Abstract
BACKGROUND:
The objective of this study is to determine if point-of-care ultrasound (POCUS) pre-procedure identification of landmarks can decrease failure rate, reduce procedural time, and decrease the number of needle redirections and reinsertions when performing a lumbar puncture (LP).
METHODS:
This was a prospective, randomized controlled trial comparing POCUS pre-procedure identification of landmarks versus traditional palpation for LP in a cohort of patients in the emergency department and intensive care unit.
RESULTS:
A total of 158 patients were enrolled. No significant difference was found in time to completion, needle re-direction, or needle re-insertion when using POCUS when compared to the traditional method of palpation.
CONCLUSION:
Consistent with findings of previous studies, our data indicate that there was no observed benefit of using POCUS to identify pre-procedure landmarks when performing an LP.
KEY WORDS: Ultrasound, Lumbar puncture, Spinal tap
INTRODUCTION
Lumbar puncture (LP) is a procedure that is routinely performed in both the emergency department (ED) and intensive care unit (ICU) to diagnose life-threatening conditions such as meningitis and subarachnoid hemorrhage (SAH).[1] The traditional method to perform an LP relies on palpation to identify landmarks that define the appropriate spinal level for needle insertion. Palpation of these landmarks can be complicated by obesity, prior back surgery, and anatomic variation such as scoliosis.[2,3] These complications can result in failure of the LP. The failure to expeditiously obtain CSF while performing an LP has been estimated to be as high as 38.5% when using the traditional method of palpation of landmarks.[4]
The inability to complete an LP or repeated attempts can negatively impact patient care and result in additional discomfort for the patient.[5,6] Even when LP is successful, it may be complicated by the need for multiple redirections and reinsertions. This has been shown to increase the frequency of traumatic results, thereby obscuring their interpretation.[7,8] Further complications may include damage to surrounding soft tissue, nerve injury, pain and epidural hematoma.[9] In an attempt to increase LP success, prior studies have evaluated point-of-care ultrasound (POCUS) to identify the appropriate inter-spinous space for needle advancement.[10]
The primary objective of this study was to determine if POCUS pre-procedure identification of landmarks can decrease failure rate, reduce procedural time, and decrease the number of needle redirections and reinsertions when performing an LP.
METHODS
Study design
This was a prospective, randomized controlled trial comparing POCUS pre-procedure identification of landmarks versus traditional palpation for LP. The study was approved by the Institutional Review Board.
Study setting and population
The study was performed in a metropolitan level-1 Trauma Center that supports Emergency Medicine and Internal Medicine Residency Programs and Emergency Ultrasound and Critical Care Fellowships. The ED has an annual census of 57 000 patients and the Medical ICU has an annual census of 4 000 patients.
Selection of participants
We enrolled a convenience sample of patients between September 2011 and November 2014. Undergraduate research associates present between the hours of 8 am and midnight sought out any patient undergoing LP in the Emergency Department or Intensive Care Unit for study participation. Patient inclusion criteria included age 18 years and older, ability to provide written and verbal consent in either English or Spanish, and requiring LP as part of their care. All pregnant patients and prisoners were excluded from the study. All patients underwent LP performed by a resident physician, but supervised by attending emergency medicine or internal medicine physician. Physicians involved in data collection included first-year, second-year, and third-year emergency medicine residents and internal medicine residents. All physicians underwent a formal training session which comprised didactic and hands-on components. The didactic portion of the training session included a thirty-minute oral presentation with visual illustrations of how to visualize the spinous process using POCUS. No instruction was given on how to perform an LP using traditional methods.
Study protocol
Any patient requiring a lumbar puncture as part of their treatment or work up that met inclusion criteria were approached by research associates for enrollment in the study. After written, informed consent was obtained, subjects were randomized into one of two groups: the palpation only or the POCUS. Each patient enrolled alternated between the POCUS and palpation groups. All data was collected at bedside by research assistants. For patients in the POCUS group, the physician used ultrasound to identify landmarks prior to needle insertion, not for dynamic guidance. For patients in the palpation only group, the physician palpated the landmarks prior to the LP in the traditional method.
Ultrasound technique
For patients randomized to the POCUS group, ultrasound was used prior to needle insertion to map out the appropriate landmarks. The patient was either positioned lateral recumbent or sitting upright based on whether an opening pressure was required, body habitus and physician preference. A SonoSite Edge ultrasound machine (SonoSite FUJIFILM, Botthell WA) with a 10–5 MHz linear array probe was used for image acquisition. A 5–3 MHZ curvilinear probe could also be used at the physician’s discretion for patients with increased body habitus.
