Abstract
Purpose
A significant limitation of checkpoint blockade immunotherapy is the relatively low response rate (e.g. ~20% with PD-1 blockade in lung cancer). In this study, we tested whether strategies which increase T cell infiltration to tumors can be efficacious in enhancing immunotherapy response.
Experimental Design
We performed an unbiased screen to identify FDA-approved oncology agents with ability to enhance T cell chemokine expression with the goal of identifying agents capable of augmenting immunotherapy response. Identified agents were tested in multiple lung tumor models as single agents and in combination with PD-1 blockade. Additional molecular and cellular analysis of tumors was used to define underlying mechanisms.
Results
We found that histone deacetylase (HDAC) inhibitors (HDACi) increased expression of multiple T cell chemokines in cancer cells, macrophages and T cells. Using the HDACi romidepsin in vivo, we observed increased chemokine expression, enhanced T cell infiltration, and T cell-dependent tumor regression. Importantly, romidepsin significantly enhanced the response to PD-1 blockade immunotherapy in multiple lung tumor models, including nearly complete rejection in two models. Combined romidepsin and PD-1 blockade also significantly enhanced activation of tumor-infiltrating T cells.
Conclusions
These results provide evidence for a novel role of HDACs in modulating T cell chemokine expression in multiple cell types. In addition, our findings indicate that pharmacological induction of T cell chemokine expression represents a conceptually novel approach for enhancing immunotherapy response. Finally, these results suggest that combination of HDAC inhibitors with PD-1 blockade represents a promising strategy for lung cancer treatment.
Introduction
Lung cancer is a leading cause of cancer-related death around the world and the 5-year survival has remained unchanged for decades. Importantly, recent studies have demonstrated the considerable potential of immunotherapy in the treatment of lung cancer and other malignancies (1, 2). In particular, blockade of CTLA-4 and PD-1 checkpoint cell surface receptors on T cells is a promising approach (3, 4). CTLA-4 and PD-1 deliver inhibitory signals following binding to their ligands CD80/86 and PD-L1/2, respectively, and blocking binding of these ligands with antibodies augments anti-tumor T cell responses (1, 2). PD-1 blockade is an especially promising approach (3, 4), yet response rates are relatively low at ~20% in lung cancer, indicating that combinatorial approaches are needed to enhance efficacy. Combinatory therapies currently being evaluated include blockade of multiple checkpoint receptors, as well as use of vaccines, radiation and agonistic mAb (1, 5, 6). There is growing interest in efficacious combinations of small molecule chemotherapeutics with immunotherapy to enhance response rates (6–8). Several traditional therapies are dependent upon immune activation, including induction of immunogenic cell death (e.g. by anthracyclines) (9), an increase in granzyme B permeability of tumor cells (e.g. by taxol) (10), and alterations in metabolite and amino acid levels within the tumor microenvironment (7, 11). In this study, we tested the hypothesis that strategies which increase expression of T cell chemokines and T cell infiltration to tumors will be especially efficacious in enhancing response to PD-1 blockade.
Previous studies have demonstrated that increased tumor expression of T cell chemokines, such as CCL5 and Cxcl10, is associated with a better response to immunotherapy (12). Furthermore, expression of T cell chemokines is strongly and positively associated with increased T cell infiltration and improved patient survival (13–15). Conversely, poor T cell infiltration in tumors can be associated with resistance to immunotherapy. Based on these findings, we tested the hypothesis that oncology agents capable of enhancing expression of T cell attracting chemokines will augment the response to immunotherapy. To this end, we screened a library of FDA-approved oncology agents specifically for their ability to induce expression of T cell chemokines. Interestingly, only a single class of agents – histone deacetylase (HDAC) inhibitors (HDACi), were found to robustly induce expression of multiple chemokines in tumor cells, tumor-infiltrating macrophages and T cells. HDACi romidepsin treatment triggered a strong anti-tumor immune response in mice and enhanced PD-1 blockade immunotherapy in multiple tumor models. These findings indicate the significant potential benefit of pairing checkpoint blockade immunotherapy with HDACi for near-term clinical use. In addition, our findings indicate that therapeutic approaches which up-regulate T cell chemokine expression represent a novel strategy for augmenting the response to immunotherapy.
Materials and Methods
Mice, cells and reagents
All mice were bred and housed in the animal facility at Moffitt Cancer Center under specific pathogen-free conditions. 129S4/SvJaeJ mice were obtained from Jackson labs (Bar Harbor, Maine). All animal experiments were performed in accordance with the Institutional Animal Care and Use Committee. Mouse LKR-13 has KRAS G12D mutation (16) while 393P and 344SQ (kindly provided by Dr. J. Kurie, MD Anderson Cancer Center) have KRAS G12D and TP53 mutations (R172H) (17). For bioluminescence imaging, LKR cells were transduced with a replication-deficient lentivirus in which luciferase expression was driven by the thymidine kinase promoter. All lung cancer cell lines were maintained in RPMI 1640 with 10% fetal bovine serum. CD11b+ cells were isolated from LKR tumors using microbeads (Miltenyi) and cultured in DMEM media. 48h later, non-adherent cells were removed and attached cells were stimulated with romidepsin. FDA-approved oncology agents were utilized from the Approved Oncology Drugs Set (97 agents) provided by the Developmental Therapeutics Program of NCI. Anti-mCD4 (Clone GK1.5), mCD8 (Clone 2.43), mIFNγ (Clone R4-6A2), and mPD-1 (Clone RMP1-14) were purchased from Bio-X-Cell, along with matching isotype controls. Romidepsin and other HDACi were purchased from Selleckchem and used at the following concentrations: vortinostat 10 μM, MS275 0.5 μM, MGCD0103 1 μM, LBH-589 0.1 μM. mIFNγ (25 ng/ml) was purchased from eBioscience and hIFNγ (100 ng/ml) from Pestka Biomedical. TAK-779 was purchased from Sigma and Collagenase D was from Roche.
High-throughput viability assay and screening
FDA-approved oncology agents were utilized from the Approved Oncology Drugs Set (97 agents) from the Developmental Therapeutics Program of NCI. Beckman-Coulter Biomek® FXP robotic liquid handling system was used for drug treatment in 96-well plates following which cell viability was determined. Briefly, LKR cells were plated in 96-well plates at a concentration of 2,000 cells/100μl of RPMI with 10% FBS. 24h later, oncology agents were individually introduced in triplicate wells in DMSO to achieve final concentrations of 10μM, 1μM, 0.1μM, and 0.01μM. A viability assay was performed 48h following drug administration using Cell Counting Kit-8 (Dojindo Laboratories) as per the manufacturer’s instructions. Absorbance for the standard curve was determined 24h after plating 2000, 1000, 500, 250, 125 and 62.5 LKR cells per 100μl. Lethal Dose 50 (LD50) values for oncology agents were calculated using “Dose-response – Inhibition: log(inhibitor) vs. normalized response” in GraphPad Prism 5 software. Agents which did not induce cell death were used at 10μM (see Table S1). LD50 of romidepsin for LKR at 48 hours was 23nM. However, the LD50 range in different lung cancer lines used here was 23–35nM. To treat different cell-lines with the same romidepsin concentration, we used it at 30nM.
RNA analysis, microarray studies, ELISA
RNA was isolated using a Qiagen RNeasy Kit, reverse transcribed and subjected to quantitative PCR analysis, as previously described (13, 18). For tumor RNA analysis, tumors were frozen in liquid nitrogen and homogenized in a Bead Beater. Tumor RNA was extracted using Qiagen RNeasy Kit. Microarray analysis was performed using the Mouse Genome 430 2.0 Arrays as described (13).
Tumor studies
Cells were harvested in logarithmic growth phase after being cultured for less than 2 weeks, washed once in injection medium (phenol-free DMEM supplemented with 2% FBS) and counted. 1×106 cells were injected s.c. and tumors were monitored for growth by measurements 2–3 times per week. The tumor volume was determined as length x length x width/2. Romidepsin was injected i.p. (2 mg/kg) on days 14, 16 and 18 after tumor inoculation. Anti-PD-1 was injected i.p. (300 μg/mouse per injection) on days 15, 17 and 19 after tumor inoculation. Isotype controls were injected in control mice. Anti-CD4 and anti-CD8 (300μg/mouse) were injected i.p. as indicated in Fig. S3. TAK-779 (150 μg/mouse) or anti-IFNγ (200 μg/mouse) was injected on day 12 and then twice a week. Mice were sacrificed when s.c. tumors reached a diameter of 20mm or when they showed signs of morbidity. Relative tumor size between treatment groups was analyzed using the t test with Welch’s correction. To determine presence of infiltrating T cells, tumors were chopped using forceps and scalpels, digested in the Collagenase D buffer with 2mg/ml Collagenase D at 37°C for 45–75min, passed through 70μm strainer and then subjected to FACS analysis as indicated in figures. In the orthotopic model, 50,000 tumor cells were injected percutaneously into the left lateral thorax in mice anesthetized with sodium pentobarbital (50 mg/kg body weight). For bioluminescence imaging (BLI) in the orthotopic model, the IVIS Imaging system was used as previously described (19). A conditional mutant KRASG12D autochthonous knock-in mouse model of lung cancer (20) was obtained from Jackson Laboratories, Bar Harbor, ME. At ~6 weeks of age, KRASG12D mice were injected with 5×106 PFU of adenovirus expressing CRE (Ad-CRE) through the intra-tracheal (i.t.) route. Pre-treatment tumor volume was determined by MRI to non-invasively monitor and assess tumor volumes longitudinally starting at 3 months after Ad-CRE injection. 2 rounds of romidepsin+anti-PD-1 treatment, as described in s.c. model, were given immediately and 2 weeks after determining pre-treatment tumor volumes. Post-treatment MRI was performed 4 weeks after pre-treatment MRI. These studies were performed in the Moffitt Small Animal Imaging Laboratory (SAIL) Core facility using a 7-T horizontal magnet (ASR 310, Agilent Technologies).
