Highlights
-
•
Duplication cysts seen commonly in the pediatric population is a rare entity in the elderly.
-
•
Surgical resection is necessary due to possible complications.
-
•
Laparoscopic management aids early recovery and minimum morbidity.
Abstract
Introduction
Gastrointestinal duplication cysts are rare, generally found in infants and young adults. Adult presentation is rare.
Presentation of the case
We present an elderly lady who presented with right iliac fossa pain. Imaging showed a terminal ileal duplication cyst. Laparoscopic right hemicolectomy was done.
Histopathology confirmed ileal duplication cyst with reactive appendicitis.
Discussion
Surgical resection is deemed appropriate management due to known complications like obstruction, hemorrhage, perforation and malignant degeneration. Resection of only the cyst is adequate in completely isolated cases. However, others require resection of adjoining small bowel.
Conclusion
We highlight the rare occurrence in elderly and its management laparoscopically.
1. Introduction
Gastrointestinal duplication cysts are rare and generally manifest in the pediatric age group with acute abdomen. The entity is rare in adults with only few cases reported so far. They may arise anywhere in the alimentary tract from the mouth to the anus. They are connected to the bowel with a well-defined muscular coat and characteristically lined by gastrointestinal mucosa. Adults are generally asymptomatic or may have vague abdominal symptoms [1]. Obstruction, hemorrhage, perforation and malignancy may complicate the condition. We present here one such rare case of terminal ileal duplication cyst with reactive appendicitis in an elderly lady that was managed laparoscopically.
2. Presentation of the case
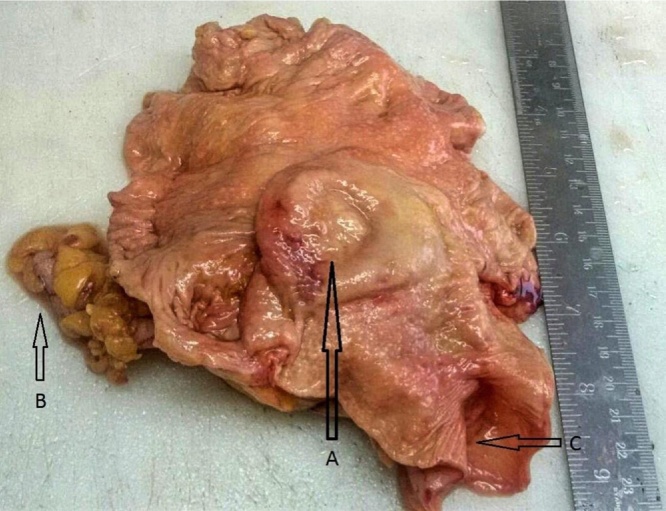
A 61 years lady presented with generalized abdominal pain, on and off since 6 months that was conserved with oral medications (antibiotics and analgesics) but had increased in severity in the last two months. There was no associated vomiting, fever or change in bowel or bladder habits. Her physical examination was unremarkable except for mild tenderness in the right iliac fossa. She had an elevated leukocyte count (14,000cu/mm3). Ultrasonography (USG) of the abdomen done at another institue showed a cystic structure in the right lower abdomen. We further evaluated her with a Computed Tomography (CT) that revealed a well-defined cystic bilobed lesion (7.6 × 4.7 × 3.5 cm) extending from the intramural portion of the medial wall of the caecum to immediately posterior to the ileocaecal junction with multiple enlarged ileocaecal mesenteric lymph nodes (Fig. 1A & 1B). The Appendix was seen separately. The findings were suggestive of an ileocaecal duplication cyst with secondary infection. Intraoperatively, a mass was found just proximal to the ileocaecal junction adherent to the surrounding mesentery with multiple enlarged mesenteric lymph nodes. A laparoscopic right hemi-colectomy with side to side stapled anastomosis was done. Grossly on cut opening the specimen, a bulging cyst at the terminal ileum measuring 5.5 × 5 cm, filled with clear mucoid fluid. It had a flat lining with a focally granular appearance (Fig. 2). Histopathology confirmed a terminal ileal duplication cyst(Fig. 3) with reactive appendicitis and reactive follicular hyperplasia in the involved lymph nodes. The cyst was non-communicating with the lumen. The cyst lining was found to be columnar with villiform projections lined by columnar foveolar type gastric epithelium but no inflammation on high and low resolution (Fig. 4A&B). No malignant degeneration was seen. The post-operative period was uneventful and the patient was discharged after five days. The patient is on regular follow-up and symptom free.
