Abstract
Background
Obesity negatively impacts motor function leading to an increase in fall risk. Massive weight loss improves some aspects of gait on flat ground. However, we have little information about whether gait changes during flat ground walking and during more complex motor tasks beyond flat ground walking.
Objectives
Our objectives were to examine how massive weight loss after Roux-en-Y bariatric surgery affects gait during flat ground walking and obstacle crossing one year post surgery.
Setting
United States
Methods
Nineteen adult females walked under five conditions: initial baseline walking on flat ground, crossing three obstacle heights, and final baseline walking on flat ground for a total of 25 trials. Spatio-temporal gait parameters were collected simultaneously using a gait carpet and body-worn sensors.
Results
Gait improved post surgery with the strongest effect observed for double limb support time during flat ground walking (p<.001) and obstacle crossing (p<.001). The reduction in body mass index was correlated with improved swing (p<.01) and double limb support time (p<.01) during flat ground walking and improved swing during obstacle crossing on low (p<.01), medium (p<.01), and high (p<.01) obstacles. Improved gait post surgery was more pronounced on high obstacles for velocity (p<.001) and double limb support time (p<.001).
Conclusions
Massive weight loss results in improved spatio-temporal gait patterns during flat ground walking. Examining how massive weight loss affects spatio-temporal gait may help create ways to encourage a more active lifestyle for adults with obesity.
Keywords: obesity, gait, bariatric surgery, walking, obstacles
Introduction
Obesity, defined as elevated body mass index (BMI), affects over 30% of U.S. adults [1] and is classified as a disease [2]. Obesity negatively impacts motor function; adults with obese BMI (BMI ≥ 30 kg/m2) walk with slower velocities, shorter step lengths, and more time in double limb support compared to adults with normal BMI [3–5]. Presumably, they walk more slowly, take shorter steps, and have longer foot contact to increase stability. These modifications could affect recovering from a loss of balance to prevent falls (e.g., impaired postural control during quiet stance) [6]; fall risks are 50% higher for adults with obesity above 65 years old [7].
Bariatric surgery is a direct method for inducing massive weight loss. After Roux-en-Y bariatric surgery, adults’ body mass decreases by nearly 35% with most weight loss occurring by one year post surgery [8]. In studies showing improved gait during flat ground walking at 3 months [9], 8.8 months [10], 12 months [11–13], and up to 5 years [14], after surgery, patients decreased step width (i.e., lateral distance between the feet) [9, 10], and increased velocity, step length, and single limb support time [9].
Despite the potential for massive weight loss to improve gait parameters related to fall risks, we know little about gait changes after bariatric surgery. Although valuable information exists about some changes in gait after bariatric surgery, gait has mainly been examined during flat ground walking. Atypical gait linked with obesity is more pronounced when meeting an external constraint [15] such as obstacle crossing [16]. Thus, it is unknown if improvements on flat ground transfer to tasks beyond flat ground. Our aims were to determine spatio-temporal gait differences before and one year after bariatric surgery: 1) during flat ground walking, 2) during obstacle crossing, and 3) between a reduction in BMI and gait post-surgery. We hypothesized that massive weight loss would lead to improved gait during flat ground walking and obstacle crossing.
Materials and Methods
Participants
Nineteen female adults (Mean age=44.16, SD=8.2) with obese BMI were recruited at XXXXX Medical Center from the Nutrition and Weight Management and Bariatric Surgery Clinics (Table 1).
Table 1.
Demographic and anthropometric information for participants. Means are provided with standard deviations in parentheses.
| Pre-surgery | Post-surgery | |
|---|---|---|
| Weight (kg) | 114.5 (14.7) | 81.3 (16.5) |
| Height (cm) | 164.7 (6.8) | |
| BMI (kg/m2) | 42.3 (4.2) | 29.96 (5.1) |
| % Excess BMI Lost | 74.65 (25.1) |
BMI=body mass index
Patients between 30 and 60 years old and eligible to undergo Roux-en-Y bariatric surgery were included. All participants walked independently without assistive devices. Participants were excluded if they had or were scheduled to undergo knee surgery, were receiving dialysis, or being treated for cancer. The study was approved by the XXXXX Institutional Review Board and conformed to the Declaration of Helsinki. Informed written and verbal consent were obtained before testing began.
