Abstract
BACKGROUND CONTEXT
Comparing research studies of low back pain is difficult because of heterogeneity. There is no consensus among researchers on inclusion criteria or the definition of an episode.
PURPOSE
This study aimed to determine pattern(s) of recurrent non-specific low back pain from data collected over 27 months.
STUDY DESIGN/SETTING
This study used retrospective cohort study using administrative claims from multiple payers. Although claims are designed for capturing costs, not clinical complexity, they are valid for describing utilization patterns, which are not affected by potential “upcoding.”
PATIENT SAMPLE
The patient sample consisted of population-based, nationally generalizable sample of 65,790 adults with continuous medical and pharmaceutical commercial health insurance who received health care for incident, non-specific low back pain. Potential subjects were excluded for plausible cause of the pain, severe mental illness, or cognitive impairment.
OUTCOME MEASURES
Diagnostic and therapeutic health-care services, including medical, surgical, pharmaceutical, and complementary, received in inpatient, outpatient, and emergency settings were the outcome measures for this study.
METHODS
The methods used for this study were latent class analysis of health-care utilization over 27 months (9 quarters) following index diagnosis of non-specific low back pain occurring in January–March 2009 and an analysis sample with 60% of subjects (n=39,597) and validation sample of 40% (n=26,193).
RESULTS
Four distinct groups of patients were identified and validated. One group (53.4%) of patients recovered immediately. One third of patients (31.7%) may appear to recover over 6 months, but maintain a 37–48% likelihood of receiving care for low back pain in every subsequent quarter, implying frequent relapse. Two remaining groups of patients each maintain very high probabilities of receiving care in every quarter (65–78% and 84–90%), predominantly utilizing therapeutic services and pain medication, respectively. Probabilistic grouping relative to alternatives was very high (89.6–99.3%). Grouping was not related to demographic or clinical characteristics.
CONCLUSIONS
The four distinct sets of patient experiences have clear implications for research. Inclusion criteria should specify incident or recurrent cases. A 6-month clean period may not be sufficiently long to assess incidence. Reporting should specify the proportion recovering immediately to prevent mean recovery rates from masking between-group differences. Continuous measurement of pain or disability may be more reliable than measuring outcomes at distinct endpoints.
Keywords: Claims analyses, Classification, Cohort studies, ICD-9 codes, Incident low back pain, Latent class analysis, Natural history, Non-specific low back pain, Recurrent low back pain
Introduction
Research on treatments for low back pain has been challenged by differences in definitions, inclusion criteria, baseline assessments, and outcome measures, producing results that often cannot be directly compared [1–5]. Significant progress has been made in identifying specific spinal disorders which can be confidently attributed to structural pathologies such as intervertebral disk herniation or spinal stenosis, leading to a better understanding of effective treatments for those conditions [6–8]. The remaining cases, referred to as non-specific low back pain, comprising approximately 85% of all low back pain cases, have multifactorial causes and varied salient features with great clinical impact and cost [9,10].
The traditional time-based categorization of low back pain into acute or chronic has shifted to a broad acceptance of pain characterization as “recurrent,” “persistent,” or “fluctuating.” [2,11–17] The National Institutes of Health Pain Consortium’s Task Force on Research Standards for Chronic Low Back Pain defined a chronic case as one which has resulted in pain on at least half the days in the last 6 months, explicitly allowing for short pain-free periods [1]. The amount of time required to distinguish a discrete episode from a chronic case remains unknown [2,3]. With no standard definition of an episode, some meta-analyses have defined acute cases based on a long-standing but weakly substantiated classification of symptoms lasting less than 6 weeks [11,12]. Differentiating between incident and recurrent episodes presents another important challenge because low back pain itself may cause anatomic, functional, neurologic, or structural changes [1,18,19]. Lack of differentiation to date could explain substantial within-study heterogeneity. Few studies report on whether inclusion criteria require incidence [20]. Symptom-free periods used to ascertain incidence have ranged from 28 days to a lifetime history [4,21]; some consider the specification “arbitrary” [2]. Research and clinical practice would benefit from a clinically based definition of an episode, including the duration required to make it a new episode.
Prior studies have investigated recurrence of non-specific low back pain over 6 or 12 months [13,15,16]. The objective of the present study is to determine the pattern(s) of recurrent non-specific low back pain from data collected over more than 2 years.
Material and methods
We identified 65,790 adults who received health care for incident non-specific low back pain between January and March, 2009. We required two claims of low back pain, possibly on the same day, to avoid identification based on incorrect coding. We analyzed 27 months of health-care utilization data for each subject following their index diagnosis. The care was documented in the Ingenix Impact Research Database, which includes adjudicated medical and pharmaceutical claims for a nationally representative sample of commercial insurance consumers. We only included members with continuous medical and pharmaceutical coverage to be sure that periods with no health-care utilization were not the result of missing data. We limited the sample to adults aged 18–64 as people aged 65 and above are likely to be covered by Medicare and so could have low back pain services that are not in commercial claims.
The methodology for identifying non-specific low back pain using administrative data is fairly well established, with researchers largely agreeing on which codes should be used [22]. There is consensus on the use of complete, five-digit International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for their specificity. For example, code 738, “Other acquired deformity,” includes subcodes that specify spondylolisthesis, which is widely considered to be a specific, confirmable cause of low back pain [6], as well as subcodes that indicate non-specific low back pain.
We specified a set of five-digit ICD-9-CM codes identifying non-specific low back pain consistent with previous literature (Table 1) [23–28].
Table 1.
