Abstract
Little is known about the cardiovascular effects of modest weight loss. To determine whether weight losses limited to 5–10 % are sufficient to produce cardiovascular health benefits, data from 401 overweight and obese adults who enrolled in a behavioral weight loss program from 2003 to 2011 were analyzed. Primary outcomes were changes in fasting glucose, triglycerides, and cholesterol. Patients who lost 5–10 % showed significant reductions in triglycerides, total cholesterol, and low-density lipoprotein (LDL) cholesterol. Patients who lost >10 % experienced significantly greater improvements in triglycerides, total cholesterol, and LDL cholesterol than patients losing less. For higher-risk patients, those who lost 5–10 % significantly reduced fasting glucose, triglycerides, and total cholesterol; those who lost >10 % improved on all risk factors (except HDL cholesterol) and to a significantly greater degree than those losing less. Five to 10 % weight losses produced improvements in cardiovascular risk factors, but greater weight losses were associated with even greater improvement.
Keywords: Obesity, Weight loss, Cardiovascular disease, Risk factors
Obesity remains an important public health concern given its widespread prevalence and association with risk for developing chronic disease [1]. Obesity places individuals at greater risk for health complications such as heart disease, stroke, diabetes, hypertension, dyslipidemia, metabolic syndrome, respiratory problems, and some types of cancer [2, 3]. There is evidence that even modest weight loss (e.g., 5–10 %) can reduce cardiovascular disease risk even when the patient remains in the obese range [4–8]. Based on these findings, current guidelines recommend a 5–10 % loss of starting weight as an initial goal as a means of obtaining the health benefits of weight loss [9–12] and a weight loss of 5 % or more is one of the benchmarks used by the Food and Drug Administration in evaluating potential obesity medications [13].
Most of the evidence supporting the benefits of modest weight loss is derived from studies reporting average change in risk factors among groups with average weight loss in the 5–10 % range [5–7]. This does not directly address the effects of weight losses limited to 5–10 %. Participants losing greater amounts of weight (i.e., greater than 10 %) may positively skew the average improvement in cardiovascular risk factors. Additionally, most of the available data are derived from highly controlled research studies, which limit generalizability.
Only a few studies have investigated the effects of varying degrees of modest weight loss directly. Among patients who had formerly lost weight on a very low calorie diet (VLCD), at 3-year follow-up, both those who initially lost 5–9 % and those who initially lost ≥10 % of their baseline weight maintained improvements in fasting glucose and triglycerides, but only the latter group showed reductions in systolic and diastolic blood pressure [14]. One-year data in the Look AHEAD trial with diabetic participants showed that weight loss limited to 5–10 % was associated with significant improvements in cardiovascular risk factors, with even greater improvements achieved by those who lost more than 10 % of their starting weight [15]. Among a small sample of hypercholesterolemic women who had lost weight in an intensive 48-week program, subjects maintaining a 5–10 % loss and those with <5 % loss both showed significant reductions from baseline in triglycerides, but only those maintaining a >10 % loss showed significant improvement in total and low-density lipoprotein (LDL) cholesterol [16].
The current study extends these findings by assessing the benefits of varying degrees of modest weight loss among a heterogeneous sample of participants in a relatively short-term, moderate-intensity, community-based obesity treatment program. We hypothesized that participants who lost 5–10 % of their initial body weight would significantly improve their cardiovascular health and that greater weight losses would yield even more significant improvements.
METHODS
Patients
We examined archival data from 604 adult patients who consecutively enrolled, from 2003 to 2011, in a comprehensive, individually delivered lifestyle change program at the Weight Management Center at the Medical University of South Carolina (MUSC). This retrospective analysis was deemed exempt from review by the MUSC Institutional Review Board.
Because assessment of risk factor changes required data from laboratory tests at the beginning and end of the program, patient data were included only if the patient (1) completed the program and (2) had pre-treatment and post-treatment laboratory data on at least one risk factor. As in previous studies, we defined program completion as attending at least 50 % of the program visits with attendance spanning at least 70 % of the program’s standard duration [17–19]. In the present program, this represented attendance at eight or more visits including some attendance at or beyond visit 11. Excluding data from patients who did not complete the program and/or those missing risk factor data produced a sample of 401 patients.
