Abstract
BACKGROUND:
Hospital emergency department (ED) use by patients from residential aged care facilities (RACFs) is not always appropriate, and this calls for interventions to avoid some unnecessary uses. This study aims to compare patterns of ED use by RACF patients with and without a Hospital in the Nursing Home (HiNH) program.
METHODS:
RACF patients presenting to EDs of a hospital with and a hospital without this program during pre- and post-intervention periods were included. Data on patient demographics and ED presentation characteristics were obtained from the Emergency Department Information System database, and were analysed by descriptive and comparative statistics.
RESULTS:
In both hospitals, most RACF residents presenting to EDs were aged between 75–94 years, female, triaged at scale 3 to 5, and transferred on weekdays and during working hours. Almost half of them were subsequently admitted to hospitals. In accordance with the ICD-10-AM diagnostic coding system, diagnoses that consistently ranked among the top three reasons for visiting the two hospitals before and after intervention included Chapter XIX: injury and poisoning and Chapter X: respiratory diseases. Associated with the intervention, significant decreases in the numbers of presentations per 1 000 RACF beds were identified among patients diagnosed with Chapter XI: digestive diseases [rate ratio (95%CI): 0.09 (0.04, 0.22); P<0.0001] and Chapter XXI: factors influencing health status and contact with health services [rate ratio (95%CI): 0.22 (0.07, 0.66); P=0.007].
CONCLUSION:
The HiNH program may reduce the incidence of RACF residents visiting EDs for diagnoses of Chapter XI and Chapter XXI.
KEY WORDS: Residential aged care, Emergency department, Presenting complaint
INTRODUCTION
Hospital emergency departments (EDs) provide a full range of emergency care for patients who require either immediate treatment for life-threatening illnesses or some less urgent care, accessible 24 hours a day and seven days a week.[1] The EDs play a vital role in providing acute care and access to the hospital care systems in every community; however their ability is limited by the problem of overcrowding which is now occurring worldwide.[2–4]
A substantial demand on the emergency department comes from patients living in residential aged care facilities (RACFs).[5,6] Residents of RACFs represent the frailest population group in society, with chronic disease, atypical symptoms, multiple co-morbidities, cognitive and functional impairment, and social problems.[7–10] Compared with their community-dwelling peers, RACF residents have a higher rate of ED presentations and repeat visits, and are more prone to hospital acquired infections or complications.[11,12] ED utilization by RACF residents is affected by access to general practitioners (GPs), availability of alternate RACF care and primary care, socio-demographic factors, and transportation facilities.[12,13] A considerable proportion of presentations from RACFs to EDs have been considered by previous researchers as inappropriate or avoidable,[8,10] providing the potential to intervene to reduce the burden on EDs from RACF residents. The Hospital in the Nursing Home (HiNH) program in Queensland Australia is such an initiative aimed at reducing unnecessary ED presentations from RACF patients.
A good understanding of the patterns of ED utilisation by RACF residents will have obvious implications for designing better interventions to address RACF population’s complex and special needs and to prevent unnecessary or inappropriate ED use by them. However to date, little is known regarding the current patterns of ED use by aged care residents in Australia and no evaluation has ever been conducted to disclose the impact of the HiNH intervention on the patterns. This study thus aims to determine how the characteristics (particularly the common diagnoses on presentation) of hospital ED visits made by RACF residents changed with the HiNH intervention in Queensland Australia. We hypothesize in this study that, after the intervention, there would be reduced numbers of ED presentations from RACFs with diagnoses that could be relatively simply coped with, while there might be no changes for presentations with other complicated diagnoses.
METHODS
Study design
This was a pre-post controlled study of an intervention (the HiNH program). The HiNH intervention was funded by the Queensland government and operated mainly by a team of ED-based nurses. Major components of the intervention included sending clinical staff from hospitals to RACFs to provide outreach services for RACF patients, and providing support and education for RACF staff and GPs to increase their knowledge and confidence in the acute care for their patients, such that an increased range of procedures (e.g., urinary catheter change, parenteral antibiotic administration, wound care, etc.) could be alternatively provided within patients’ own facilities instead of at EDs. In this study, we examined the general patterns of ED utilization by RACF residents, and whether the patterns (the common presenting complaints, in particular) changed with the intervention.