The iliac crests were palpated and used to identify the L4–L5 intervertebral space. The probe was placed in a transverse plane at the level of L5 (Figure 1). The spinous process at this level was visualized by ultrasound and appeared sonographically as a hyperechoic structure with distal shadowing (Figure 2). A skin marking pen was used to mark the midline of the L5 spinous process. The probe was then moved superiorly to visualize the L4 and L3 spinous processes, which were also marked. The probe was removed and the centers of L3, L4 and L5 were marked. The operator was then able to visualize the L4–L5 and L3–L4 intervertebral spaces located between the markings. The patient was then prepared and draped in the usual sterile fashion, and LP was performed using the markings in addition to standard palpation.
Figure 1.

Illustration depicting position of the probe in the transverse plane on the lumbar spine.
Figure 2.
Transverse ultrasound image of the midline lumbar spine. Spinal process is noted in the midline with shadowing distally.
Outcome measures
The primary outcome measures were needle redirections, needle reinsertions, time-to-CSF, and success of procedure by employing POCUS. A redirection was defined as redirecting the spinal needle in an attempt to find the interspinous space following skin penetration. A reinsertion was defined as removing and reinserting the spinal needle into skin. A total of ten attempts of redirections or reinsertions were considered a failed procedure by the study design team given no standard definition of unsuccessful LP. Data were also collected on age, BMI, procedure position and history of prior back surgery.
Data analysis
All data were entered and stored in RedCap,[11] and they were analyzed using Stata SE (Version 13.1, StataCorp, College Station, Tx) statistical software. Categorical data were presented as proportions and percentages. Categorical outcome measures were evaluated using the Chi-Square test or Fischer’s exact test. Intention-to-treat analysis was used for participants who were switched from the palpation to ultrasound group and vice versa. These patients were switched because the physician operator deemed it clinically appropriate. Numerical data were presented as a median value with the interquartile range (IQR). We used the Wilcoxon’s rank- sum test to compare outcomes for each group.
The study was powered to 80% with 95% confidence intervals and 5% alpha error. Sample size was calculated using a statistical calculator (“http://www.dssresearch.com/toolkit/sscalc/size_a2.asp”). Based on this power, 54 participants were needed for each group, or 108 total patients, to give us the desired effect size. This calculation allowed us to determine a calculable difference in number of needle insertions or redirections.
Data were also collected on two sub-populations in which landmark identification has been purported to be difficult: the obese and those with prior back surgery. Obese patients were defined as having a BMI of greater than 30.[12] Patients self-reported whether they had a prior history of back surgery.
RESULTS
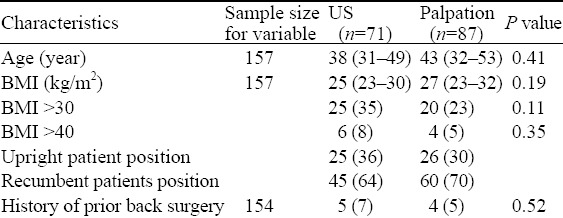
A total of 181 patients were assessed for eligibility and 158 patients were enrolled. Of those participants, 87 were randomized to the palpation group and 71 to the POCUS group (Figure 3). Eleven participants were switched from the POCUS to palpation group and two participants were switched from the palpation to the POCUS group due to provider preference. Within the palpation group, 39 patients were male and 48 patients were female. For the POCUS group, 29 patients were male and 42 patients were female. During the study, 37 unique ED and 22 unique ICU physicians performed the LPs. Demographic and procedural data are shown in Table 1. There was no significant difference in age, BMI, patient positioning, prior back surgery, or first operator level of training between the palpation only and POCUS groups.
Figure 3.
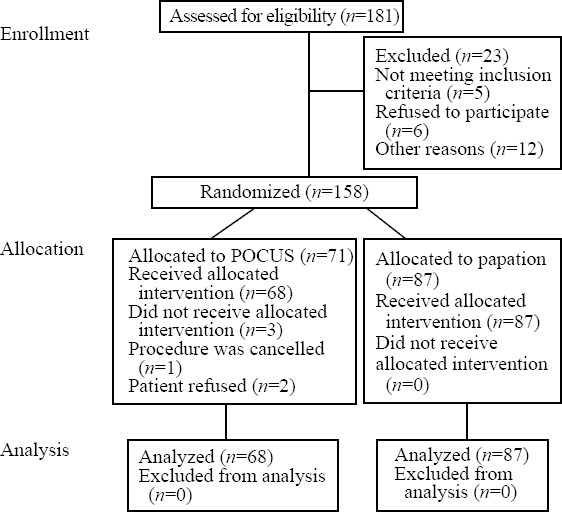
Consort flow diagram illustrating patient distribution.
Table 1.