Fig. 1.
A Contrast Enhanced CT scan (coronal view) showing a well-defined bilobed cystic lesion (7.6 × 4.7 × 3.5 cm) involving ileocaecal junction.
B Contrast Enhanced CT scan (axial view) showing the cystic lesion non-communicating with the lumen.
Fig. 2.
Gross specimen showing collapsed cyst (non communicating) in the lumen of terminal ileum, Appendix seen.
Fig. 3.
A Microphotograph of the duplication cyst H & E stain, 40 x magnification, showing the ileal mucosa below and the gastric mucosa showing foveolar epithelium with mucous glands beneath. A muscle wall is seen in between which is partially fibrosed.
B Microphotograph of the Appendix showing the reactive follicles suggesting appendicitis.
Fig. 4.
A 400 x resolution histopathology slide showing cyst wall lined by columnar foveolar type gastric epithelium and at places thrown into villiform projections. No goblet cells are seen. Sub-epithelium shows mucous glands.
B 100 x resolution showing gastric mucous lining characterized by columnar foveolar type gastric epithelium. Sub-epithelium shows multiple mucous glands.
3. Discussion
Duplication cyst is a rare congenital anomaly presenting in pediatric patients that is most commonly seen in the ileum [2]. It was first described by Wendel [3]. There have been few cases of its presentation in adults reported ever since. The condition is usually seen in males. A number of etiological theories have been suggested, of which persistence of the fetal gut diverticula or ‘aborted Gemini’, and defect in the recanalization of the primitive gut are the most accepted. Any failure in the transition process of the intestinal tract from solid to tubular state between 6 and 8 weeks of intrauterine life may lead to the formation of duplication cysts [4]. These cysts have an outer muscular lining with an inner gastrointestinal lining. They are generally intra-abdominal; however intra-thoracic and thoraco-abdominal duplication cysts are also encountered. As these congenital malformations share a common blood supply with adjoining gastrointestinal tract, its complete excision may demand resection-anastomosis of adjoining gastrointestinal tract.
Duplication cysts are most commonly diagnosed in early life between 1- 2 years of age with intestinal obstruction or a palpable mass. In adults, the condition may be left undiagnosed. Commonly, they present with vague abdominal complaints. However, they may also present acutely in the setting of obstruction, hemorrhage or perforation [5]. Due to the risk of progression from benign pathology to malignancy or other complication, surgery should be offered, preferably minimally invasive approach to all symptomatic or asymptomatic patients. Rarely, the cyst may cause a fistula with the adjoining structure [6]. Duplication cysts may be associated with malrotation, esophageal duplication and vertebral anomalies [3], [7]. A cyst may be termed as a true duplication cyst if it fulfills the three criteria: attachment to any part of the gastrointestinal tract, lined by any gastrointestinal epithelium and containing smooth muscle in its wall [8]. It may be cystic or tubular. Cystic duplication cysts are commoner. They do not communicate with the bowel, but may share a common wall and blood supply. Tubular duplication cysts communicate with the intestinal lumen [8].
The preoperative diagnosis can be made on USG and CT. The cystic nature of the lesion is visible on USG. The diagnosis can be confirmed even on USG if the characteristic inner echogenic layer and the hypoechogenic outer muscular layer can be defined [2]. Kumar et al. proposed a ‘five layered cyst wall’ sign seen on ultrasonography delineating the outermost hyperechoic serosa, hypoechoic muscularis propria, hyperechoic submucosa, hypoechoic muscularis mucosa and the innermost hyperechoic mucosa [9]. CT scan shows the fluid filled cystic structures or the tubular structures with slightly enhancing walls in close proximity to the small bowel. Endoscopic ultrasound may also be used for the evaluation of duplication cysts. Surgery is imperative in symptomatic patients. There is no data available for the management in asymptomatic patients. However, it is deemed beneficial to surgically treat these cases due to the possible malignant change in duplication cysts [10]. Surgery entails resecting the involved bowel, however, in completely isolated cysts; excision of these may be done without resecting the bowel. Ileal duplication cysts are known to show heterotropic gastric mucosa [11].
