Abstract
Objectives
We assessed a worksite intervention designed to promote tobacco control among manufacturing workers in Greater Mumbai, India.
Methods
We used a cluster-randomized design to test an integrated health promotion/health protection intervention, which addressed changes at the management and worker levels. Between July 2012 and July 2013, we recruited 20 worksites on a rolling basis and randomly assigned them to intervention or delayed-intervention control conditions. The follow-up survey was conducted between December 2013 and November 2014.
Results
The difference in 30-day quit rates between intervention and control conditions was statistically significant for production workers (OR=2.25, P=0.03), although not for the overall sample (OR=1.70; P=0.12). The intervention resulted in a doubling of the 6-month cessation rates among workers in the intervention worksites compared to those in the control, for production workers (OR=2.29; P=0.07) and for the overall sample (OR=1.81; P=0.13), but the difference did not reach statistical significance.
Conclusions
These findings demonstrate the potential impact of a tobacco control intervention that combined tobacco control and health protection programming within Indian manufacturing worksites.
Introduction
There is an urgent need for effective tobacco control initiatives in response to the rising global burden of tobacco, particularly in the developing world.1,2 The World Health Organization (WHO) predicts that of the more than 8 million people globally who are expected to die from tobacco-related causes by 2030, 80% will be from low- and middle-income countries (LMICs).3 India faces particular challenges, given its population of 1.2 billion and widespread use of multiple forms of tobacco, with overall prevalence rates of 48% among men and 20% among women.4–6 In 2010, over 1 million Indians were expected to die from tobacco-related causes.7,8 Reflecting the pervasive use of smokeless forms of tobacco, India has one of the highest oral cancer rates in the world,9,10 still on the rise.11 Although India was an early signatory to the Framework Convention on Tobacco Control and smoking is banned in public places such as enclosed worksites,12 enforcement mechanisms are weak, few resources are available to support tobacco use cessation, the prevalence of quitting remains low, and social norms rarely support quitting.4
Growing attention is being paid to these mounting global disparities in tobacco use.13,14 The National Cancer Institute (NCI) recently formed its Center for Global Health aimed at reducing the global burden of cancer.15 In the U.S. and other high-income countries, employer initiatives have contributed to tobacco control. Such efforts are uncommon within India, although policy leaders and Indian employers alike are increasingly examining the implications of non-communicable diseases and risk-related behaviors such as tobacco use for productivity and economic growth.16–20
The WHO,21 the National Institute for Occupational Safety and Health (NIOSH),22 and others23,24 have recommended new models for workplace interventions that aim to reduce hazards in the physical and psychosocial work environments while also providing support for individual behavior changes such as quitting tobacco use. This approach has been shown to be efficacious in promoting smoking cessation, particularly for blue-collar workers who face dual health risks because of their high rates of risk-related behaviors, such as tobacco use, and exposures to occupational hazards.25–27
We applied this approach in the Mumbai Worksite Tobacco Control Study, which tested the effectiveness of a worksite intervention in increasing tobacco use cessation among manufacturing workers. The purpose of this manuscript is to present findings related to the following hypotheses: (1) tobacco use cessation rates, defined as six-month continuous abstinence of all tobacco use (primary outcome) and 30-day abstinence (secondary outcome), will be significantly greater in intervention worksites compared to control worksites; and (2) improvements in tobacco use cessation rates in the intervention group relative to the control group will be greater among production workers compared to managers and office workers.
Methods
This cluster randomized controlled trial (RCT) tested the effectiveness of the Healthy, Safe, and Tobacco-free Worksites intervention in increasing tobacco use cessation among workers. The worksite was the unit of intervention and randomization. This study was a collaboration among the Harvard T.H. Chan School of Public Health (HSPH), the Dana-Farber Cancer Institute, and New England Research Institutes in Boston, Massachusetts, and the Healis-Sekhsaria Institute for Public Health in Mumbai. This study was approved by the Healis and HSPH Institutional Review Boards, as well as by the Indian Council of Medical Research, and has been registered with clinicaltrials.gov and the Clinical Trial Registry of India.
