Abstract
Lifestyle behaviors across the 24-h spectrum (i.e., sleep, sedentary, and active behaviors) drive metabolic risk. We describe the development and process evaluation of BeWell24, a multicomponent smartphone application (or “app”) that targets behavior change in these interdependent behaviors. A community-embedded iterative design framework was used to develop the app. An 8-week multiphase optimization strategy design study was used to test the initial efficacy of the sleep, sedentary, and exercise components of the app. Process evaluation outcomes included objectively measured app usage statistics (e.g., minutes of usage, self-monitoring patterns), user experience interviews, and satisfaction ratings. Participants (N = 26) logged approximately 60 % of their sleep, sedentary, and exercise behaviors, which took 3–4 min/day to complete. Usage of the sleep and sedentary components peaked at week 2 and remained high throughout the intervention. Exercise component use was low. User experiences were mixed, and overall satisfaction was modest.
Keywords: Physical activity, Exercise, Insomnia, Diabetes, Sitting, mHealth
BACKGROUND
The metabolic syndrome [1] is strongly linked prospectively to diabetes, cardiovascular disease, and mortality [2]. US Veterans are at higher risk for the metabolic syndrome than the general population due to disproportional rates of obesity [3], dyslipidemia [4], and hyperinsulinemia [4]. This disparate burden among Veterans is likely driven by lifestyle behaviors, including insufficient physical activity [3] and poor sleep quality/duration [5]. Sedentary behavior (i.e., sitting/reclining with low energy expenditure [6]) has also emerged as an important and independent risk factor for cardiometabolic health [7]. Although high rates of overweight/obesity have been reported among Veterans [8], rates of sedentary behavior are currently not known in this population.
The unique and independent effects that sleep, sedentary behavior, and physical activity have on cardiometabolic health are well described [7, 9–15]. These behaviors, however, are inextricably related to one another given that they are each bound by the 24-h day (i.e., increasing or decreasing time in one inevitably requires modifications to the others) [16]. Recent work that adequately accounts for the interdependency of these behaviors found that re-allocating 30 min/day of sedentary time with equal time of either sleep, light activity, or exercise improved cardiometabolic outcomes, most notably triglycerides, fasting glucose and insulin, and waist circumference [17]. These behaviors may also operate synergistically. Daytime exercise temporally improves sleep quality (i.e., wakefulness after sleep onset) during the subsequent night of sleep and reduced wakefulness in turn increases exercise the following day [18]. Furthermore, changes in sleep and physical activity may have an additional cascading effect on dietary consumption [19] that may further augment cardiometabolic health. Harnessing these potential synergies in an optimal fashion may result in more potent behavioral interventions on cardiometabolic health.
State-of-the-art, personal technologies such as the smartphone are promising approaches to intervene across the 24-h period given their ubiquity and capability to deliver tailored information and feedback. Smartphone (e.g., iPhone, Android, Windows) ownership among Americans has grown to 53 % [20]. Uptake is quite high in Iraq and Afghanistan Veterans (by virtue of their younger age [20]), and the Veterans Health Administration (VHA) has several system-wide initiatives to deliver mHealth applications directly to patients through a “VA App Library” [21]. As the largest integrated health-care system in the US that is already developing a large mHealth infrastructure, the VHA represents a key platform to leverage the dissemination of mHealth applications.
This article describes development and initial process evaluation of BeWell24, a multicomponent smartphone application that targets behavior change (alone and in combination) in behaviors that make up the 24-h spectrum (i.e., sleep, sedentary behavior, and physical activity). Specifically, this paper reports on the following aspects of BeWell24: (1) the user-centered iterative design process undertaken for app development, (2) quantitative process-level outcomes related to app usage during the intervention, and (3) post-intervention qualitative feedback from users regarding app design and satisfaction. The information gathered from this study will be used to inform future development of the app, larger-scale efficacy trials, and provide generalizable insights for other researchers developing health behavior change apps in Veteran and other populations.
METHODS
BeWell24 app development and description
App development process
BeWell24 was developed using a community-embedded iterative design framework adapted from a previous mHealth design process [22]. The planning and design team included an interdisciplinary research team (N = 9; experts in sleep, sedentary behavior, and physical activity behavior change techniques), target users (N = 7; Veterans meeting eligibility criteria for the main efficacy trial), and an mHealth software engineer (N = 1). These stakeholders were involved in each step of the app development process described below. First, Veterans Health Administration interdisciplinary clinical staff (N = 22; including primary care physicians, staff nurses, nurse practitioners, psychiatrists, social workers, and case managers) participated in focus groups (N = 5) to review and discuss paper prototypes prepared by the research team and the mHealth software engineer. These focus groups were synthesized using a rapid assessment process [23] where themes related to desired app content were identified, refined by the research team, and incorporated into the app design by the mHealth software engineer. Next, functional prototypes were presented to target users in one-on-one, face-to-face sessions using a rapid and iterative prototyping method [24]. A “think-aloud” data solicitation protocol was used to gather information from users related to navigation tasks, overall look and feel of the app, and desired app functions. The think-aloud protocol asked participants to perform various app-related tasks and to verbalize whatever crosses their mind during the task performance [25]. Participants were given $25 USD for their participation. Summaries of each user experience were discussed among the research team, and feedback led the mHealth software engineer to make appropriate modifications. Functional prototypes were continuously improved and then brought back to the users to ensure modifications addressed the concerns. This process was repeated until consensus among the users was reached. Consensus was determined when no new modifications were rated and all existing modifications were satisfactorily addressed (approximately three visits/user).
