Abstract
Background
The Bari-Active trial showed that a physical activity intervention (PAI), versus standard pre-surgical care control (SC), produced significant increases in daily bout-related moderate-to-vigorous PA (MVPA in ≥10-minutes bouts) preoperatively. The current study examined whether PAI also produces superior improvements in psychological/motivational processes that may be important for PA adoption.
Objectives
Compare PAI and SC on baseline to post-intervention changes in PA-related enjoyment, self-efficacy, and motivations; and examine whether greater bout-related MVPA changes are associated with greater improvements in these variables.
Setting
University Hospital, United States.
Methods
Participants [(87% female; Body Mass Index (BMI)=45.0±6.5 kg/m2] were randomly assigned to 6 weeks of PAI (n=40) or SC (n=35). PAI received weekly counseling sessions to increase daily walking exercise. At baseline and post-intervention, both groups completed 7-day objective PA monitoring and questionnaires to evaluate changes in bout-related MVPA and PA enjoyment, self-efficacy, and motivation.
Results
Retention was 84% at post-intervention. Intent-to-treat analyses showed that PAI on average reported more favorable changes than SC in PA enjoyment, self-efficacy, amotivation (i.e. lack of PA motivation), and identified and intrinsic regulations (i.e. more autonomous PA motivations) (p<0.01). In PAI completers (n=33), changes in bout-related MVPA and psychological/motivational variables were unrelated.
Conclusion
PAI produced greater improvements in PA-related enjoyment, self-efficacy, and motivations, than SC. The lack of association between objectively-measured PA changes and psychological/motivational processes highlights the need for future research to identify which processes are most important for PA adoption and maintenance, and to determine whether the method used to measure PA affects the pattern of association.
Keywords: physical activity, intervention, self-efficacy, motivation, enjoyment, bariatric surgery
INTRODUCTION
Adoption of habitual physical activity (PA) represents a major behavioral challenge in bariatric surgery patients (1). Studies using objective PA monitors show that preoperatively, nearly all (95%–98%) of patients are inactive (2–5), defined as <150 minutes/week of moderate-to-vigorous intensity PA (MVPA) in ≥10-minute bouts (i.e. bout-related MVPA) (6). Postoperatively, patients on average demonstrate either no changes or only modest increases in bout-related MVPA, thus remaining inactive (3–5). A greater concern is that nearly two-thirds (63%) of patients do not perform any bout-related MVPA (2–5). Given that bariatric surgery alone appears to be insufficient for producing clinically meaningful changes in PA, there is a clear need to better understand factors, particularly psychological/motivational processes, that underlie PA behavior change, and specifically, adoption of habitual bout-related MVPA in this population.
Few studies have assessed PA-related psychological/motivational processes in bariatric surgery patients. Findings suggest: psychological barriers to PA adoption (e.g., low motivation and self-efficacy or confidence in ability to regularly perform PA) are common (7–10); patients can experience pre- to postoperative improvements in PA cognitions (e.g., self-efficacy) (11); preoperative PA cognitions may contribute to postoperative PA changes (11); and intervention-related increases in physical fitness are not accompanied by improvements in exercise self-efficacy and perceived PA benefits preoperatively (12). However, the above studies are limited by lack of: objective PA measurement, evaluation of changes in theoretically-based psychological/motivational processes in a randomized controlled trial (RCT), and examination of associations between psychological/motivational processes and bout-related MVPA.
The Bari-Active trial tested the effects of a 6-week preoperative PA intervention (PAI) versus a standard care control condition (SC) on post-intervention changes in objectively-measured bout-related MVPA. We previously reported that on average PAI produced large increases in bout-related MVPA from baseline to post-intervention (4.4 to 21.0 minutes/day) versus no change in SC (7.9 to 7.6 minutes/day) (13). The current study compares PAI vs. SC on changes in theoretically-based psychological/motivational processes underlying PA adoption including enjoyment (14), self-efficacy (15), and motivational regulations (16), the latter referring to different motivations for PA that reside along a continuum ranging from amotivation (i.e. lacking motivation for PA) to intrinsic regulation (i.e. autonomous motivation for PA derived from enjoyment of PA). We hypothesized that PAI would report significantly greater baseline to post-intervention improvements in PA enjoyment, self-efficacy, and PA motivations (i.e. indicating a shift from a lack of motivation or extrinsic motivation towards more intrinsic motivations) than SC. Additionally, we predicted that greater increases in bout-related MVPA would be independently related to greater improvements in these variables among PAI completers.