Study Population and Sample
We recruited 22 worksites to this study, two of which were included in a pilot test of the intervention. Twenty worksites were included in the full-scale RCT; ten were randomly assigned to intervention and ten to control. Worksite eligibility criteria included: (1) employ at least 200 production workers; this definition was expanded to include at least 60% of the workforce to be comprised of production workers; (2) be located in the Greater Mumbai area, including the Mumbai, Thane, or Raigad districts; (3) be involved in some type of manufacturing; and (4) be willing to provide a current employee roster as part of survey planning. Participating worksites agreed to be randomly assigned to the intervention or the delayed intervention control condition; participate in the intervention if assigned to the intervention condition; and participate in the planned data collection activities, regardless of assigned condition. Companies recruited to the study manufactured a range of products. We described the process of worksite recruitment in a prior manuscript.28 Of the 20 companies participating in the study at baseline, 17 participated in the final survey. One intervention and two control worksites dropped out of the follow-up survey, due to personnel changes (intervention site); competing priorities, including labor negotiations; and loss of interest related to dissatisfaction with being assigned to the control condition. The trial was otherwise completed as planned.
All workers were eligible to participate in the intervention. At each survey time point, we surveyed a census of permanent workers employed by the worksite, based on a roster provided by the company; to ensure that we included all employees, new workers not included on the roster were also surveyed.
Intervention conditions
Worksites were randomly assigned to the intervention or delayed intervention control condition on a rolling basis in blocks of four worksites, after each block of sites completed the baseline survey, by the biostatistician on Boston, with the India team blinded to the process.
Delayed intervention Control group
Worksites randomized to this condition were offered two health education events: (1) between the baseline and follow-up surveys, one non-tobacco related health education event, either on HIV/AIDS or stress management, offered by a trained health educator; (2) after completion of the follow-up survey, one tobacco-related health education event (Table 1). In addition, we provided a program overview and educational materials to management at the completion of the intervention.
Table 1.
Intervention components by condition
| Program A (Intervention) - Healthy, Safe and Tobacco Free Worksites’ program | Program B (Delayed Intervention Control) | |
|---|---|---|
| Management Level |
|
|
| Worker Level |
|
|
Intervention Group -- “The Healthy, Safe, and Tobacco-free Worksites Program”
The nine-month intervention addressed changes at the management and worker levels, and aimed to capitalize on and supplement existing efforts in occupational safety and health (OSH) (Table 1). The intervention was designed based on careful formative research, including pilot testing of a part of the intervention in two pilot worksites.
Interventions for management
Study staff provided consultation on adoption and implementation of a worksite tobacco control policy. All worksites were encouraged to implement a tobacco control policy; the consultation with management focused on compliance with legislation banning smoking in public places, and additionally encouraged expansion of policies to include prohibiting use of smokeless tobacco. As part of efforts to support OSH, a safety expert conducted an industrial hygiene walk-through to identify potential workplace hazards, and provided a brief consultation based on the report, recommending changes to reduce exposures.
Interventions for individual workers
The program targeted both tobacco users and non-users, with the aim of providing support for quitting and building social norms around tobacco control. While all worksite employees were invited to participate in the program, it was specifically designed for the production workers who have higher rates of tobacco use. The intervention centered around six health education events for workers conducted by trained study health educators (Table 1). Each event was offered onsite during multiple 15 to 20 minute sessions delivered during a single day at every intervention company. These health education events and corresponding materials were designed to increase workers’ understanding of the risks associated with tobacco use, their motivations to quit or help someone quit, and the skills and social support needed for cessation. The information was provided through discussions, audio-visuals, and participatory activities. The messages and materials additionally linked tobacco control with the work environment to enhance their salience and communicate messages about OSH.
Data collection
At baseline, prior to randomization, we surveyed workers in the 20 worksites on a rolling basis as worksites were recruited to the study (July 2012 – July 2013). Survey administration, conducted onsite in English, Hindi, and Marathi, included options for interviewer-and self-administered formats; we used highest education level attained as a proxy for literacy and offered those who completed grade 12 or higher the self-administered version, and those with less education were interviewed by a trained interviewer. The follow-up survey was conducted using the same methods in 17 of the 20 sites between 14 and 18 months post-completion of the baseline assessment (December 2013 – November 2014).
In addition, we tracked implementation of the intervention protocol. For the management intervention, senior study staff responsible for this intervention completed process tracking forms for each meeting, including meeting attendees, total meeting time, and topics addressed. Health educators tracked the worker-level intervention; for each health education event, process tracking included the total number of participating workers, average time spent on each session with workers, whether or not specific topics or activities were implemented as per the protocol, and the number of materials displayed at each event.
Measures
Tobacco use and cessation were measured by self-report using standard items.29–31 Tobacco use status was assessed at baseline and final, and included assessment of current users of any tobacco, using separate items to assess smoking and use of smokeless tobacco. Tobacco use cessation was defined as cessation of using any tobacco product, measured among respondents to the follow-up survey who reported using tobacco in the last 18 months, to capture those using tobacco at the beginning of the intervention. Among these users, we defined six-month continuous cessation (primary outceom) as having quit using any tobacco in the past 18 months and not using any tobacco in last 6 months. In the same sample, thirty-day tobacco quit status (secondary outcome) was defined as having quit using tobacco in the last 18 months and not using any tobacco in the last 30 days. No changes were made to trial outcomes.