MRI Studies
Mice were placed in an induction chamber and anesthetized with 2% isoflurane for transfer onto a mouse cradle and maintained under anesthesia. A respiration pad was used for monitoring respiration rate, where a steady state breathing rate of 50–60 breathes per minute was achieved. A fiber optic rectal thermometer was used to monitor the temperature, and a core body temperature of 37 ± 1 °C was sustained. The MRI experiments were done on a 7 Tesla Agilent ASR 310 equipped with nested 205/120/HDS gradient insert in a bore size of 310 mm. Two RF coils, a 35-mm Litzcage coil (Doty Scientific, Inc.) and a 24-mm Litzcage coil (Doty Scientific, Inc), were used depending on the sizes and weights of the mice. Coronal multislice T2-weighted fast spin echo images were acquired with TE = 30.05 ms, TR = 1497.52 ms, field of view of 90 × 40 mm2, and, 20 slices of 1.2 mm thickness and a data matrix of 256 × 128 × 20. Rather than using respiratory gating, additional images were acquired to offset the effects of motion (32 averages). These images were acquired within 13 minutes. To quantify the tumor burden within the lungs, T2-weighted images were used to manually draw regions of interest with the Image Processing Toolbox in MATLAB. These were done on a slice-by-slice basis, and care was taken to avoid the heart, blood vessels, and the mediastinum. Tumors were segmented using Otsu multi-thresholding, and total tumor volume was determined by summing those lesions for all slices within the total multislice volume of interest. This was an iterative process, and additional T1-weighted images, and multislice maximum intensity projections were used to discriminate vessel from lesion.
ELISPOT
ELISPOT was used to detect IFNγ produced by CD8 and CD4 T cells as described (21). Mouse tumor cells were processed as described previously (22) and subjected to the magnetic bead separation for isolating CD8 T and CD4 T cells according to manufacturer’s recommendations (Miltenyi). Next, 4×105/well CD8 or CD4 T cells and 1×105/well of 5000 rads irradiated tumor cells were plated in triplicate wells and incubated in 96-well plates at 37°C for 24h. LKR cells were stimulated with IFNγ to increase MHC expression. T cells were also cultured alone or with Concavalin A as negative and positive controls, respectively. Plates were washed 6 times with PBS + 0.05% Tween 20 and 100 μl/well of biotinylated anti-IFNγ detecting antibody (eBioscience, Cat No. 13-7312-85) diluted to 1 μg/ml in PBS + 0.05% Tween 20 was added. Avidin-HRP (BD Biosciences, Cat No. 554058) was used as detection reagent. Spot counting was done with an AID ELISPOT Reader System (Autoimmun Diagnostika GmbH, Strassberg, Germany).
Flow cytometric analysis
Cells were incubated for 5 minutes at room temperature with Fc block, and DAPI was added prior to analysis to assess viability. Flow cytometric analysis was performed on an LSR II cytometer (BD Biosciences). Data were acquired using CellQuest software (BD Biosciences) and analyzed using FlowJo software (Tree Star). For tumor infiltrating T cells, cells were gated on strict forward and side scatter parameters to ensure single cell analysis. Additionally, the DAPI- population was used for viable cells. Finally, cells were assessed for CD3 and CD4 or CD8 expression. The FACS antibodies used were: APC anti-mouse MHC Class I (H-2Kb) (Cat No. 17-5958-82) and PE-Cyanine 7 anti-Mouse CD45 (Cat No. 25-0451-82) were purchased from eBioscience, PE CD274 (B7-H1, PD-L1) anti-mouse mAb (clone MIH5) (Cat No. A14764) was from Life Technologies, Biotin anti-mouse CD95 (Cat No. 554256), anti-mouse CD16/CD32 (Mouse BD Fc Block™) (Cat No. 553142) PE anti-mouse CD3 (Cat No. 553063), FITC anti-mouse CD4 (Cat No. 553729) and PerCP-Cy5.5 anti-mouse CD8 (Cat No. 551162), were from BD Biosciences. Cell culture supernatants were tested for presence of IFNγ using a CBA assay (BD Biosciences).
Statistical Analysis
Statistical analysis was performed using 2-tailed Student’s t test, Student’s t test with Welch’s correction, and Fisher’s exact test. GraphPad Prism 5 software (GraphPad Software Inc.) was used with significance determined at P < 0.05.
Results
Screening of oncology drugs to identify agents with ability to induce T cell chemokine expression
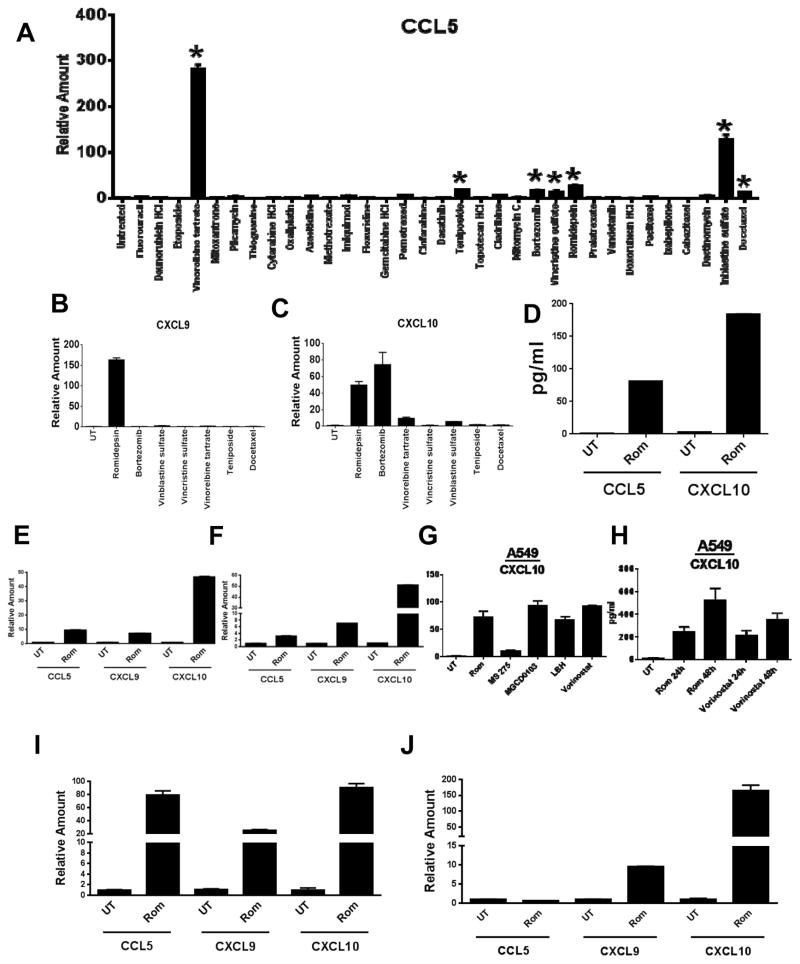
To identify agents capable of enhancing T cell chemokine expression, we utilized the Approved Oncology Drugs Set consisting of 97 agents. In addition to conventional cytotoxic chemotherapy drugs, this set also includes epigenetic agents and targeted agents such as proteasome and kinase inhibitors. Based on the rationale that driver oncogenic mutations may also impact the response to treatment, we used the KRAS mutant LKR-13 (LKR) lung cancer cell line (16) as a model system since KRAS is frequently mutated in lung adenocarcinoma. The approach to determine concentrations of different agents for equitable comparison was based on their LD50 and is described in Supplementary Materials. Expression of T cell attracting chemokine genes (Ccl5, Cxcl9 and Cxcl10) is regulated by NF-κB and IFNγ-induced pathways (23, 24); consequently, agents which potentially module activity of these pathways may induce T cell chemokine expression. Within the subset of agents that induced cytotoxicity (see Table S1), several agents (vinrelobine, teniposide, bortezomib, vincristine, romidepsin, vinblastine and docetaxel) induced Ccl5 mRNA (>10-fold) in the original screen (Fig. 1A; full list of agents is shown in Fig. S1); however, only the HDAC inhibitor (HDACi) romidepsin additionally induced strong expression of Cxcl9 and Cxcl10 at LD50 concentrations (30nM; Fig. 1B, C). For Cxcl10 in particular, this effect of romidepsin was evident across a range of different concentrations (5nM–30nm) (Fig. S2A). An additional HDACi in the Oncology Drugs Set, vorinostat, on the other hand increased Cxcl9 and Cxcl10 expression more strongly than Ccl5 expression (Fig. S2B). Focusing on romidepsin, we further confirmed that romidepsin treatment also increased CCL5 and CXCL10 secretion in LKR cells by ELISA (Fig. 1D; CXCL9 was not tested). We further validated enhanced gene expression of Ccl5, Cxcl9 and Cxcl10 in the mouse lung cancer cell line 344SQ (17), bearing mutations in KRAS and TP53, and the human A549 lung cancer line (Fig. 1E–F). Since Cxcl10 showed the highest fold induction (Fig. 1E–F), we evaluated changes in expression of this T cell chemokine in further studies. Ability to induce CXCL10 gene expression was shared at LD50 concentration dosing by several other clinically relevant HDACi MS-275, MGCD0103, LBH-589, and vorinostat in A549 cells (Fig. 1G), and with matching increases in CXCL10 protein levels demonstrated for both romidepsin and vorinostat (Fig. 1H). Since myeloid cells are known to express Ccl5, Cxcl9 and Cxcl10, we also tested romidepsin ability to induce these chemokines in Raw 264.7 macrophages. Importantly, romidepsin potently induced gene expression of all 3 chemokines (Fig. 1I). Finally, romidepsin also triggered Cxcl9 and Cxcl10 expression in macrophages isolated from LKR tumors (Fig. 1J). These results indicate that amongst oncology agents in clinical use, HDACi are powerful activators of T cell chemokine expression.
