Highlights
-
•
Be aware of the rare occasion of PE in patients with intestinal obstruction without other etiological factors.
-
•
Preoperative diagnosis of PE may be impossible.
-
•
Management of PE in case of intestinal obstruction requires urgent surgery.
Keywords: Peritoneal encapsulation, Congenital peritoneal membrane, Case report intestinal obstruction
Abstract
Introduction
Peritoneal Encapsulation (PE) is a scarce congenital malformation, characterized by a supplementary peritoneal membrane that covers all or a part of the small intestine.
Presentation of case
PE was unexpectantly discovered in a young woman during laparotomy for bowel obstruction. There were no specific pre-operative indications of this malformation. The operation was uneventful.
Discussion
PE is a very rare congenital anatomical anomaly that is difficultly identified pre-operatively. PE is mainly asymptomatic, but in some cases, like in the presented one, PE presents with small bowel obstruction. Surgeons should be aware of this malformation and suspect it when encountering a patient with small bowel obstruction without other etiological factors.
Conclusion
Knowledge of this peculiar congenital anomaly is pivotal, so that accurate diagnosis and appropriate management of it are direct and efficient.
1. Introduction
Peritoneal Encapsulation (PE) is a very rare congenital malformation, characterized by a supplementary peritoneal membrane that covers partially or totally the small intestine [1], [2]. The majority of cases of PE remain asymptomatic and diagnosed accidentally during autopsy and/or surgery [3], [4]. Nevertheless, in some cases, as in the presented one, PE presents with small bowel obstruction [1], [2], [4], [5], [6].
2. Case report
A 28-year-old female referred to the Emergency Department presenting diffuse and intense abdominal pain within the last 8 h, associated with nausea for the last 12 h. At the admission she was afebrile and with normal vital signs. Physical examination revealed a fixed asymmetrical distension of the abdomen and deep pain on palpation in the left upper quadrant of the abdomen, associated with hard consistency and signs of peritoneal irritation. Blood test results of the patient were in the normal spectrum.
The patient had past history of a birth with caesarean section 3 years ago, and an episode of intense colicky abdominal pain of unknown origin a year ago. During that previous episode, she mentioned that exploratory laparoscopy was performed. Laparoscopy did not reveal any pathology of the abdomen and she was managed conservatively. No more investigation had been conducted till she proceeded to our institution.
Subsequent abdominal radiograph revealed distension of small bowel loops with multiple air-fluid levels. Abdominal CT revealed small bowel loops nestled against the left side of the abdomen, dilatation of the small intestine and features of intestinal obstruction (Fig. 1). Exploratory laparotomy was immediately performed.
Fig. 1.
Axial CT images showing intestinal obstruction and converged to the left side of the abdominal cavity small bowel loops.
Intraoperatively, a thin membrane was discovered in the left upper quadrant of the abdominal viscera encasing all the small intestine (Fig. 2). The accessory peritoneal membrane, was located between the parietal peritoneum and the posterior abdominal wall and it had the appearance of a supplementary peritoneal capsule through which the ‘trapped’ small bowel loops were visible (Fig. 3). The membrane added pressure on the small intestine loops and specifically on a loop of the terminal ileum, causing small bowel obstruction. Immediate excision of the accessory peritoneal membrane released the intestinal loops into the peritoneal cavity and subsequently allowed better bowel mobility (Fig. 4). Intestinal resection was not required since the small intestine was normal in appearance and had active peristalsis. The operation was uneventful and the patient was discharged the 7th postoperative day without complications.
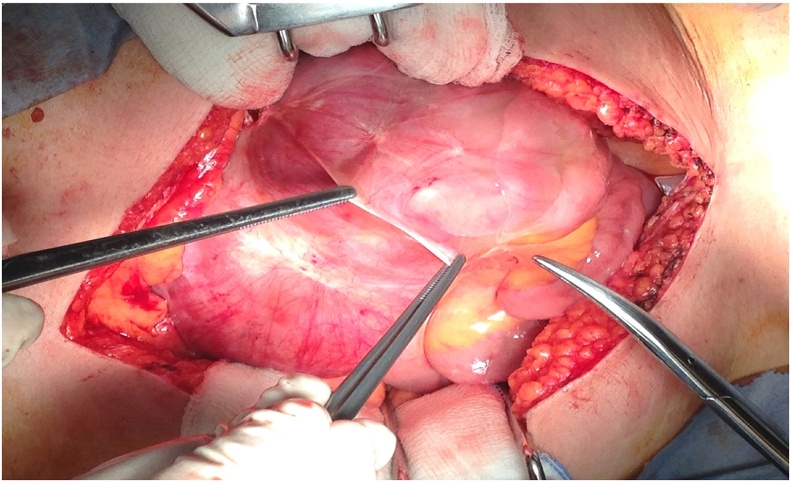
Fig. 2.
The peritoneal capsule discovered intraoperatively.