App description—overview
BeWell24 was developed in a component fashion such that each component (i.e., sleep, sedentary, and exercise) was able to operate as a stand-alone app or be integrated with other components in a seamless fashion. This design decision was made early in the developmental process given the hypothesized synergistic nature of the components and the desire to test their single and combined impact on health outcomes. App components were informed by leading behavioral theories and behavior change techniques described by Michie et al. [26] Table 1 summarizes these behavioral strategies and how they were implemented in the app.
Table 1.
Description of behavior change strategies in the sleep, sedentary, and exercise components of BeWell24
| App component | Theoretical underpinning | BCT grouping | Strategy to implement BCT in BeWell24 |
|---|---|---|---|
| Sleep | Sleep education; sleep hygiene; stimulus control therapy | Goals and planning | • “Wake time calculator” to identify selectable goal for regular wake time |
| • Problem-solving strategies through “show me tips” interactive tool for common sleep-related beliefs and behaviors | |||
| Feedback and monitoring | • Graphical daily/weekly feedback on sleep duration, sleep onset latency, wakefulness after sleep onset, and sleep quality rating | ||
| Shaping knowledge | • Information on behavioral (e.g., alcohol, tobacco) and emotional (e.g., arousal) antecedents to sleep | ||
| Associations | • Reducing prompts/cues associating bed with “trying” to fall asleep with user-generated “my sleepy list” activities when having trouble falling asleep | ||
| Sedentary | Self-regulation | Feedback and monitoring | • Graphical daily/weekly feedback on context-specific sitting behaviors |
| Natural consequences | • Education on link between excessive sitting and chronic disease | ||
| Associations | • “My routines” tool to identify prompts/cues to reduce sitting (e.g., stand time a commercial appears on TV) | ||
| Repetition and substitution | • “Where do I sit?” tool to suggest context-specific replacements of sitting additional sleep or lifestyle behaviors | ||
| Exercise | Social cognitive theory | Goals and planning | • Selectable goal for weekly physical activity |
| • Problem-solving strategies through “give me tips” interactive tool for common barriers to exercise | |||
| Feedback and monitoring | • Graphical daily/weekly feedback on exercise behaviors | ||
| Shaping knowledge | • Advice and instruction on type and duration of exercise | ||
| Natural consequences | • Education on link between exercise and chronic disease | ||
| Associations | • “Motivate me” tool to identify prompts/cues to increase exercise motivation |
BCT behavior change technique, derived from Michie et al. [27]
Self-monitoring component
This component was developed with the primary goal of allowing rapid self-tracking of targeted behaviors across the full 24 h in 5-min increments. Aside from basic self-monitoring, this component does not directly provide any behavioral feedback or behavioral strategies. The data captured via self-monitoring was designed to be integrated as behavioral feedback into each of the three behavioral app components (i.e., sleep, sedentary, and exercise) which are described below. Users allocated time to sleep, sedentary, other, and exercise activities using a “drag and swipe” interaction (Fig. 1a). Users were provided standardized definitions of each activity by tapping on the icon at the top of each activity column. Sleep activities included any nap or main sleep period, and users were encouraged to report all time in bed for the purpose of sleep. Sedentary activities included any sitting behaviors (e.g., sitting at desk, watching television). Exercise activities included any moderate-vigorous physical activity such as brisk walking, jogging/running, and aerobic exercise. The “other” category (denoted by the yellow asterisk column in Fig. 1a) was designed to account for all other activities not fitting into the previous categories, with examples including household chores, light gardening, leisurely walking, and other activities of light intensity. Users were then able to annotate more detailed information about the reported activities by double-tapping on the activity. For sleep, users completed a sleep log commonly used in the field to define sleep quality metrics including sleep onset latency, wakefulness after sleep onset and sleep efficiency, and sleep quality (Fig. 1b) [28]. All sleep was reported by the user, and the accelerometer in the phone was not used for this purpose. For sedentary behavior, users allocated their sitting into five contexts (work, television, socializing, transportation, and other) using basic sliders to account for the reported sitting (Fig. 1c). These contexts were selected based on the most frequently reported sitting behaviors [29]. For exercise, user allocated activity into five types (running/jogging, brisk walking, other cardiovascular exercise, resistance/weight training, other moderate/vigorous exercise) using checkboxes (Fig. 1d). These types were selected based upon feedback from the target users. Checkboxes were used over sliders since these exercise activities are typically completed in bouts of a single activity (Fig. 1).
Fig. 1.