ICD-9 diagnosis and procedure codes used to specify the study population
| ICD-9 | Definition | |
|---|---|---|
| Codes used to define inclusion criteria and to confirm a low back pain-free clean period before index diagnosis of non-specific low back pain | 353.4 | Lumbosacral root lesions, not elsewhere classified |
| 721.3 | Lumbosacral spondylosis without myelopathy | |
| 721.4 | Thoracic or lumbar spondylosis with myelopathy | |
| 721.42 | Spondylosis with myelopathy, lumbar region | |
| 721.5 | Kissing spine | |
| 721.6 | Ankylosing vertebral hyperostosis | |
| 721.7 | Traumatic spondylopathy | |
| 721.8 | Other allied disorders of spine | |
| 721.9 | Spondylosis of unspecified site | |
| 721.90 | Spondylosis of unspecified site without mention of myelopathy | |
| 721.91 | Spondylosis of unspecified site with myelopathy | |
| 722.1 | Displacement of thoracic or lumbar intervertebral disc without myelopathy | |
| 722.3 | Schmorl nodes | |
| 722.30 | Schmorl nodes, unspecified region | |
| 722.32 | Schmorl nodes, lumbar region | |
| 722.5 | Degeneration of thoracic or lumbar intervertebral disc | |
| 722.52 | Degeneration of lumbar or lumbosacral intervertebral disc | |
| 722.90 | Other and unspecified disc disorder of unspecified region | |
| 722.93 | Other and unspecified disc disorder of lumbar region | |
| 724.2 | Lumbago | |
| 724.3 | Sciatica | |
| 724.4 | Thoracic or lumbosacral neuritis or radiculitis, unspecified | |
| 724.5 | Unspecified backache | |
| 724.6 | Disorders of sacrum | |
| 724.8 | Other symptoms referable to back | |
| 724.9 | Other unspecified back disorders | |
| 739.3 | Non-allopathic lesion of lumbar region, not elsewhere classified | |
| 739.4 | Non-allopathic lesion of sacral region, not elsewhere classified | |
| 846 | Sprain and strain of sacroiliac region | |
| 846.0 | Sprain and strain of lumbosacral (joint) (ligament) | |
| 846.1 | Sprain and strain of sacroiliac (ligament) | |
| 846.2 | Sprain and strain of sacrospinatus (ligament) | |
| 846.3 | Sprain and strain of sacrotuberous (ligament) | |
| 846.8 | Other specified sites of sacroiliac region sprain and strain | |
| 846.9 | Unspecified site of sacroiliac region sprain and strain | |
| 847.2 | Lumbar sprain and strain | |
| 847.3 | Sprain and strain of sacrum | |
| 847.4 | Sprain and strain of coccyx | |
| 847.9 | Sprain and strain of unspecified site of back |
| ICD-9 code | Code description | |
|---|---|---|
| Diagnosis codes used as exclusion criteria | Specific causes of back pain | |
| 722.10, 722.2, 722.6, 722.73 | Intervertebral disc herniation | |
| 724.00, 724.02, 724.03, 724.09 | Spinal stenosis | |
| 738.4, 738.5, 756.11, 756,12 | Spondylolisthesis | |
| 806.0–806.9 | Fracture of vertebral column | |
| 805.1, 805.3, 805.5, 805.7, 805.9 | Open vertebral fractures without spinal cord injury | |
| 805.0, 805.2, 805.4, 805.6, 805.8 | Closed vertebral fractures without spinal cord injury | |
| 733.1 | Pathologic fractures | |
| 839–839.59 | Vertebral dislocations | |
| 720.0–720.9 | Inflammatory spondyloarthropathies | |
| 324.1 | Intraspinal abscess | |
| 353.2, 353.3, 721.0, 721.1, 721.2, 721.41, 722.0, 722.11, 722.4, 722.71, 722.72, 722.81, 722.82, 722.91, 722.92, 723.0, 723.4, 724.01 | Cervical and thoracic disorders (only if primary diagnosis) | |
| Procedure codes used as exclusion criteria | 03.2–03.29 | Chordotomy |
| 81.01–81.03 | Cervical and dorsal fusions | |
| 03.0–03.1, 03.4–03.8, 03.93, 03,94, 03.97, 03.98, 80.5–80.59, 81.00, 81.04–81.09 | Back surgery | |
| 78.59, 78.69 | Possible back surgery | |
| 140–239.9 | Neoplasms | |
| 630–676 | Pregnancy | |
| 730–730.99 | Osteomyelitis | |
| E800–E849.9 | Vehicular accidents |
The majority of subjects with a claim using this diagnosis code were excluded for having a claim with a diagnosis of intervertebral disk herniation (353.4, 89.7%; 721.4, 58.8%; 722.1, 100.0%; 722.5, 90.1%; 722.6, 80.1%; and 724.03, 91.2%).
International Classification of Diseases, Ninth Revision, Clinical Modification.
To identify subjects with incident low back pain, we required a 6-month clean period before the index diagnosis. We excluded potential subjects with any claim documenting nonspecific low back pain during the clean period (see Table 1). We also excluded subjects with a plausible cause of the pain, including specific structural pathologies that could result in low back pain (intervertebral disc herniation, spinal stenosis, and spondylolisthesis), back surgery, pregnancy, or trauma. (See Table 1 for the list of diagnosis and procedure codes used.) Back pain may also be attributed to existing conditions such as neoplasm, inflammation, or infection [28]. We excluded people with evidence of these conditions during the clean period and, because they could be identified during diagnostic investigation of low back pain, within 90 days after their index diagnosis (n=14,371). Finally, we excluded people with serious mental illness, intellectual disabilities, or dementia (n=811), who are less likely to make their own health-care decisions [29,30].