Covariates
Socio-demographic characteristics were measured by self-report using standard items, including age, gender, tenure at worksite (less than one year vs. one year or more), economic wellbeing (ownership of refrigerator, vehicle, or neither), education, and marital status. We also assessed employee’s job title using information provided by the worksite; we coded job title as production or non-production based on employees’ department and job title provided by the employer.
Statistical methods
Initial power calculations were based on a planned recruitment of 20 worksites randomized into the two groups with an average of 72 tobacco users per worksite for a total sample size of 720 workers per group. Based on prior findings regarding quit rates among tobacco users in Mumbai,32 we assumed that 2% of users in the control group would quit using tobacco; also assuming a within worksite correlation of 0.05, this sample size provided 80% power to detect a quit rate of 9% in the intervention group as statistically significantly different from the control group rate at the 5% significance level.
We controlled for the clustering of workers in worksites in all analyses. Preliminary analysis assessed balance in the two conditions with respect to age, gender, occupation/position, worksite tenure, economic wellbeing, education, marital status, and tobacco use using mixed effect linear modeling methods, with intervention as a fixed effect and worksite as a random effect. For analysis of the intervention effect, we used mixed effect logistic regression analysis of quit status on intervention group (fixed effect), controlling for worksite (random effect). We did not control for randomization block.
Results
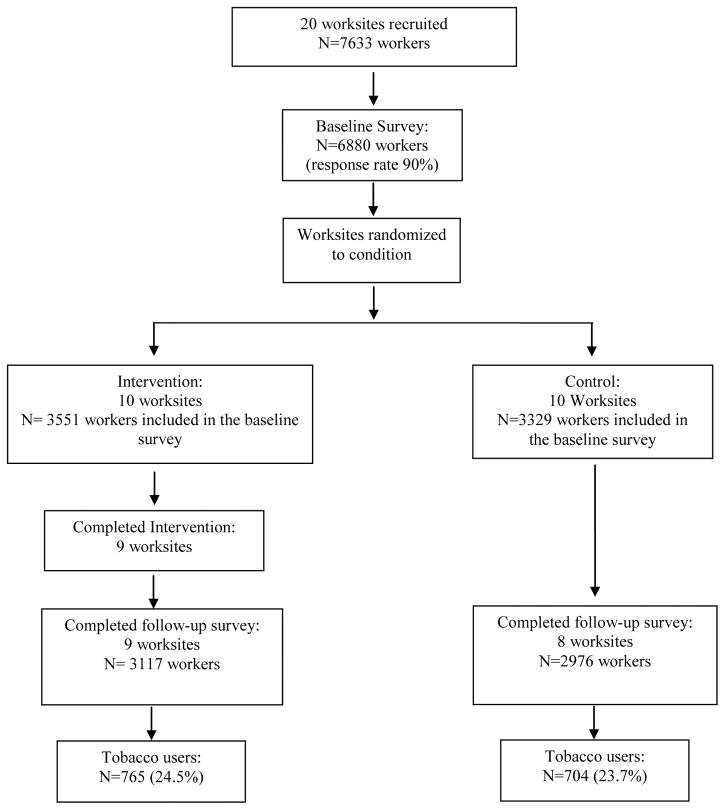
Twenty manufacturing worksites that employed 7633 workers were recruited to the study on a rolling basis. A total of 6880 workers (90.1%) responded to the baseline survey. Three of the 20 worksites did not complete the study (1 intervention and 2 control). As per the protocol, all workers present on the day of the follow-up survey were invited to participate in the survey. Based on the number of workers included on the worksite rosters, at baseline, the estimated response rate in these 9 Intervention worksites was 89.6% (3362/3753), and in 8 Control worksites, 91.2% (2776/3043). At follow-up, the number of workers in each worksite changed due to turnover as well as new workers joining the workforce; we did not, however, have access to updated numbers of total employees. A total of 3117 workers in the nine intervention worksites and 2976 workers in the eight control worksites participated in the follow-up survey. Among those completing the follow-up survey, 765 (24.5%) from the intervention worksites and 704 (23.7%) from control worksites reported they were tobacco users at the beginning of the intervention, and were included in the analysis of cessation. (See Figure 1.)
Figure 1.