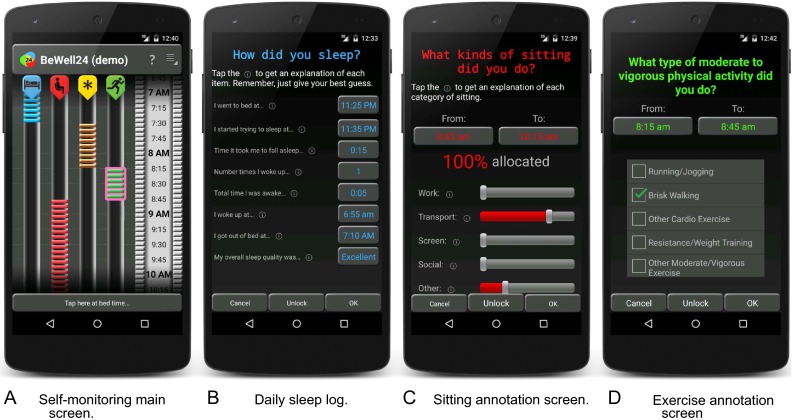
Screenshots of BeWell24 self-monitoring component. a Self-monitoring main screen. b Daily sleep log. c Sitting annotation screen. d Exercise annotation screen
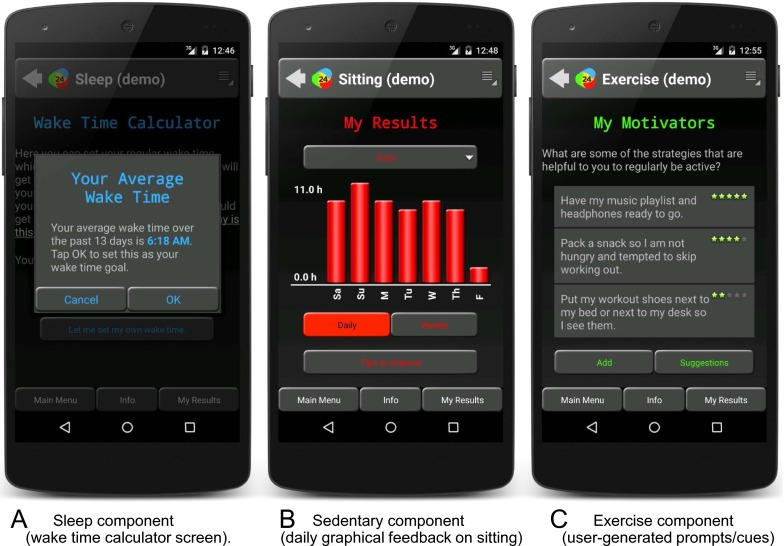
Sleep component
The sleep component included sleep education, sleep hygiene, and stimulus control therapy. The content was developed based upon recommendations from major sleep health organizations (American Academy of Sleep Medicine [30], National Sleep Foundation [31]) and the existing “VA CBT-i coach” behavioral sleep treatment app deployed throughout VHA hospitals in conjunction with the national Cognitive Behavioral Therapy for Insomnia dissemination program and available on iOS and Google app stores [32]. Sleep education and hygiene have modest efficacy but are fundamental to sleep intervention [27]. The app included education on the basic needs and functions of sleep (e.g., sleep drive, circadian rhythm, sleep stages), sleep-promoting factors (e.g., cool and quiet sleep environment, exercise), and harmful sleep behaviors (e.g., excessive alcohol, caffeine, tobacco). Stimulus control therapy is based on an operant paradigm which teaches individuals to re-associate the bed and bedroom with cues for sleep and promotes a consistent sleep-wake pattern and is recognized as a gold standard behavioral treatment for poor sleep [33]. Interactive components including a wake time calculator and personalized sleep tips were included (Fig. 2a).
Fig. 2.
Screenshots of BeWell24 sleep, sedentary, and exercise components. a Sleep component (wake time calculator screen). b Sedentary component (daily graphical feedback on sitting). c Exercise component (user-generated prompts/cues)
Sedentary component
The sedentary component was based on self-regulatory strategies [34]. This component provided graphical feedback on total sitting time and time spent sitting at work, watching television, socializing, transportation, and other activities. Basic education on the health risks of prolonged sitting was provided, along with user-generated prompts/cues to break up sitting during common sitting activities (e.g., “whenever I watch TV I will get up at the commercial and complete a small task”) and context-specific tips to replace sitting with additional sleep or lifestyle behaviors were provided (to avoid confound with the exercise component, recommendations to increase exercise were not included). Feedback about sitting behaviors were updated into the component immediately as the behaviors were reported in the self-monitoring app. Users could access this feedback at any time, and summaries were provided through the app to participants each week (Fig. 2b).