METHODS
Design
Potential participants were referred to the research center by 3 hospital clinics in Rhode Island, USA between April 2010 and January 2014. Patients who expressed interest in participating after being presented a study flyer, provided their contact information, and received surgeon approval to engage in a walking exercise program were contacted for telephone screening. Eligible candidates attended an orientation/baseline visit involving informed consent, height and weight measurements, and questionnaires assessing PA-related enjoyment, self-efficacy, and motivation. Additionally, participants wore an activity monitor for 7 days, then returned and were randomized to 6 weeks of PAI or SC.
At post-intervention, participants again completed questionnaires and 7-day activity monitoring. Participants received a $50 honorarium upon completion of both the baseline and post-intervention assessment visits. Study procedures were approved by The Miriam Hospital Institutional Review Board (clinicaltrials.gov registration NCT00962325).
Participants
Participants were 80 individuals aged 18–70 years old with severe obesity (body mass index (BMI) ≥35 kg/m2) seeking bariatric surgery. Additionally, participants had to report being inactive (i.e. <150 MVPA bout-related minutes per week)(6) but having the ability to walk ≥2 blocks unassisted. Individuals were ineligible if they were scheduled to undergo bariatric surgery <10 weeks during screening, participating in another PA or weight loss program, intended to move to another geographic location during the study, or had medical, psychiatric, or language barriers that would interfere with adherence to the protocol.
Randomization
Participants were randomly assigned 1:1 to PAI or SC using a computer-generated random permuted blocking procedure with blocks of size 2, 4, and 6.. Assignment to condition was concealed from the participant and the research team until a participant completed the baseline assessment.
Physical Activity Intervention (PAI)
PAI involved 6 consecutive weekly individual face-to-face sessions with the primary author (along with standard pre-surgical care). Sessions lasted 30–45 minutes and included the following objectives/tasks: review participants' PA self-monitoring records and progress toward goals; problem-solve barriers to PAI goals; teach strategies to achieve PAI goals; set weekly bout-related walking exercise and step goals; develop a daily action plan for achieving goals; and assigning homework focusing on behavior change strategies. PAI content was derived from the PA component of the lifestyle intervention implemented in the Diabetes and Prevention Program and Look AHEAD trials (17–18) and supplemented with additional content and strategies to target theoretically-based psychological/motivational processes underlying PA adoption and maintenance, primarily PA enjoyment, self-efficacy, and autonomous types of motivation (14–16). For example, participants were assisted in identifying ways to both increase the pleasant aspects (e.g., walk at a scenic park to enhance the PA experience) and decrease the unpleasant aspects (e.g., walking with a friend to reduce boredom) of exercise. Additionally, participants received specific, measurable, and attainable daily and weekly goals tailored to initial PA levels to enhance self-efficacy. Finally, to foster a shift towards more autonomous motivation, emphasis was placed on achieving intrinsic versus extrinsic PA rewards, providing a variety of strategies from which to choose to achieve PAI goals, and encouraging exploration of congruence between efforts to change PA behavior and values (13, 16). See Bond et al. (13) for a detailed description of topics, content, and strategies covered.
The primary goal of the PAI was to increase bout-related walking performed at a moderate intensity by 30 minutes/day. A secondary goal was to increase steps taken by 5,000/day. At the initial intervention session, participants received a monitoring log and pedometer to track and motivate progress towards the intervention goals. Participants recorded number of bout-related walking minutes and steps taken at the end of each day. For the first week, participants were instructed to maintain their usual PA patterns to establish a baseline for daily bout-related walking and steps. Baseline values were then used to determine goals and rate of progression over the subsequent intervention weeks. For the second week, participants were prescribed 10 additional bout-related walking minutes/day and 1,000 steps/day compared to baseline levels. For remaining weeks, 5 minutes of daily bout-related walking and 1,000 daily steps were added to the prior week's prescription.
Standard Pre-Surgical Care Control (SC)
SC participants attended regular preoperative clinic visits to receive standard care. The surgical teams advised adoption of an active lifestyle but gave no formal PA prescription or behavioral strategies.