Gait Measurements and Obstacles
Data were collected simultaneously using a GAITRite Walkway system (CIR Systems Inc., Sparta, NJ) and wearable sensor technology (LEGSys™, Biosensics, Cambridge, MA [17, 18]). The GAITRite mat was a 4.88 m long × 0.61 m wide pressure-sensitive mat with a temporal resolution of 120 Hz and a spatial resolution of 1.27 cm. LEGSys™ includes five wearable sensors containing triaxial gyroscopes, accelerometers, and magnetometers [17, 18]. Dependent variables selected included velocity (cm/s) and percent of gait cycle spent in swing and double limb support.
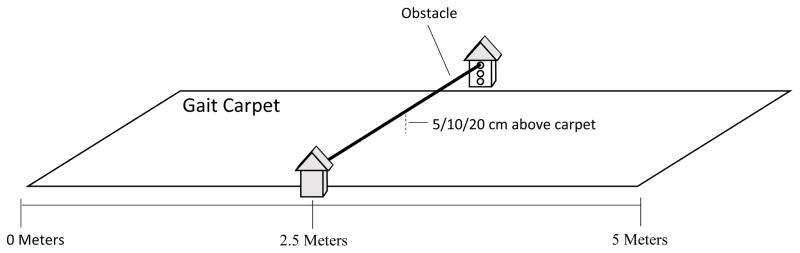
For the obstacle task, participants stepped over obstacles of various heights. Obstacles were created using a wooden dowel (121 cm long) and two rectangular towers (9 cm × 10 cm × 22 cm) with holes drilled at 4 cm, 8 cm, and 16 cm (low, medium, and high). Towers were placed halfway down the walking path (8 m) on either side of the GAITRite with the dowel fitted into corresponding holes in each tower (Figure 1).
Figure 1.
Obstacle crossing experimental setup. Participants began obstacle trials at the far end of the carpet facing the wooden dowel. They crossed three obstacle heights created by fitting the dowel into corresponding holes in each tower.
Procedure
After consenting, participants’ height and weight were measured using a stadiometer and scale, respectively. They were then fitted with five LEGSys™ sensors attached with stretchable Velcro straps to anterior aspects of both thighs above the knees, anterior portions of both shins above the ankles, and posteriorly on the small of the back.
Participants walked at a self-selected pace for 25 trials down a 16-m walking path with the GAITRite in the center. The 25 trials included five conditions for five trials each: initial baseline, crossing obstacles of three heights, and final baseline. Initial and final baselines involved walking on flat ground without obstacles. For obstacle conditions, low, medium, and high obstacles were placed halfway down the path. Obstacle height order was randomized using a random number generator and counterbalanced between patients.
Statistical Analyses
All analyses were conducted using SPSS version 22.0. Pearson’s correlation statistic was used to examine relationships between changes in BMI and gait from pre- to post-surgery. Autocorrelations were conducted to examine possible trial order learning effects. To determine differences in gait, we used linear models of change; one for each dependent variable with two within subject factors as independent variables: sessions and conditions. Since there were multiple measures within each participant with data for left and right legs, generalized estimating equations (GEE) were used in model estimation. This approach acknowledges clustering observations at the participant level while providing consistent estimates of associations between variables. Post hoc analyses consisted of pairwise comparisons. The Bonferroni correction was used for all tests. Effect sizes are reported via Cohen’s d after p-values.
Results
Available Data
Of the expected 475 trials pre- and post-surgery, 454 and 452 trials were available for analyses respectively. Missed trials were due to equipment failure. Data collected from the gait carpet and LEGSys™ were correlated for velocity (r(19)=.90, p=.015), swing phase (r(19)=.93, p=.007), and double limb support (r(19)=.92, p=.01). BMI pre and post surgery were available for all participants (Table 1). BMI decreased by 29%.