Exercise component
The physical activity component primarily included goal setting, feedback, and problem-solving, as social cognitive theory-based techniques [35], and was adapted from the evidence-based “Fit-Minded” intervention [36]. Participants were encouraged to set goals (based on their self-reported activity in the self-monitoring component of the app) to increase the frequency and duration of their exercise. Behavioral targets progressively increased and aimed for participants to reach national guidelines for physical activity [9]. Users were given the option of the possible goal formats: (a) “recommended” goal (i.e., 110 % of weekly average of previous two weeks of reported exercise behavior); (b) national guidelines (i.e., 150 min/week of moderate-vigorous exercise); or (c) user defined (i.e., users could input their own desired goal). Users were allowed to modify their goal at any time (Fig. 2c).
Technical considerations
BeWell24 was operational on Android 2.3 and higher platforms. Development on other platforms was withheld until efficacy was established. BeWell24 did not collect location or other contextual data, and the system required a study ID to be entered by a research staff member prior to use. No other potentially identifiable information was collected (e.g., Internet protocol addresses, international mobile station equipment identity number). This process allowed BeWell24 to collect only de-identified data from the user. These data were uploaded directly to study servers via wireless or Wi-Fi connection each time the app was opened or a function in the app was performed.
Process evaluation of first-generation intervention study
Recruitment and participants
The target population was US Veterans currently receiving clinical care at a regional VHA hospital in the Southwestern United States, aged 35–60 years, who were measured as overweight/obese (BMI ≥ 25 kg/m2), with a fasting glucose of ≥100 mg/dL. Eligibility criteria also included reporting of (a) insufficient physical activity (defined as endorsing activity ranking categories ≤4 on the Stanford Brief Activity Survey [37], which closely aligns with national physical activity guidelines [9]), excessive sitting (defined as ≥8 h of sitting from the International Physical Activity Questionnaire [38]), and short sleep duration (<7 h/night), or a mild/moderate sleep complaint (modified version of the Insomnia Severity Index [39]). Recruitment methods included distributing flyers in clinic waiting and exam rooms and targeted mailings. Eligible participants were required to have their own Android smartphone because research indicates that users’ adoption of an electronic system is improved when they are familiar with a device [40]. All participants completed a telephone screening to determine eligibility. Institution review boards governing the local VHA hospital and the university in which some of the researchers were affiliated approved all study procedures. All participants provided written informed consent.
Study design
The primary aim of the first-generation testing of BeWell24 was to identify which of the three intervention components elicited significant behavior change in the respective targeted behaviors. To optimize efficiency and to explore potential synergies among the behavioral outcomes, a multiphase optimization strategy (MOST) research design was used. A full-factorial 2 × 2 × 2 screening experiment was conducted such that users were randomized to one of eight possible combinations of the sleep, sedentary, and exercise components of the app (k): none (k = 1), one of three app components (k = 3), two of three app components (k = 3), or all three app components (k = 1). This design is displayed in Table 2. All eligible participants underwent a 3-week run-in period where they received the self-monitoring component only. Participants attended two additional visits during the 8 weeks to complete study-related assessments.
Table 2.
Multiphase optimization strategy design for first-generation pilot study of BeWell24
| Experimental condition number | Intervention components | ||
|---|---|---|---|
| Physical activity component | Sedentary behavior component | Sleep component | |
| 1 | No | No | No |
| 2 | No | No | Yes |
| 3 | No | Yes | No |
| 4 | No | Yes | Yes |
| 5 | Yes | No | No |
| 6 | Yes | No | Yes |
| 7 | Yes | Yes | No |
| 8 | Yes | Yes | Yes |
All participants were encouraged to use the self-monitoring component throughout the intervention
Process-level measures of app usage, user experience, and satisfaction
App usage was measured using BeWell24’s built-in tracking capabilities that recorded all navigation activities performed by the user. These data were sent to a data acquisition web service on a central server. Usage statistics included the number of minutes the self-monitoring was employed (i.e., time users spent entering data), percent of the 24-h day reported by the participant within the self-monitoring component, and minutes of usage of the sleep, sedentary, and exercise components (i.e., time spent viewing and interacting with these components of the app).
Following the intervention period, structured interviews were conducted using open-ended questions. All participants were queried as to the self-monitoring component of the app, while the other components (sleep, sedentary, and exercise) were asked only if they were randomized to that component. Additionally, participants were asked questions related to satisfaction with the app at the end of the interview. These questions were developed by the research team and pertained to whether they would (a) recommend the app to another Veteran (yes/no), (b) continue using the app after the study (yes/no), (c) download the app from an app store if available (yes/no), as well as (d) an overall satisfaction rating for BeWell24 on a scale of 0 (not at all satisfied) to 10 (completely satisfied). The interviews were conducted by trained research staff, audio-recorded, and lasted approximately 30 min.
Data analysis
Demographics, usage data, and satisfaction ratings were summarized using means, standard deviations, frequencies, and percentages. To access the objective usage data, .xml files generated by the app and stored on a secure server hosting the app were downloaded locally and summarized from seconds to daily and weekly levels prior to descriptive analysis. All quantitative analyses were performed using SAS Enterprise Guide 6.1 (Cary, NC, 2013).