Measures
Objective measurement of MVPA. The SenseWear Armband (SWA; BodyMedia, Inc., Pittsburgh, PA) was used to objectively evaluate baseline to post-intervention changes in the primary outcome—i.e. daily bout-related MVPA. This outcome was chosen because purposeful or structured walking is likely to be captured by bout-related MVPA. The SWA is a wireless multi-sensor monitor worn on the upper right triceps muscle that integrates tri-axial accelerometer data with physiologic sensors to estimate energy expenditure (EE) and intensity of activities. Pattern-recognition algorithms match sensor data to an activity class (e.g., walking) that best describes each minute of activity, which is linked to a regression model mapping the sensor values and physiologic parameters to EE. The SWA has demonstrated acceptable levels of agreement with criterion measures of EE in healthy and older adults(19–20) and produces MVPA estimates similar to other objective research-grade monitors(21–22).
Participants were asked to wear the SWA during waking hours for 7 consecutive days at baseline and post-intervention follow-up. Wear-time was assessed using the SenseWear Professional Software (Version 7.0). Metabolic equivalent (MET) values were used to determine daily minutes spent in bout-related and total MVPA (i.e. ≥3 METs). Interruption involving ≤ 1 continuous minute below 3 METs was allowed when calculating MVPA bouts. SWA wear-time of ≥6 hours/day on ≥4 days per assessment was required for inclusion in analysis(13).
PA enjoyment
The 18-item Physical Activity Enjoyment Scale (PACES) evaluated changes in PA enjoyment(23). Participants rated how they “felt at the moment about physical activity” using a 7-point bipolar scale (e.g., [1] “It's very pleasant” to [7] “It's not fun at all”). Higher PACES scores reflect greater PA enjoyment and predict PA behavior within the context of PA promotion interventions involving inactive adults(14, 24–25).
PA self-efficacy
Change in self-efficacy for MVPA was assessed using a validated brief 5-item questionnaire(26). Participants indicated their confidence being physically active in challenging situations (e.g., “when I am tired”) on a scale of 1 (“not at all confident”) to 5 (“extremely confident”). Higher scores indicate greater self-efficacy and predict of higher levels of PA readiness and behavior(14, 26).
PA motivation
The Behavioral Regulation for Exercise Questionnaire-2 (BREQ-2) evaluated changes in PA motivations(27). The BREQ-2 includes 19 items, rated on a five-point Likert-scale, from 0 (“not true of me”) to 4 (“very true of me”), that assess motivation types along a continuum with extrinsic or non-autonomous forms at one end (i.e. amotivation—e.g., “I think that exercising is a waste of time” and external regulation—e.g., “I exercise because other people tell me I should”) and increasingly intrinsic or autonomous forms at the other end (i.e. introjected regulation—e.g., “I feel guilty when I do not exercise”, identified regulation— e.g., “I value the benefits/advantages of exercising” and intrinsic motivation—e.g., “I enjoy my exercise sessions”). The mean of the 5 subscales is calculated to score the degree of each motivation type separately. Research has shown high reliability for the BREQ-2 subscales and higher scores on subscales representing more intrinsic types of motivation to be predictive of higher levels of PA(27–28).
Other Measures
A demographics (i.e. age, sex, race/ethnicity, marital status, educational level) questionnaire was completed at baseline. Weight was measured at baseline and post-intervention follow-up.
Statistical Analysis
Analyses were performed using SPSS Statistics for Windows (version 20.0; SPSS, IBM Corp, Armonk, NY). Descriptive statistics including means and standard deviations (SD) and frequency counts were calculated to describe participants' characteristics including MVPA and PA-related enjoyment, self-efficacy, and motivation at baseline and post-intervention follow-up. Comparison of changes in psychological/motivational processes were assessed via analysis of covariance (ANCOVA), adjusting for baseline values, age, sex, and BMI. The above analysis followed the intent-to-treat (ITT) principle in which missing PA enjoyment, self-efficacy, and motivation data at post-intervention follow-up were substituted with baseline values (assuming no change in the values).29 In PAI completers (i.e. participants who attended all 6 intervention sessions and complete baseline and post-intervention follow-up assessments), linear regression evaluated associations between changes in daily bout-related MVPA and related psychological/motivational variables. Changes in bout-related MVPA were used to predict changes in each of the psychological/motivational variables (i.e. PA enjoyment, self-efficacy, and specific types of motivation on which PAI and SC groups significantly differed based on the aforementioned ANCOVA analyses), adjusting for baseline levels of psychological/motivational processes and bout-related MVPA, age, sex, and BMI. Linear regression analyses were repeated with daily steps and total MVPA minutes; however, given that these analyses produced a pattern of results identical to bout-related MVPA, only results with bout-related MVPA (i.e. primary outcome) are shown. Significance tests were two-tailed, with α=0.05. This trial was designed to have 80% power to detect significant between-group differences in bout-related MVPA of at least 10 minutes/day with a sample size of at least 75.