Complex, latent class models require more information than simple ones [31]. Both the test and validation sample required large numbers of subjects. We randomly assigned the subjects to a 60% test sample (n=39,597) or a validation sample (n=26,193).
Health-care services data
We collected all medical claims for non-specific low back pain for 27 months (nine 90-day quarters) following each subject’s index diagnosis of low back pain. The primary diagnosis is commonly interpreted as the most clinically meaningful diagnosis, indicating the most salient aspect of the patient’s condition during the visit [32]. We included only claims with a relevant primary diagnosis to demonstrate the pattern of health-care services sought specifically for low back pain.
In order not to double-count services, we defined a visit as one encounter with one provider in 1 day and applied hierarchical logic to determine the type of service most salient to the patient. For example, a visit resulting in one therapeutic service claim and one evaluation and management claim was considered therapeutic.
We identified filled prescriptions associated with an episode of non-specific low back pain within the same 27-month period. Medications included narcotics, both agonist analgesics and agonist-antagonist, and non-narcotics including non-steroidal anti-inflammatory (NSAID) analgesics, centrally acting analgesics, non-steroidal anti-inflammatory analgesics, glucocorticoids, and skeletal muscle relaxants. Pharmaceutical claims cannot be directly linked to low back pain because they do not have a diagnosis code. We used the Episode Treatment Grouper(®) (ETG) which has been used in prior research to identify people with clinical conditions from claims data, to identify episodes [33,34].
For each 90-day quarter, a dichotomous indicator identified whether the patient received a specific type of service during the quarter. The four indicators identified (1) a filled prescription for pain medication not associated with a procedure, (2) a surgical procedure, epidural steroid injection, or imaging, (3) therapeutic manipulation, or (4) an office visit not associated with a prescription, procedure, or therapeutic services. The indicators are statistically independent across quarters.
Statistical analysis
Latent class analysis (LCA) identifies distinct subgroups (classes) of people who share unmeasurable (latent) characteristics that are inferred from a set of categorical variables. In this case, LCA used the four variables indicating whether each patient received each type of service during each quarter to identify groups with distinct utilization patterns and probabilistically assign each patient to one group.
For each group, LCA specified the probability of its members receiving each type of service for non-specific low back pain. The options included the probability of receiving, in each quarter (1) no service; (2) each type of service alone (eg, pain medication or therapeutic manipulation); (3) each combination of two types of service (eg, both pain medication and therapeutic manipulation); and (4) three or more types of service. Combining multiple types of service into one category avoided potential estimation problems due to sparseness in the data.
The number of groups is specified by the researcher. As the number of groups increases, the results reflect more precise underlying patterns. The researcher selects the model with the number of groups that best fit the data based on three criteria. First, the patterns must be clinically or behaviorally meaningful. Second, the goodness-of-fit statistics should demonstrate a close fit to the underlying data, achieving a balance of fit and parsimony [31]. Third, the model should not be overspecified to the sample.
We used Statistical Analysis Software PROC LCA Version 1.3.0 and employed the Akaike’s Information Criterion, then Bayesian Information Criterion goodness-of-fit statistics [31,35]. We estimated a series of models with 2, 3, 4, 5, and 6 groups.
Results
The four-class model produced four exhaustive, non-overlapping groups of subjects, each with a distinct pattern of low back pain health-care utilization with strong goodness of fit. The additional group identified by the five-class model did not add information or improve the goodness of fit substantially. Three of the four groups were labeled “Recurrent” as the service utilization pattern implied recurrent pain. Almost half (46.6%) of the patients were moderately to very likely to receive health-care services for low back pain in each of the nine quarters (90-day periods) following index diagnosis. This means each subject had a moderate to high likelihood of receiving services in any given quarter. (If patients had continuous low back pain, a group with an approximately 100% likelihood in all quarters would have emerged. This did not happen, even in the six-group model).
The groups were created based on their overall utilization. Patients in the “Recurrent-PainMed” group (7.4% of the sample) had the highest overall utilization. These patients had an average 0.89 probability of services in each quarter. Subjects in the “Recurrent-Therapeutic Services” group (8.1% of the sample) were nearly as likely (average 0.74) to receive low back pain care in each quarter (Fig. 1).
Fig. 1.
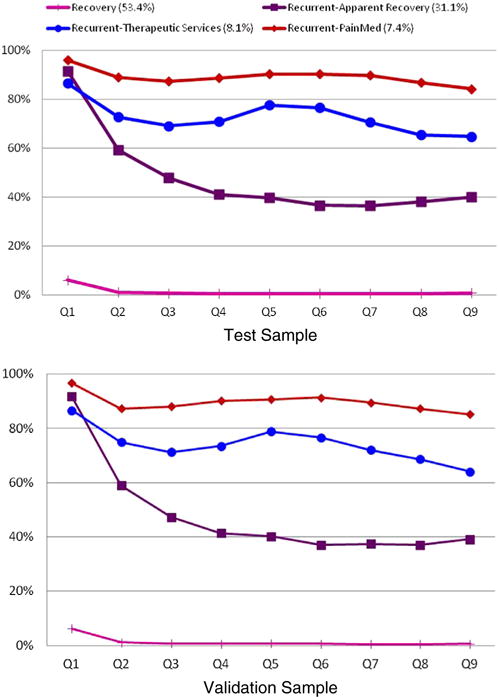
Likelihood of receiving any health care for low back pain, in each of nine quarters after index non-specific low back pain diagnosis, in four distinct groups of patients.