Interviews were transcribed verbatim and analyzed using a case study approach in QSR NVivo10 (Cambridge, MA, 2010). This approach allows the investigator to study multiple bounded systems (cases) from interviews producing descriptive reports of cases and common themes across these cases [41, 42]. Two coders reviewed the data separately to develop themes and then discussed these themes until they came to agreement. Thematic categories were developed based on the major topics of the interview questions [41].
RESULTS
Participants
Twenty-six participants were enrolled in the study. Participants were 49.0 ± 8.9 years of age (range, 36 to 65 years), primarily men (85 %), and Caucasian (73 %). Participants were obese (BMI = 35.0 ± 8.3 kg/m2). Five subjects withdrew from the study during the 3-week run-in period and were not randomized. Reasons for withdrawal were due to unrelated health concern (n = 1), burdensome assessment protocol (n = 2), and loss of contact (n = 1). Four subjects were lost to follow-up after randomization (17/21, 81 % retention). Reasons for lost to follow-up were due to unrelated health concerns (n = 1) and loss of contact (n = 3). There were no differences in demographic characteristics between withdrawn and lost to follow-up participants from participants who completed the study (N = 17). All available data, from both completers and non-completers, are included in subsequent analyses. Only completers participated in qualitative interviews at the conclusion of the intervention (n sleep component = 6; n sedentary component = 10; n exercise component = 6).
Process-level usage statistics
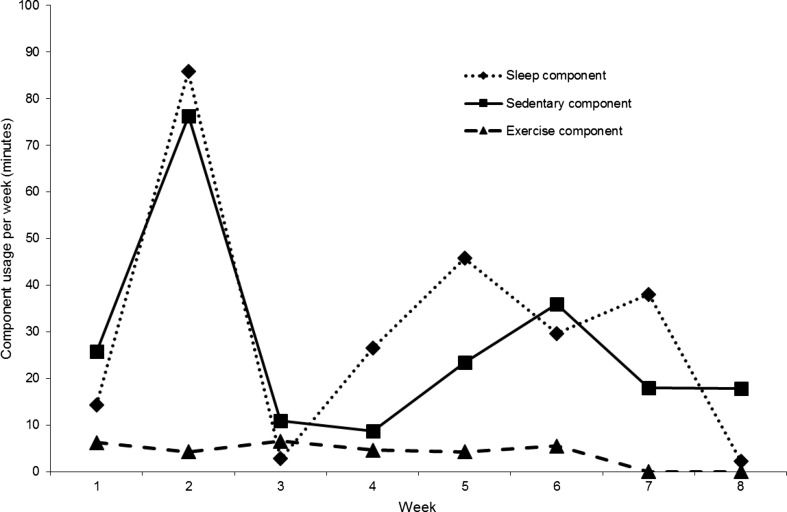
Figure 3 displays usage data and reported time for the self-monitoring component of the app. Usage remained steady throughout the run-in and intervention periods. On average, participants self-monitored about 60 % of the 24-h day and this monitoring took 3–4 min per day to complete. Figure 4 displays usage data for each of the sleep, sedentary, and exercise components. Peak usage occurred during week 2 of the intervention for both the sleep and sedentary components, but on average steadied at around 30 min/week for these two components. Usage of the exercise component remained lower than the sleep and sedentary components throughout the intervention period (<10 min/week).
Fig. 3.
Use per day (minutes) and reported time (% of 24-h day) of the self-monitoring component during run-in and intervention periods
Fig. 4.
Use per week (minutes) of sleep, sedentary, and exercise components during the intervention period by us
Qualitative interview results
Major themes emerged from the qualitative data related to each of the app components. Self-monitoring themes included awareness, ease of use, and time spent using the self-monitoring component. Behavioral app component (i.e., sleep, sedentary, and physical activity) themes included content, awareness/motivation or behavior, and modifications/recommendations. These are described in detail below.
Self-monitoring component (n = 17)
Experience with the self-monitoring component yielded three major themes, including awareness, ease of use, and time spent using the app. Participants reported that monitoring their activity helped them to become more aware of their behavior, for example, “I could see from the app that I needed to do more physical activity”; these participants also mentioned that they liked to see the data, e.g., “…my own little video game, trying to level up the next day.” One participant felt that seeing information on the app was discouraging because they were more aware of sedentary behavior, “I was sitting a lot of time because of my job, so that was kind of discouraging.” The self-monitoring was reportedly easy to use as several participants stated, “I found it easy,” “it was easy to do,” and “it’s a simple program.” A few participants mentioned that it was easy as long as they did not experience problems, or remembered to use the app. Many of the participants felt that the app did not take that long to use. Participants stated “[it] only takes a matter of minutes,” “10 minutes,” and “[it] takes 30 seconds to program that thing every morning.” One participant shared that it took a lot of time to report activities at first; however, over time, it became easier to use daily. Another participant mentioned it was used early in the intervention but then “got less interested in doing it.”