RESULTS
Recruitment and retention
Recruitment and retention data were reported previously(13). Of 293 patients screened by telephone, 213 were excluded, resulting in 80 participants who were randomized. Five participants were inactivated after randomization due to being scheduled for surgery prior to study completion (n=4) and family emergency (n=1). Of the remaining 75 participants, 63 (84%) completed the post-intervention follow-up with no differences in retention between groups. Study completers only differed from non-completers on age (47.1±8.4 vs. 40.3±9.4 years old, p=0.01).
Baseline characteristics of participants
Participants' baseline characteristics are shown in Table 1. PAI and SC groups did not significantly differ on any variable. Overall, participants on average had severe obesity, were predominantly female, middle-aged, non-Hispanic White with some college education. Participants averaged 33 MVPA minutes/day, of which roughly 20% was accumulated in ≥10-minute bouts. Regarding PA-related psychological/motivational processes, participants on average had low PA enjoyment (i.e. 79 on 126-point scale) and self-efficacy (2.8 on 0–5 scale) scores. Similarly, participants on average had both low external (amotivation and external regulation) and internal (introjected, identified, and intrinsic regulation) motivations for PA, with BREQ-2 scores on each of these domains falling below 2.5 on a 0-4 scale.
Table 1.
Baseline characteristics of participants randomized to the Physical Activity Intervention (PAI) and Standard Surgical Care Control (SC) conditions
| PAI | SC | ||
|---|---|---|---|
| Full Sample (N = 75) | Condition (N = 40) | Condition (N = 35) | |
| Demographic and anthropometric characteristics | |||
| Sex (%) | |||
| Men | 13.3 | 15.0 | 11.4 |
| Women | 86.7 | 85.0 | 88.6 |
| Age, mean (SD), years | 46.0 (8.9) | 44.2 (9.2) | 48.1 (8.1) |
| Race (%) | |||
| American Indian | 2.7 | 5.0 | 0.0 |
| Black | 5.3 | 5.0 | 5.7 |
| White | 78.7 | 77.5 | 80.0 |
| Other | 13.3 | 12.5 | 14.3 |
| Ethnicity (%) | |||
| Hispanic | 12.0 | 12.5 | 11.4 |
| Non-Hispanic | 88.0 | 87.5 | 88.6 |
| Education (%) | |||
| High school or less | 26.6 | 17.5 | 37.1 |
| Some college | 45.3 | 55.0 | 34.3 |
| College or University Degree | 21.3 | 20.0 | 22.9 |
| Graduate Degree | 6.8 | 7.5 | 5.7 |
| Body Mass Index, mean (SD), kg/m2 | 45.0 (6.5) | 45.6 (7.0) | 44.4 (5.8) |
| Physical Activity | |||
| Total MVPA minutes/day, mean (SD) | 32.2 (27.3) | 30.1 (21.1) | 33.7 (33.2) |
| Bout-related MVPA minutes/day, mean (SD) | 6.0 (12.1) | 4.4 (5.5) | 7.9 (16.6) |
| Physical Activity Psychological/Motivational Processes | |||
| Enjoyment, mean (SD) | 79.0 (17.1) | 79.9 (17.8) | 77.9 (16.3) |
| Self-efficacy, mean (SD) | 2.8 (0.8) | 2.9 (0.8) | 2.8 (0.9) |