Approximately a third of the patients, the “Recurrent-Apparent Recovery” group (31.1% of the sample), seemed to recover as their probability of receiving back pain services declined each quarter from the first (0.92) to the fourth (0.41). However, they did not fully recover. The subsequent likelihood of each subject in this group getting care for low back pain in each quarter remained moderate, ranging between 0.37 and 0.40. The final group, “Recovery,” comprising about half the subjects (53.4%), are very unlikely to receive any health-care services for low back pain after their index diagnosis. Subjects in this group had only a 0.06 probability of receiving services in the first quarter and less than 0.01 in subsequent quarters.
The two groups with the greatest likelihood of back pain services use different types as well as volume of services. Table 2 shows the minimum probability of receiving each type of service in a given quarter. (If a patient received three or four types of services in a quarter, the specific types received cannot be distinguished.) After the first 90 days, patients in the Recurrent-PainMed group had an average 0.89 probability of services in each quarter. They had a minimum 0.71–0.83 probability of filling a prescription for pain medication, alone or with another type of service, in each quarter. In contrast, subjects in the Recurrent-Therapeutic Services group had at least a 0.51 chance of receiving therapeutic services, including physical therapy, occupational therapy, and chiropractic manipulation in each quarter (Table 2 and Fig. 2). Overall, subjects in the Recurrent-Apparent Recovery group did not tend to get any particular type of service.
Table 2.
Likelihood of subjects in each latent class receiving each type of service during each quarter after incident low back pain diagnosis
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | |
|---|---|---|---|---|---|---|---|---|---|
| Recurrent-therapeutic services | |||||||||
| Test sample (8.1%) | |||||||||
| Min. injection/imaging/surgerya | 3.8% | 3.3% | 2.8% | 2.4% | 2.4% | 1.6% | 2.0% | 1.9% | 1.7% |
| Min. therapeutic servicesa | 51.2% | 54.1% | 53.5% | 57.9% | 66.6% | 66.6% | 60.3% | 53.9% | 51.0% |
| Min. prescription pain medicationsa | 24.8% | 18.3% | 14.0% | 12.0% | 12.8% | 12.5% | 11.7% | 12.0% | 13.7% |
| Any low back pain care | 86.5% | 72.8% | 69.1% | 70.8% | 77.6% | 76.5% | 70.6% | 65.5% | 64.8% |
| Validation sample (7.6%) | |||||||||
| Min. injection/imaging/surgerya | 3.1% | 3.0% | 2.4% | 1.9% | 1.9% | 1.7% | 2.6% | 1.7% | 1.9% |
| Min. therapeutic servicesa | 52.1% | 56.7% | 57.9% | 63.1% | 70.2% | 68.5% | 61.3% | 55.5% | 51.0% |
| Min. prescription pain medicationsa | 24.1% | 16.8% | 13.8% | 12.9% | 12.3% | 11.8% | 10.5% | 12.7% | 13.0% |
| Any low back pain care | 86.5% | 74.9% | 71.2% | 73.5% | 78.9% | 76.6% | 72.1% | 68.6% | 64.0% |
| Recurrent-pain medications | |||||||||
| +Test sample (7.4%) | |||||||||
| Min. injection/imaging/surgerya | 2.5% | 2.8% | 2.7% | 2.1% | 2.3% | 2.0% | 1.7% | 2.1% | 2.2% |
| Min. therapeutic servicesa | 38.8% | 22.8% | 17.3% | 15.3% | 14.4% | 14.6% | 15.1% | 13.8% | 13.5% |
| Min. prescription pain medicationsa | 51.0% | 71.4% | 75.9% | 79.1% | 82.7% | 83.0% | 82.5% | 79.1% | 75.0% |
| Any low back pain care | 96.0% | 88.9% | 87.3% | 88.6% | 90.4% | 90.4% | 89.7% | 86.9% | 84.2% |
| Validation sample (7.6%) | |||||||||
| Min. injection/imaging/surgerya | 2.4% | 2.5% | 2.9% | 2.3% | 2.4% | 2.7% | 2.0% | 2.1% | 2.0% |
| Min. therapeutic servicesa | 41.1% | 23.3% | 19.2% | 16.6% | 14.5% | 14.3% | 13.4% | 13.6% | 13.9% |
| Min. prescription pain medicationsa | 53.0% | 71.4% | 75.3% | 79.9% | 82.5% | 83.3% | 80.5% | 77.8% | 75.0% |
| Any low back pain care | 96.7% | 87.2% | 88.0% | 90.1% | 90.6% | 91.3% | 89.5% | 87.2% | 85.1% |
| Recurrent-apparent recoverers | |||||||||
| Test sample (31.1%) | |||||||||
| Min. injection/imaging/surgerya | 3.4% | 3.8% | 3.0% | 2.8% | 2.7% | 2.5% | 2.3% | 2.4% | 2.4% |
| Min. therapeutic servicesa | 54.2% | 23.0% | 15.2% | 11.4% | 9.7% | 7.4% | 7.9% | 9.2% | 10.4% |
| Min. prescription pain medicationsa | 29.3% | 23.4% | 17.9% | 15.6% | 14.8% | 14.5% | 14.3% | 15.2% | 16.7% |
| Any low back pain care | 91.6% | 59.1% | 47.8% | 41.1% | 39.7% | 36.6% | 36.6% | 38.1% | 39.9% |
| Validation sample (31.6%) | |||||||||
| Min. injection/imaging/surgerya | 3.3% | 3.9% | 3.1% | 2.7% | 2.6% | 2.3% | 2.6% | 2.4% | 2.5% |
| Min. therapeutic servicesa | 54.4% | 23.5% | 15.0% | 11.5% | 10.0% | 8.9% | 8.9% | 9.0% | 10.4% |
| Min. prescription pain medicationsa | 29.5% | 22.6% | 17.7% | 16.4% | 15.5% | 14.3% | 14.7% | 15.3% | 15.6% |
| Any low back pain care | 91.7% | 58.9% | 47.2% | 41.4% | 40.2% | 37.1% | 37.4% | 37.1% | 39.2% |
| Recovery | |||||||||
| Test sample (53.4%) | |||||||||
| Min. injection/imaging/surgerya | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Min. therapeutic servicesa | 5.1% | 0.9% | 0.6% | 0.4% | 0.4% | 0.5% | 0.5% | 0.5% | 0.7% |
| Min. prescription pain medicationsa | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Any low back pain care | 6.0% | 0.9% | 0.6% | 0.4% | 0.4% | 0.5% | 0.5% | 0.5% | 0.7% |
| Validation sample (53.3%) | |||||||||
| Min. injection/imaging/surgerya | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Min. therapeutic servicesa | 5.5% | 1.1% | 0.7% | 0.6% | 0.7% | 0.6% | 0.5% | 0.4% | 0.6% |
| Min. prescription pain medicationsa | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Any low back pain care | 6.2% | 1.1% | 0.7% | 0.6% | 0.7% | 0.6% | 0.5% | 0.4% | 0.6% |
Percentages are based on the given type of service being the only, or one of two, types received during the quarter. If a patient received three or four types of service during the quarter, the individual types of service cannot be distinguished.