Sleep behavior component (n = 6)
Approximately half of the participants indicated the sleep component was easy to use when they stated, “real simple, push a button,” and “pretty much straightforward.” In relation to content, one participant reported dissatisfaction with the sleep component because “it didn’t tell me…movement…or actual sleep.” Another participant said, “It asked a lot of redundant questions.” A few participants reported not liking the functionality of entering information or the inability to see the information entered. A participant reported liking the flexibility of the sleep component because it allowed one to push a button to start sleep or enter the time. Approximately half of the participants also reported greater awareness of their sleep behaviors using the sleep component. One participant said, “I stay in bed too much,” while another said, “I don’t sleep as much as I thought I was.” When asked about modifications or recommendations for the app, a few participants reported recommendations for some type of report/results that they could “refer to” for information on their sleep in the past (last week, day before, etc.).
Sedentary behavior component (n = 10)
The three major themes for the sedentary component of the app were content, awareness/motivation for behavior, and modifications/recommendations. With respect to content, participants suggested that the sedentary component was easy to use, interesting, and easy to understand. Some participants did not like the content. Their reasons for dislike ranged from “didn’t have functionality” to “it’s just a pain and I don’t know the rewards would be…worth the effort it took to mess with it.” Many participants felt more aware of their sitting behavior as a result of using this component, “I’m more aware…I just need to figure out how to motivate myself to not sit so much.” Another participant said, “…well the sitting was an eye opener for me.” One participant reported behavior change as a result of the awareness, “Made me get up and go down to the other office, walking down instead of picking up the phone. Made me walk across the hospital to show someone where to go instead of sitting there trying to explain it.” When asked about modifications or recommendations for the sedentary component, a few participants suggested having more options for “things to try… a better list or more varied list.” Other participants said they wanted to have a report, or results that provided feedback about their total time sitting during a specific day or in days/at times prior. One person felt giving them a handout would have been just as effective as the mobile phone app for modifying their sitting behaviors.
Exercise component (n = 7)
There were no clear themes that emerged from the exercise component. A few participants reported barriers to using the exercise component of the app such as having “to make more of an effort to take the time to complete it on my own outside of the study… I’m bad at remembering to do things with 2 small children.” Another participant entered exercise information at the end of the day and could not remember their activity, “sometimes it gets late and then it’s like okay, what did I do this morning?” Another participant noted that “exercise is not a word that is in my database.” A few participants shared the same modification for the exercise component suggesting that the app have the ability to track activities such as cleaning the house as opposed to lifting weights. One participant suggested, “…include like my activity with the kids ‘cause I felt like that was more, …it wasn’t as vigorous as running or jogging, … think it would have been nice to include that in the physical activity.”
Overall satisfaction ratings
Among completers, all participants (100 %) indicated that they would recommend BeWell24 to another participant. The majority reported that they would like to continue using the app (73 %) and would download the app from an app store if it were available (82 %). Finally, participants provided an overall satisfaction rating of 7.2 ± 1.7 (out of 10; range, 5–10).
DISCUSSION
The purpose of this study was to describe the development and initial process evaluation of BeWell24, a multicomponent smartphone application that targets behavior change in sleep, sedentary behavior, and physical activity. We found preliminary evidence that BeWell24 is a feasible smartphone app for use among Veterans with increased metabolic risk. The qualitative data suggested that the app components, with the exception of the exercise component, were regularly used, and usage was sustained across the intervention period. The qualitative interviews provided insights into positive and negative features of the app and its components. The satisfaction ratings suggested modest to high ratings of the app overall with a willingness to continue using the app.
There was considerable evidence supporting the usefulness of the self-monitoring component of the app. Participants were able to complete this portion in <5 min/day, and there was consensus that it was easy to use. This is an important finding given that paper-based daily exercise and sleep logs often take 5 min or longer and may be more burdensome to complete. The qualitative interviews indicated participants were willing to check in with the app throughout the day, suggesting perhaps more accurate self-monitoring given reduced recall. It should be noted that participants were given a brief training (approximately 5 min) at the beginning of the study on using the self-monitoring component. This was in response to our user testing that suggested it was necessary to instruct participants on the “swipe and drag” interface and how it can be optimally used. This brief training circumvented initial frustrations with the app and likely contributed to the reported ease of use in the sample. The other interesting finding was the roughly 60 % completion rate of the 24-h period. It is difficult to compare this completion rate with other studies given that few other studies have implemented a full 24-h protocol, and the duration (11 continuous weeks in total) in which participants were asked to self-monitor was quite lengthy. We also acknowledge that attrition rates were higher than similar trials. It is possible that this was due to overly burdensome self-monitoring; however, there was no evidence to suggest a decline in the completion rate through the run-in and intervention periods. Alternatively, this attrition rate could have been due to other factors specific to the Veteran population, including busy schedules, lack of transportation for study visits, and other health complications.
Among the sleep, sedentary, and exercise components, we found mixed acceptability. Based on usage data, participants spent considerable time early in the intervention period using the sleep and sedentary components. This would be expected as there were considerable techniques (shaping knowledge, natural consequences) within these components that required more intense reading and information gathering. Usage subsided after week 3, but remained at or near 20 min/week for the sleep and sedentary components. Additionally, a theme that emerged in the qualitative results across both the sleep and sedentary components was the enhanced self-awareness of the participants’ behaviors.
