medical prescription opioid use may experience greater levels of child harms. Non-medical prescription opioid use appears to be one of a complex constellation of social environmental factors that could potentially contribute to harmful environments for children. In addition to lowering morbidity and mortality among users, efforts to reduce non-medical prescription opioid use could also positively impact child well-being.
Highlights.
A Bayesian space-time analysis of California zip codes from 2001–2011 is presented
Prescription opioid overdoses are related to hospital discharges for child maltreatment/injury
Communities with more non-medical prescription opioid use have greater levels of child harms
Acknowledgments
Role of Funding Source
This study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (P60-AA006282). NIAAA had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation review or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
The study authors had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. JP Wolf and WR Ponicki designed the study. JP Wolf, WR Ponicki, & A Gaidus were involved in data acquisition, preparation, and analysis. JP Wolf & NJ Kepple developed the study framing, prepared, and edited the manuscript.
Conflict of interest
All authors have no conflicts of interest to declare.
REFERENCES
- Albert VN, Barth RP. Predicting growth in child abuse and neglect reports in urban, suburban, and rural counties. Soc. Serv. Rev. 1996;70:58–82. [Google Scholar]
- Alturi S, Sudarshan G, Manchikanti L. Assessment of the trends in medical use and misuse of opioid analgesics from 2004 to 2011. Pain Physician. 2014;17:E119–E128. [PubMed] [Google Scholar]
- Berglund KJ, Balldin J, Berggren U, Gerdner A, Fahlke C. Childhood maltreatment affects the serotonergic system in male alcohol-dependent individuals. Alcohol. Clin. Exp. Res. 2013;37:757–762. doi: 10.1111/acer.12023. [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Shanahan M, Appleyard Carmody K. Promoting supportive parenting in new mothers with substance-use problems: a pilot randomized trial of residential treatment plus an attachment-based parenting program. Infant Ment. Health J. 2014;35:81–85. doi: 10.1002/imhj.21427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12:657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- Brownstein JS, Green TC, Cassidy TA, Butler SF. Geographic information systems and pharmacoepidemiology: using spatial cluster detection to monitor local patterns of prescription opioid abuse. Pharmacoepidemiol. Drug Saf. 2010;19:627–637. doi: 10.1002/pds.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. Atlanta: CDC; 2012. [Accessed on August 1, 2015]. Vital signs: Unintentional injury deaths among persons aged 0–19 years- United States 2000–2009. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6115a5.htm?s_cid=mm6115a5_w. [Google Scholar]
- Center for Disease Control and Prevention. WONDER. [Accessed on August 1, 2015];2014 http://wonder.cdc.gov.
- Cerda M, Ransome Y, Keyes KM, Koenen KC, Tracy M, Tardiff K, Vlahov D, Galea S. Prescription opioid mortality trends in New York City, 1990–2006: examining the emergence of an epidemic. Drug Alcohol Depend. 2013;132:53–62. doi: 10.1016/j.drugalcdep.2012.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerovac S, Roberts AHN. Burns sustained by hot bath and shower water. Burns. 2000;26:251–259. doi: 10.1016/s0305-4179(99)00127-8. [DOI] [PubMed] [Google Scholar]
- Coulton CJ, Crampton DS, Irwin M, Spilsbury JC, Korbin JE. How neighborhoods influence child maltreatment: a review of the literature and alternative pathways. Child Abuse Negl. 2007;31:1117–1142. doi: 10.1016/j.chiabu.2007.03.023. [DOI] [PubMed] [Google Scholar]
- Coulton CJ, Korbin JE, Su M. Neighborhoods and child maltreatment: a multi-level study. Child Abuse Negl. 1999;23:1019–1040. doi: 10.1016/s0145-2134(99)00076-9. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. Annual Report 2011: The State Of The Drugs Problem In Europe. Lisbon: Publications Office Of The European Union; 2011. [Accessed on June 1, 2016]. pp. 87–91. from http://www.emcdda.europa.eu/publications/annual-report/2011. [Google Scholar]
- Ewigman B, Kivlahan C, Land G. The Missouri Child Fatality Study: underreporting of maltreatment fatalities among children younger than 5 years of age, 1983 through 1986. Pediatrics. 1993;91:330–337. PMID: 8424006. [PubMed] [Google Scholar]