Fig. 2.
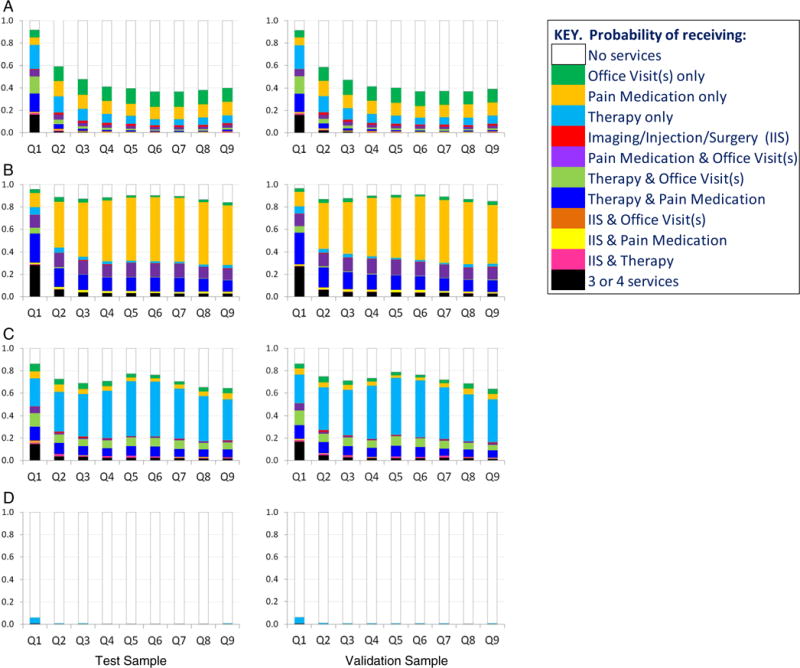
Distribution of type of health-care services in each group of people with non-specific low back pain, over nine quarters after index low back pain diagnosis.
Subjects in the Recurrent-PainMed group were also most likely to receive multiple types of service in any given quarter. In the first 90 days after diagnosis, they have a 0.73 probability of getting two or more types of service during the quarter, compared with 0.56 for the Recurrent-Apparent Recovery, and 0.48 for the Recurrent-Therapeutic Services groups. After the third quarter, during which the likelihood is 0.32, it declined slowly to 0.25 in quarter 9. In contrast, subjects in the Recurrent-Therapeutic Services group had a 0.17–0.21 likelihood of getting multiple services for low back pain during quarters 3 through 9, and the likelihood in the Recurrent-Apparent Recovery group was far lower, at 0.05–0.09.
Group characteristics
The four groups did not differ by sex, ranging from 53.1% to 54.3% (p=.53). The mean age for the groups was similar (range: 44.7–45.3 years) though statistically different (p<.0001). A review of the literature produced no consistent set of comorbidities to be assessed other than depression and anxiety. In this commercially insured population, all comorbidities were relatively rare. Table 3 compares comorbidities in at least 1% of the test sample across groups.
Table 3.