Fig. 1. HDACi induce expression of multiple T cell chemokines in mouse and human lung cancer cell lines.
(A) Ccl5 mRNA expression was determined by real-time PCR in LKR cells after treatment with a subset of oncology agents that induced cytotoxicity. Expression was normalized to ribosomal 18s RNA and is shown as fold change compared to DMSO treated LKR (set at 1). Asterisks indicate 10-fold or greater increase in expression. Samples were run in triplicate and reported as mean +/− SEM. (B) Cxcl9 and (C) Cxcl10 mRNA expression is shown following 24h treatment of LKR cells with indicated agents. Expression levels were determined as in Fig. 1A. (D) Secreted levels of CCL5 and Cxcl10 in LKR cells were determined by ELISA following romidepsin treatment (30nM) for 48h. (E–F) Ccl5, Cxcl9 and Cxcl10 mRNA expression in mouse lung cancer line 344SQ and human lung cancer line A549 was determined 24h after treatment with romidepsin (30nM). (G) Cxcl10 mRNA expression was determined in A549 following treatment with 30nM romidepsin, 500nM MS275, 1μM MGCD0103, 100nM LBH-589, and 10μM vorinostat for 24h. (H) Secreted levels of Cxcl10 in A549 were determined by ELISA following 30nM romidepsin or 10μM vorinostat treatment for indicated time periods. (I) Mouse Raw macrophages were treated with romidepsin (30nM) following which mRNA expression of Ccl5, Cxcl9 and Cxcl10 was determined. (J) CD11b+ cells were isolated from LKR tumors and cultured for 2 days following which adherent macrophages were stimulated with romidepsin (30nM) for 24h and mRNA expression of Ccl5, Cxcl9 and Cxcl10 was determined.
Anti-tumor effect of romidepsin accompanies increased T cell chemokine expression and is critically dependent on T cells
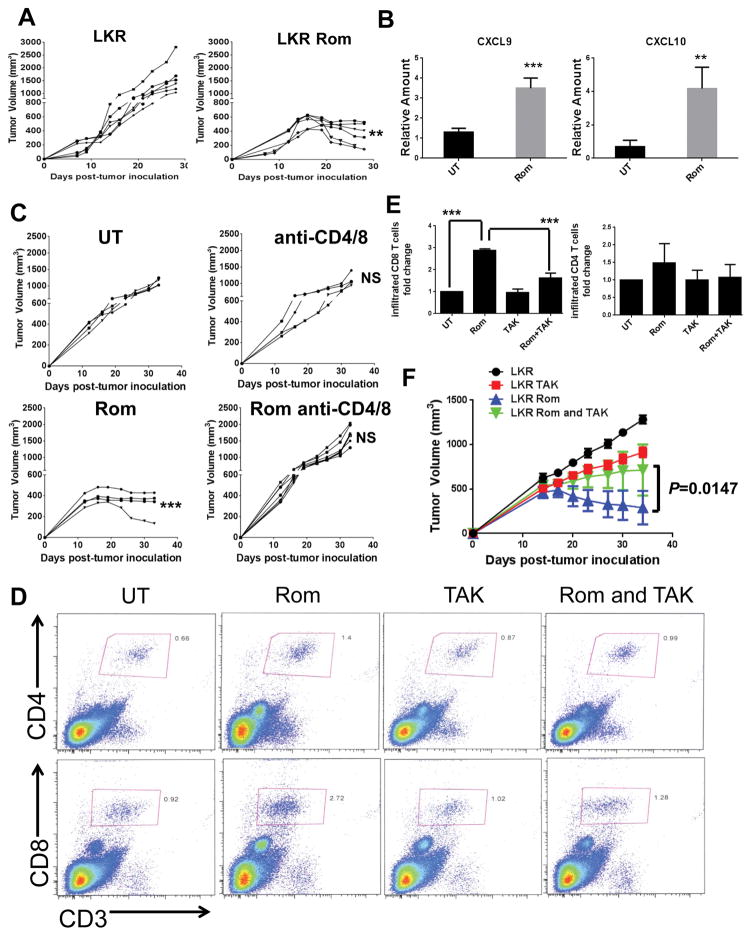
To determine the effects of romidepsin on tumor growth in vivo, we implanted LKR cells subcutaneously in syngeneic immuno-competent 129S4/SvJaeJ mice and allowed tumors to grow beyond 200 mm3 (day 12–14). Romidepsin given on days 14, 16 and 18 after tumor cell inoculation at 2 mg/kg, a dose well below the MTD of 5.6 mg/kg (25), induced a highly significant decrease in tumor growth in LKR (p=0.0024; final tumor volume) (Fig. 2A). While tumor rejection was not observed with this treatment regimen, a prolonged period of stable disease was seen (Fig. 2A). Consistent with in vitro studies, we found that whole-tumor gene expression of T cell chemokines was significantly enhanced after romidepsin treatment (Fig. 2B). To determine whether T cells were necessary for the observed response to romidepsin, mice were pre-treated with depleting mAbs against both CD4 and CD8 (Fig. S3–4). Although T cell depletion did not significantly impact the growth of LKR tumors alone, it completely reversed the anti-tumor effects of romidepsin (p<0.0001; final tumor volume) (Fig. 2C). Thus a critical mechanism of action of this HDACi likely involves enhancement of anti-tumor T cell responses. Furthermore, despite ability to induce cell death in vitro, these results indicate that romidepsin does not have a direct therapeutic effect on tumor cells.
Fig. 2. Anti-tumor effect of romidepsin accompanies increased T cell chemokine expression and is critically dependent on T cells.
(A) 129 mice were inoculated s.c. with 106 LKR cancer cells. Effect of romidepsin (Rom) treatment (2mg/kg on days 14,16,18) on tumor growth over indicated time periods is shown. Each line represents a single mouse. Significance of tumor size difference is indicated compared to untreated control mice at the last time-point. (B) Cxcl9 and Cxcl10 mRNA expression was determined in day 16 s.c LKR tumors by RT-PCR after two romidepsin injections. UT: untreated mice. Results shown represent 3–4 tumors that were individually analyzed. (C) Same as in “2A” except, where indicated, depleting antibodies to CD8 and CD4 T cells were injected. (D) Mice with day 14 tumors were untreated or treated with romidepsin on days 14 and 16 after which different group tumors (3–4 tumors) were pooled before FACS to determine CD4 (CD3+CD4+) and CD8 (CD3+CD8+) percentages in total viable cells (day 17). TAK-779 (150ug/mouse) was injected on day 12 and 15 where indicated. (E) Combined results of 3 independent experiments showing fold increase in presence of CD8 and CD4 T cells in tumors compared to untreated tumors (set at 1) after indicated treatments. Statistical significance (t-test) is shown for indicated comparisons. (F) Effect of romidepsin and TAK-779 on tumor growth over indicated time periods. Romidepsin treatment was as in “2A”. TAK-779 was injected 2 days prior to romidepsin treatment and continued for twice a week for the length of the experiment. Measurement of 5 tumors/group are indicated as mean +/− SEM. Statistical significance is indicated as *p<0.05, **p<0.01, ***p<0.001. NS: not significant.