Both usage data and qualitative results for the exercise component were indeed in contrast to the sleep and sedentary components. Usage of the exercise component was low throughout the intervention period, and feedback from participants during the interviews suggested a general lack of satisfaction. While the sample was too small to confirm, rates of lost to follow-up were higher among persons assigned to the exercise component, suggesting this dissatisfaction may have affected overall participation in the intervention. Participants reported a lack of identification with the term “exercise” and were discouraged that lifestyle behaviors of lighter intensity (e.g., household chores, light gardening) were not targeted with this component. In view of emerging data suggesting the cardiometabolic benefit of light-intensity activity [13, 17, 43], the exercise component should be re-formatted to support change across a wider range of behaviors, including those of lighter intensity. Indeed, this may also support greater synergies with the sedentary component, given that reducing sedentary behavior often means re-allocating time into standing and lighter forms of walking and moving behaviors. These behaviors may or may not be planned or intense enough to be considered exercise, but nevertheless are health-enhancing in nature [9].
Strengths and limitations
An important strength of this study was harnessing the built-in capabilities of the smartphone to passively and objectively capture process-level usage statistics. Furthermore, these usage patterns were localized to specific components of the app, providing important insights for which components were acceptable and which were not to the participants. We also followed an extensive and iterative design process which included design considerations and feedback from a diverse set of stakeholders. This included behavioral experts, mHealth design experts, VHA clinical teams, and Veterans themselves. The small sample size precludes any definitive recommendations to be made about BeWell24. However, the preliminary nature of this study, along with the MOST design, was ideally suited for this early-stage investigation and is appropriate to inform larger-scale investigations with an adapted and refined version of BeWell24. A second important limitation to this study was the incomplete nature of the qualitative interviews and satisfaction ratings given that we were unable to ascertain these study elements from those lost to follow-up. Our final sample of completers likely provided a positively biased viewpoint of BeWell24 and its components, and understanding the reasons and experiences of those who did not continue using the app likely would have resulted in a fuller understanding of how the app could be improved.
Future directions
Logical next steps for this work include refining each of the app components, based upon feedback, and testing BeWell24 in a larger cohort of Veterans. From an efficacy perspective, results from the ongoing trial regarding changes in sleep, sedentary, and exercise behaviors will largely guide the final “packaged” intervention. However, the process-level results presented here will inform interim modifications that could be made to enhance the potency of each of the included app components. In addition, more in-depth and enhanced functionality could be included within each of these app components and they could be tested as stand-alone apps. This is currently underway with the sleep component, where additional functionality is being added and is being tested in a cohort of Iraq and Afghanistan Veterans with insomnia. Finally, the promising findings related to the feasibility of a 24-h self-monitoring component suggest this tool could have value as a stand-alone app or to support other mHealth interventions. Important next steps for this component include validation against an objective monitor and integration with consumer-based wearable monitors for more passive tracking.
CONCLUSIONS
BeWell24 represents a new approach to address disproportionate rates of metabolic risk and related diseases in Veterans by targeting the full 24-h spectrum of health behaviors. Overall, BeWell24 was found to have acceptable levels of usage and acceptability among Veterans. This followed a very extensive app design process which incorporated diverse perspectives unique to this Veteran cohort. This formative work will inform the final development of BeWell24 for use in a larger-scale trial which leverages synergies across the 24 h to improve cardiometabolic health in Veterans and may also serve as a model for development and process evaluation of mHealth apps in other populations.
Acknowledgments
This study was funded in part by the Virginia G. Piper Charitable Trust. This research was partially supported with resources and the use of facilities at the Phoenix Veterans Affairs Health Care System. The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government. The authors would like to thank Sean Branscome, Joseph Brinkman, Sarah Bryant, Rickman Fish, Peter Reaven, and Justin Zeien for their assistance in app development and study execution.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Adherence to ethical principles
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Implications
Practice: Practitioners may consider using mHealth technologies to intervene on multiple behaviors across the 24-h spectrum.
Policy: The Veterans Health Administration represents a key platform for developing and disseminating evidence-based mHealth interventions.
Research: A smartphone-based intervention targeting sleep, sedentary, and active behaviors may be feasible to deliver in a sample of US Veterans with increased metabolic risk, and future research is needed to understand whether this combination of behaviors may improve cardiometabolic risk biomarkers.
Contributor Information
Matthew P. Buman, Email: matthew.buman@asu.edu.
Dana R. Epstein, Email: dana.epstein@va.gov.
Monica Gutierrez, Email: moni.gutierrez@asu.edu.
Christine Herb, Email: Christine.herb@va.gov.
Kevin Hollingshead, Email: kevin.hollingshead@asu.edu.
Jennifer L. Huberty, Email: Jennifer.huberty@asu.edu.
Eric B. Hekler, Email: eric.hekler@asu.edu.
Sonia Vega-López, Email: Sonia.vega.lopez@asu.edu.
Punam Ohri-Vachaspati, Email: punam.ohri-vachaspati@asu.edu.