- Fang X, Brown DS, Florence CS, Mercy JA. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl. 2012;36:156–165. doi: 10.1016/j.chiabu.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald PJ. Where the individual meets the ecological: a study of parent drinking patterns, alcohol outlets, and child physical abuse. Alcohol. Clin. Exp. Res. 2013;37:993–1000. doi: 10.1111/acer.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald PJ, Ring L, LaScala EA. An ecological assessment of the population and environmental correlates of childhood accident, assault, and child abuse injuries. Alcohol. Clin. Exp. Res. 2008;32:1969–1975. doi: 10.1111/j.1530-0277.2008.00785.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Holmes MR, Wolf JP. The dark side of social support: understanding the role of social support, drinking behavior and alcohol outlets for child physical abuse. Child Abuse Negl. 2014;38:1106–1119. doi: 10.1016/j.chiabu.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Kepple NJ, Holmes M. The geography of drug market activities and child maltreatment. Child Maltreat. 2012;17:144–152. doi: 10.1177/1077559512443124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Needell B, Gruenewald PJ. Is the physical availability of alcohol and illicit drugs related to neighborhood rates of child maltreatment? Child Abuse Negl. 2005;29:1049–1060. doi: 10.1016/j.chiabu.2004.12.014. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Weiss RE. Using Bayesian space-time models to understand the substance use environment and risk for being referred to Child Protective Services. Subst. Use Misuse. 2008;43:239–251. doi: 10.1080/10826080701690649. [DOI] [PubMed] [Google Scholar]
- Fresithler B, Bruce E, Needell B. Understanding the geospatial relationship of neighborhood characteristics and rates of maltreatment for black, hispanic, and white children. Soc. Work. 2007;52:7–16. doi: 10.1093/sw/52.1.7. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Brennenstuhl S, Frank J. The association between childhood physical abuse and heart disease in adulthood: findings from a representative community sample. Child Abuse Negl. 2011;34:689–698. doi: 10.1016/j.chiabu.2010.02.005. [DOI] [PubMed] [Google Scholar]
- GeoLytics. Geolytics Estimates Premium. East Brunswick, NJ: GeoLytics, Inc.; 2013. [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high income countries. Lancet. 2009;373:3–9. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Golub A, Elliott L, Brownstein HH. The opiate pain reliever epidemic among U.S. arrestees 2000–2010: regional and demographic variations. J. Ethn. Subst. Abuse. 2013;12:1–29. doi: 10.1080/15332640.2013.759498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 2011;115:221–228. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Remer LG, LaScala EA. Testing a social ecological model of alcohol use: the California 50-city study. Addiction. 2014;109:736–745. doi: 10.1111/add.12438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Narcotics Control Board. New York: International Narcotics Control Board; 2012. [Accessed on June 1, 2016]. Narcotic Drugs: Estimated World Requirements For 2013 - Statistics For 2011 (No. T.13.XI.2) from https://www.incb.org/incb/en/narcotic-drugs/Technical_Reports/2012/narcotic-drugs-technical-report_2012.html. [Google Scholar]
- Landen MG, Bauer U, Kohn M. Inadequate supervision as a cause of injury deaths among young children in Alaska and Louisiana. Pediatrics. 2003;111:328–331. doi: 10.1542/peds.111.2.328. PMID: 12563059. [DOI] [PubMed] [Google Scholar]
- Lee BA, Reardon SF, Firebaugh G, Farrell CR, Matthews SA, O’Sullivan D. Beyond the census tract: patterns and determinants of racial segregation at multiple geographic scales. Am. Sociol. Rev. 2008;73:766–791. doi: 10.1177/000312240807300504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS--a Bayesian modeling framework: concepts, structure, and extensibility. Stats Comput. 2000;10:325–337. [Google Scholar]
- Marshall BD, Galea S, Wood E, Kerr T. Longitudinal associations between types of childhood trauma and suicidal behavior among substance users: a cohort study. Am. J. Public Health. 2013;103:e69–e75. doi: 10.2105/AJPH.2013.301257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, Ryden J, Derogatis LR, Bass EB. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277:1362–1368. [PubMed] [Google Scholar]
- Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J. Rural Health. 2016;32:204–218. doi: 10.1111/jrh.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton CM. The moderating effect of substance abuse service availability on the relationship between child maltreatment and neighborhood alcohol availability. Child Youth Serv Rev. 2013;35:1933–1940. doi: 10.1016/j.childyouth.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton CM, Simmel C, Peterson NA. Neighborhood alcohol outlet density and rates of child abuse and neglect: moderating effects of access to substance abuse services. Child Abuse Negl. 2014;38:952–961. doi: 10.1016/j.chiabu.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic and meta-analysis. PLoS Med. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozanne-Smith J, Day L, Parsons B, Tibballs J, Dobbin M. Childhood poisoning: access and prevention. J. Pediatrics Child Health. 2001;37:262–265. doi: 10.1046/j.1440-1754.2001.00654.x. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Strickler GK, Kreiner PW, Koris CM. Controlled substance prescribing patterns—Prescription Behavior Surveillance System, Eight States, 2013. MMWR Surveill. Summ. 2015;64:1–14. doi: 10.15585/mmwr.ss6409a1. [DOI] [PubMed] [Google Scholar]
- Ponicki WR, Gruenewald PJ, Remer LG. Spatial panel analyses of alcohol outlets and motor vehicle crashes in California: 1999–2008. Accid. Anal. Prev. 2013;55:135–143. doi: 10.1016/j.aap.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam-Hornstein E, Cleves MA, Licht R, Needell B. Risk of fatal injury in young children following abuse allegations: evidence from a prospective, population-based study. Am. J. Public Health. 2013;103:e39–e44. doi: 10.2105/AJPH.2013.301516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reifler LM, Droz D, Bailey JE, Schnoll SH, Fant R, Dart RC, Bucher Bartelson B. Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Med. 2012;13:434–442. doi: 10.1111/j.1526-4637.2012.01327.x. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR. 2016;64:1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Rutkow L, Chang HY, Daubresse M, Webster DW, Stuart EA, Alexander GC. Effect of Florida’s Prescription Drug Monitoring Program and pill mill laws on opioid prescribing and use. JAMA Intern. Med. 2015;175:1642–1649. doi: 10.1001/jamainternmed.2015.3931. [DOI] [PubMed] [Google Scholar]
- Schnitzer PG, Slusher P, Van Tuinen M. Child maltreatment in Missouri: combining data for public health surveillance. Am. J. Prev. Med. 2004;27:379–384. doi: 10.1016/j.amepre.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Shei A, Hirst M, Kirson NY, Enloe CJ, Birnbaum HG, Dunlop WC. Estimating the health care burden of prescription opioid abuse in five European countries. Clinicoecon Outcomes Res. 2015;7:477–488. doi: 10.2147/CEOR.S85213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperry DM, Widom CS. Child abuse and neglect, social support, and psychopathology in adulthood: a prospective investigation. Child Abuse Negl. 2013;37:415–425. doi: 10.1016/j.chiabu.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl. 2007;31:517–530. doi: 10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Child Maltreatment 2012. [Accessed on August 1, 2015];2013 from http://acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment.
- Wildeman C, Emanuel N, Leventhal JM, Putnam-Hornstein E, Waldfogel J, Lee H. The prevalence of confirmed maltreatment among US children, 2004 to 2011. JAMA Pediatr. 2014;168:706–713. doi: 10.1001/jamapediatrics.2014.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winn D, Agran PF, Castillo DN. Pedestrian injuries to children younger than 5 years of age. Pediatrics. 1991;88:776–782. PMID: 1896282. [PubMed] [Google Scholar]
- World Health Organization. World Report On Child Injury Prevention. [Accessed on June 1, 2016];2008 from http://www.who.int/violence_injury_prevention/child/injury/world_report/en/ [PubMed]
- Wright E, Kooreman HE, Greene MS, Chambers RA, Banerjee A, Wilson J. The iatrogenic epidemic of prescription drug abuse: county-level determinants of opioid availability and abuse. Drug Alcohol Depend. 2014;138:209–215. doi: 10.1016/j.drugalcdep.2014.03.002. [DOI] [PubMed] [Google Scholar]
- Zhu L, Waller LA, Ma J. Spatial-temporal disease mapping of illicit drug abuse or dependence in the presence of misaligned ZIP codes. GeoJournal. 2013;78:463–474. doi: 10.1007/s10708-011-9429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]