Importantly, we observed increase in T cell infiltration in pooled sets of day 17 LKR tumors after romidepsin treatment, e.g. CD4: 0.6% to 1.4% and CD8: 0.9 to 2.7% in the experiment shown (Fig. 2D). However, combined results from 3 independent experiments showed that a significant increase in infiltration was evident in CD8 but not in CD4 T cells (Fig. 2E). Microarray studies showed that Ccl5 and Cxcl9/10 were the only T cell chemokines induced after romidepsin treatment (Table S2). To examine whether T cell recruitment was necessary for the anti-tumor effect of romidepsin, we pre-treated mice with TAK-779, an inhibitor of CCR5 and CXCR3 (26), the receptors of CCL5 and Cxcl9/10/11, respectively. TAK-779 prevented the romidepsin-induced increase in T cell density (CD4: 1.4% to 0.9% and CD8: 2.7% to 1.2%), but did not reduce steady state T cell numbers (CD4: 0.6% to 0.8% and CD8: 0.9 to 1.0%) (Fig. 2D). As with a significant increase in CD8 T cell infiltration after romidepsin treatment, a significant decrease in infiltration after TAK-779 was evident for CD8 but not CD4 T cells in combined results from 3 independent experiments (Fig. 2E). Although TAK-779 did slightly reduce LKR tumor growth when used alone, it also abrogated the effect of romidepsin treatment, indicating a crucial role for the CCR5 and/or CXCR3 receptors and their respective chemokines (Fig. 2F). Collectively, these findings suggest a mechanism whereby T cell chemokine expression induced by romidepsin promotes T cell recruitment, which in turn drives an anti-tumor response and promotes disease stabilization.
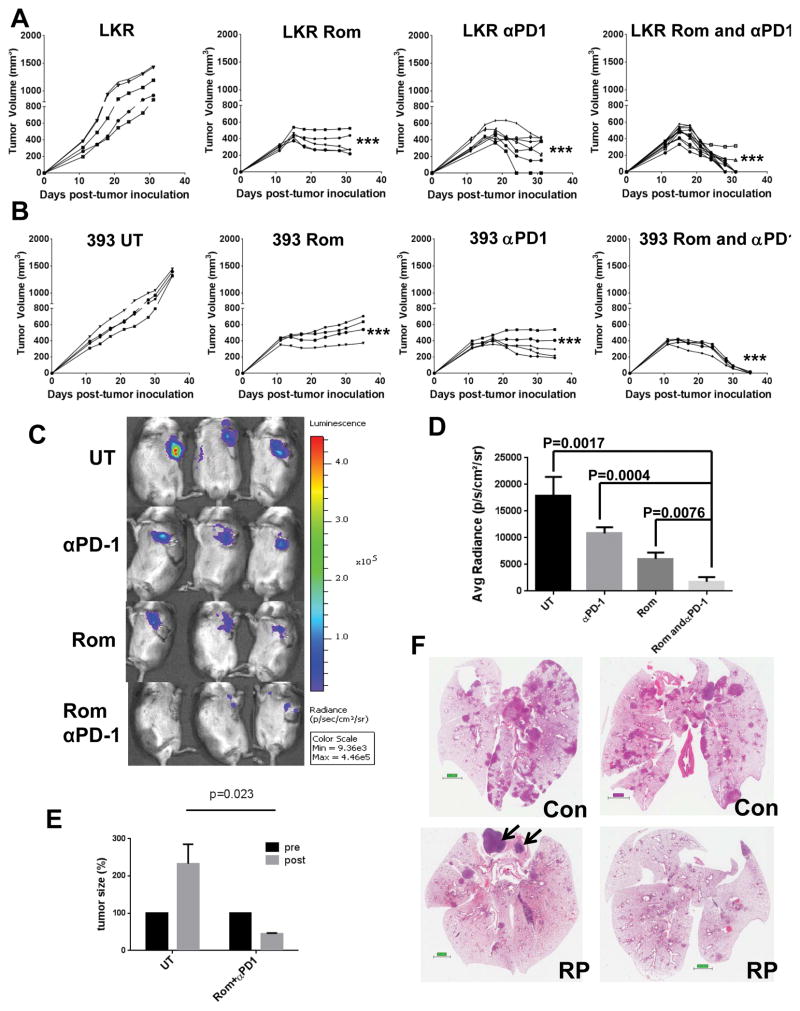
Romidepsin enhances response to anti-PD-1 immunotherapy leading to tumor rejection
The response to PD-1 blockade has been associated with interrelated parameters of T cell infiltration, an Th1/IFNγ signature, and tumor PD-L1 expression (4, 27–29), suggesting therapies that augment T cell infiltration or effector function could synergize with checkpoint blockade. We first assessed PD-L1 levels in mouse LKR, 393P and 344SQ lung cells (16, 17) in vitro with or without 24hrs of exposure to romidepsin or IFNγ. Importantly romidepsin treatment increased PD-L1 levels although this did not compare in magnitude to the increase observed with IFNγ (Fig. S5). We next determined whether LKR tumors were responsive to anti-PD-1 therapy by injecting anti-PD-1 on days 15, 17 and 19 after tumor inoculation. Tumor growth was significantly reduced by anti-PD-1 treatment, but complete rejection was seldom observed over the 30 day period (1/7 mice) (Fig. 3A). While occasional tumor rejection was seen over ~30 days, longer-term follow of 47 days in separate experiments showed that neither romidepsin nor anti-PD-1 caused tumor rejection beyond 30 days (Fig. S6A). Instead, for both romidepsin and anti-PD-1 treatments, robust tumor growth resumed after a period of stasis (Fig. S6A). To evaluate synergism between romidepsin and anti-PD-1 therapy, romidepsin was administered on days 14, 16 and 18, with anti-PD-1 administered on each subsequent day. Combined anti-PD-1 and romidepsin significantly reduced tumor growth compared to individual treatments with romidepsin (p=0.0008) or anti-PD-1 (p=0.0041) (Fig. 3A) and rejection was noted in 9/11 tumors (Fisher Exact Test, p<0.0001) (Fig. S6B). Furthermore, no regrowth of rejected tumors was observed in anti-PD-1 and romidepsin treated mice (Fig. S6C). We also evaluated combination therapy with romidepsin and anti-PD-1 in the 344SQ and 393P tumor models. Tumor rejection was not seen with 344SQ tumors, but combined anti-PD-1 and romidepsin treatment significantly delayed tumor growth compared to either individual treatment (Fig. S7). A more pronounced response was observed with 393P tumors, as complete tumor rejections were observed with combination therapy in 5/5 animals, but in none of the tumor bearing animals treated with individual agents (Fig. 3B). The striking difference in response in 344SQ and 393P tumor models is however not due to differences in oncogene/tumor-suppressor mutations as they both harbor KRAS and TP53 mutations (17).
Fig. 3. Romidepsin enhances response to anti-PD-1 immunotherapy leading to tumor rejection.
(A) 129 mice were inoculated and treated with romidepsin as in “2A” with or without 300μg/mouse anti-PD-1 antibody on days 15,17,19 as indicated. Significance of tumor size difference is indicated compared to untreated control mice at the last time-point. (B) Same as in “3A” except 393P (393) tumors were studied. (C) 50,000 LKR cells were injected in mouse thorax. Treatment regimen was as in “A” except it was started on day 6. BLI was performed 14 days after tumor cell injection. (D) Signal of 3 mice/group is shown as mean +/− SEM with significance of differences in groups indicated by p-values. (E) Effect of combined romidepsin and anti-PD-1 treatment in a conditional mutant KRASG12D autochthonous model of lung cancer. MRI was used to determine total baseline tumor volume (Pre), followed by the initiation of romidepsin and anti-PD-1 treatment (Post). Change in tumor volume (baseline set at 100%) after treatment (n=3) or no treatment (UT, n=3) is indicated over a 1 month period. (F) H&E staining of two untreated and treated lung specimens from “E”. Bar=2mm. Arrows indicate contaminating lymphoid tissue. Statistical significance is indicated by p-values or as *p<0.05, **p<0.01, ***p<0.001. NS: not significant.