The study was conducted at the ED of two public hospitals in Queensland Australia: the Royal Brisbane and Women’s Hospital (RBWH, intervention group) and the Logan Hospital (LH, control group). RBWH introduced the HiNH program in February 2006, while LH performed the usual practice. Both hospitals are metropolitan principal referral hospitals located in South East Queensland, providing a similarly wide range of clinical services including emergency care, outpatient and admitted patient services. This study included a pre-test period (from June to August in 2005) and a post-test period (from June to August in 2011). It was likely that the intervention effect would come to a stable status after a reasonable length of implementation (e.g., in 2011), as compared with the very first beginning stage of its implementation. In addition, there were no fundamental changes (e.g., policy changes) within these two hospitals from 2005 to 2011 known to the authors, except that the intervention hospital began to carry out the HiNH program in 2006.
Data collection
Data for this study were sourced from Emergency Department Information System (EDIS), an Australian public hospital information dataset to track patients’ ED episode. This database allowed the identification of people who lived in RACFs and had presentations to the EDs of RBWH (cases) and LH (controls) during the included pre-test and post-test periods. Identification of patients residing in RACFs were based on the following criteria: 1) address and phone number in EDIS matched any accredited RACF; 2) referral or discharge destination coded as RACF; and 3) free text search included any words or recognized abbreviations that indicated an RACF, e.g., nursing home, NH, aged care facility, etc.
The ED case records were then accessed, and for each de-identified patient presentation, we collected the patient’s demographic data (age, gender) and ED presentation related data, including Australasian Triage Scale (ATS) score, International Classification of Diseases (ICD) code, the day and time of ED arrival, and disposition from ED relating to whether the individual was discharged or admitted to hospital). The ATS score contained a five-tier triage scale showing the acuity of presentations (Scale 1 being the most urgent to Scale 5 being the least urgent). Generally, patients grouped to ATS 1 & 2 must be seen immediately, and those grouped to ATS 3–5 could wait and be seen in order of arrival at EDs. The ICD code was grouped into the ICD disease chapters (from chapter I to chapter XXII), according to ICD-10-AM index (10th version, Australian modification), showing patients’ presenting clinical complaints for visiting the ED.
Data analysis
Subject characteristics and patterns of emergency department use were summarized by groups of patients presenting to the ED of RBWH and LH over the pre- and post-test period, in the format of numbers (percentages) for categorical variables. Pearson’s chi-square test was used to identify differences in the frequency distribution of the categorical variables. With regard to the most common presenting complaints, the top ten were summarized as numbers (proportions) of presentations falling into this diagnosis chapter. The top ten diagnoses were identified and ranked, according to the number of presentations with this diagnosis from RACFs as well as the presentation rates (i.e., the numbers of presentations with this diagnosis per 1 000 RACF beds). Poisson log-linear model was adopted to compare whether significant differences exist in the presentation rate for each of the top diagnosis chapters associated with the HiNH intervention. The threshold for statistical significance was P<0.05. Statistical analysis was performed with SPSS v. 21 (IBM Corp., Armonk, NY).
Ethical approval
The study was reviewed and approved by the Ethical Review Committee of the Queensland University of Technology, Brisbane Australia (Reference No.: 1000000457).
RESULTS
A comprehensive search on the EDIS database identified that there were 449 vs. 207 presentations to the EDs from 2 127 vs. 921 RACF beds in the catchment areas of RBWH vs. LH during the pre-intervention period (June to August, 2005). While during the post-intervention period, there were 393 vs. 265 presentations to RBWH vs. LH from 2 485 vs. 1 313 RACF beds. This equaled to 211 vs. 225 ED presentations per 1 000 RACF beds per three months to RBWH vs. LH before intervention, while 158 vs. 202 ED presentations per 1 000 RACF beds to RBWH vs. LH after intervention. From the 3-month pre-intervention to 3-month post-intervention period, the number of presentations to the ED from 1 000 RACF beds decreased by 25.1% in RBWH, while only by 10.2% in LH. In addition, our data showed ED presentations from RACFs accounted for 2.3% and 1.6% of the total presentations during this period in RBWH and LH, respectively.