The sample was primarily female (79.8 %) and Caucasian (82.5 %), consistent with our overall patient population. Mean weight was 97.67 kg (SD = 21.30), mean BMI was 35.1 (SD = 7.39), and mean age was 47.7 years (SD = 13.4). At entry, 45 patients (11.2 %) were diabetic based on either self-reported type 2 diabetes or baseline fasting glucose ≥126 mg/dl. Additional baseline patient characteristics can be found in Table 1.
Table 1.
Cardiovascular risk factor values, pre-treatment and post-treatment
| Variables | N | Pre-treatment (M ± SD) | Post-treatment (M ± SD) | p a | η p 2 | Correlation of Δ with percent weight loss | P b |
|---|---|---|---|---|---|---|---|
| Weight (kg) | 401 | 97.67 ± 21.30 | 88.40 ± 19.41 | <.001 | .788 | – | – |
| BMI (kg/m2) | 377 | 35.10 ± 7.39 | 31.77 ± 6.86 | <.001 | .771 | – | – |
| Glucose | 359 | 99.28 ± 23.75 | 96.21 ± 18.17 | .001 | .032 | – | – |
| Women | 287 | 97.76 ± 22.65 | 95.46 ± 18.07 | – | – | −.037 | .269 |
| Men | 72 | 105.20 ± 26.97 | 99.18 ± 18.38 | – | – | .233 | .025 |
| Triglyceridesc | 358 | 120.37 ± 76.67 | 91.12 ± 52.84 | <.001 | .276 | – | – |
| Women | 286 | 109.69 ± 58.28 | 90.85 ± 53.80 | – | – | .262 | <.001 |
| Men | 72 | 162.40 ± 116.52 | 92.18 ± 49.21 | – | – | .213 | .037 |
| Total cholesterolc | 357 | 192.40 ± 36.12 | 171.75 ± 32.10 | <.001 | .323 | – | – |
| Women | 286 | 194.64 ± 33.65 | 176.37 ± 29.92 | – | – | .330 | <.001 |
| Men | 71 | 183.55 ± 43.69 | 153.15 ± 34.03 | – | – | .279 | .010 |
| LDL cholesterol | 358 | 118.21 ± 31.53 | 105.75 ± 28.06 | <.001 | .175 | – | – |
| Women | 286 | 120.01 ± 29.70 | 108.35 ± 26.57 | – | – | .217 | <.001 |
| Men | 72 | 110.78 ± 37.48 | 95.44 ± 31.47 | – | – | .414 | <.001 |
| HDL cholesterol | 358 | 50.21 ± 14.62 | 47.60 ± 13.75 | .001 | .033 | – | – |
| Women | 286 | 52.79 ± 14.36 | 49.81 ± 13.60 | – | – | .123 | .019 |
| Men | 72 | 40.04 ± 10.77 | 38.81 ± 10.49 | – | – | −.055 | .325 |
Note that significant changes and correlations are indicated by italicized p values. Percent weight loss was coded as a positive value, and risk factors were coded as negative values. Effect sizes indicated by partial eta-squared (η p 2); .04, .25, and .64 indicate weak, moderate, and strong effects, respectively [20]
aPre-treatment versus post-treatment, two-way repeated measure ANOVA
bPearson’s bivariate correlations, percent weight change with change in each cardiovascular risk factor, gender-specific
cRisk factors for which there were significant time by gender interactions
Measures
Patients’ weights were obtained weekly using a Mettler-Toledo Panther digital scale. Blood samples were obtained after 12-h fasts prior to enrollment and again about 2 weeks before the end of the program. Fasting glucose, triglycerides, total cholesterol, LDL cholesterol, and high-density lipoprotein (HDL) cholesterol were chosen as markers of cardiovascular disease risk. Fasting glucose, triglycerides, total cholesterol, and HDL cholesterol were all directly measured; LDL cholesterol was calculated using the following formula: LDL = total cholesterol − HDL cholesterol − (triglycerides/5). Blood pressure data were not consistently available due to staff availability and scheduling issues; thus, blood pressure was not included among the other cardiovascular risk factors.