| Motivational types, mean (SD) | |||
| Amotivation | 0.6 (0.8) | 0.7 (0.9) | 0.5 (0.7) |
| External regulation | 0.8 (0.8) | 0.8 (0.8) | 0.7 (0.8) |
| Introjected regulation | 1.7 (1.0) | 1.6 (1.0) | 1.8 (1.0) |
| Identified regulation | 2.2 (0.8) | 2.1 (0.8) | 2.3 (0.8) |
| Intrinsic regulation | 1.7 (1.0) | 1.7 (1.1) | 1.7 (0.9) |
Changes in PA psychological/motivational processes
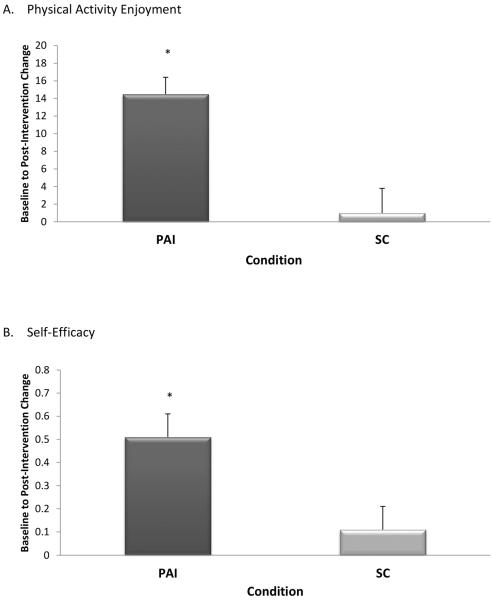
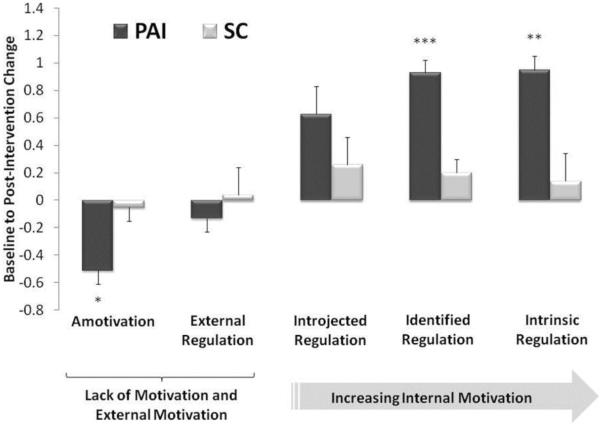
Changes in PA enjoyment and self-efficacy, controlling for baseline values, age, sex, and BMI, are shown in Figure 1 by condition. PAI produced significantly greater improvements in PA enjoyment (79.9±17.8 to 94.4±17.7 vs. 77.9±16.3 to 78.9±16.8) and self-efficacy (2.9±0.8 to 3.4±0.8 vs. 2.8±0.9 to 2.9±0.9) versus SC (p<0.005). Likewise, as shown in Figure 2, PAI produced greater decreases in amotivation (0.7±0.9 to 0.2±0.6 vs. 0.5±0.7 to 0.5±0.8) and greater increases in identified (2.1±0.8 to 3.0±0.6 vs. 2.3±0.8 vs. 2.5±0.8) and intrinsic (1.7±1.1 to 2.7±0.9 vs. 1.7±0.9 vs. 1.8±1.2) motivation compared to SC participants (p<0.01), after adjusting for baseline value, age, sex, and BMI. Changes in the external and introjected motivational types did not significantly differ between PAI and SC.
Figure 1.
Comparison of baseline to post-intervention changes in physical activity enjoyment and self-efficacy between participants randomized to the Physical Activity Intervention (PAI) and Standard Pre-Surgical Care Control (SC) conditions
Note. PAI = Physical Activity Intervention; SC = Standard Pre-Surgical Care Control
Mean ± Standard Error (SE) values shown
*p < 0.001
Note. PAI = Physical Activity Intervention; SC = Standard Pre-Surgical Care Control
Mean ± Standard Error (SE) values shown
*p = 0.004
Figure 2.
Comparison of baseline to post-intervention changes in physical activity motivational types between participants randomized to the Physical Activity Intervention (PAI) and Standard Pre-Surgical Care Control (SC) conditions
Note. PAI = Physical Activity Intervention; SC = Standard Pre-Surgical Care Control
Mean ± Standard Error (SE) values shown
* p = 0.005, ** p = 0.001, *** p < 0.001
Associations between changes in bout-related MVPA and PA psychological/motivational processes in PAI condition
Changes in PA enjoyment, self-efficacy, and those types of motivation shown to significantly differ between PAI and SC groups (i.e., amotivation, identified regulation, and intrinsic regulation)were regressed on changes in daily bout-related MVPA in PAI completers (n=33) controlling for baseline values, age, sex, and BMI. Larger changes in bout-related MVPA were not associated with larger improvements in any of the PA psychological/motivational variables (p range = 0.20–0.90).