Comparison of patients in the US and palpation groups
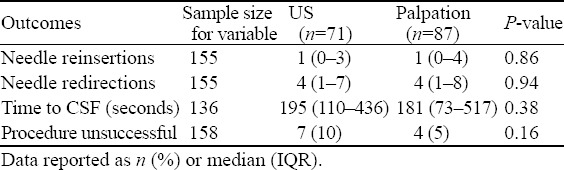
Our data suggest that there was no difference in LP failure rate between the palpation only and POCUS groups (Table 2). In the palpation only group, four LPs were unsuccessful and in the POCUS group, only seven LPs were unsuccessful. Other parameters of LP success, such as needle reinsertion, needle redirection, and time-to-CSF were similar across both groups.
Table 2.
Outcomes for all patients
DISCUSSION
We observed no significant difference in needle redirections, needle reinsertions, time-to-CSF, and success of procedure by employing POCUS. This is consistent with a growing body of the literature that suggests a negligible to small effect of POCUS on the success rate of LP.[13–16] Our study also corroborates similar findings by Peterson et al[15] who found that, in a sample of 100 patients randomized to ultrasound and palpation only groups, there was no benefit of US in reducing procedural success, needle insertions, and procedure time. It is worth noting that Peterson et al[15] also did not find a benefit of US in patients with difficult landmarks. There was a difference, however, in how Peterson et al[15] operationalized difficult landmarks compared to how we operationalized it. Peterson et al[15] operationalized difficult LPs as those considered by the operator to have difficult to palpate landmarks. This measure is subject to operator bias since operators of different experience levels may disagree as to the clarity of a patient’s landmarks. In the present study we defined participants with BMI >30 and participants with a history of back surgery as difficult landmarks in accordance with data showing that it is more difficult to identify landmarks in this population.[2,3] This approach will likely prove more reproducible in the long-run, given less dependence on subjective operator perspective.
Despite these differences, both studies showed an influence of US on LP success in these “difficult to palpate” patients. Trends that favored US were not appreciable in both the Peterson et al[15] and the present study. It is possible that US is still beneficial in other subgroups not defined by Peterson et al[15] or the present study. Other studies have shown that US can improve LP success in pregnant patients[17,18] and would likely be useful in patients with dependent edema (e.g. CHF, cirrhosis). A recent study by Chin et al[19] showed a significant improvement in epidural success when POCUS was used in patients with difficult anatomic landmarks. The difficult landmarks were defined as one or more of the following: (1) BMI >35 kg/m2; (2) at least moderate lumbar scoliosis; and (3) spinal surgery involving removal of two or more spinous processes of the L2–L5 vertebrae. The discrepancy between the Chin study, the Peterson and the present study may be due to the experience of operators. All operators in the Chin study were anesthesia fellows or clinicians with at least 5 years of clinical experience. In contrast, in the Peterson and the present study, operators had varying degrees of clinical experience.
In contrast to the aforementioned studies, a recent meta-analysis by Cho et al[20] aggregated the data of 12 randomized controlled studies that tested the influence of US on LP success. The 12 studies had a sample size range between 30[21] and 370.[17] None of the individual studies showed an independent effect of US on procedure failure. However, when the studies were aggregated, an absolute risk reduction of 0.059 for LP failure was found. The disparity of Cho et al with the present findings and prior studies performed in the ED may be secondary to the aggregation of obstetric patients with ED patients. Obstetric patients are generally younger and healthier than typical ED patients. The findings from the meta-analysis may also suggest that larger studies are needed to truly test the role of US in modifying the failure rate of LPs. The failure rate of LPs was, overall, very low. When combining the failure rate of LPs in our study (11/158) with those of the meta-analysis (50/1 234), only 61 (4.4%) patients out of 1 392 LPs were unsuccessful. Therefore, larger studies may be needed to measure determinants of LP success.
Our study expands the scope of prior studies. The previously performed studies had a small sample size of at most 100 patients. A small enrollment number yields a reduced power to detect a statistically significant result. Meta-analyses, although they benefit from improved sample size, are at risk of publication bias and the combination of multiple studies with unstandardized methodology. The presented study contains the advantages of previous studies such as randomized, prospective design in addition to a larger sample size. Further large, multi-center trials are needed to truly evaluate the influence of US on LP failure rate while avoiding the known caveats of meta-analysis.
Limitations
Our patient population was a convenience sample of patients which may have produced a selection bias. Then, after patients were randomized to an intervention, the patients and providers were not blinded to the type of intervention. Blinding both patients and providers would have been logistically impossible, but by not having blinding may have introduced an additional bias to the study results. Also, because our study took place over the span of three years, it is possible that providers received varied levels of ultrasound training during this time and may have become more experienced as the trial continued. Therefore, there may have been bias as a result of provider ability to perform the POCUS assisted procedure, though hopefully negated by the procedures being averaged out over the academic year. Lastly, we expected differences resulting from user variability to aggregate towards a mean. User variability may have simply increased standard deviations of our effects.