Weight loss program
The Focus weight loss program is a fee-for-service program offered by the Weight Management Center at the Medical University of South Carolina. This program was self-selected by each patient. The 15-week program combines one-on-one visits with a registered dietitian, exercise physiologist, or psychology staff according to the treatment protocol. Visits are brief (15–30 min) and include review of dietary and exercise records, behavioral goal attainment, review of specific lifestyle change topics, and behavioral goal setting for the following week. The diet for the first 8 weeks consists of three nutrition bars (averaging 150 kcal/each) and two to three nutrition shakes (averaging 180 kcal/each), plus one structured food-based meal. The nutrition shakes were obtained from Health Management Resources (Boston, MA) and the nutrition bars from both Robard Corporation (Mt. Laurel, NJ) and HealthWise (Grovetown, GA). Macronutrient content of both shakes and bars were balanced with moderate carbohydrates (about 45 %), protein (about 30 %), and fat (about 25 %). During the rest of the program, patients are placed on an all-food or mostly food-based (limited use of meal replacements) diet of approximately 1200 kcal/day. Throughout the program, patients are expected to engage in daily self-monitoring of dietary intake, weight (including graphing), and activity/exercise (pedometers). Patients are encouraged to work toward meeting nationally recommended guidelines for physical activity (150 min of moderate-vigorous physical activity per week). However, weekly physical activity goals were individualized to take into account starting activity level and capacity.
Statistical analyses
Data were analyzed using SPSS 21 statistical software. Weight loss was computed as the difference between the participant’s baseline weight (visit 1) and weight at the last week of attendance. Weight loss was analyzed as absolute change in weight and as percent of baseline weight. Two-way repeated measure analysis of variance (ANOVA) tests assessed pre-post-changes in weight and each of the cardiovascular risk factors and whether these changes differed between men and women. Pearson’s bivariate correlations were computed between percent weight loss and risk factor changes. Analysis of covariance (ANCOVA) tests examined the effect of amount of weight loss on amount of risk factor change while controlling for the effects of baseline risk factor values, baseline BMI, gender, and age. Significant main effects were further explored with Tukey’s HSD post hoc tests between pairs of weight loss groups.
These analyses were again conducted separately for patients initially at higher risk initially, i.e., those whose screening values on that risk factor were outside recommended limits (fasting glucose >100 mg/dl, triglycerides >150 mg/dl, total cholesterol >200 mg/dl, LDL cholesterol >160 mg/dl, or low HDL cholesterol <50 mg/dl for women and <40 mg/dl for men) [21–23]. Lastly, Pearson’s chi-squared analyses were used to test whether the amount of weight loss affected the number of higher-risk patients who achieved normalized risk factor values by the end of the weight loss program.
RESULTS
Mean weight loss over the course of the program was 9.26 kg (SD = 4.99) and 9.38 % (SD = 4.42 %) of baseline weight. Both men and women lost a significant amount of weight, but men lost significantly more weight than did women, F (1, 399) = 86.78, p < .001 (11.51 vs. 8.85 %, respectively). For the entire sample, significant reductions (ps < .001) were seen on weight, fasting glucose, triglycerides, total cholesterol, LDL cholesterol, and (although undesirable) HDL cholesterol. In the case of triglycerides and total cholesterol, men experienced greater reductions than women (see Table 1). Correlation coefficients were calculated between percent weight loss and change in risk factors. Results indicated that, with a few exceptions, the improvement in risk factor status was significantly related to the degree of weight loss (see Table 1).
Relation of degree of weight loss to level of risk factor improvement
Patients were divided into the following weight loss groups: <5 % (N = 59), 5–10 % (N = 153), and >10 % (N = 183). Six patients who gained weight over the program were eliminated from all analyses examining differences between weight loss groups. There were no differences between the weight loss groups on baseline BMI or on any of their baseline risk factor values, for men or women. However, all baseline risk factor values differed significantly between men and women; thus, effects of gender were analyzed where sample sizes allowed.