Participant flow
Sample Characteristics
Socio-demographic characteristics of workers in the two groups were comparable at baseline, with no statistically significant differences (data not shown). At baseline in the 20 worksites, the tobacco use rates were 24.8% in intervention worksites and 20.0% in control worksites (p=0.44). We compared the baseline sample characteristics and tobacco use prevalence between worksites that completed the study and those that dropped out (data not shown); there were no significant differences in tobacco use prevalence (23.1% in worksites completing the study, 21.2% in the three that dropped out) and in most other co-variates; where differences were significant, the magnitude of the difference was small (e.g., workers in worksites completing the study were slightly older, somewhat more likely to be employed for more than a year, and somewhat more likely to be married compared to those in sites that dropped out). There were no differences in the socio-demographic characteristics of respondents to the follow-up survey between intervention and control worksites (see Table 2).
Table 2.
Participants characteristics by intervention group among participants in the final survey in the 9 intervention and 8 control worksites
| Intervention among participants in follow-up survey (N=3117) | Control among participants in follow-up survey (N=2976) | P value* | |
|---|---|---|---|
| Age | 37.4 (± 11.09) | 36.9 (± 10.13) | 0.92 |
| Gender | 0.70 | ||
| Male | 2971 (95.3%) | 2765 (92.9%) | |
| Female | 146 (4.7%) | 211 (7.1%) | |
| Worker status | 0.65 | ||
| Production workers | 2348 (79.7%) | 2312 (79.3%) | |
| Non Production workers | 597 (20.3%) | 602 (20.7%) | |
| Tenure at worksite | 0.97 | ||
| Less than 1 year | 317 (10.2%) | 348 (11.7%) | |
| 1 year or more than 1 year | 2788 (89.8%) | 2623 (88.3%) | |
| Economic wellbeing | 0.651 | ||
| Both refrigerator and vehicle | 1566 (50.6%) | 1188 (40.3%) | |
| Either refrigerator or vehicle | 759 (24.5%) | 892 (30.3%) | |
| None | 767 (24.8%) | 867 (29.4%) | |
| Education | 0.392 | ||
| None – 6th standard | 251 (8.1%) | 251 (8.4%) | |
| 7th – 10th standard | 1013 (32.5%) | 1090 (36.7%) | |
| 12th standard or diploma | 914 (29.4%) | 925 (31.1%) | |
| graduation + | 935 (30.0%) | 705 (23.7%) | |
| Marital status | 0.47 | ||
| Currently married | 2379 (76.4%) | 2385 (80.3%) | |
| Currently not married | 733 (23.6%) | 585 (19.7%) |
Adjusted for the clustering of workers in worksites.
Comparing none vs. all others
Comparing graduation + vs. all others
Intervention delivery
Based on the analysis of the process tracking data, seven of the 10 intervention worksites implemented all six planned health education events; two worksites implemented two events, and one worksite did not conduct any event and dropped out of the study. For the intervention for managers, the tobacco policy consultation was implemented in all 10 intervention worksites; one of the ten worksites refused the OSH consultation.
Tobacco use cessation
As shown in Table 3, the intervention resulted in a doubling of the 6-month cessation rates among workers in the intervention worksites compared to those in the control; this difference in rates was not statistically significant for the overall sample (OR=1.81; p=0.13) or for production workers only (OR=2.29; p=0.07). The within-worksite correlation was 0.10. The magnitude of the difference in 30 day quit rates between the two groups was comparable to the 6 month rates and was statistically significant for production workers (OR=2.25, p=0.03), although not for the sample overall (OR=1.70; p=0.12).
Table 3.
Tobacco use cessation by Intervention Group in the 9 intervention worksites and 8 control worksites completing the Follow-up Survey
| Intervention | Control | OR | 95% CL | |
|---|---|---|---|---|
|
|
||||
| Total workers: | n=765* | n=704* | ||
| 6M quitters | 63 (8.2%) | 34 (4.8%) | 1.81 | 0.85 – 3.89 |
| 30 day quitters | 132 (17.3%) | 78 (11.1%) | 1.70 | 0.87 – 3.32 |
| Production workers | n=604 | n=579 | ||
| 6M quitters | 49 (8.1%) | 23 (4.0%) | 2.29 | 0.93 – 5.65 |
| 30 day quitters | 109 (18.0%) | 54 (9.3%) | 2.25 | 1.07 – 4.70 |
| Non-production workers | n=124 | n=114 | ||
| 6M quitters | 11 (8.9%) | 11 (9.7%) | 0.93 | 0.36 – 2.37 |
| 30 day quitters | 18 (14.5%) | 23 (20.2%) | 0.67 | 0.34 – 1.33 |
37 participants in Intervention group and 11 participants in Control group were missing for worker status.