Amongst the adult cases presented so far, some had degenerative changes in the cyst leading to malignancy. Table 1 gives a brief overview of the same. Our case did not show any such degenerative changes.
Table 1.
Overview of reported duplication cysts in adults.
| S. No. | Author | Age/Sex and relevant findings. | Diagnosis | Lap/open |
|---|---|---|---|---|
| 1 | Collaud S et al. [12]. | Adult, right lower abdomen pain. Pre-op imaging showed infected cyst. | Completely isolate ileal duplication cyst with low grade mucinous cystadenoma. | – |
| 2. | Isamu Hoshino et al. [13]. | Adult, abdominal pain. CT showed cystic mass in the small bowel with intussusception, Hepatic and renal cysts also present | Ileal duplication cyst | Laparotomy with small bowel resection and anastomosis. |
| 3. | Tomas et al. [14]. | Adult, asymptomatic with past history of bilateral breast cancer, CT: non communicating cystic lesion in the terminal ileum | Mucinous cystadenoma in isolated ileal duplication cyst(on antimesenteric side) | Surgical resection. |
| 4. | Otter M.I. et al. [15]. | 52yrs/M, urinary symptoms. | Intestinal duplication cyst. | Surgical resection. |
| 5. | Smith J.H. et al. [16]. | Adult | Ileal duplication cyst with carcinoid tumor | Surgical resection. |
| 6. | Kim H.S. et al. [17]. | 19yrs/F, rt. Upper quadrant pain, CT showing ileocolic intussusception with cystic mass at tip. | Ileal duplication cyst. | Surgical resection. |
| 7. | Gregor Blank et al. [18]. | 51yrs/M, asymptomatic. | Ileal duplication cyst with adenocarcinoma. | Surgical resection of cyst without bowel resection. |
4. Conclusion
We highlight the rare occurrence of terminal ileal duplication cyst in the elderly. Surgical treatment is necessary due to the probable malignant transformation of duplication cysts. Laparoscopy adds on the advantage of minimally invasive approaches. Though rare, a differential diagnosis of duplication cyst should be considered in adult patients with cystic lesions of or in proximity to gastro-intestinal tract.
Conflict of interest
None.
Funding
None.
Ethical approval
Ethics Committee, Lilavati Hospital and Research Center.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor - in - Chief of this journal on request.
Author contribution
Kamal Yadav and Priyanka Sali wrote the paper.
Bhushan Bhole analyed the data.
Hitesh Mehta and Chandralekha Tampi performed the study.
Guarantor
Kamal Yadav.
Hitesh Mehta.
Contributor Information
Kamal S. Yadav, Email: dockamalyadav@gmail.com.
Priyanka A. Sali, Email: drpriyankasali@gmail.com.
Bhushan Bhole, Email: drbhushanbhole@yahoo.co.in.
Chandralekha Tampi, Email: chandralekhatampi@gmail.com.
Hitesh Mehta, Email: drhiteshmehtaa0aa@gmail.com.