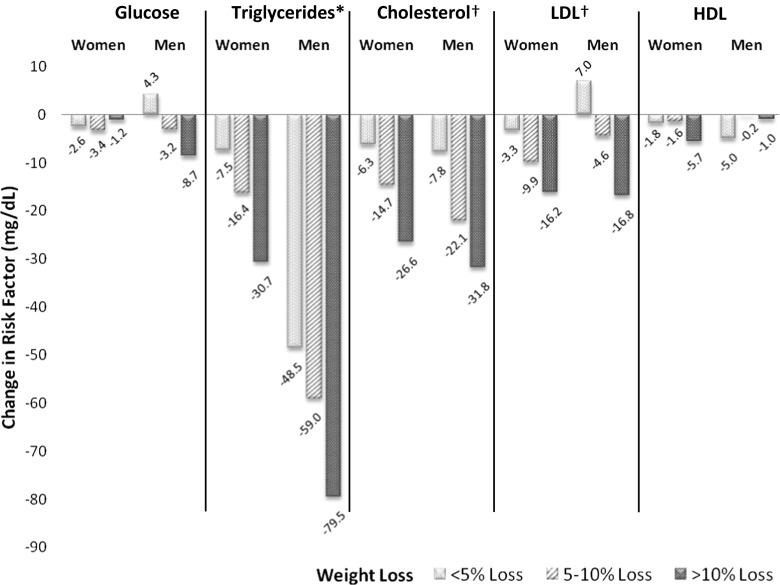
Patients who lost <5 % of their starting weight experienced a significant reduction only in triglycerides (see Fig. 1). Patients who lost 5–10 % of their starting weight showed significant reductions in total cholesterol, LDL cholesterol, and triglycerides, with men experiencing a greater reduction than women on triclycerides. Patients who lost >10 % of their weight saw significant reductions in all five risk factors, including HDL cholesterol, an undesirable change. In this group, men had greater reductions in fasting glucose and triglycerides than women while the reverse was true for HDL cholesterol.
Fig. 1.
Change in risk factors by weight loss group and gender. Asterisk indicates that after adjusting for baseline triglyceride value, baseline BMI, gender, and age, losing >10 % decreased triglycerides significantly more than losing 5–10 %, which in turn decreased triglycerides more than losing <5 % (p < .05). Dagger indicates that after adjusting for effects of baseline risk factor values, baseline BMI, gender, and age, losing >10 % decreased risk factor values significantly more than losing 5–10 and <5 %, with no other differences (p < .05)
In direct comparisons of the three weight loss groups, patients with >10 % weight loss had greater improvements in triglycerides, total cholesterol, and LDL cholesterol than did both patients with <5 % loss and those with 5–10 % loss. Further, patients who lost 5–10 % had greater reductions in triglycerides than patients who lost <5 %. There were no other differences across weight loss groups.
Changes among patients with higher-risk baseline values
Additional analyses were conducted for each risk factor including only patients who had higher-risk baseline levels of that particular risk factor (see Table 2). Among these patients, significant reductions (ps < .001) were seen for fasting glucose, triglycerides, total cholesterol, and LDL cholesterol; there was no change in HDL cholesterol. Furthermore, men experienced greater reductions on triglycerides and total cholesterol than women. Correlations between weight loss and risk factor change were generally consistent with those seen with the entire sample, with degree of change in risk factor related to degree of weight loss, although less significantly so.
Table 2.
Cardiovascular risk factor values, pre-treatment and post-treatment, for patients with higher-risk values at baseline
| Variables | N | Pre-treatment (M ± SD) | Post-treatment (M ± SD) | p a | η p 2 | Correlation of Δ with percent weight loss | P b |
|---|---|---|---|---|---|---|---|
| Weight (kg) | 325 | 98.56 ± 21.40 | 89.16 ± 19.51 | <.001 | .784 | – | – |
| BMI (kg/m2) | 307 | 35.45 ± 7.41 | 32.07 ± 6.86 | <.001 | .764 | – | – |
| Glucose | 119 | 120.11 ± 30.62 | 106.77 ± 24.40 | <.001 | .191 | – | – |
| Women | 86 | 119.09 ± 30.28 | 107.31 ± 25.18 | – | – | −.031 | .388 |
| Men | 33 | 122.78 ± 31.75 | 105.36 ± 22.55 | – | – | .284 | .054 |
| Triglyceridesc | 85 | 225.36 ± 88.72 | 142.40 ± 66.39 | <.001 | .538 | – | – |