Characteristics of subjects in test and validation samples by assigned class
| Test sample | Recovery (n=21,145) |
Recurrent-therapeutic services (n=3,207) |
Recurrent-pain medication (n=2,930) |
Recurrent-apparent recoverers (n=12,315) |
Total (n=39,397) |
p-Value |
|---|---|---|---|---|---|---|
| Sex (% Female) | 53.9% | 53.1% | 54.3% | 53.8% | 54.0% | .53 |
| Age mean (SD) | 44.7 (11.0) | 45.7 (10.8) | 45.3 (11.0) | 45.2 (10.8) | 45.0 (11.0) | <.0001 |
| Comorbiditiesa | ||||||
| Chronic pulmonary disease | 3.8% | 4.3% | 4.1% | 3.9% | 3.9% | .27 |
| Diabetes | 3.8% | 4.4% | 3.6% | 3.4% | 3.8% | .15 |
| Alcohol/drug dependency | 2.7% | 3.2% | 2.6% | 2.4% | 2.7% | .21 |
| Rheumatologic disease | 2.5% | 2.2% | 2.2% | 2.2% | 2.4% | .29 |
| Myocardial infarction | 1.8% | 2.2% | 1.8% | 1.7% | 1.9% | .43 |
| Migraines | 1.9% | 1.3% | 1.8% | 1.7% | 1.8% | .14 |
| Validation sample | Recoverers (n=13,969) |
Therapeutic services (n=1,974) |
Painkillers (n=1,973) |
Apparent recoverers (n=8,277) |
Total (n=26,193) |
p-Value |
|---|---|---|---|---|---|---|
| Sex (% Female) | 53.5% | 53.5% | 53.6% | 52.9% | 53.5% | .97 |
| Age mean (SD) | 44.7 (10.9) | 45.2 (11.0) | 45.4 (10.9) | 45.6 (11.0) | 45.0 (10.9) | <.0001 |
| Comorbiditiesa | ||||||
| Chronic pulmonary disease | 3.9% | 4.6% | 4.0% | 3.9% | 3.9% | .66 |
| Diabetes | 3.9% | 3.5% | 3.9% | 4.2% | 3.9% | .70 |
| Alcohol/drug dependency | 2.6% | 2.3% | 2.6% | 3.1% | 2.6% | .42 |
| Rheumatologic disease | 2.3% | 2.4% | 2.4% | 1.9% | 2.3% | .63 |
| Myocardial infarction | 1.7% | 2.1% | 1.9% | 2.6% | 1.9% | .08 |
| Migraine | 1.8% | 2.3% | 1.7% | 1.4% | 1.8% | .24 |
Comorbidities present in at least 1% of the test sample are listed. Other comorbidities assessed include osteoporosis (0.9%), cerebrovascular disease (0.5%), liver disease (0.5%), renal disease (0.4%), depression (0.4%), peripheral vascular disease (0.3%), anxiety (0.3%), congestive heart failure (0.2%), ulcer (0.2%), and AIDS (0.1%).
There was no evidence of seasonality in utilization for three of the groups.
Strength of assignment
Each subject had a probability of being assigned to each of the four groups based on their empirical experience. Probabilities ranged from 0.99 (0.049) for Recoverers to 0.89 (0.14 SD) for the Therapeutic Services group. The mean probability for being in a group other than the assigned group ranged from 0.00 to 0.10. These probabilities compare well with published probabilities of 0.74–0.93 and >0.70 [13,16]. There is no test to determine whether the assignments were correct.
Validation sample
The 40% validation sample produced almost identical results to the test sample. Table 2 demonstrates that not only was the distribution of patients across the four groups very similar, but also the probability of receiving given sets of services was similar, within groups, across quarters. Table 3 shows that the samples have similar demographic and clinical profiles.
Discussion
We identified four discrete groups of patients with distinct experiences of non-specific low back pain as reflected in health-care utilization. For almost half the patients, an incident diagnosis was a very strong predictor of recurrent utilization. The Recurrent-PainMed and Recurrent-Therapeutic Services groups experienced near-continuous symptoms up to 27 months after diagnosis, with occasional but brief relapses. A third group, Recurrent-Apparent Recoverers, initially appeared to improve but sustained a moderate likelihood of receiving services each quarter, suggesting less frequent relapses.
The fourth group appears to improve immediately, with an extremely low likelihood of receiving care after the incident diagnosis, even in the first quarter.
There was no evidence of seasonality. Each subject’s index diagnosis was between January 1 and March 30 so services in the fifth quarter after diagnosis occurred in the first half of the following year. The slight increase of services for Recurrent-Therapeutic Services group in Quarter 5 could reflect renewed insurance benefits, as most commercial plans offer a limited number of therapeutic services in any given plan year. However, there is no increase in Quarter 9, as would be expected if this were the case.
Our findings are consistent with previous literature showing a “general pattern of improvement over time (rapid initial improvement followed by a plateau),” [11,36] with the important addition that the plateau is at a moderate to high level. Those subjects whose low back pain will recur at all will likely use a high volume of services over time. Although we did not analyze costs, the continued high volume of treatment clearly would incur significant costs [37,38].
Future research could investigate the differences between a 6- and 12-month clean period and determine how patterns differ for people with recurrent, versus incident, low back pain. Researchers with access to administrative data that are linked to clinical data could investigate associations with structural, demographic, and psychosocial factors and work toward predicting which patients would end up in each group.
Implications for non-specific low back pain research
This study has several implications for advancing research on non-specific low back pain research. First, a clean period with no pain or loss of function must be at least 6, and preferably 12, months long to identify incident cases adequately. Over 6 months, half of incident cases have at least an 80% chance of getting care for a relapse. A 6-month clean period will identify and exclude most non-incident cases.
Second, our results reinforce the need for specifying and reporting inclusion criteria. If only recurrent cases are included, few subjects would be expected to make a full recovery over 6 months. If only incident cases are included, half the subjects may improve rapidly. Only results from studies with similar populations can be validly compared. Registries should also be sure to require adequate clean periods.
Third, recovery rates are not likely to have normal distribution. Mean rates of short-term improvement, although commonly reported, may be skewed by the Recovery class. We concur with the NIH Task Force’s recommendation to report the proportion of subjects who achieve certain thresholds rather than aggregated change from the baseline in the study population [1].
Fourth, measuring outcomes only at predetermined endpoints is subject to bias because relapse is randomly distributed. Continuous data collection may more accurately reflect treatment effectiveness as well as differentiate between continuous episodes and relapses [4,5]. Outcomes could include assessments of cumulative experience, such as total weeks with specific levels of symptoms. Tools such as text messages have been used to collect such data frequently with minimal respondent burden [15,39].