DISCUSSION
We previously showed that PAI produced significant increases in bout-related MVPA compared to SC participants who did not change (13), demonstrating that behavioral intervention can produce substantial changes in PA behavior before large weight losses and the myriad of other benefits that occur after bariatric surgery. This study extends those findings by demonstrating that PAI also facilitates enhancement of psychological/motivational processes underlying PA behavior including PA enjoyment, self-efficacy, and autonomous motivation (14–16).
At baseline, both PAI and SC participants reported low PA enjoyment and self-efficacy similar to that reported in a previous study of overweight adults who remained inactive during a home-based PA intervention. (30). However, at post-intervention, PAI produced increases in levels of PA enjoyment (+14.5 vs. +1.0 on a 126-point scale) and self-efficacy (+0.5 vs. +0.1 on a 5-point scale) that were markedly greater than those produced by SC. Moreover, levels of PA enjoyment and self-efficacy after PAI intervention were consistent with those reported by participants who became active during the above mentioned previous PA intervention trial. (30).
PAI and SC participants also reported severe PA motivational deficits at baseline comparable to individuals with severe mental illnesses (e.g., major depressive disorder) (31). At post-intervention, PAI produced more favorable changes in motivational processes compared to SC, including greater decreases in amotivation and greater increases in identified and intrinsic motivation. However, while PAI participants at post-intervention decreased to very low levels of amotivation, they increased to only moderate levels of identified and intrinsic motivation (i.e. 3.0 and 2.7 on a 0-4 scale). Nonetheless, the overall pattern of change in motivation produced by PAI reflects a shift towards more autonomous motivation such that PA behavior is driven more by intrinsic (e.g., “I enjoy my exercise sessions”) than extrinsic (e.g., “I exercise because other people tell me I should”) reasons (16, 26, 31). Taken together, greater improvements in PA enjoyment, self-efficacy, and autonomous motivations suggests that PAI was effective in helping patients to: develop more favorable affective judgments of their PA experience (32), become more confident in their ability to perform PA even when faced with barriers (14, 26), and increase internal regulation of their PA behavior (16, 27).
Interestingly, and contrary to our hypothesis, greater increases in bout-related MVPA were not associated with greater increases in PA enjoyment, self-efficacy, and motivation among PAI completers. It is possible that these particular psychological/motivational processes might be less associated with habitual PA adoption and more associated with PA maintenance (14, 29), or that other psychological/motivational constructs that we did not measure might be more strongly related to PA adoption. For example, recent qualitative data suggest that additional psychological/motivational factors such as social support (e.g., increased social interaction while performing PA would enhance PA enjoyment and motivation) and time management (e.g., dedicating specific time for PA) would facilitate adoption of habitual PA before bariatric surgery. Conversely, factors such as body dissatisfaction (e.g., concerns about being watched or judged while performing PA) and preference for engaging in sedentary behaviors and other activities rather than structured PA during leisure time (e.g., would rather watch TV, catch up on sleep, or spend time with friends) undermine likelihood of habitual PA adoption (8). Another interpretation of these findings concerns the method by which PA was measured—i.e. what is most relevant to change in PA-related psychological/motivational processes may be perceived or self-reported changes versus actual or objectively-measured changes. As we have shown, self-reported and objectively-measured changes in bout-related MVPA differ markedly in bariatric surgery patients (3). Thus, an objectively small increase in bout-related MVPA might be perceived as large and subsequently produce larger changes in enjoyment and motivation. Our findings in combination with those from previous research showing associations between self-reported PA and psychological/motivational factors (12) suggests that the way in which PA behavior and these factors are measured may influence the findings, and should be carefully considered, especially in bariatric surgery patients who appear to overestimate changes in PA (3).
This study has several strengths that advance previous research examining psychological/motivational processes underlying PA behavior in bariatric surgery patients (8–13): it is the first to evaluate changes in theoretically-based psychological/motivational processes using validated measures (14–16, 23–28, 30) in a RCT. Additionally, this study is the first to examine associations between changes in psychological/motivational processes and intervention-related changes in objectively-measured bout-related MVPA.