We computed a post-hoc analysis of the power to detect a between-group difference in this study, using the observed six-month cessation data. The within-worksite correlation for the resulting sample was 0.10 and the quit rate in the control group was 4.8%. Given these findings, the actual power of the study to detect the observed quit rate in the intervention group, 8.4%, as significantly different from that in the control group was 21%. The final sample size provided 80% power to detect a difference of 10 percentage points between the two groups.
Discussion
There is an increasing need for evidence-based interventions to address the rising public health epidemic related to tobacco use in LMICs. This study used a cluster-randomized design to test the efficacy of a worksite intervention designed to promote tobacco control among manufacturing workers in Mumbai. We hypothesized that the intervention would result in increased tobacco use cessation among workers, particularly production workers, in worksites randomly assigned to receive the intervention, compared to those in the control group. We found a doubling of quit rates between intervention and control worksites among production workers; this difference was statistically significant for 30-day quit rates but not for six-month sustained cessation.
To our knowledge, this is the first worksite tobacco control study in India using a rigorous randomized controlled design that has demonstrated the efficacy of a worksite intervention for workers’ tobacco use cessation. Nonetheless, there is an emerging literature exploring the potential of worksite approaches to reducing risks associated with non-communicable diseases (NCDs). For example, Prabhakaran and colleagues reported that a worksite intervention program to reduce cardiovascular disease (CVD) risk factors among employees of six industrial worksites was successful in reducing overall CVD risk, and reported significant reductions in mean body weight, waist circumference, blood pressure, serum cholesterol, and plasma glucose levels in the intervention group relative to the control.19 Thakur and colleagues described the development and feasibility of a 12-month intervention in three industries to address the physical work environment, psychosocial work environment and promoting healthy behavior, with a particular focus on NCD risk factors. Others have used oral cancer screening for individual workers to promote cessation. 33–36 This manuscript contributes to this emerging literature on the potential efficacy of workplace interventions designed to improve behaviors associated with NCD risk, such as tobacco control.
Nonetheless, we did encounter challenges in integrating this tobacco control intervention with occupational safety and health efforts. The health and wellbeing of production workers are significantly influenced by their exposures on the job, and the burden of these exposures is on the rise in LMICs.37–39 Within the public health community, it is important that we take a comprehensive view of the factors influencing worker health, considering the duality of intersecting factors that shape health outcomes – including risk-related behaviors such as tobacco use as well as the potential for exposures to hazards on the job. This comprehensive approach necessitates the participation of multiple stakeholders, including business and labor leaders, policy makers who may be able to ensure implementation of legislation designed to protect and promote worker health, and the public health research and advocacy communities, whose voices can shape research and policy directions.
These findings may be limited because they rely on self-reported tobacco use. We took numerous precautions to minimize reporting bias, including use of anonymous surveys, use of separate intervention and survey staff, and informing workers that the results would only be communicated in the aggregate and that no personal information would be provided to their employer. Biochemical validation of cessation was not feasible in this population-based study conducted in a worksite setting in which the appearance of drug testing would be unwelcome; in addition, other reports in India have found that biochemical assessments may have low sensitivity in detecting use of smokeless tobacco, especially prevalent in this population.40,41 In addition, because of the influx of new workers, the cessation rates include those workers who were only partially exposed to intervention, possibly diluting the final results. Also, we estimated our response rate at baseline using rosters provided by the worksites, which may have been incomplete; at follow-up, we were unable to calculate the response rate because we do not have adequate information about the accurate denominators.
This study was underpowered to detect the difference in six-month quit rates observed here. Our power was compromised by the loss of three sites, including one intervention site and two control sites. In addition, although we estimated the six-month quit rate in the intervention group accurately for our power calculations, we underestimated both the quit rate in the control group and the within-worksite correlation. With increasing awareness of the harms of tobacco use, tobacco use cessation is slowly increasing in India. Future studies in India will need to be powered to appropriately take into consideration an increasing rate of quitting likely to be observed as part of the secular trend. Also, although these results may have relevance beyond the Mumbai, we acknowledge that generalizability may be restricted to similar manufacturing worksites in this region.