| Women | 57 | 203.52 ± 55.75 | 150.09 ± 70.65 | – | – | .242 | .035 |
| Men | 28 | 268.32 ± 121.57 | 126.75 ± 54.59 | – | – | .281 | .074 |
| Total cholesterolc | 150 | 225.85 ± 21.18 | 194.16 ± 25.05 | <.001 | .494 | – | – |
| Women | 127 | 224.93 ± 19.49 | 196.07 ± 24.15 | – | – | .339 | <.001 |
| Men | 23 | 230.54 ± 28.21 | 183.61 ± 27.82 | – | – | .243 | .132 |
| LDL cholesterol | 32 | 173.50 ± 14.88 | 140.50 ± 26.64 | <.001 | .510 | – | – |
| Women | 25 | 172.50 ± 14.52 | 138.36 ± 28.60 | – | – | .318 | .061 |
| Men | 7 | 177.25 ± 16.65 | 148.14 ± 17.51 | – | – | .101 | .414 |
| HDL cholesterol | 170 | 39.10 ± 6.48 | 38.84 ± 8.05 | .422 | .004 | – | – |
| Women | 129 | 41.23 ± 5.71 | 41.02 ± 7.67 | – | – | .066 | .229 |
| Men | 41 | 32.65 ± 3.88 | 32.00 ± 4.70 | – | – | −.238 | .067 |
Note that significant changes and correlations are indicated by italicized p values. Percent weight loss was coded as a positive value, and risk factors were coded as negative values. Effect sizes indicated by partial eta-squared (η p 2); .04, .25, and .64 indicate weak, moderate, and strong effects, respectively [20]
aPre-treatment versus post-treatment, two-way repeated measure ANOVA
bPearson’s bivariate correlations, percent weight change with change in each cardiovascular risk factor, gender-specific
cRisk factors for which there were significant time by gender interactions
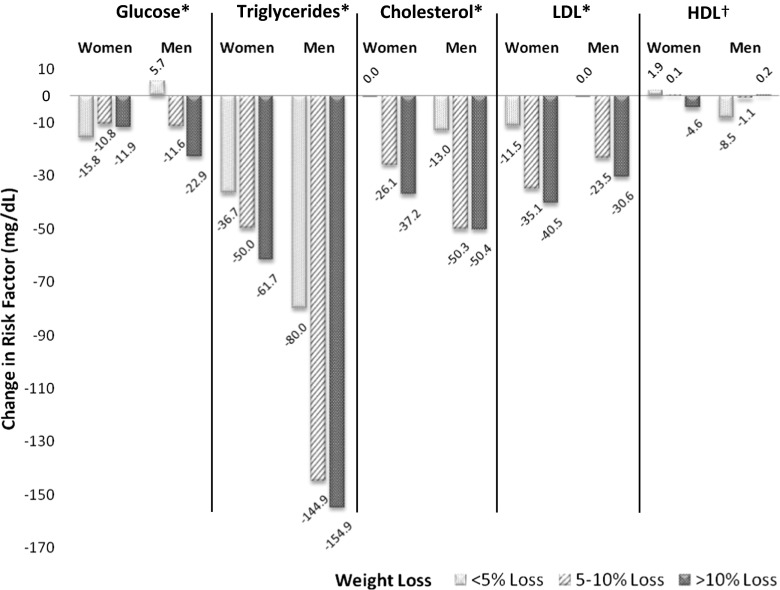
Patients with higher-risk baseline risk factor values who lost <5 % had significant reductions only in total cholesterol (Fig. 2). Those who lost 5–10 % showed significant improvements in fasting glucose, total cholesterol, and triglycerides, with men showing greater improvement than women on triglycerides, but no change in LDL or HDL cholesterol. Higher-risk patients who lost >10 % achieved significant improvements in all of their respective risk factors except HDL cholesterol. Again, for triglycerides, men experienced greater reductions than women.
Fig. 2.
Change in risk factors by weight loss group and gender, among patients with elevated baseline risk factors. Asterisk indicates that after adjusting for effects of baseline risk factor values, baseline BMI, gender, and age, losing >10 % decreased risk factor values significantly more than losing 5–10 and <5 %, with no other differences (p < .05). Dagger indicates that after adjusting for effects of baseline HDL value, baseline BMI, gender, and age, there was a significant time by sex interaction (p < .05)
Comparing weight loss groups within these high-risk patients showed that those who lost >10 % experienced greater reductions in fasting glucose, triglycerides, and total and LDL cholesterol than did either high-risk patients who lost 5–10 % or those who lost <5 %, even after controlling for baseline risk factor values, baseline BMI, gender, and age. For HDL cholesterol, men’s post-treatment HDL cholesterol was higher with greater weight loss, while women’s HDL cholesterol was lower with greater weight loss. There were no other differences across weight loss groups.