Patterns of ED use by RACF residents in RBWH and LH were summarized in Table 1. Over the included study periods, the majority of patients presenting to the ED from RACFs were aged between 75 and 94 (73.9% for RBWH and 72.4% for LH) and were females (62.8% for RBWH and 64.6% for LH). Approximately 80% of RACF patients were triaged at ATS 3 to 5 on their ED arrival. They had relatively low acuity of illness and instead of requiring to be seen immediately; they could wait at the ED for clinical assessment and treatment within an acceptable length of time (generally 30 to 120 minutes of maximum waiting time). Over half of RACF transfers arrived at the ED during weekdays (75.4% for RBWH and 73.3% for LH) and normal working hours (60.7% for RBWH and 57.8% for LH). As a result of ED visits, about half of RACF patients were admitted to hospitals (53.7% for RBWH and 55.7% for LH) and the remaining was discharged (46.3% for RBWH and 44.3% for LH). From pre-intervention period to post-intervention period, a decreased percentage of RACF patients (–7.1%) were subsequently admitted in RBWH, while an increased percentage of patients (17.5%) were admitted in LH.
Table 1.
Patterns of emergency department use in RBWH and LH by RACF residents, n (%)
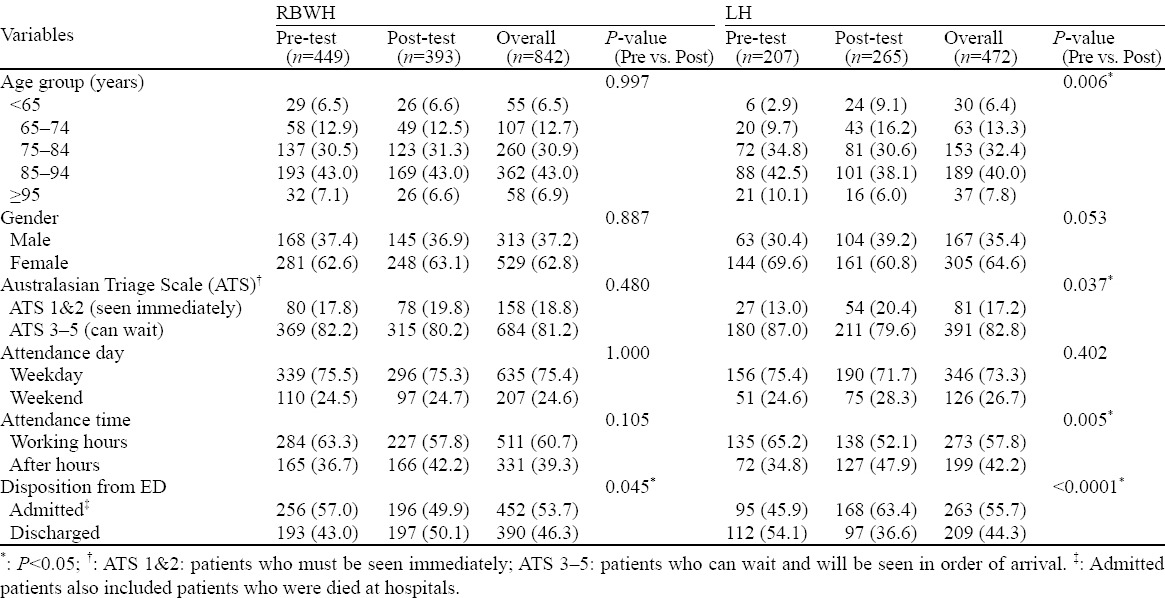
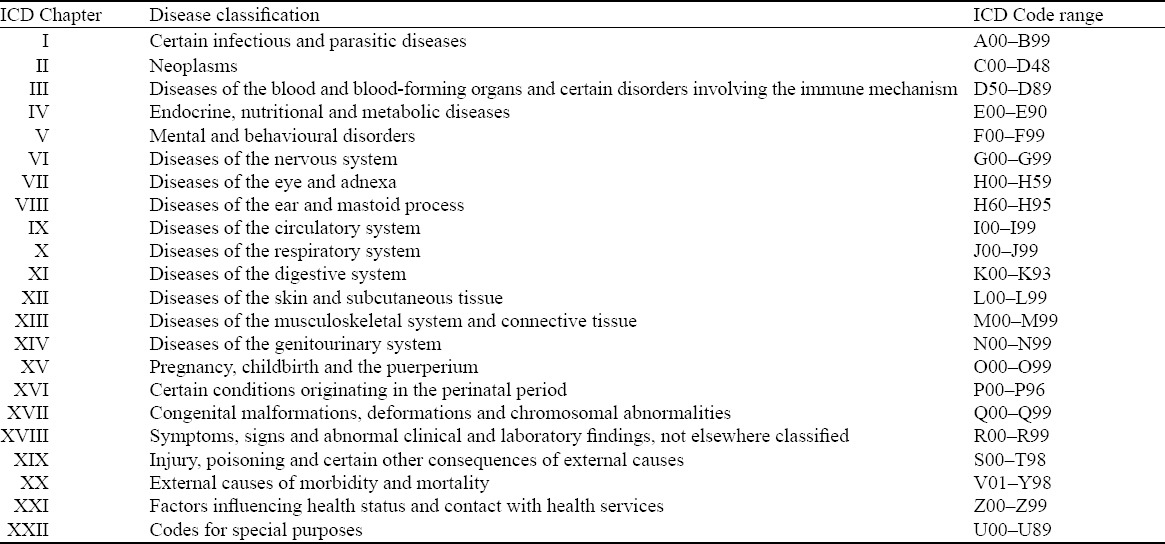
Table 2 presents a list of ICD diagnosis chapters and the ICD code ranges covered by each chapter, based on which we grouped the ICD codes extracted from the EDIS database into the corresponding ICD chapters, from Chapter I to Chapter XXII.