This study has also certain limitations. While results provide evidence that PAI produces significant improvements in PA enjoyment, self-efficacy, and autonomous motivations, it is not known if these benefits extend beyond the brief PAI period. Thus, future studies are needed to determine whether initial PAI-related improvements in psychological/motivational processes can help patients to further increase and maintain PA changes over longer follow-up periods. Given that the SC and PAI conditions were not matched on amount of therapist contact; social factors related to attention, interest, and encouragement might have contributed to group differences. Finally, given that only 25% of patients who underwent initial screening were randomized, it is unclear whether levels of PA enjoyment, self-efficacy, and motivation reported in our study sample are representative of the general bariatric surgery population.
In conclusion, the present study extends previous findings from the Bari-Active trial by showing that a behavioral intervention is not only effective for promoting habitual PA adoption in patients seeking bariatric surgery, but also enhancing PA enjoyment, internal motivations for PA, and confidence in ability to overcome PA barriers. These findings also have important clinical implications given that they provide support for communicating to patients the message that while habitual PA might seem aversive prior to adoption, they are likely to find it enjoyable once they do start even before experiencing the benefits of bariatric surgery. Findings showing lack of association between changes in objectively-measured PA and PA enjoyment, self-efficacy, and motivation highlight the need for additional research that uses both subjective and objective PA measures in combination with measures of psychological/motivational processes to clarify associations between these variables in bariatric surgery patients. Moreover, given that the present study is one of the few to investigate the role of psychological factors in PA participation among bariatric surgery patients, future studies are needed to identify psychological and other modifiable determinants of PA behavior in bariatric surgery patients. Such studies are necessary to not only enhance researchers' and clinicians' understanding of why patients are inactive but to also help identify suitable intervention targets for promoting increased PA adoption and maintenance.
Acknowledgements
This research was supported by a grant from the National Institutes of Health/National Institute of Diabetes & Digestive & Kidney Diseases (K01 DK083438, PI: Bond). The authors would like to thanks the Bari-Active subjects for their participation.
Source of Support: National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK83438)
Trial Registration: clinicaltrials.gov Identifier: NCT00962325
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement None of the authors have conflicts of interest to disclose.
REFERENCES
- 1.Bond DS, Thomas JG. Measurement and intervention on physical activity and sedentary behaviors in bariatric surgery patients: emphasis on mobile technology. Eur Eat Disord Rev. 2015;23:470–78. doi: 10.1002/erv.2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bond DS, Jakicic JM, Vithiananthan S, et al. Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surg Obes Relat Dis. 2010;6:72–8. doi: 10.1016/j.soard.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative changes in bariatric surgery patients: self-report vs. objective measures. Obesity (Silver Spring) 2010;18:2395–97. doi: 10.1038/oby.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King WC, Hsu JY, Belle SH, et al. Pre- to postoperative changes in physical activity: report from the longitudinal assessment of bariatric surgery-2 (LABS-2) Surg Obes Relat Dis. 2012;8:48–59. doi: 10.1016/j.soard.2011.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King WC, Chen JY, Bond DS, et al. Objective assessment of changes in physical activity and sedentary behavior: pre- through 3 years post-bariatric surgery. Obesity (Silver Spring) 2015;23:1143–50. doi: 10.1002/oby.21106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 7.Bond DS, Thomas JG, Ryder BA, Vithiananthan S, Pohl D, Wing RR. Ecological momentary assessment of the relationship between intention and physical activity behavior in bariatric surgery patients. Int J Behav Med. 2013;20:82–7. doi: 10.1007/s12529-011-9214-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zabatiero J, Hill K, Gucciardi DF, et al. Beliefs, barriers and facilitators to physical activity in bariatric surgery candidates. Obes Surg. 2015 Sep 1; doi: 10.1007/s11695-015-1867-4. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Peacock JC, Sloan SS, Cripps B. A qualitative analysis of bariatric patients' post-surgical barriers to exercise. Obes Surg. 2014;24:292–8. doi: 10.1007/s11695-013-1088-7. [DOI] [PubMed] [Google Scholar]