We calculated the number of higher-risk patients who attained normal risk factor levels after having started with higher-risk baseline values of the respective risk factor. Small sample sizes in some of the subgroups precluded significance testing. However, as can be seen in Table 3, with all risk factors other than HDL cholesterol, the percent of patients who normalized their risk factor levels increased with increased weight loss.
Table 3.
Risk factor normalization by weight loss group, for patients with higher-risk values at baseline
| Risk factor | <5 % | 5–10 % | >10 % | |||
|---|---|---|---|---|---|---|
| N a | Percent normalized (N) | N a | Percent normalized (N) | N a | Percent normalized (N) | |
| Glucose | 15 | 26.7 % (4) | 42 | 38.1 % (16) | 57 | 52.6 % (30) |
| Triglycerides | 8 | 12.5 % (1) | 28 | 50 % (14) | 49 | 71.4 % (35) |
| Total cholesterol | 19 | 15.8 % (3) | 56 | 44.6 % (25) | 73 | 74 % (54) |
| LDL cholesterol | 4 | 50 % (2) | 10 | 70 % (7) | 18 | 77.8 % (14) |
| HDL cholesterol | – | – | – | – | – | – |
| Womenb | 20 | 15 % (3) | 51 | 21.6 % (11) | 56 | 7.1 % (4) |
| Men | 2 | 0 % (0) | 11 | 9.1 % (1) | 28 | 3.6 % (1) |
aNumber of patients with high baseline risk factor values on that specific risk factor who ended up losing either <5, 5–10, or >10 % of their starting weight
bNote that due to the significant weight loss group by gender interaction for HDL cholesterol, those data are presented separately by gender
DISCUSSION
Interpretation of results
Consistent with previous reports, patients who lost an average of nearly 10 % of their initial weight experienced significant reductions on all risk factors examined: fasting glucose, triglycerides, total cholesterol, LDL cholesterol, and HDL cholesterol (an undesirable change). However, when the sample was subdivided according to amount of weight loss, patients losing only 5–10 % showed improvement on only three risk factors (triglycerides, total cholesterol, and LDL cholesterol), whereas those who lost >10 % showed improvement on all risk factors except HDL. Patients losing <5 % improved only on triglycerides. Further, patients who lost >10 % showed greater improvement on triglycerides, total cholesterol, and LDL cholesterol than did both those losing only 5–10 %, those who lost <5 %.
Improvement on a risk factor is most important for patients at higher risk, so it is noteworthy that numerically greater improvements were generally seen when the risk factor was initially at a higher-risk level. Importantly, a considerable number of patients with initially high-risk values achieved normalized risk factor values at the end of treatment. More than one third of patients with high-risk baseline levels of fasting glucose, triglycerides, total cholesterol, and LDL cholesterol achieved normal ending values on the relevant risk factor.
Within these higher-risk groups, level of risk factor improvement differed as a function of amount lost, with patients losing >10 % reaping the greatest improvements in glucose, triglycerides, total cholesterol, and LDL cholesterol. Patients losing a modest amount of weight (i.e., 5–10 %) showed smaller but significant improvements in fasting glucose, triglycerides, and total cholesterol but no changes in LDL or HDL cholesterol.
The overall decrease in HDL cholesterol in the present study was somewhat disappointing given the commonly assumed benefits of weight loss on this cardio-protective lipoprotein. A systematic review of the effect of weight loss on lipids reported that while the beneficial effects of weight loss on total cholesterol and LDL cholesterol are consistent, their effects on HDL cholesterol are much less consistent [24]. Studies have reported increases [25, 26], no change or decrease [27, 28], and an initial decrease followed by rebound to baseline levels with continued weight loss or maintenance [16].