This study used a rigorous randomized design, with worksites as the unit of intervention and randomization; the analyses controlled for the clustering of respondents within worksites. This study was implemented with manufacturing workers who face dual risks related to occupational hazards and are likely to have higher rates of tobacco use than white-collar workers. The intervention was designed to address tobacco control in a comprehensive manner, with the additional focus on occupational safety and health based on recent recommendations from WHO, NIOSH and others.21–24 This study demonstrates the feasibility and potential efficacy of implementing a tobacco control intervention in a challenging setting, requiring support from management as well as a committed team of health educators who traveled sometimes long distances to worksites and offered intervention events across shifts to ensure broad access. Despite the challenges to implementation, the intervention was delivered as planned in a majority of sites.
In conclusion, this worksite intervention resulted in a doubling of tobacco use cessation among production workers, providing an innovative and effective response to the rising need for evidence-based tobacco control interventions in India. Few evidence-based approaches are currently available to inform the creation of an infrastructure to support tobacco use cessation. This randomized trial is of particular importance because it was effective in promoting tobacco use cessation among production workers, where prevalence rates are especially high. This study also points to the ongoing need to strengthen the occupational safety and health infrastructure within Indian worksites, which may provide a useful platform for broad-based initiatives to support workers’ safety and health, including through tobacco control. This study points to important next steps for future worksite interventions with important implications for policy-makers within India as well as more broadly in LMICs.
What this paper adds.
What is already known
Blue-collar workers are more likely to use tobacco than white-collar workers, a disparity that is consistently observed in both high-income countries such as the U.S. and low- and middle income countries, such as India.
Workplace interventions that integrate health promotion with occupational safety and health have been shown to increase tobacco use cessation rates for blue-collar workers in the U.S.
With its large population and high prevalence of multiple forms of tobacco use, India represents an important case example of the need for interventions to redress disparities in tobacco use by occupation.
Important gaps
There is a significant need to address the accelerating use of tobacco in low- and middle-income countries and to attend to disparities in tobacco use in these areas.
Prevalence of quitting is low in India, and few supports are available for those wanting to quit.
There is little evidence to inform worksite-based tobacco control interventions in low- and middle income countries, including in India.
What this study adds
This worksite intervention resulted in a doubling of tobacco use cessation among production workers.
As a result of this study, we now know that a worksite tobacco control intervention that builds on a company’s occupational safety and health infrastructure can successfully improve tobacco use cessation rates among production workers in Indian manufacturing worksites.
Acknowledgments
Funding
This study was funded by the National Cancer Institute, Grant number R01 CA140304 and K05CA10866.
Dr. Sorensen expresses appreciation for the support of the Rockefeller Foundation and its Bellagio Center Academic Writing Residency, which provided time and space for preparing the first draft of this manuscript. The authors wish to thank the numerous investigators and staff members in India and USA who contributed to this study, including from USA, Linnea Benson-Whelan, Ellen Connorton, Diane Chen, Josh Gagne, Tarub Mabud, Taylor Schwartz, Clara Setiawan, Melanie Silverman, Shamaila Usmani, K. Viswanath, Lorraine Wallace and the Health Communication Core, Dana-Farber Cancer Institute (www.healthcommcore.org); and from India, Sameer Narake, Mayuri Sawant, Juhi Gautam, Nirmal Ahuja, Bharti Prabhakar, Ravi Govande, V. N. Prabhu, and Ashish Mishra. In addition, this work could not have been completed without the participation of the 22 worksites in Mumbai, participants in the formative research conducted to plan this study, the study’s scientific advisory board, and Healis-Sekhsaria Health Educators and staff.
Footnotes
Contributions of the authors: All authors certify that they have contributed substantially to: (1) the conception and design or analysis and interpretation of data, (2) the drafting or revision of the manuscript, and (3) the approval of the final version.
Glorian Sorensen was the Principal Investigator for the study, ensured that the study maintained rigorous scientific standards, conceptualized the manuscript and was responsible for drafting the manuscript, incorporating the co-authors’ input, and finalizing the draft; she is responsible for the overall content as guarantor.
Mangesh Pednekar was responsible for oversight of day-to-day study operations in India, and contributed to writing the manuscript.
Laura Shulman Cordeira was the U.S. Project Director for the study, contributed to conceptualizing and planning the intervention, and contributed to writing the paper.
Pratibha Pawar was responsible for planning and implementation of the process tracking and analyzed these data for the paper; she also contributed to management of the field operations, and contributed to writing the manuscript.
Eve Nagler was responsible for planning the intervention, contributed to quality control for study implementation, and contributed to writing the paper.
Anne M. Stoddard was the lead biostatistician for the study, contributed to overall decisions about study design and implementation, and contributed to writing the paper.
Hae-Young Kim conducted the analyses for the paper and contributed to writing the paper.