Andrea C. Hekler, Email: andrea.hekler@va.gov.
Carol M. Baldwin, Email: carol.baldwin@asu.edu.
References
- 1.Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28(7):1769–1778. doi: 10.2337/diacare.28.7.1769. [DOI] [PubMed] [Google Scholar]
- 3.Nelson KM. The burden of obesity among a national probability sample of veterans. J Gen Intern Med. 2006;21(9):915–919. doi: 10.1007/BF02743137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson ML, Pietz K, Battleman DS, Beyth RJ. Prevalence of comorbid hypertension and dyslipidemia and associated cardiovascular disease—page 2. Prevalence. 2004;10:926–932. [PubMed] [Google Scholar]
- 5.Faestel PM, Littell CT, Vitiello MV, Forsberg CW, Littman AJ. Perceived insufficient rest or sleep among veterans: behavioral Risk Factor Surveillance System 2009. J Clin Sleep Med. 2013;9(6):577–584. doi: 10.5664/jcsm.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 7.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das SR, Kinsinger LS, Yancy WS, Jr, et al. Obesity prevalence among veterans at Veterans Affairs medical facilities. Am J Prev Med. 2005;28(3):291–294. doi: 10.1016/j.amepre.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 10.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 12.Atienza A, Moser RP, Perna F, et al. Objective and self-reported physical activity and biomarkers of chronic disease in NHANES. Med Sci Sports Exerc. 2010.
- 13.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 15.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 16.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170(4):519–527. doi: 10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 18.Dzierzewski JM, Buman MP, Giacobbi PR, Jr, et al. Exercise and sleep in community-dwelling older adults: evidence for a reciprocal relationship. J Sleep Res. 2014;23(1):61–68. doi: 10.1111/jsr.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nedeltcheva AV, Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153(7):435–441. doi: 10.7326/0003-4819-153-7-201010050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pew Research Center’s Internet & American Life Project. Mobile technology fact sheet. 2014; http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/.
- 21.United States Department of Veterans Affairs. VA Mobile Health Internet - eHealth. 2012; http://www.ehealth.va.gov/mobilehealth.asp. Accessed November 27, 2012.
- 22.Buman MP, Winter SJ, Sheats JL, et al. The Stanford Healthy Neighborhood Discovery Tool: a computerized tool to assess active living environments. Am J Prev Med. 2013;44(4):e41–e47. doi: 10.1016/j.amepre.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beebe J. Rapid assessment process. In: Kempf-Lenoard K, editor. Encyclopedia of Social Measurement: Three Volume Set. San Diego, CA: Academic Press/Elsevier; 2005. pp. 285–291. [Google Scholar]
- 24.Dow SP, Klemmer SR. The efficacy of prototyping under time constraints. Des Think. 2011; 111–128.
- 25.Jaaskelainen R. Think-aloud protocol. Handb Transl Stud. 2010;1:371. doi: 10.1075/hts.1.thi1. [DOI] [Google Scholar]
- 26.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 27.Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7(3):215–225. doi: 10.1053/smrv.2001.0246. [DOI] [PubMed] [Google Scholar]
- 28.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An american academy of sleep medicine report. Sleep. 2006;29(11):1415–1419. [PubMed] [Google Scholar]
- 31.National Sleep Foundation. Sleeping Tips & Tricks. 2015; http://sleepfoundation.org/sleep-tools-tips/healthy-sleep-tips. Accessed February 27, 2015.
- 32.U. S. Department of Veterans Affairs. Mobile App: CBT-i Coach - PTSD: National Center for PTSD. 2014; http://www.ptsd.va.gov/public/materials/apps/cbti-coach-app.asp. Accessed March 10, 2015.
- 33.Bootzin RR, Epstein DR. Understanding and treating insomnia. Annu Rev Clin Psychol. 2011;7:435–458. doi: 10.1146/annurev.clinpsy.3.022806.091516. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A. The primacy of self-regulation in health promotion. Appl Psychol. 2005;54(2):245–254. doi: 10.1111/j.1464-0597.2005.00208.x. [DOI] [Google Scholar]
- 35.Bandura A. Self-efficacy: the exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- 36.Huberty JL, Vener J, Sidman C, et al. Women bound to be active: a pilot study to explore the feasibility of an intervention to increase physical activity and self-worth in women. Women Health. 2008;48(1):83–101. doi: 10.1080/03630240802132120. [DOI] [PubMed] [Google Scholar]
- 37.Taylor-Piliae RE, Norton LC, Haskell WL, et al. Validation of a new brief physical activity survey among men and women aged 60–69 years. Am J Epidemiol. 2006;164(6):598–606. doi: 10.1093/aje/kwj248. [DOI] [PubMed] [Google Scholar]
- 38.Hagstromer M, Oja P, Sjostrom M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(6):755–762. doi: 10.1079/PHN2005898. [DOI] [PubMed] [Google Scholar]
- 39.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003; 425–478.
- 41.Creswell JW. Qualitative inquiry and research design: choosing among five approaches. Sage; 2012.
- 42.Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. Sage; 1994.
- 43.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]