References
- 1.Kuo H.C., Lee H.C., Shin C.H., Sheu J.C., Chang P.Y., Wang N.L. Clinical spectrum of alimentary tract duplication in children. Acta Paediatr. Taiwan. 2004;45(2):85–88. [PubMed] [Google Scholar]
- 2.Kim Y., Kim Y., Jeong Y., Moon W., Gwak H. Ileal duplication cyst: y-configuration on in vivo sonography. J. Pediatr. Surg. 2009;44(7):1462–1464. doi: 10.1016/j.jpedsurg.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Ríos S.S., Noia J.L., Nallib I.A. Adult gastric duplication cyst: diagnosis by endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) Rev. Esp. Enferm. Dig. 2008;100(9):586–590. doi: 10.4321/s1130-01082008000900011. [DOI] [PubMed] [Google Scholar]
- 4.Teele R.L., Henschke C.I., Tapper D. The radiographic and ultrasonographic evaluation of enteric duplication cysts. Pediatr. Radiol. 1980;10(1):9–14. doi: 10.1007/BF01644338. [DOI] [PubMed] [Google Scholar]
- 5.Shah A., Du J., Sun Y., Cao D. Dynamic change of intestinal duplication in an adult patient: a case report and literature review. Case Rep. Med. 2012;2012:1–3. doi: 10.1155/2012/297585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islah M.A.R., Hafizan T. Perforated ileal duplication cyst presenting with right iliac fossa pain mimicking perforated appendicitis. Med. J. Malaysia. 2008;63(1):63–64. [PubMed] [Google Scholar]
- 7.Srivastava P., Gangopadhyay A., kumar V., Upadhyaya V., Sharma S., Jaiman R. Noncommunicating isolated enteric duplication cyst in childhood. J. Pediatr. Surg. 2009;44(7):e9–e10. doi: 10.1016/j.jpedsurg.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 8.Habib K., Khan M., Sheehan A., Coker O. Adenocarcinoma in ileal duplication cyst: case report and review of literature. Open Med. 2009;4(3) [Google Scholar]
- 9.Kumar D., Ramanathan S., Haider E., Khanna M., Otero C. Gastroenterology Revisiting the forgotten sign: five layered gut signature and Y configuration in enteric duplication cysts on high resolution ultrasound. J. Gastroenterol. Hepatol. 2015;30(7) doi: 10.1111/jgh.12903. 1111–1111. [DOI] [PubMed] [Google Scholar]
- 10.Gümüs M., Kapan M., Gümüs H., Önder A., Girgin S. Unusual noncommunicating isolated enteric duplication cyst in adults. Gastroenterol. Res. Pract. 2011;2011:1–3. doi: 10.1155/2011/323919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler D., Liu R. Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc. Ultrasound. 2014;3(3):152. doi: 10.4103/2303-9027.138783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collaud S., Bayerl C., Wille G., Zehnder A., Grieder F., Meili S. Mucinous cystadenoma arising in a completely isolated infected ileal duplication cyst. S. Afr. J. Surg. 2012;50(2):45–46. [PubMed] [Google Scholar]
- 13.Hoshino I., Maruyama T., Fukunaga T., Matsubara H. Intussusceptions associated with an ileal duplication cyst. Intern. Med. 2011;50(11) doi: 10.2169/internalmedicine.50.5213. 1255–1255. [DOI] [PubMed] [Google Scholar]
- 14.Tomas D., Zovak M., Čiček S., Šulentić P., Jukić Z., Krušlin B. Mucinous cystadenoma arising in an isolated ileal duplication cyst. J. Gastrointest. Cancer. 2007;38(2-4):127–130. doi: 10.1007/s12029-008-9023-1. [DOI] [PubMed] [Google Scholar]
- 15.Otter M., Marks C., Cook M. An unusual presentation of intestinal duplication with a literature review. Digest. Dis. Sci. 1996;41(3):627–629. doi: 10.1007/BF02282353. [DOI] [PubMed] [Google Scholar]
- 16.Smith J.H., Hope P.G. Carcinoid tumor arising in a cystic duplication of the small bowel. Arch. Pathol. Lab. Med. 1985;109(1):95–96. [PubMed] [Google Scholar]
- 17.Kim H., Sung J., Park W., Kim Y. An ileal duplication cyst manifested as an ileocolic intussusception in an adult. Turk. J. Gastroenterol. 2015;25(1):196–198. doi: 10.5152/tjg.2014.4011. [DOI] [PubMed] [Google Scholar]
- 18.Blank G., Königsrainer A., Sipos B., Ladurner R. Adenocarcinoma arising in a cystic duplication of the small bowel: case report and review of literature. World J. Surg. Oncol. 2012;10(1):55. doi: 10.1186/1477-7819-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]