Luciferease expressing LKR cells were also injected in the lung as an orthotopic tumor model. As with s.c tumors, the greatest anti-response was seen after combined anti-PD-1 and romidepsin treatment as determined by bioluminescence imaging (BLI) (Fig. 3C–D). Finally, we evaluated the effect of combined romidepsin and anti-PD-1 treatment in a conditional mutant KRASG12D autochthonous knock-in mouse model of lung cancer (20). Tumor growth was initiated by intra-tracheal injection of replication-deficient adenovirus expressing CRE recombinase, as previously described (20). 3 months later, MRI was used to determine total baseline tumor volume, followed by 2 rounds of treatment with 3 doses each of romidepsin and anti-PD-1 treatment. Tumor volume evaluated 1 month after the first MRI increased more than 2-fold in untreated mice (Fig. 3E). In mice treated with romidepsin and anti-PD-1, tumor volume was significantly reduced by approximately 50% (Fig. 3E). As expected, H&E staining of untreated lung specimens showed significantly larger tumor burden than the lungs of treated mice (Fig. 3F). Together, these findings provide strong rationale for evaluating combined romidepsin and anti-PD-1 mAb therapy in the clinic.
Romidepsin synergizes with IFNγ to enhance tumor immunogenicity
Microarray studies showed that many of the romidepsin induced genes were known targets of IFNγ (e.g. T cell chemokines, MHC and FAS) (Table S2). Interestingly, expression of the key IFNγ-induced transcription factor STAT1 was also increased by romidepsin (Table S2), potentially linking effects of this HDACi to IFNγ signaling. Using additional microarray studies, we tested the possibility that romidepsin may impact IFNγ-induced gene expression. Interestingly, we found that expression of Ccl5 and Cxcl9/10 was synergistically increased after romidepsin and IFNγ treatment (Fig. S8A). In addition, as with romidepsin alone treatment (Table S2), we also found increase in expression of STAT1 (3 out of 45 up-regulated probe sets). Interestingly, MHC and FAS gene expression was increased after romidepsin treatment (Table S2) but which was not further enhanced by IFNγ. These results indicate that combined romidepsin and IFNγ treatment can potentiate expression of a subset of genes regulated by these agents, including T cell chemokines and STAT1. We validated our microarray data demonstrating increased expression of Cxcl10 in LKR cells by real time PCR (Fig. S8B). Synergism between romidepsin and IFNγ was also pronounced in 393P cells (Fig. S8C).
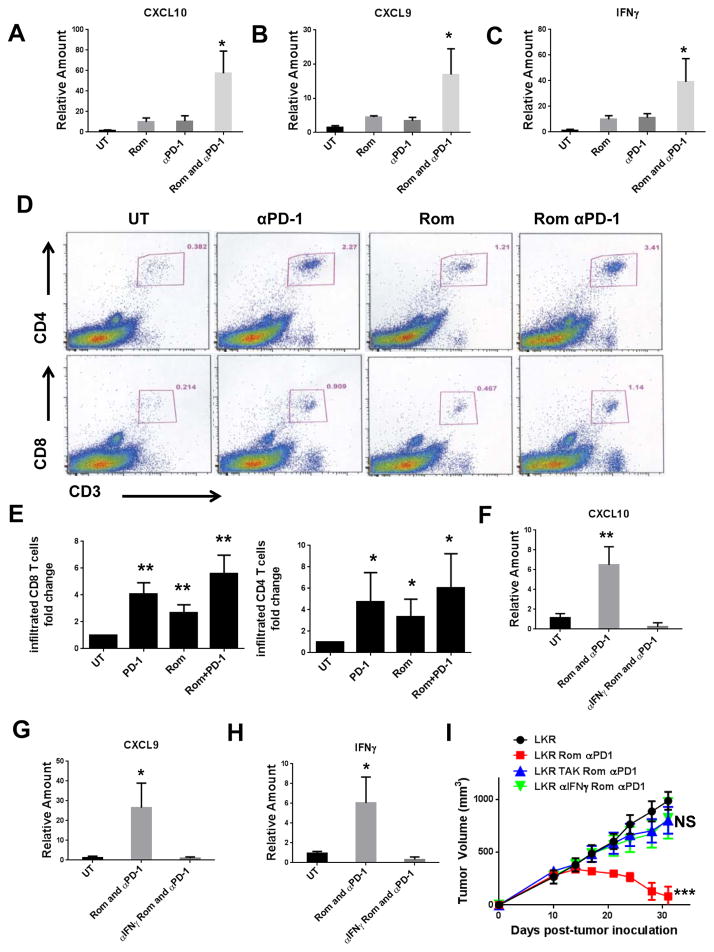
Previous studies have demonstrated that anti-PD-1 enhances T cell chemokine expression and T cell infiltration, and that this effect is mediated by IFNγ production (30). Based upon the ability of IFNγ to synergistically promote chemokine expression with romidepsin in vitro, we postulated that IFNγ was also a central regulator of the anti-tumor response seen with romidepsin and anti-PD-1 in vivo. Consistent with this interpretation, combination therapy in mice bearing LKR tumors increased tumor expression of Cxcl10 and Cxcl9 by 50-fold and 15-fold, respectively (Fig. 4A–B). This compared to only a 10-fold increase in tumor expression of Cxcl10 and a 5-fold increase in Cxcl9 in the single agent control groups (Fig. 4A–B). The chemokine expression pattern was closely matched by increased expression of IFNγ within the tumors of mice treated with both therapeutic agents (Fig. 4C). Chemokine expression levels correlated with T cell density, with the highest numbers of CD4 and CD8 T cells present within the tumors of animals treated with combination therapy (Fig. 4D–E).
Fig. 4. Crucial requirement for IFNγ in romidepsin and anti-PD-1 induced tumor rejection.
(A–C) Cxcl10, Cxcl9 and IFNγ mRNA expression was determined in s.c LKR tumors by RT-PCR after two romidepsin (Rom) and/or anti-PD-1 antibody injections. Results shown represent 3–4 tumors that were individually analyzed. Significance is indicated compared to untreated control mice. (D) 129 mice with day 14 tumors were untreated (UT) or treated with romidepsin on days 14 and 16 and/or anti-PD-1 antibody on days 15 and 17 after which different group tumors were pooled before FACS to determine CD4 (CD3+CD4+) and CD8 (CD3+CD8+) percentages in total viable cells (day 19). (E) Combined results of 3 independent experiments showing fold increase in presence of CD8 and CD4 T cells in tumors compared to untreated tumors (set at 1) after indicated treatments. Statistical significance (t-test) is shown for indicated comparisons. (F–H) Same as 4A-C except anti-IFNγ antibody (200ug/mouse) was injected 2 days prior to the first treatment. (I) Tumor growth showing the effect of TAK-779 (150ug/mouse) and IFNγ antibody on tumor bearing mice treated with romidepsin and anti-PD-1 antibody. TAK-779 or IFNγ antibody was injected 2 days prior to romidepsin treatment and continued for twice a week for the length of the experiment. Measurement of 5 tumors/group are indicated as mean +/− SEM. Significance of tumor size difference is indicated compared to untreated control mice at the last time-point. “ns” indicates not significant.
Crucial requirement for IFNγ in romidepsin and anti-PD-1 induced tumor rejection
We next determined whether IFNγ was functionally required to promote chemokine expression and mediate the anti-tumor effects of combination therapy. To this end, we used an anti-IFNγ antibody to neutralize endogenous IFNγ starting 2 days before initiation of romidepsin/anti-PD-1 treatment. IFNγ neutralization completely abrogated the induction of Cxcl9/Cxcl10 expression within tumors after romidepsin and anti-PD-1 treatment (Fig. 4F–G). Furthermore, neutralization of IFNγ also substantially reduced T cell infiltration (Fig. S9). IFNγ neutralization also blocked the induction of IFNγ gene expression (Fig. 4H), consistent with a feed-forward signaling pathway where production of IFNγ by T cells enhances tumor cell immunogenicity (31), in turn further enhancing T cell recruitment and function. Finally, we found that IFNγ neutralization ablated the effects of combination therapy, with tumor growth comparable to untreated controls (Fig. 4I). As with reversion of romidepsin therapy alone (Fig. 2F), administration of the CCR5/CXCR3 inhibitor TAK-779 also prevented a response to combination therapy (Fig. 4I). Thus, romidepsin and anti-PD-1 treatments synergize by promoting a chemokine-IFNγ positive feedback loop through tumor cell and T cell intermediaries.