In conclusion, there was no observed benefit of using POCUS when performing an LP. These findings further support the growing body of the literature to support the abandonment of POCUS in trying to increase the success rate of LP.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Lahham S proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006;296:2012–2022. doi: 10.1001/jama.296.16.2012. [DOI] [PubMed] [Google Scholar]
- 2.Ružman T, Gulam D, Haršanji Drenjančević I, Venžera-Azenić D, Ružman N, Burazin J. Factors associated with difficult neuraxial blockade. Local Reg Anesth 7. :47–52. doi: 10.2147/LRA.S68451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55:1122–1126. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 4.de Filho GR, Gomes HP, da Fonseca MH, Hoffman JC, Pederneiras SG, Garcia JH. Predictors of successful neuraxial block: a prospective study. Eur J Anaesthesiol. 2002;19:447–451. doi: 10.1017/s0265021502000716. [DOI] [PubMed] [Google Scholar]
- 5.Seeberger MD, Kaufmann M, Staender S, Schneider M, Scheidegger D. Repeated dural punctures increase the incidence of postdural puncture headache. Anesth Analg. 1996;82:302–305. doi: 10.1097/00000539-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Shah KH, Richard KM, Nicholas S, Edlow JA. Incidence of traumatic lumbar puncture. Acad Emerg Med. 2003;10:151–154. doi: 10.1111/j.1553-2712.2003.tb00033.x. [DOI] [PubMed] [Google Scholar]
- 7.Heasley DC, Mohamed MA, Yousem DM. Clearing of red blood cells in lumbar puncture does not rule out ruptured aneurysm in patients with suspected subarachnoid hemorrhage but negative head CT findings. Am J Neuroradiol. 2005;26:820–824. [PMC free article] [PubMed] [Google Scholar]
- 8.Mazor SS, McNulty JE, Roosevelt GE. Interpretation of traumatic lumbar punctures: who can go home? Pediatrics. 2003;111:525–528. [PubMed] [Google Scholar]
- 9.Evans RW. Complications of lumbar puncture. Neurol Clin. 1998;16:83–105. doi: 10.1016/s0733-8619(05)70368-6. [DOI] [PubMed] [Google Scholar]
- 10.Ferre RM, Sweeney TW. Emergency physicians can easily obtain ultrasound images of anatomical landmarks relevant to lumbar puncture. Am J Emerg Med. 2007;25:291–296. doi: 10.1016/j.ajem.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Vallejo MC, Phelps AL, Singh S, Orebaugh SL, Sah N. Ultrasound decreases the failed labor epidural rate in resident trainees. Int J Obstet Anesth. 2010;19:373–378. doi: 10.1016/j.ijoa.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011;115:94–101. doi: 10.1097/ALN.0b013e31821a8ad4. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.No authors listed. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68:899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 15.Peterson MA, Pisupati D, Heyming TW, Abele JA, Lewis RJ. Ultrasound for routine lumbar puncture. Acad Emerg Med. 2014;21:130–136. doi: 10.1111/acem.12305. [DOI] [PubMed] [Google Scholar]
- 16.Nomura JT, Leech SJ, Shenbagamurthi S, Sierzenski PR, O’Connor RE, Bollinger M, et al. A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med. 2007;26:1341–1348. doi: 10.7863/jum.2007.26.10.1341. [DOI] [PubMed] [Google Scholar]
- 17.Vallejo MC, Phelps AL, Singh S, Orebaugh SL, Sah N. Ultrasound decreases the failed labor epidural rate in resident trainees. Int J Obstet Anesth. 2010;19:373–378. doi: 10.1016/j.ijoa.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Lee WS, Jeong WJ, Yi HY. The usefulness of ultrasound-assisted lumbar puncture on adult patients in the emergency center: comparison with classic lumbar puncture. J Korean Soc Emerg Med. 2008;19:562–568. [Google Scholar]
- 19.Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011;115:94–101. doi: 10.1097/ALN.0b013e31821a8ad4. [DOI] [PubMed] [Google Scholar]
- 20.Cho YC, Koo DH, Oh SK. Comparison of ultrasound-assisted lumbar puncture with lumbar puncture using palpation of landmarks in aged patients in an emergency center. J Korean Soc Emerg Med. 2009;20:304–309. [Google Scholar]
- 21.Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth. 2002;14:169–175. doi: 10.1016/s0952-8180(01)00378-6. [DOI] [PubMed] [Google Scholar]