Prakash C. Gupta was the Co-Principal Investigator of the study and the lead investigator in India. He contributed to overall study design and planning, and to conceptualizing and writing the paper.
References
- 1.Siddiqi K, Newell J, Robinson M. Getting evidence into practice: what works in developing countries? Int J Qual Health Care. 2005;17:447–54. doi: 10.1093/intqhc/mzi051. [DOI] [PubMed] [Google Scholar]
- 2.McMichael C, Waters E, Volmink J. Evidence-based public health: what does it offer developing countries? J Public Health (Oxf) 2005;27:215–21. doi: 10.1093/pubmed/fdi024. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-free Environments. Available at: http://www.who.int/tobacco/mpower/2009/en/index.html.; Secondary WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-free Environments. 2009a Available at: http://www.who.int/tobacco/mpower/2009/en/index.html.
- 4.Sharma DC. India’s welcome to foreign tobacco giants prompts criticism. The Lancet. 1998;352:1204. doi: 10.1016/S0140-6736(05)60546-6. [DOI] [PubMed] [Google Scholar]
- 5.Stewart BW, Kleihues P, editors. World Cancer Report. Lyon, France: IARC Press; 2003. [Google Scholar]
- 6.International Institute for Population Sciences. Global Adult Tobacco Survey (GATS) India 2009–2010. New Delhi: Ministry of Health and Family Welfare, Government of India; 2010. [Google Scholar]
- 7.Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358:1137–47. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 8.Sinha DN, Palipudi KM, Gupta PC, et al. Smokeless tobacco use: A meta-analysis of risk and attributable mortality estimates for India. Indian J Cancer. 2014;51(Suppl):S73–7. doi: 10.4103/0019-509X.147477. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Tobacco or health: A global status report: Country profiles by region. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 10.Reddy KS, Gupta PC. Report on Tobacco Control in India. New Delhi, India: Ministry of Health and Family Welfare, Government of India; 2004. [Google Scholar]
- 11.Gupta PC, Ray CS, Murti PR, et al. Rising incidence of oral cancer in Ahmedabad City. Indian J Cancer. 2014;51:67–72. doi: 10.4103/0019-509X.147476. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Tobacco Free Initiative. MPower brochures. http://www.who.int/tobacco/mpower/publications/en/index.html.; Secondary Tobacco Free Initiative. MPower brochures. 2011 http://www.who.int/tobacco/mpower/publications/en/index.html.
- 13.Beaglehole R, Bonita R, Alleyne G, et al. NCDs: celebrating success, moving forward. Lancet. 2011;378:1283–4. doi: 10.1016/S0140-6736(11)61559-6. [DOI] [PubMed] [Google Scholar]
- 14.Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–47. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 15.National Cancer Institute. Center for Global Health. http://www.cancer.gov/aboutnci/globalhealth.; Secondary Center for Global Health. 2011 http://www.cancer.gov/aboutnci/globalhealth.
- 16.Thakur JS, Bains P, Kar SS, et al. Integrated healthy workplace model: An experience from North Indian industry. Indian J Occup Environ Med. 2012;16:108–13. doi: 10.4103/0019-5278.111750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reddy KS, Prabhakaran D, Chaturvedi V, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–69. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahuja R. [Last accessed on 2010 Jul 1];Healthy workplace in corporate sector, India; Confederation of Indian Industry. 2007 Feb; Available From: http://whoindia.org/EN/Section20/Section29_1414.htm.
- 19.Prabhakaran D, Jeemon P, Goenka S, et al. Impact of a worksite intervention program on cardiovascular risk factors: a demonstration project in an Indian industrial population. J Am Coll Cardiol. 2009;53:1718–28. doi: 10.1016/j.jacc.2008.12.062. [DOI] [PubMed] [Google Scholar]
- 20.Bloom DE, Cafiero ET, Jané-Llopis E, et al. The Global Economic Burden of Noncommunicable Diseases. Geneva: 2011. [Google Scholar]
- 21.Burton J. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices. 2010 http://apps.who.int/iris/bitstream/10665/113144/1/9789241500241_eng.pdf?ua=1.
- 22.Schill AL, Chosewood LC. The NIOSH Total Worker Health program: an overview. J Occup Environ Med. 2013;55:S8–11. doi: 10.1097/JOM.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 23.Health Canada. Workplace Health System. http://www.hc-sc.gc.ca/ewh-semt/pubs/occup-travail/index-eng.php#work.