Romidepsin synergizes with anti-PD-1 to enhance function of tumor infiltrating T cells
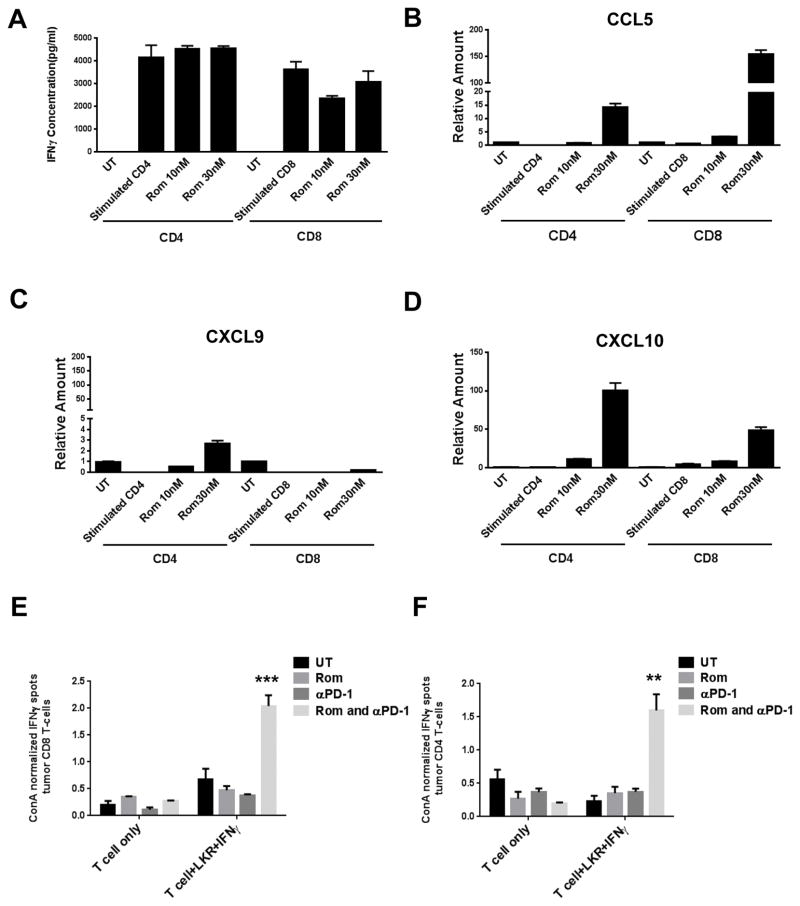
We next sought to determine potential direct effect of romidepsin on T cells in vitro and in vivo. First, in T cells stimulated with TCR/CD28 engagement, we did not see any significant impact of romidepsin on IFNγ secretion (Fig. 5A). Previous studies suggest that T cells can also express CCL5 and CXCL10 (32, 33). We therefore next tested the interesting possibility that romidepsin may also induce expression of these chemokines in T cells. Indeed, a substantial increase in expression of Ccl5 and Cxcl10 was seen after romidepsin treatment of both CD4 and CD8 T cells (Fig. 5B–D). Therefore, in addition to tumor cells and macrophages, romidepsin can also enhance expression of chemokines in T cells. Finally, we determined whether romidepsin also enhances T cell functionality in vivo. Importantly, the frequency of tumor CD8 and CD4 cells that produce IFNγ ex vivo in response to LKR cells in an ELISPOT assay was significantly increased by combination therapy (Fig. 5E–F). This measure of T cell functionality was not increased by either romidepsin or anti-PD-1 therapy alone, again highlighting the synergistic nature of the combination. Therefore, in addition to promoting T cell infiltration, romidepsin can also enhance recruited T cell function in manner that synergizes with PD-1 blockade.
Fig. 5. Romidepsin synergizes with anti-PD-1 to enhance function of tumor infiltrating T cells.
(A) Purified CD4 and CD8 T cells were stimulated with anti-CD3/CD28 (2μg/ml) for 48h followed by addition of romidepsin at indicated concentrations for another 24h. Cell culture supernatants were tested for presence of IFNγ using a CBA assay. (B–D) Purified CD4 and CD8 T cells were stimulated as in “A” following which mRNA expression of Ccl5, Cxcl9 and Cxcl10 was determined. (E–F) IFNγ ELISPOT of tumor CD8 and CD4 T cells cultured alone, with ConA treatment, or with LKR as indicated. T cells, per group, were pooled and samples were run in triplicate (mean± SEM). Results were normalized to ConA treatment in the same sample T cells. Significance is indicated for comparison of romidepsin+anti-PD-1 treated vs. untreated control mice.
Discussion
Recent clinical studies have demonstrated the considerable potential of immunotherapy in cancer treatment. However, even with combinatorial approaches with anti-CTLA-4 and anti-PD-1, there remain a significant percentage of patients that do not derive a clinical benefit (34). We hypothesized that oncology agents that enhance T cell recruitment would increase response to immunotherapy. We screened a library of FDA-approved oncology drugs to determine ability to induce expression of Ccl5, Cxcl9 and Cxcl10 and found that only a single agent class, HDACi, was capable of inducing expression of these chemokines. Most importantly, the HDACi romidepsin induced a strong T cell dependent anti-tumor response and combinatory treatment with anti-PD-1 induced tumor regression or rejection across multiple lung tumor models. Since multiple HDACi and PD-1 blockade agents (Pembrolizumab and Nivolumab) are now FDA-approved, combinatory therapy with these two agent classes may represent a promising approach for lung cancer treatment in the near-term.
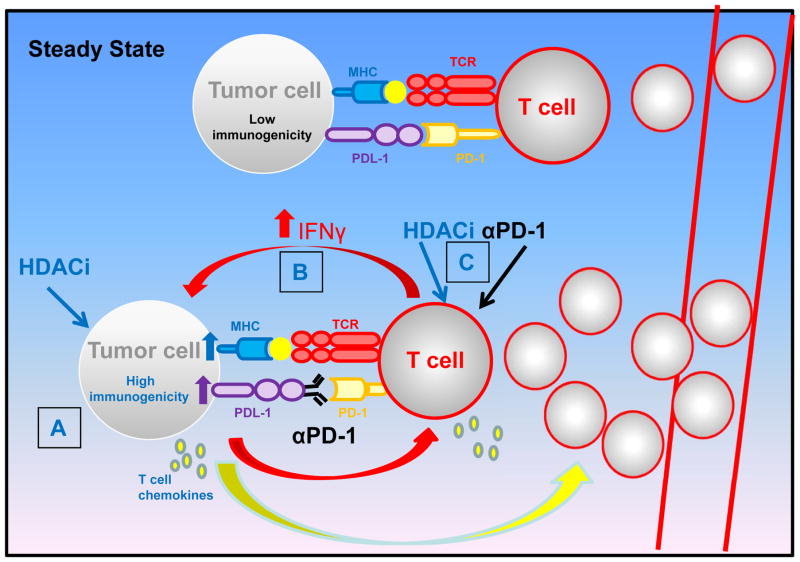
As suggested by recent clinical results (27), the response to anti-PD-1 is restricted by poor T cell infiltration into tumors. We found that HDACi therapy alone increases tumor expression of Cxcl9 and Cxcl10, promoting T cell recruitment and a period of tumor stasis (see Fig. 6). The increase in T cell recruitment was typically more significant for CD8 T cells, the subset strongly implicated in benefit from PD-1 blockade therapy (27). Chemokine expression may depend on multiple cell types as our results indicate romidepsin ability to induce expression in tumor cells, macrophages and T cells. However, HDACi treatment also upregulated PD-L1 expression, which may limit T cell functionality (Fig. 6) (35). On the other hand, combination therapy unleashes an IFNγ-dependent response to promote maximal T cell chemokine expression and T cell recruitment without sensitization of T cells to the upregulation of PD-L1 on tumor cells (Fig. 6). Limiting CCR5/CXCR3-dependent recruitment of T cells or neutralizing IFNγ prevents response to combination therapy, implicating both steps as critical for therapeutic efficacy. We utilized multiple tumor models (LKR, 393P and 344SQ) to show greater efficacy of combined treatment vs. individual treatments. In the KRAS autochthonous model, however, only the effect of combined romidepsin and anti-PD-1 treatment was studied. Additional studies will therefore be required to determine whether combined treatment is also more efficacious in this model compared to single treatments. Interestingly, recent studies showed reduced immune surveillance in lung adenocarcinoma with mutations in the STK11/LKB1 tumor suppressor (36, 37). The impact of therapeutic regimens identified here on treatment response of KRAS/STK11 as well as the widely used KRAS/TP53 autochthonous model (38) will therefore also be important to determine.
Fig. 6. Model of mechanism of synergy between HDACi and anti-PD-1 treatment.
In the steady-state, T cell function is curtailed through multiple immunosuppressive mechanisms including PD-1. Additionally, tumor cells have low immunogenicity, including minimal MHC and T cell chemokine expression, or T cell infiltration. In the illustrated treatment scenario with HDACi and anti-PD-1, multiple mechanisms are unleashed that contribute towards tumor eradication. (A) HDACi induce T cell chemokine expression in multiple cell types, including tumor cells and T cells, resulting in enhanced T cell recruitment. (B) When treated with PD-1 blockade and HDACi, anti-PD-1 enhances IFNγ expression in T cells and tumor cells become more responsive to IFNγ through HDACi mediated effects. This results in high MHC expression and the highest T cell chemokine expression, which serves to recruit additional T cells. (C) Finally, both anti-PD-1 and HDACi may directly and synergistically enhance T cell function.