Strengths and Limitations
We studied the utilization of care for non-specific low back pain in almost 40,000 patients for 27 months, compared with existing studies following under 800 subjects for 6 or 12 months [13,15,16]. Not only were the resulting categorizations of recovery types stable, with very strong average group assignments, but they were also validated with a second sample of 26,000. The cohort is generalizable to an adult, commercially insured population. It is possible that coverage policies and utilization review affected subjects’ treatment options. Our analysis focused on frequency, not type, of treatment, but our results could underestimate underlying need.
Administrative claims databases are designed to track expenditures, not medical care. Interpretation of results must be grounded with the caveat that they are based on data from people who sought care, were insured, whose care was accurately reported, and whose claims were accepted by the insurer. Paid claims are an underestimate of underlying pain or disability [40,41].
Administrative data have numerous, well-documented limitations, including miscoding, whether intentional or from documentation errors [42]. Concerns with administrative data that may affect costs, such as “upcoding,” [43] or understanding clinical complexity are not relevant as they would not affect utilization rates.
Studies of low back pain using administrative data have been criticized for lacking clear definitions and methods, in particular, for not detailing the diagnoses used as inclusion or exclusion criteria and not specifying the diagnosis and procedure codes used [22]. The present study avoids these flaws by presenting transparent methodology.
We required subjects to have continuous medical and pharmaceutical coverage to ensure that quarters with no utilization accurately reflect time periods with no reimbursed low back pain care rather than missing data. Many subjects were likely employed during the entire time period and, as evidenced by the low rate of comorbidities, are likely to be healthier than the US population. Employment has been associated with improvement in functional status due to low back pain [44]. Almost half the subjects received frequent low back pain care; a less healthy population may have greater need.
Conclusions
Research on non-specific low back pain should carefully specify inclusion and exclusion criteria. Research on incident cases should require a symptom-free period of at least 6 months. Results should specify achievement of thresholds rather than mean change.
Acknowledgments
The authors are grateful to Dan Dunn and OptumInsight, Inc. for granting permission to use the Ingenix Impact Research Database.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: GN: Nothing to disclose. CMM: Nothing to disclose. HJC: Nothing to disclose. MS: Nothing to disclose. JFB: Nothing to disclose.
None of the authors have a financial interest in, or conflict of interest regarding, the study methods or results.
References
- 1.Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, et al. Report of the NIH task force on research standards for chronic low back pain. Spine J. 2014;39:1128–43. doi: 10.1097/BRS.0000000000000434. [DOI] [PubMed] [Google Scholar]
- 2.Stanton TR, Latimer J, Maher CG, Hancock MJ. A modified Delphi approach to standardize low back pain recurrence terminology. Eur Spine J. 2011;20:744–52. doi: 10.1007/s00586-010-1671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamper SJ, Stanton TR, Williams CM, Maher CG, Hush JM. How is recovery from low back pain measured? A systematic review of the literature. Eur Spine J. 2011;20:9–18. doi: 10.1007/s00586-010-1477-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Vet HC, Heymans MW, Dunn KM, Pope DP, van der Beek AJ, Macfarlane GJ, et al. Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine. 2002;27:2409–16. doi: 10.1097/01.BRS.0000030307.34002.BE. [DOI] [PubMed] [Google Scholar]
- 5.Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Tosteson ANA, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, Andersson G, et al. Comparative effectiveness evidence from the spine patient outcomes research trial: surgical versus nonoperative care for spinal stenosis, degenerative spondylolisthesis, and intervertebral disc herniation. Spine. 2011;36:2061–8. doi: 10.1097/BRS.0b013e318235457b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radcliff K, Hilibrand A, Lurie JD, Tosteson TD, Delasotta L, Rihn J, et al. The impact of epidural steroid injections on the outcomes of patients treated for lumbar disc herniation: a subgroup analysis of the SPORT trial. J Bone Joint Surg Am. 2012;94:1353–8. doi: 10.2106/JBJS.K.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lurie JD, Moses RA, Tosteson ANA, Tosteson TD, Carragee EJ, Carrino JA, et al. Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine. 2013;38:1216–25. doi: 10.1097/BRS.0b013e31828ce66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Indrakanti SS. Value-based care in the management of spinal disorders: a systematic review of cost-utility analysis. Clin Orthop Relat Res. 2012;470:1106–23. doi: 10.1007/s11999-011-2141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.da C Menezes Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LOP. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012;184:E613–24. doi: 10.1503/cmaj.111271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heuch I, Foss IS. Acute low back usually resolves quickly but persistent low back pain often persists. [12 mo] J Physiother. 2013;59:127. doi: 10.1016/S1836-9553(13)70166-8. [DOI] [PubMed] [Google Scholar]
- 13.Tamcan O, Mannion AF, Eisenring C, Horisberger B, Elfering A, Muller U. The course of chronic and recurrent low back pain in the general population. Pain. 2010;150:451–7. doi: 10.1016/j.pain.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 14.Foster NE. Barriers and progress in the treatment of low back pain. BMC Med. 2011;9:108. doi: 10.1186/1741-7015-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Axen I, Bodin L, Bergstrom G, Halasz L, Lange F, Lövgren PW, et al. Clustering patients on the basis of their individual course of low back pain over a six month period. BMC Musculoskelet Disord. 2011;12:99. doi: 10.1186/1471-2474-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol. 2006;163:754–61. doi: 10.1093/aje/kwj100. [DOI] [PubMed] [Google Scholar]