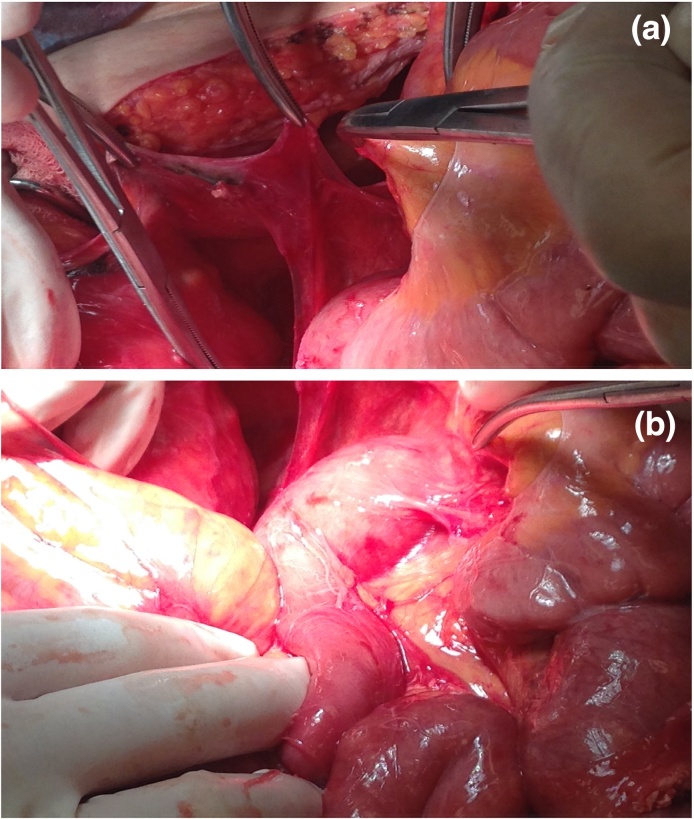
Fig. 3.
The bowel loops into the peritoneal capsule.
Fig. 4.
Excision of the peritoneal capsule. The small bowel loops were released into the peritoneal cavity.
3. Discussion
PE was first described by Cleland in 1868 [7]. It is a peculiar congenital anatomical anomaly, characterized by an accessory peritoneal membrane covering all or part of the small bowel [1], [2]. This peritoneal membrane is laterally attached to the ascending and descending colon, superiorly the transverse colon and inferiorly the posterior surface of the parietal peritoneum [3]. It may cover the entire small intestine or part of it from the Trietz angle till the ileocolic junction [1], [4]. The great omental-if it is present-it covers the membrane but it is utterly separated from it [2], [4], [5], [8].
PE is believed to be caused by abnormal return of the small intestine in the abdominal cavity of the fetus during the 12th fetal week. Subsequently, the yolk’s sac coat migrates with the intestine, rather than staying in the umbilical pedicle [2] and causes the formation of an additional peritoneal membrane [3]. PE can occur with other congenital anomalies as well. More specifically, it can occur with incomplete situs inversus and congenital epigastric hernia [6].
The definition of the true incidence of PE has been hindered due to the failure to distinguish this condition from Abdominal Cocoon, which is an idiopathic condition and Sclerosing Encapsulating Peritonitis [8], which is a chronic inflammatory disease [9]. Nevertheless, there are no more than 50–60 reported cases of PE [10].
Most of the PE cases remain asymptomatic and diagnosed accidentally during autopsy and/or surgery [3], [4] but in some cases, like in the present one, PE presents with small bowel obstruction [1], [2], [4], [5], [6].
Patients with bowel obstruction due to PE, present with clinical signs such as asymmetrical abdominal distension, differences in consistency on abdominal palpation [3], [11] as in the presented case and vomiting. Clinical symptoms that patients may mention are nausea and intense abdominal pain [2]. Some patients may have episodes of intermittent abdominal pain or sub-acute bowel obstruction episodes, prior to the final diagnosis of PE [3], [12]. In the present case, the patient probably had a sub-acute bowel obstruction episode the year before proceeding to our institution according to her medical history.
Preoperative diagnosis of PE may be impossible [1] since the radiological findings are usually normal or non-specific in case of intestinal obstruction [1], [2] like in the presented case. Nevertheless, X-ray, ultrasonography, CT of the abdomen and barium study may contribute to preoperative diagnosis of PE [8], [10], [12], [13].
Management of PE in case of intestinal obstruction requires urgent surgery, that includes excision of the congenital membrane and lysis of the adhesions among the loops [4] as performed in the presented case. PE has a high survival rate after operation, with low recurrence [11].
4. Conclusion
PE is a peculiar congenital anomaly, nearly never diagnosed or even suspected preoperatively [2]. Surgeons should be aware of this malformation and suspect it when encountering a patient with small bowel obstruction without other etiological factors. Thus, knowledge of this malformation is pivotal in order to establish an accurate diagnosis and for the appropriate management of it.
Key learning points:
-
•
Be aware of the rare occasion of PE in patients with intestinal obstruction without other etiological factors.
-
•
Preoperative diagnosis of PE may be impossible.
-
•
Management of PE in case of intestinal obstruction requires urgent surgery.
Conflict of interest
None.