Interestingly, we found that individual depletion of CD4 or CD8 T cells was sufficient to reverse the anti-tumor effect of romidepsin (Fig. S10). In addition to increasing infiltration, an important finding was the increase in tumor-infiltrating CD4 and CD8 function after combination therapy (Fig. 5E–F). This increase may be a consequence of romidepsin-induced increase in tumor cell immunogenicity (e.g. through upregulation of MHC expression), coupled with direct augmentation of T cell function by anti-PD-1 and potentially by romidepsin (Fig. 6). Interestingly, previous studies indicate that in addition to promoting T cell recruitment, Cxcl10 also enhances effector T cell function (33, 39). Therefore, another interesting possibility is that romidepsin triggered Cxcl10 expression synergizes with anti-PD-1 to enhance T cell function. Further studies will be required to determine specifically how HDACi ± anti-PD-1 modulate T cell function. An important related issue is the effect of in vivo HDAC dose. While we used a dose below the MTD of romidepsin, it is possible that higher dosing may adversely impact function of T cells or other cell-types crucial for the anti-tumor response and thereby reduce therapeutic efficacy. The HDACi dose capable of inducing beneficial epigenetic changes and gene expression but without cytotoxicity towards T cells will also be important to determine for clinical use of these agents when combined with immunotherapeutics. HDACi treatment has previously been reported to induce systemic MDSC depletion leading enhancement of T cell responses induced by checkpoint blockade (40). However, we found that romidepsin treatment of mice did not impact MDSC numbers (Fig. S11), suggesting that effects of HDACi treatment observed here are not due to MDSC depletion.
Histone modification by histone acetyltransferases (HATs) is typically associated with increased gene expression while removal of acetyl groups by HDACs represses gene expression. Although overall NF-κB activity was crucial for romidepsin-induced T cell chemokine expression, romidepsin did not enhance nuclear translocation of NF-κB (data not shown). In contrast, romidepsin increased STAT1 mRNA and further enhanced STAT1 protein levels after IFNγ treatment (Fig. S12). A likely mechanism of synergy may therefore involve IFNγ activation of STAT1 coupled with romidepsin-induced histone modifications to maximize gene expression. It is also likely that genes uniquely regulated by romidepsin or IFNγ act in concert to promote anti-tumor responses. Interestingly, it was recently shown that romidepsin decreased levels of β-catenin by upregulating expression of its inhibitor SFRP1 (41). In addition, β-catenin signaling was recently shown to suppress checkpoint immunotherapy response (42). An interesting possibility that requires careful examination is whether suppression of β-catenin signaling is an additional mechanism by which romidepsin promotes the anti-PD-1 response.
While the present study focused on pan-HDACi, we also tested HDACi specific for HDAC1+2, HDAC3, HDAC4, HDAC6 and HDAC8. However, we did not observe induction of Cxcl9/10 T cell chemokine expression as was evident after romidepsin or vorinostat treatment. Additional studies will be required to determine whether these genes are specifically regulated by an HDAC other than the above or whether inhibition of multiple HDACs is required for induction of expression. In an important recent study, it was shown that enhancer of zeste homologue 2 (EZH2)-mediated histone H3 trimethylation (H3K27me3) and DNA methyltransferase 1 (DNMT1)-mediated DNA methylation repress ovarian tumor cell expression of Cxcl9 and Cxcl10 (43). Importantly, inhibitors of EZH2, such as DZNep or GSK126, and DNMT1 inhibitor 5-AZA-dC enhance chemokine expression to promote effector T cell trafficking to the tumor and the response to PD-L1 blockade immunotherapy (43). This study, together with our findings, indicate that regulation of chemokine expression is subject to control by multiple and distinct epigenetic mechanisms. Modulation of tumor immunogenicity by drugs that target epigenetic mechanisms may therefore represent a promising area for translational research and clinical intervention (44).
HDACi are approved for treatment of certain hematologic malignancies, but have failed to demonstrate efficacy in solid tumors. Interestingly, the combination of the HDACi entinostat with 5-AZA-dC has shown benefit in lung cancer treatment, highlighting the potential for HDACi to augment response to other epigenetic therapies (45). Importantly, supportive of our findings, a recent study showed that the HDACi vorinostat increased CD8 T cell infiltration in human lung tumors (46). In the pre-clinical setting, there is also evidence of immune modulation by HDACi (47–50). Based on the novel findings reported here, we strongly believe that the combination of HDACi with immunotherapy represents a powerful approach for cancer treatment. Notably, several clinical trials employing this combinatory approach are now underway, including one at our institution in NSCLC patients.
Supplementary Material
Statement of Translational Relevance.
Insufficient tumor-infiltrating T cells is recognized as a major resistance mechanism to immunotherapy. Here we tested the hypothesis that strategies which increase expression of T cell chemokines and T cell infiltration to tumors will be efficacious in enhancing immunotherapy response. We utilized a screening approach to identify FDA-approved oncology agents and discovered a novel ability of HDAC inhibitors (HDACi) to induce expression of T cell chemokines. HDAC inhibitors strongly augmented response to PD-1 immunotherapy in multiple lung tumor models. Our findings indicate that approaches utilizing induction of T cell chemokine expression represent a conceptually novel strategy for enhancing immunotherapy response. The combination of HDACi and PD-1 blockade will be tested in several clinical trials, including a trial in NSCLC at our institution. We believe the findings described in this study can provide a framework for mechanistic assessment of the impact of this combination on patient tumors.
Acknowledgments
We thank Dr. Kenyon Daniel and Nan Sun (Chemical Biology core) for help setting up chemotherapy agent screening and Dr. Lu Chen for help with statistical analysis. We thank Dr. J. Kurie (M.D. Anderson Cancer Center) for providing 393P and 344SQ cells. We also acknowledge help provided by Flow Cytometry, Molecular Genomics, Pathology and Comparative Medicine core facilities at the Moffitt Cancer Center. This work was supported by lung cancer SPORE P50 CA119997, funds from the Moffitt Cancer Center Lung Cancer Center of Excellence, National Natural Science Foundation of China (Grant no. 81472183), and NIH R01 AI0802685.
Footnotes
The authors disclose no potential conflicts of interest.
References
- 1.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–64. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma P, Allison JP. Immune checkpoint targeting in cancer therapy: toward combination strategies with curative potential. Cell. 2015;161:205–14. doi: 10.1016/j.cell.2015.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. The New England journal of medicine. 2012;366:2455–65. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. The New England journal of medicine. 2012;366:2443–54. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Twyman-Saint Victor C, Rech AJ, Maity A, Rengan R, Pauken KE, Stelekati E, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature. 2015;520:373–7. doi: 10.1038/nature14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melero I, Berman DM, Aznar MA, Korman AJ, Perez Gracia JL, Haanen J. Evolving synergistic combinations of targeted immunotherapies to combat cancer. Nat Rev Cancer. 2015;15:457–72. doi: 10.1038/nrc3973. [DOI] [PubMed] [Google Scholar]
- 7.Adams JL, Smothers J, Srinivasan R, Hoos A. Big opportunities for small molecules in immuno-oncology. Nature reviews Drug discovery. 2015 doi: 10.1038/nrd4596. [DOI] [PubMed] [Google Scholar]
- 8.Zitvogel L, Galluzzi L, Smyth MJ, Kroemer G. Mechanism of action of conventional and targeted anticancer therapies: reinstating immunosurveillance. Immunity. 2013;39:74–88. doi: 10.1016/j.immuni.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Ma Y, Adjemian S, Mattarollo SR, Yamazaki T, Aymeric L, Yang H, et al. Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity. 2013;38:729–41. doi: 10.1016/j.immuni.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Ramakrishnan R, Assudani D, Nagaraj S, Hunter T, Cho HI, Antonia S, et al. Chemotherapy enhances tumor cell susceptibility to CTL-mediated killing during cancer immunotherapy in mice. J Clin Invest. 2010;120:1111–24. doi: 10.1172/JCI40269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho PC, Bihuniak JD, Macintyre AN, Staron M, Liu X, Amezquita R, et al. Phosphoenolpyruvate Is a Metabolic Checkpoint of Anti-tumor T Cell Responses. Cell. 2015;162:1217–28. doi: 10.1016/j.cell.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ji RR, Chasalow SD, Wang L, Hamid O, Schmidt H, Cogswell J, et al. An immune-active tumor microenvironment favors clinical response to ipilimumab. Cancer Immunol Immunother. 2012;61:1019–31. doi: 10.1007/s00262-011-1172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hopewell EL, Zhao W, Fulp WJ, Bronk CC, Lopez AS, Massengill M, et al. Lung tumor NF-kappaB signaling promotes T cell-mediated immune surveillance. J Clin Invest. 2013;123:2509–22. doi: 10.1172/JCI67250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. The New England journal of medicine. 2003;348:203–13. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 15.Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. The New England journal of medicine. 2005;353:2654–66. doi: 10.1056/NEJMoa051424. [DOI] [PubMed] [Google Scholar]