- 10.Hübner C, Baldofski S, Zenger M, et al. Influences of general self-efficacy and weight bias internalization on physical activity in bariatric surgery candidates. Surg Obes Relat Dis. 2014 Nov 25; doi: 10.1016/j.soard.2014.11.013. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Wouters EJ, Larsen JK, Zijlstra H, van Ramhshorst B, Geenen R. Physical activity after surgery for severe obesity: the role of exercise cognitions. Obes Surg. 2011;21:1894–9. doi: 10.1007/s11695-010-0276-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baillot A, Mampuya WM, Comeau E, Méziat-Burdin A, Langlois MF. Feasibility and impacts of supervised exercise training in subjects with obesity awaiting bariatric surgery: a pilot study. doi: 10.1007/s11695-013-0875-5. [DOI] [PubMed] [Google Scholar]
- 13.Bond DS, Vithiananthan S, Thomas JG, et al. Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis. 2015;11:169–77. doi: 10.1016/j.soard.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis BA, Williams DM, Frayeh A, Marcus BH. Self-efficacy versus perceived enjoyment as predictors of physical activity behaviour. Psychol Health. 2015 Nov 5;:1–28. doi: 10.1080/08870446.2015.1111372. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heiss VJ, Petosa RL. Social cognitive theory correlates of moderate-intensity exercise among adults with type 2 diabetes. Psychol Health Med. 2016;21:92–101. doi: 10.1080/13548506.2015.1017510. [DOI] [PubMed] [Google Scholar]
- 16.Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78. doi: 10.1186/1479-5868-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25:2165–71. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Look AHEAD Research Group. Wadden TA, West DS, Delahanty L, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring) 2006;14:737–52. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calabró MA, Lee JM, Saint-Maurice PF, Yoo H, Welk GJ. Validity of physical activity monitors for assessing lower intensity activity in adults. Int J Behav Nutr Phys Act. 2014;11:119. doi: 10.1186/s12966-014-0119-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mackey DC, Manini TM, Schoeller DA, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–13. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unick JL, Bond DS, Jakicic JM, et al. Comparison of two objective monitors for assessing physical activity and sedentary behaviors in bariatric surgery patients. Obes Surg. 2012;22:347–52. doi: 10.1007/s11695-011-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berntsen S, Hageberg R, Aanstad A, et al. Validity of physical activity monitors in adults participating in free-living activities. Br J Sports Med. 2010;44:657–64. doi: 10.1136/bjsm.2008.048868. [DOI] [PubMed] [Google Scholar]
- 23.Kendzierski D, DeCarlo KJ. Physical activity enjoyment scale: two validation studies. J Sport Exerc Psychol. 1991;13:50–64. [Google Scholar]
- 24.Williams DM, Papandonatos GD, Napolitano MA, Lewis BA, Whitely JA, Marcus BH. Perceived enjoyment moderates the efficacy of an individually-tailored physical activity intervention. J Sport Exerc Psychol. 2006;28:300–09. [Google Scholar]
- 25.Ivanova E, Jensen D, Cassoff J, Fei G, Knäuper B. Acceptance and commitment therapy improves exercise tolerance in sedentary women. Med Sci Sports Exerc. 2015;47:1251–58. doi: 10.1249/MSS.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 26.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 27.Markland D, Tobin V. A modification of the Behavioral Regulation in Exercise Questionnaire to include an assessment of motivation. J Sport Exerc Psychol. 2004;26:191–96. [Google Scholar]
- 28.Duncan LR, Hall CR, Wilson PM, Jenny O. Exercise motivation: a cross-sectional analysis examining its relationship with frequency, intensity, and duration of exercise. Int J Behav Nutr Phys Act. 2010;7:7. doi: 10.1186/1479-5868-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ware JH. Interpreting incomplete data in studies of diet and weight loss. N Engl J Med. 2003;348:2136–37. doi: 10.1056/NEJMe030054. [DOI] [PubMed] [Google Scholar]
- 30.Williams DM, Lewis BA, Dunsiger S, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36:186–94. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vancampfort D, Stubbs B, Venigalla SK, Probst M. Adopting and maintaining physical activity behaviors in people with severe mental illness: The importance of autonomous motivation. doi: 10.1016/j.ypmed.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 32.Rhodes RE, Fiala B, Conner M. A review and meta-analysis of affective judgments and physical activity in adult populations. Ann Behav Med. 2009;38:180–204. doi: 10.1007/s12160-009-9147-y. [DOI] [PubMed] [Google Scholar]