Consent
Written consent for the publication of this case report and accompanying images was obtained from the patient. The consent can be provided to the Editor if he asks so.
Ethical approval
This is a Case Report for which the patient provided informed consent.
Funding
There is no source of funding.
Authors’ contributions
Mariolis conceived of the study and participated in its coordination. Zoulamoglou contributed to the gathering of the data and the preparation of images. Zarokosta carried out the literature review. Piperos, Kalles, Tsiaousis, Kaklamanos and Sgantzos contributed to the preparation of the manuscript. Flessas was senior consultant in charge of this case report. Zoulamoglou, Mariolis and Flessas contributed to the refinement of the case report. All authors have approved the final article.
Guarantor
The Guarantor who is responsible for the present case report is Theodoros Mariolis-Sapsakos. He Conceived of the study, he had access to the data and participated in study’s coordination.
Contributor Information
Menelaos Zoulamoglou, Email: m.zoulamoglou@gmail.com.
Ioannis Flessas, Email: iflessas@gmail.com.
Maria Zarokosta, Email: mzarokosta@gmail.com.
Theodoros Piperos, Email: theo.piperos@gmail.com.
Vasileios Kalles, Email: vassilis_kalles@yahoo.gr.
Ioannis Tsiaousis, Email: jtsiaoussis@med.uoc.gr.
Ioannis Kaklamanos, Email: ikakla@med.uoa.gr.
Markos Sgantzos, Email: sgantzos@med.uth.gr.
Theodoros Mariolis-Sapsakos, Email: theodorosmariolis@yahoo.gr.
References
- 1.Teixeira D., Costa V., Costa P., Alpoim C., Correia P. Congenital peritoneal encapsulation. World J. Gastrointest. Surg. 2015;7(8):174–177. doi: 10.4240/wjgs.v7.i8.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naraynsingh V., Maharaj D., Singh M., Ramdass M.J. Peritoneal encapsulation: a preoperative diagnosis is possible. Postgrad. Med. J. 2001;77:725–726. doi: 10.1136/pmj.77.913.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Taan O.S., Evans M.D., Shami J.A. An asymptomatic case of peritoneal encapsulation: case report and review of the literature. Cases J. 2010;3:13. doi: 10.1186/1757-1626-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sherigar J.M., McFall B., Wali J. Peritoneal encapsulation: presenting a small bowel obstruction in an elderly woman. Ulster Med. J. 2007;76:42–44. [PMC free article] [PubMed] [Google Scholar]
- 5.Chew M.H., Sophia Hadi I., Chang G., Ong H.S., Wong W.K. A problem encapsulated: the rare encapsulation syndrome. Singap. Med. J. 2006;47:808–810. [PubMed] [Google Scholar]
- 6.Ince V., Dirican A., Yilmaz M., Barut B., Ersan V., Yilmaz S. Peritoneal encapsulation in a patient with incomplete situs inversus. J. Coll. Phys. Surg. Pak. 2012;22(10):659–660. doi: 10.2012/JCPSP.659660. [DOI] [PubMed] [Google Scholar]
- 7.Browne L.P., Patel J., Guillerman R.P., Hancon I.C., Cass D.L. Abdominal cocoon: a unique presentation in an immunodeficient infant. Pediatr. Radiol. 2012;42:263–266. doi: 10.1007/s00247-011-2135-y. [DOI] [PubMed] [Google Scholar]
- 8.Naidoo K., Kinoo Mewa S., Singh B. Hindawi Publishing Corporation CRS; 2013. Small Bowel Injury in Peritoneal Encapsulation Following Penetrating Abdominal Trauma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akbulut S. Accurate definition and management of idiopathic sclerosing encapsulating peritonitis. World J. Gastroenterol. 2015;21(2):675–687. doi: 10.3748/wjg.v21.i2.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wani I., Wani K.A., Wani M., Bhat G., Shah M. Peritoneal encapsulation, left paraduodenal hernia with retroperitonealization of inferior mesenteric vein leading to triple obstruction. IJCRI. 2013;4(3):169–174. [Google Scholar]
- 11.Rajagopal A.S., Rajagopal R. Conundrum of the cocoon: report of a case and review of the literature. Dis. Colon Rectum. 2003;46:1141–1143. doi: 10.1007/s10350-004-7295-5. [DOI] [PubMed] [Google Scholar]
- 12.Shamsuddin S., Bilal M., Rehman B., Najeeb E., Faisal S. Peritoneal encapsulation presenting as small bowel obstruction in a 16 year old girl. J. Ayub Med. Coll. Abbottabad. 2012;24(July–December(3–4)):215. [PubMed] [Google Scholar]
- 13.Mitrousias V., Alexiou E., Katsanas A., Batzalexis K., Germanos S. The helix sign in the peritoneal encapsulation syndrome: a new sign in a rare cause of bowel obstruction? J. Gastrointest. Liver Dis. 2015;24(June (2)):144. doi: 10.15403/jgld.2014.1121.242.hlx. [DOI] [PubMed] [Google Scholar]