Initial and Final Baseline Walking
Before surgery, BMI was not correlated with velocity (r(19)=−.22, p>.05), double support (r(19)=.26, p>.05) or single limb support time (r(19)=−.26, p>.05). However, post surgery, the higher the BMI difference, the greater the swing phase at initial (r(19)=.66, p=.002) and final (r(19)=.77, p<.001) baselines. Higher BMI differences were associated with less double limb support at initial and final baseline (rs ranged from −.65 to −.77, all ps <.01) post surgery. No learning effects were found based on the autocorrelation results (all ps>.05).
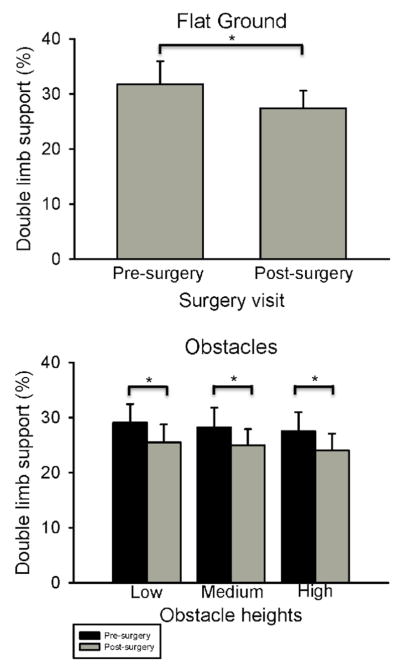
One year after surgery, adults increased swing by 5% and decreased double limb support by 14% (Figure 2). Velocity was 4% higher at final versus initial baseline (Tables 2A & 3).
Figure 2.
Percent double limb support on flat ground and during obstacle crossing. Data presented are means and standard deviations. Asterisks represent pre- to post-surgery decreases in double limb support at p<.05.
Table 2A.
Differences in gait at initial and final baseline for pre and post surgery (post minus pre surgery). Means are provided with standard deviation in parentheses.
| Initial Baseline | Final Baseline | |
|---|---|---|
| Velocity (cm/s) | 5.6* | 2.9* |
| (0.2) | (0.5) | |
| Swing (%) | 2.2+ | 1.4+ |
| (0.4) | (2.5) | |
| Double limb support (%) | −4.4+ | −4.2+ |
| (1.4) | (0.7) |
pre/post surgery effects
initial/final baseline effects
Table 3.
Generalized Estimating Equations Results
| Result | Statistic | p-value | Cohen’s d |
|---|---|---|---|
| Initial and final baseline walking | |||
| Session effect: Swing phase | Wald X2(1, N=19)=9.54 | p=.002 | d=−0.92 |
| Session effect: Double limb support | Wald X2(1, N=19)=26.17 | p<.001 | d=1.20 |
| Session effect: Velocity | Wald X2(1, N=19)=6.31 | p=.012 | d=−0.29 |
| Obstacle crossing | |||
| Session effect: Swing phase | Wald X2(1, N=19)=12.34 | p<.001 | d=−0.74 |
| Session effect: Double limb support | Wald X2(1, N=19)=19.12 | p<.001 | d=1.08 |
| Condition effect: Velocity | Wald X2(2, N=19)=40.50 | p<.001 | See text |
| Condition effect: Swing | Wald X2(2, N=19)=27.58 | p<.001 | See text |
| Condition effect: Double limb support | Wald X2(2, N=19)=37.76 | p<.001 | See text |
| Obstacle approach versus end | |||
| Session effect: Velocity | Wald X2(1, N=19)=7.01 | p=.008 | See text |
| Session effect: Swing phase | Wald X2(1, N=19)=53.27 | p<.001 | See text |
| Session effect: Double limb support | Wald X2(1, N=19)=57.39 | p<.001 | See text |
| Condition effect: Velocity | Wald X2(2, N=19)=38.77 | p<.001 | See text |
| Condition effect: Swing | Wald X2(2, N=19)=104.59 | p<.001 | See text |
| Condition effect: Double limb support | Wald X2(2, N=19)=69.29 | p<.001 | See text |
| Interaction: Velocity | Wald X2(2, N=19)=9.19 | p<.001 | See text |
Obstacle Crossing
Decreased BMI from pre to post surgery was correlated with gait during obstacle conditions. Post surgery, for low (r(19)=.55, p=.014), medium (r(19)=.56, p=.014), and high (r(19)=.54, p=.016) obstacles, higher decreases in BMI were linked with greater swing phases. For all three obstacles, the higher the drop in BMI, the less the double limb support one year later (rs ranged from −.45 to −.54, all ps <.05).