Limitations
There are a few limitations of our data that are worth noting. First, while comparisons across weight loss groups clearly showed that degree of risk factor improvement was related to amount of weight loss, the improvements seen were not necessarily attributable solely to weight loss. It is not possible to disentangle the effects of weight loss per se from the other impacts of the dietary and exercise changes that the program promoted. Second, our study was limited by the absence of a control group. However, the purpose of this study was not to determine whether the treatment program was more effective than no or different treatment nor to determine whether the treatment program caused improvements in risk factors. Rather, it was to associate given amounts of weight loss with given amounts of risk factor changes. Another limitation is the short-term nature of this study. While the absence of long-term data represents a shortcoming, the examination of the relation of degree of weight loss to risk factor changes occurring within a relatively brief intervention is a novel contribution. Such information is relevant both to clinicians and to patients as a guide to the likely effects of differing amounts of weight loss within a near-term perspective. We were not able to consistently account for medication usage or changes to medications, which may have affected lab results at the end of the program for some patients. Finally, generalizability of our results may be limited. Similar to commercial weight loss programs, our sample consisted of mostly Caucasian females [29]. Additionally, given that our program included meal replacements, our results may not generalize to lifestyle interventions that do not.
Contributions to science
Our findings are consistent with the few prior studies that directly compared risk factor improvements across weight loss categories. However, those studies either reported data from longer-term or more intensive weight loss programs or had more restricted patient samples (e.g., only females or patients with diabetes) [14–16]. The present study extends these findings to a more heterogeneous group of patients in an ongoing, relatively short-term, moderate-intensity obesity treatment program open to the community.
Data supporting claims of health benefits of 5–10 % weight loss have typically been based on sample-wide weight loss averages and sample-wide average improvement in health risk factors. Because of this, it has been unclear whether risk factor improvement might have been positively skewed by individuals losing greater than modest amounts of weight. The present results generally support the common recommendation that 5–10 % weight loss may improve cardiovascular risk factors. At the same time, they show that greater weight losses generally produce greater improvements and may be necessary for normalization of risk factors.
Clinical and public health implications
Our findings point to several potential implications for clinicians and public health. Clinicians providing weight loss treatment may want to encourage small goals to achieve modest weight loss. For many, achieving a body mass index in the “normal” range can be a daunting task. However, psychoeducation around the health benefits of smaller weight losses may provide patients with motivation to reach weight loss goals attainable in the short term. Indeed, there is some evidence to suggest that small changes lead to longer-term, sustained weight losses [30]. On a broader scale, America on the Move (AOM) is a national public health initiative focused on encouraging Americans to make small changes regarding physical activity and calorie intake (e.g., increasing steps by 2000 steps per day and consuming 100 fewer calories per day). Our findings suggest that small changes associated with modest weight losses may decrease significant cardiovascular risk factors and that programs and initiatives targeting individuals on a national level may help to improve the public health impact of this message.
Future directions and conclusions
Future research should attempt to replicate and extend these findings by incorporating a longer-term follow-up period. Additionally, more research is needed to develop more scalable weight loss interventions capable of producing weight loss similar to that in the present study, so that larger segments of the population can participate in them and achieve the health benefits of modest weight loss. In the interim, the present results support the message that weight loss of 5–10 % is good and a greater loss is even better.
Acknowledgments
Preparation for this manuscript was supported in part by the National Cancer Institute under award number R25CA057699, which provided support for Joanna Buscemi during manuscript preparation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with ethical standards
Author’s statement of conflict of interest and adherence to ethical standards
Joshua D. Brown, Joanna Buscemi, Vanessa Milsom, Robert Malcolm, and Patrick M. O’Neil declare that they have no conflict of interest. All procedures were conducted in accordance with ethical standards.
Footnotes
Implications
Practice: Health care providers delivering obesity treatment should provide education to patients regarding the benefits of modest weight loss.
Policy: Resources should be devoted to develop scalable weight loss programs to encourage modest weight loss.
Research: Further research is needed to determine the longer-term effects of modest weight loss on cardiovascular risk factors.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121:21–33. doi: 10.3810/pgm.2009.11.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–2589. doi: 10.1210/jc.2004-0535. [DOI] [PubMed] [Google Scholar]
- 4.Stevens VJ, Obarzanek E, Cook NR, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134:1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 5.Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–1575. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord. 1992;16:397–415. [PubMed] [Google Scholar]
- 7.Vidal J. Updated review on the benefits of weight loss. Int J Obes Relat Metab Disord. 2002;26(Suppl 4):S25–S28. doi: 10.1038/sj.ijo.0802215. [DOI] [PubMed] [Google Scholar]
- 8.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pietrzykowska NB. Benefits of 5–10 percent weight loss. 2014. Available at: http://www.obesityaction.org/wp-content/uploads/Benefits-of-5-10-Percet-Weight-loss.pdf.