- 16.DuPage M, Cheung AF, Mazumdar C, Winslow MM, Bronson R, Schmidt LM, et al. Endogenous T cell responses to antigens expressed in lung adenocarcinomas delay malignant tumor progression. Cancer cell. 2011;19:72–85. doi: 10.1016/j.ccr.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gibbons DL, Lin W, Creighton CJ, Rizvi ZH, Gregory PA, Goodall GJ, et al. Contextual extracellular cues promote tumor cell EMT and metastasis by regulating miR-200 family expression. Genes Dev. 2009;23:2140–51. doi: 10.1101/gad.1820209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang J, Wang X, Hussain S, Zheng Y, Sanjabi S, Ouaaz F, et al. Distinct roles of different NF-kappa B subunits in regulating inflammatory and T cell stimulatory gene expression in dendritic cells. J Immunol. 2007;178:6777–88. doi: 10.4049/jimmunol.178.11.6777. [DOI] [PubMed] [Google Scholar]
- 19.Valenzuela JO, Iclozan C, Hossain MS, Prlic M, Hopewell E, Bronk CC, et al. PKCtheta is required for alloreactivity and GVHD but not for immune responses toward leukemia and infection in mice. J Clin Invest. 2009;119:3774–86. doi: 10.1172/JCI39692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson EL, Willis N, Mercer K, Bronson RT, Crowley D, Montoya R, et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev. 2001;15:3243–8. doi: 10.1101/gad.943001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assudani D, Cho HI, DeVito N, Bradley N, Celis E. In vivo expansion, persistence, and function of peptide vaccine-induced CD8 T cells occur independently of CD4 T cells. Cancer Res. 2008;68:9892–9. doi: 10.1158/0008-5472.CAN-08-3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruffell B, Affara NI, Cottone L, Junankar S, Johansson M, DeNardo DG, et al. Cathepsin C is a tissue-specific regulator of squamous carcinogenesis. Genes Dev. 2013;27:2086–98. doi: 10.1101/gad.224899.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casola A, Henderson A, Liu T, Garofalo RP, Brasier AR. Regulation of RANTES promoter activation in alveolar epithelial cells after cytokine stimulation. American journal of physiology Lung cellular and molecular physiology. 2002;283:L1280–90. doi: 10.1152/ajplung.00162.2002. [DOI] [PubMed] [Google Scholar]
- 24.Burke SJ, Goff MR, Lu D, Proud D, Karlstad MD, Collier JJ. Synergistic expression of the CXCL10 gene in response to IL-1beta and IFN-gamma involves NF-kappaB, phosphorylation of STAT1 at Tyr701, and acetylation of histones H3 and H4. J Immunol. 2013;191:323–36. doi: 10.4049/jimmunol.1300344. [DOI] [PubMed] [Google Scholar]
- 25.Imai T, Adachi S, Nishijo K, Ohgushi M, Okada M, Yasumi T, et al. FR901228 induces tumor regression associated with induction of Fas ligand and activation of Fas signaling in human osteosarcoma cells. Oncogene. 2003;22:9231–42. doi: 10.1038/sj.onc.1207184. [DOI] [PubMed] [Google Scholar]
- 26.Breser ML, Motrich RD, Sanchez LR, Mackern-Oberti JP, Rivero VE. Expression of CXCR3 on specific T cells is essential for homing to the prostate gland in an experimental model of chronic prostatitis/chronic pelvic pain syndrome. J Immunol. 2013;190:3121–33. doi: 10.4049/jimmunol.1202482. [DOI] [PubMed] [Google Scholar]
- 27.Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–71. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Science translational medicine. 2012;4:127ra37. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–7. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peng W, Liu C, Xu C, Lou Y, Chen J, Yang Y, et al. PD-1 blockade enhances T-cell migration to tumors by elevating IFN-gamma inducible chemokines. Cancer Res. 2012;72:5209–18. doi: 10.1158/0008-5472.CAN-12-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunn GP, Koebel CM, Schreiber RD. Interferons, immunity and cancer immunoediting. Nature reviews Immunology. 2006;6:836–48. doi: 10.1038/nri1961. [DOI] [PubMed] [Google Scholar]
- 32.Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–5. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 33.Peperzak V, Veraar EA, Xiao Y, Babala N, Thiadens K, Brugmans M, et al. CD8+ T cells produce the chemokine CXCL10 in response to CD27/CD70 costimulation to promote generation of the CD8+ effector T cell pool. J Immunol. 2013;191:3025–36. doi: 10.4049/jimmunol.1202222. [DOI] [PubMed] [Google Scholar]
- 34.Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. The New England journal of medicine. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woods DM, Sodre AL, Villagra A, Sarnaik A, Sotomayor EM, Weber J. HDAC Inhibition Upregulates PD-1 Ligands in Melanoma and Augments Immunotherapy with PD-1 Blockade. Cancer immunology research. 2015;3:1375–85. doi: 10.1158/2326-6066.CIR-15-0077-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schabath MB, Welsh EA, Fulp WJ, Chen L, Teer JK, Thompson ZJ, et al. Differential association of STK11 and TP53 with KRAS mutation-associated gene expression, proliferation and immune surveillance in lung adenocarcinoma. Oncogene. 2015 doi: 10.1038/onc.2015.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skoulidis F, Byers LA, Diao L, Papadimitrakopoulou VA, Tong P, Izzo J, et al. Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer discovery. 2015;5:860–77. doi: 10.1158/2159-8290.CD-14-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen Z, Cheng K, Walton Z, Wang Y, Ebi H, Shimamura T, et al. A murine lung cancer co-clinical trial identifies genetic modifiers of therapeutic response. Nature. 2012;483:613–7. doi: 10.1038/nature10937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dufour JH, Dziejman M, Liu MT, Leung JH, Lane TE, Luster AD. IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J Immunol. 2002;168:3195–204. doi: 10.4049/jimmunol.168.7.3195. [DOI] [PubMed] [Google Scholar]
- 40.Kim K, Skora AD, Li Z, Liu Q, Tam AJ, Blosser RL, et al. Eradication of metastatic mouse cancers resistant to immune checkpoint blockade by suppression of myeloid-derived cells. Proc Natl Acad Sci U S A. 2014;111:11774–9. doi: 10.1073/pnas.1410626111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Valdez BC, Brammer JE, Li Y, Murray D, Liu Y, Hosing C, et al. Romidepsin targets multiple survival signaling pathways in malignant T cells. Blood cancer journal. 2015;5:e357. doi: 10.1038/bcj.2015.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spranger S, Bao R, Gajewski TF. Melanoma-intrinsic beta-catenin signalling prevents anti-tumour immunity. Nature. 2015;523:231–5. doi: 10.1038/nature14404. [DOI] [PubMed] [Google Scholar]
- 43.Peng D, Kryczek I, Nagarsheth N, Zhao L, Wei S, Wang W, et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature. 2015;527:249–53. doi: 10.1038/nature15520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maio M, Covre A, Fratta E, Di Giacomo AM, Taverna P, Natali PG, et al. Molecular Pathways: At the Crossroads of Cancer Epigenetics and Immunotherapy. Clin Cancer Res. 2015;21:4040–7. doi: 10.1158/1078-0432.CCR-14-2914. [DOI] [PubMed] [Google Scholar]
- 45.Juergens RA, Wrangle J, Vendetti FP, Murphy SC, Zhao M, Coleman B, et al. Combination epigenetic therapy has efficacy in patients with refractory advanced non-small cell lung cancer. Cancer discovery. 2011;1:598–607. doi: 10.1158/2159-8290.CD-11-0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma T, Galimberti F, Erkmen CP, Memoli V, Chinyengetere F, Sempere L, et al. Comparing histone deacetylase inhibitor responses in genetically engineered mouse lung cancer models and a window of opportunity trial in patients with lung cancer. Molecular cancer therapeutics. 2013;12:1545–55. doi: 10.1158/1535-7163.MCT-12-0933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vo DD, Prins RM, Begley JL, Donahue TR, Morris LF, Bruhn KW, et al. Enhanced antitumor activity induced by adoptive T-cell transfer and adjunctive use of the histone deacetylase inhibitor LAQ824. Cancer Res. 2009;69:8693–9. doi: 10.1158/0008-5472.CAN-09-1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Christiansen AJ, West A, Banks KM, Haynes NM, Teng MW, Smyth MJ, et al. Eradication of solid tumors using histone deacetylase inhibitors combined with immune-stimulating antibodies. Proc Natl Acad Sci U S A. 2011;108:4141–6. doi: 10.1073/pnas.1011037108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.West AC, Mattarollo SR, Shortt J, Cluse LA, Christiansen AJ, Smyth MJ, et al. An intact immune system is required for the anticancer activities of histone deacetylase inhibitors. Cancer Res. 2013;73:7265–76. doi: 10.1158/0008-5472.CAN-13-0890. [DOI] [PubMed] [Google Scholar]
- 50.West AC, Johnstone RW. New and emerging HDAC inhibitors for cancer treatment. J Clin Invest. 2014;124:30–9. doi: 10.1172/JCI69738. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.