From pre to post surgery, participants increased swing by 4% and decreased double limb support by 12%. We also found main effects for condition for velocity, percent swing, and percent double limb support time. Velocity was 5% higher during low versus high obstacles, swing was 1% longer during medium versus low obstacles, and percent double limb support was 3% higher during low versus medium and 6% higher in low versus high obstacles (Tables 2B & 3; Figure 2).
Table 2B.
Differences in gait parameters at obstacle conditions pre/post surgery (post minus pre surgery). Means are provided with standard deviation in parentheses.
| Low | Medium | High | |
|---|---|---|---|
| Velocity (cm/s) | −1.5* | 0.1+ | 2.5+* |
| (2.8) | (3.1) | (3.6) | |
| Swing (%) | 1.7*+ | 1.6*+ | 1.7+ |
| (0.01) | (0.6) | (0.2) | |
| Double limb support (%) | −3.6*+ | −3.3*+ | −3.5*+ |
| (0.1) | (0.7) | (0.4) |
pre/post surgery effects
obstacle condition effects
We also examined gait as patients approached (i.e., approach) or walked away from obstacles after crossing (i.e., end). Post surgery, velocity was 8% faster, swing was 6% longer, and 15% less time was spent in double limb support. We also found condition effects for velocity, swing phase, and percent double limb support. Velocity was 5% slower at high versus low (p<.001, d=.32) and medium obstacles (p<.001, d=.27), swing was 2% higher at high versus low (p<.001, d=−.71) and 1% higher at high versus medium obstacles (p=.004, d=−.42), and double limb support percent was 7% lower at high versus low (p<.001, d=.65) and 4% lower at high versus medium obstacles (p<.001, d=.41). Results showed an interaction between trial section (approach versus end) and obstacle condition. Velocity was 6% higher when approaching low versus high obstacles (p<.001, d=.32) and 5% higher when approaching medium versus high obstacles (p<.001, d=.28). Velocity was also 5% higher after crossing low (p<.001, d=.31) and medium (p<.001, d=.27) versus high obstacles.
Discussion
The purpose of this study was to examine differences in flat ground walking and obstacle crossing before and one year post bariatric surgery. After one year, patients increased swing and decreased double limb support. Patients decreased velocity on high versus low and medium obstacles.
Massive weight loss led to increased velocity. Even when normal weight adults walk with weight added, they decrease and subsequently increase velocity once the weight is removed [19]. Also, after surgery, participants decreased attempts at maintaining stability. Taking shorter, slower steps and increasing foot contact time reflects efforts to increase postural stability [6]. Less weight may have reduced compensating for postural instability and allowed patients to walk faster and spend more time balancing on one leg.
When walking at pre-determined paces, adults with higher BMI demonstrate gait that could lead to falls [15]. Adults with obesity have reduced ankle, knee, and hip range of motion [3]. They also have greater absolute ground reaction forces [20] and increased knee load [21] at paces faster than their preferred speed. These walking differences are attributed to attempts to minimize mechanical external work [22], decrease load at the knee [23], and curb energy cost and relative effort [20]. Yet, these differences are associated with increased safety risks [15]. Decreased weight following surgery can minimize obesity’s effect on walking biomechanics; adults show decreased hip and knee joint moments [10] and ground reaction forces [24, 25] following bariatric surgery. Previous work shows kinematic differences during obstacle crossing [4, 16, 26]. However, spatio-temporal parameters may be less sensitive to differences in obstacle crossing.
Double limb support improved post-surgery. Prolonged double limb support is a risk factor for predicting falls [27, 28]. In a study of 597 older adults, double limb support was the best predictor of fall risk [28]. Also, prolonged double limb support is linked with perceived fatigue [29] and increased energy expenditure [30] during walking. Thus, reduced double limb support may lead to a more active lifestyle following bariatric surgery.