- 24.Guazzi M, Faggiano P, Mureddu GF, et al. Worksite health and wellness in the European Union. Prog Cardiovasc Dis. 2014;56:508–14. doi: 10.1016/j.pcad.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Sorensen G, Stoddard A, Hunt MK, et al. The effects of a health promotion-health protection intervention on behavior change: The WellWorks Study. Am J Public Health. 1998;88:1685–90. doi: 10.2105/ajph.88.11.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sorensen G, Stoddard A, LaMontagne A, et al. A comprehensive worksite cancer prevention intervention: Behavior change results from a randomized controlled trial in manufacturing worksites (United States) Cancer Cause Control. 2002;13:493–502. doi: 10.1023/a:1016385001695. [DOI] [PubMed] [Google Scholar]
- 27.Sorensen G, Quintiliani L, Pereira L, et al. Work experiences and tobacco use: findings from the gear up for health study. J Occup Environ Med. 2009;51:87–94. doi: 10.1097/JOM.0b013e31818f69f8. [DOI] [PubMed] [Google Scholar]
- 28.Cordeira LS, Pednekar MS, Nagler EM, et al. Experiences recruiting Indian worksites for an integrated health protection and health promotion randomized control trial in Maharashtra, India. Health Educ Res. 2015 doi: 10.1093/her/cyv010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sorensen G, Pednekar MS, Sinha DN, et al. Effects of a tobacco control intervention for teachers in India: results of the Bihar school teachers study. Am J Public Health. 2013;103:2035–40. doi: 10.2105/AJPH.2013.301303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caban-Martinez AJ, Davila EP, Zhao W, et al. Disparities in hypertension control advice according to smoking status. Prev Med. 2010;51:302–6. doi: 10.1016/j.ypmed.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gutmann LB, Sobell LC, Prevo MH, et al. Outcomes research methodology of smoking cessation trials (1994–1998) Addictive Behaviors. 2004;29:441–63. doi: 10.1016/j.addbeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 32.Sorensen G, Gupta PC, Pendnekar MS. Social disparities in tobacco use in Mumbai, India: The roles of occupation, education and gender. Am J Public Health. 2005;95:1003–08. doi: 10.2105/AJPH.2004.045039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mishra GA, Majmudar PV, Gupta SD, et al. Workplace tobacco cessation program in India: A success story. Indian J Occup Environ Med. 2009;13:146–53. doi: 10.4103/0019-5278.58919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pimple S, Pednekar MS, P M, et al. Predictors of quitting tobacco-results of a worksite tobacco cessation service program among factory workers in Mumbai, India. Asian Pac J Cancer Prev. 2012;13:533–38. doi: 10.7314/apjcp.2012.13.2.533. [DOI] [PubMed] [Google Scholar]
- 35.Pimple S, Pednekar MS, Mazumdar P, et al. An Integrated Approach to Worksite Tobacco Use Prevention and Oral Cancer Screening Among Factory Workers in Mumbai, India. Asian Pac J Cancer Prev. 2012;13:527–32. doi: 10.7314/apjcp.2012.13.2.527. [DOI] [PubMed] [Google Scholar]
- 36.Mishra GA, Majmudar PV, Gupta SD, et al. Call centre employees and tobacco dependence: Making a difference. Indian J Cancer. 2010;47(Suppl S1):43–52. doi: 10.4103/0019-509X.63860. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization. Global strategy on occupational health for all: The way to health at work. Recommendations of the Second Meeting of the WHO Collaborating Centres in Occupational Health; Ocotber 11–14; Beijing, China. 1995. [Google Scholar]
- 38.Hogstedt C, Wegman DH, Kjellstrom T. The Consequences of Economic Globalization on Working Conditions, Labor Relations, and Worker’s Health. In: Kawachi I, Wamala S, editors. Globalization and Health. Oxford: Oxford University Press; 2007. pp. 138–57. [Google Scholar]
- 39.Benach J, Muntaner C, Santana V. Final Report to the WHO: Commission on Social Determinants of Health (CSDH) Employment Conditions Knowledge Network (EMCONET); 2007. http://www.who.int/social_determinants/resources/articles/emconet_who_report.pdf?ua=1. [DOI] [PubMed] [Google Scholar]
- 40.Balhara YP, Jain R, Sundar AS, et al. Use of cotinine urinalysis to verify self-reported tobacco use among male psychiatric out-patients. Lung India : official organ of Indian Chest Society. 2012;29:217–20. doi: 10.4103/0970-2113.99102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dhavan P, Bassi S, Stigler MH, et al. Using salivary cotinine to validate self-reports of tobacco use by Indian youth living in low-income neighborhoods. Asian Pac J Cancer Prev. 2011;12:2551–4. [PMC free article] [PubMed] [Google Scholar]