- 17.Von Korff M. Studying the natural history of back pain. Spine. 1994;19(18 Suppl):2041S–6S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- 18.Ivo R, Nicklas A, Dargel J, Sobottke R, Delank KS, Eysel P, et al. Brain structural and psychometric alterations in chronic low back pain. Eur Spine J. 2013;22:1958–64. doi: 10.1007/s00586-013-2692-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013;14:502–11. doi: 10.1038/nrn3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cassidy JD, Cote P, Carroll LJ, Kristman V. Incidence and course of low back pain episodes in the general population. Spine. 2005;30:2817–23. doi: 10.1097/01.brs.0000190448.69091.53. [DOI] [PubMed] [Google Scholar]
- 21.Carragee E, Alamin T, Cheng I, Franklin T, van den Haak E, Hurwitz E. Are first-time episodes of serious LBP associated with new MRI findings? Spine J. 2006;6:624–35. doi: 10.1016/j.spinee.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Sinnott PL, Siroka AM, Shane AC, Trafton JA, Wagner TH. Identifying neck and back pain in administrative data: defining the right cohort. Spine. 2012;37:860–74. doi: 10.1097/BRS.0b013e3182376508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vogt MT, Kwoh CK, Cope DK, Osial TA, Culyba M, Starz TW. Analgesic usage for low back pain: impact on health care costs and service use. Spine. 2005;30:1075–81. doi: 10.1097/01.brs.0000160843.77091.07. [DOI] [PubMed] [Google Scholar]
- 24.Kominski GF, Heslin KC, Morgenstern H, Hurwitz EL, Harber PI. Economic evaluation of four treatments for low-back pain: results from a randomized controlled trial. Med Care. 2005;43:428–35. doi: 10.1097/01.mlr.0000160379.12806.08. [DOI] [PubMed] [Google Scholar]
- 25.Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. 2007;32:382–7. doi: 10.1097/01.brs.0000254104.55716.46. [DOI] [PubMed] [Google Scholar]
- 26.Hoogendoorn W, Bongers P, de Vet HCW, Ariens G, van Mechelen W, Bouter L. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med. 2002;59:323–8. doi: 10.1136/oem.59.5.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine. 2002;27:901–9. doi: 10.1097/00007632-200205010-00002. [DOI] [PubMed] [Google Scholar]
- 28.Cherkin DC, Deyo RA, Loeser JD. Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases. Spine. 1992;17:817–25. doi: 10.1097/00007632-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Mental health: a report of the surgeon general. Rockville, MD: Substance Abuse and Mental Health Services Administration and the National Institute of Mental Health, U.S Department of Health and Human Services; 1999. [Google Scholar]
- 30.Adams JR, Drake RE. Shared decision-making and evidence-based practice. Community Ment Health J. 2006;42:87–105. doi: 10.1007/s10597-005-9005-8. [DOI] [PubMed] [Google Scholar]
- 31.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: a SAS procedure for latent class analysis. Struct Equ Model. 2007;14:671–94. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Internal Med. 2013;173:1573–81. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Landon BE, Reschovsky JD, O’Malley AJ, Pham HH, Hadley J. The relationship between physician compensation strategies and the intensity of care delivered to Medicare beneficiaries. HSR. 2011;46(6pt1):1863–82. doi: 10.1111/j.1475-6773.2011.01294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hughes DR, Bhargavan M, Sunshine JH. Imaging self-referral associated with higher costs and limited impact on duration of illness. Health Affair. 2010;29:2244–50. doi: 10.1377/hlthaff.2010.0413. [DOI] [PubMed] [Google Scholar]
- 35.Lanza ST, Dziak JJ, Huang L, Wagner AT, Collins LM. Proc LCA & Proc LTA user’s guide (Version 1.3.0) The Pennsylvania State University; University Park: The Methodology Center: 2013. [Google Scholar]
- 36.Buchbinder R, Underwood M. Prognosis in people with back pain (Commentary) CMAJ. 2013;185:325. [Google Scholar]
- 37.Ritzwoller DP, Crounse L, Shetterly S, Rublee D. The association of comorbidities, utilization and costs for patients identified with low back pain. BMC Musculoskelet Disord. 2006;7:72–81. doi: 10.1186/1471-2474-7-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wasiak R, Young AE, Dunn KM, Côté P, Gross DP, Heymans MW, et al. Back pain recurrence: an evaluation of existing indicators and direction for future research. Spine. 2009;34:970–7. doi: 10.1097/BRS.0b013e3181a01b63. [DOI] [PubMed] [Google Scholar]
- 39.Lemeunier N, Kongsted A, Axen I. Prevalence of pain-free weeks in chiropractic subjects with low back pain—a longitudinal study using data gathered with text messages. Chiropr Man Therap. 2011;19:28. doi: 10.1186/2045-709X-19-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tyree PT, Lind BK, Lafferty WE. Challenges of using medical insurance claims data for utilization analysis. Am J Med Qual. 2006;21:269–75. doi: 10.1177/1062860606288774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ. Outcome of low back pain in general practice: a prospective study. BMJ. 1998;316:1356–60. doi: 10.1136/bmj.316.7141.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Riley GF. Administrative and claims records as sources of health care cost data. Med Care. 2009;47(7 Suppl 1):S51–5. doi: 10.1097/MLR.0b013e31819c95aa. [DOI] [PubMed] [Google Scholar]
- 43.Wingert TD, Kralewski JE, Lindquist TJ, Knutson DJ. Constructing episodes of care from encounter and claims data: some methodological issues. Inquiry. 1995;32:430–43. [PubMed] [Google Scholar]
- 44.van Hooff ML, Spruit M, O’Dowd JK, van Lankveld W, Fairbank JC, van Limbeek J. Predictive factors for successful clinical outcome 1 year after an intensive combined physical and psychological programme for chronic low back pain. Eur Spine J. 2013;23:102–12. doi: 10.1007/s00586-013-2844-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