Limitations
One limitation includes use of a stationary obstacle. However, this paradigm is a safe method for testing gait after surgery. Second, we only tested female participants. Third, we did not include habituation trials to formally address possible learning effects.
Conclusions
Massive weight loss results in improved spatio-temporal gait during flat ground walking and obstacle crossing. Examining how massive weight loss affects spatio-temporal gait may help create ways to encourage a more active lifestyle for adults with obesity.
Acknowledgments
We sincerely thank the participants and lab members for assistance with data collection and processing. We also offer many thanks to Dr. David Felson for his guidance and feedback on an earlier version of this manuscript.
Support: Supported by funds from an R03 AR066344-01A1 (Gill, PI) and NIH AR47785 (Felson, PI).
Footnotes
Conflict of Interest: There are no conflicts of interest.
Disclosures
The authors have no commercial associations that might be a conflict of interest in relation to this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Flegal KM. Prevalence of obesity in the United States. JAMA. 2014;312:189–90. doi: 10.1001/jama.2014.6228. [DOI] [PubMed] [Google Scholar]
- 2.AMA. Recognition of obesity as a disease. 2013 [Google Scholar]
- 3.Hills AP, Hennig EM, Byrne NM, Steele JR. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obes Rev. 2002;3:35–43. doi: 10.1046/j.1467-789x.2002.00054.x. [DOI] [PubMed] [Google Scholar]
- 4.Hung YC, Gill SV, Meredith GS. Influence of dual task constraints on whole body organization during walking in overweight and obese children. Am J Phys Med Rehab. 2013;92:461–7. doi: 10.1097/PHM.0b013e31828cd59d. [DOI] [PubMed] [Google Scholar]
- 5.da Silva-Hamu TC, Formiga CK, Gervasio FM, Ribeiro DM, Christofoletti G, de Franca Barros J. The impact of obesity in the kinematic parameters of gait in young women. Int J Gen Med. 2013;6:507–13. doi: 10.2147/IJGM.S44768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh D, Park W, Levy MS, Jung ES. The effects of obesity and standing time on postural sway during prolonged quiet standing. Ergonomics. 2009;52:977–86. doi: 10.1080/00140130902777636. [DOI] [PubMed] [Google Scholar]
- 7.Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60:124–9. doi: 10.1111/j.1532-5415.2011.03767.x. [DOI] [PubMed] [Google Scholar]
- 8.Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:2416–25. doi: 10.1001/jama.2013.280928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vincent HK, Ben-David K, Conrad BP, Lamb KM, Seay AN, Vincent KR. Rapid changes in gait, musculoskeletal pain, and quality of life after bariatric surgery. Surg Obes Relat Dis. 2012;8:346–54. doi: 10.1016/j.soard.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Vartiainen P, Bragge T, Lyytinen T, Hakkarainen M, Karjalainen PA, Arokoski JP. Kinematic and kinetic changes in obese gait in bariatric surgery-induced weight loss. J Biomech. 2012;45:1769–74. doi: 10.1016/j.jbiomech.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Hortobagyi T, Herring C, Pories WJ, Rider P, Devita P. Massive weight loss-induced mechanical plasticity in obese gait. J Appl Physiol (1985) 2011;111:1391–9. doi: 10.1152/japplphysiol.00291.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maniscalco M, Zedda A, Giardiello C, Faraone S, Cerbone MR, Cristiano S, et al. Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obes Surg. 2006;16:836–41. doi: 10.1381/096089206777822331. [DOI] [PubMed] [Google Scholar]