- 10.Back to basics for healthy weight loss: healthy weight from the academy. Available at: http://www.eatright.org/Public/content.aspx?id=6847.
- 11.National Heart, Lung and BI. Facts about healthy weight. 2006. Available at: http://www.nhlbi.nih.gov/health/prof/heart/obesity/aim_kit/healthy_wt_facts.pdf. Accessed January 25, 2014.
- 12.Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Found. Circulation. 2004;110(18):2952–2967. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 13.Administration F and D. Guidance for Industry Developing Products for Weight Management. Revision 1 Ed. Rockville, MD; 2007:1–16. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/ucm071612.pdf.
- 14.Mancini M, Di Biase G, Contaldo F, Fischetti A, Grasso L, Mattioli PL. Medical complications of severe obesity: importance of treatment by very-low-calorie diets: intermediate and long-term effects. Int J Obes. 1981;5(3):341–352. [PubMed] [Google Scholar]
- 15.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wadden TA, Anderson DA, Foster GD. Two-year changes in lipids and lipoproteins associated with the maintenance of a 5 % to 10 % reduction in initial weight: some findings and some questions. Obes Res. 1999;7:170–178. doi: 10.1002/j.1550-8528.1999.tb00699.x. [DOI] [PubMed] [Google Scholar]
- 17.Martin CK, O’Neil PM, Binks M. An attempt to identify predictors of treatment outcome in two comprehensive weight loss programs. Eat Behav. 2002;3:239–248. doi: 10.1016/S1471-0153(02)00065-X. [DOI] [PubMed] [Google Scholar]
- 18.Lundgren JD, Malcolm R, Binks M, O’Neil PM. Remission of metabolic syndrome following a 15-week low-calorie lifestyle change program for weight loss. Int J Obes. 2009;33(1):144–150. doi: 10.1038/ijo.2008.225. [DOI] [PubMed] [Google Scholar]
- 19.Lundgren JD, O’Neil PM, Martin CK, Binks M. Smoking status and weight loss in three weight loss programs. Eat Behav. 2006;7(1):61–68. doi: 10.1016/j.eatbeh.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol: Res Pract. 2009;40(5):532–538. doi: 10.1037/a0015808. [DOI] [Google Scholar]
- 21.Cholesterol N, Program E. Third report of the National Cholesterol Education Program (NCEP) expert panel on Detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 22.Genuth S, Alberti KGMM, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26(11):3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 23.Milsom VA, Malcolm RJ, Johnson GC, et al. Changes in cardiovascular risk factors with participation in a 12-week weight loss trial using a commercial format. Eat Behav. 2014;15(1):68–71. doi: 10.1016/j.eatbeh.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Poobalan A, Aucott L, Smith WCS, et al. Effects of weight loss in overweight/obese individuals and long-term lipid outcomes—a systematic review. Obes. Rev. 2004; 5(1):43–50. Available at: http://www.ncbi.nlm.nih.gov/pubmed/14969506. [DOI] [PubMed]
- 25.Wing RR, Jeffery RW. Effect of modest weight loss on changes in cardiovascular risk factors: are there differences between men and women or between weight loss and maintenance? Int J Obes Relat Metab Disord. 1995;19(1):67–73. [PubMed] [Google Scholar]
- 26.Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care. 1998;21(3):350–359. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- 27.Ewbank PP, Darga LL, Lucas CP. Physical activity as a predictor of weight maintenance in previously obese subjects. Obes Res. 1995;3(3):257–263. doi: 10.1002/j.1550-8528.1995.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 28.Thompson PD, Jeffery RW, Wing RR, Wood PD. Unexpected decrease in plasma high density lipoprotein cholesterol with weight loss. Am J Clin Nutr. 1979;32:2016–2021. doi: 10.1093/ajcn/32.10.2016. [DOI] [PubMed] [Google Scholar]
- 29.Gudzune KA, Doshi RS, Mehta AK, et al. Efficacy of commercial weight loss programs: an updated systematic review. Ann Intern Med. 2015;162(7):501–512. doi: 10.7326/M14-2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hills AP, Byrne NM, Lindstrom R, Hill JO. “Small changes” to diet and physical activity behaviors for weight management. Obes Facts. 2013;6:228–238. doi: 10.1159/000345030. [DOI] [PMC free article] [PubMed] [Google Scholar]