- 13.de Souza SA, Faintuch J, Fabris SM, Nampo FK, Luz C, Fabio TL, et al. Six-minute walk test: functional capacity of severely obese before and after bariatric surgery. Surg Obes Relat Dis. 2009;5:540–3. doi: 10.1016/j.soard.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Froehle AW, Laughlin RT, Teel DD, 2nd, Sherwood RJ, Duren DL. Excess body weight loss is associated with nonpathological gait patterns in women 4 to 5 years after bariatric surgery. Obes Surg. 2014;24:253–9. doi: 10.1007/s11695-013-1069-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill SV, Narain A. Quantifying the Effects of Body Mass Index on Safety: Reliability of a Video Coding Procedure and Utility of a Rhythmic Walking Task. Arc Phys Med Rehab. 2012;93:728–30. doi: 10.1016/j.apmr.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Gill SV, Hung YC. Influence of weight classification on children stepping over obstacles. Am J Phys Med Rehab. 2012;91:625–30. doi: 10.1097/PHM.0b013e31824fa81e. [DOI] [PubMed] [Google Scholar]
- 17.Aminian K, Najafi B, Bula C, Leyvraz PF, Robert P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J Biomech. 2002;35:689–99. doi: 10.1016/s0021-9290(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 18.Najafi B, Helbostad JL, Moe-Nilssen R, Zijlstra W, Aminian K. Does walking strategy in older people change as a function of walking distance? Gait Pos. 2009;29:261–6. doi: 10.1016/j.gaitpost.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Aruin AS. The effect of short-term changes in the body mass on anticipatory postural adjustments. Exp Brain Res. 2007;181:333–46. doi: 10.1007/s00221-007-0931-2. [DOI] [PubMed] [Google Scholar]
- 20.Browning RC, Kram R. Effects of obesity on the biomechanics of walking at different speeds. Med Sci Sports Exerc. 2007;39:1632–41. doi: 10.1249/mss.0b013e318076b54b. [DOI] [PubMed] [Google Scholar]
- 21.Peyrot N. Biomechanical constraints associated with walking in obese individuals. Phys Ther Rev. 2012;17:352–3. [Google Scholar]
- 22.Malatesta D, Vismara L, Menegoni F, Galli M, Romei M, Capodaglio P. Mechanical external work and recovery at preferred walking speed in obese subjects. Med Sci Sports Exerc. 2009;41:426–34. doi: 10.1249/MSS.0b013e31818606e7. [DOI] [PubMed] [Google Scholar]
- 23.Peyrot N, Morin JB, Thivel D, Isacco L, Taillardat M, Belli A, et al. Mechanical work and metabolic cost of walking after weight loss in obese adolescents. Med Sci Sports Exerc. 2010;42:1914–22. doi: 10.1249/MSS.0b013e3181da8d1e. [DOI] [PubMed] [Google Scholar]
- 24.Bacha IL, Benetti FA, Greve JM. Baropodometric analyses of patients before and after bariatric surgery. Clinics (Sao Paulo) 2015;70:743–7. doi: 10.6061/clinics/2015(11)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bragge T, Lyytinen T, Hakkarainen M, Vartiainen P, Liikavainio T, Karjalainen PA, et al. Lower impulsive loadings following intensive weight loss after bariatric surgery in level and stair walking: a preliminary study. Knee. 2014;21:534–40. doi: 10.1016/j.knee.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Gill SV, Hung YC. Effects of overweight and obese body mass on motor planning and motor skills during obstacle crossing in children. Res Dev Disabil. 2014;35:46–53. doi: 10.1016/j.ridd.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 27.Maki Y, Ura C, Yamaguchi T, Murai T, Isahai M, Kaiho A, et al. Effects of intervention using a community-based walking program for prevention of mental decline: a randomized controlled trial. J Am Geriatr Soc. 2012;60:505–10. doi: 10.1111/j.1532-5415.2011.03838.x. [DOI] [PubMed] [Google Scholar]
- 28.Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:896–901. doi: 10.1093/gerona/glp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kalron A. Association between perceived fatigue and gait parameters measured by an instrumented treadmill in people with multiple sclerosis: a cross-sectional study. J Neuroeng Rehabil. 2015;12:34. doi: 10.1186/s12984-015-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuo AD, Donelan JM, Ruina A. Energetic consequences of walking like an inverted pendulum: step-to-step transitions. Exerc Sport Sci Rev. 2005;33:88–97. doi: 10.1097/00003677-200504000-00006. [DOI] [PubMed] [Google Scholar]