Table 2.
A list of ICD disease chapters and the code ranges covered by each
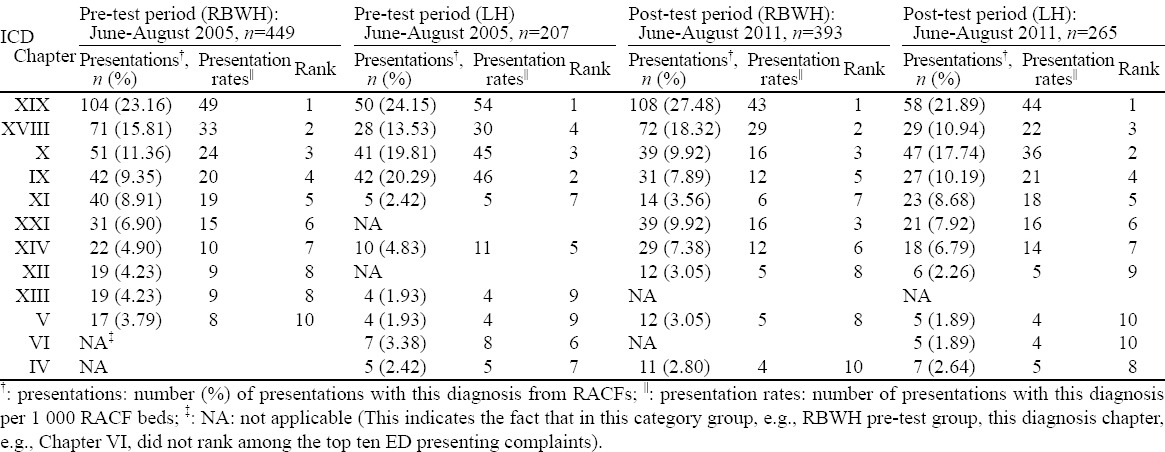
Frequencies of ED presentations falling into each disease chapter were compared, and the ten most common complaints on presentations from RACFs to EDs are shown in Table 3, which also provides a breakdown on people presenting to RBWH and to LH in the pre- and post-intervention period. Chapter XIX: injury and poisoning remained consistently as the most common (No.1) reason for RACF patients’ ED visits, accounting for over one fifth of all presentations (from 21.89% to 27.48%). Chapter X: respiratory diseases were either the second or third commonest reason for ED presentations (ranging from 9.92% to 19.81%). Chapter XVIII: symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified was among the top three medical problems on presentations in LH over the post-test period and in RBWH before and after the intervention, but was ranked fourth in LH over the pre-test period (ranging from 10.94% to 18.32%). Besides, both Chapter IX: circulatory diseases and Chapter XXI: factors influencing health status and contact with health services turned up among the top three reasons once. The remaining disease chapters were all ranked outside the top three but within the top ten most common reasons for ED visits by RACF residents, including Chapter XI: digestive diseases, Chapter XIV: genitourinary disease, Chapter XII: skin and subcutaneous tissue, Chapter XIII: musculoskeletal system and connective tissue, Chapter V: mental and behavioral disorders, Chapter VI: nervous diseases, and Chapter IV: endocrine, nutritional and metabolic diseases, all of which occupied less than 10.0% of all general presentations.
Table 3.
The ten most common reasons for ED presentations by RACF residents in RBWH and LH before and after the HiNH intervention
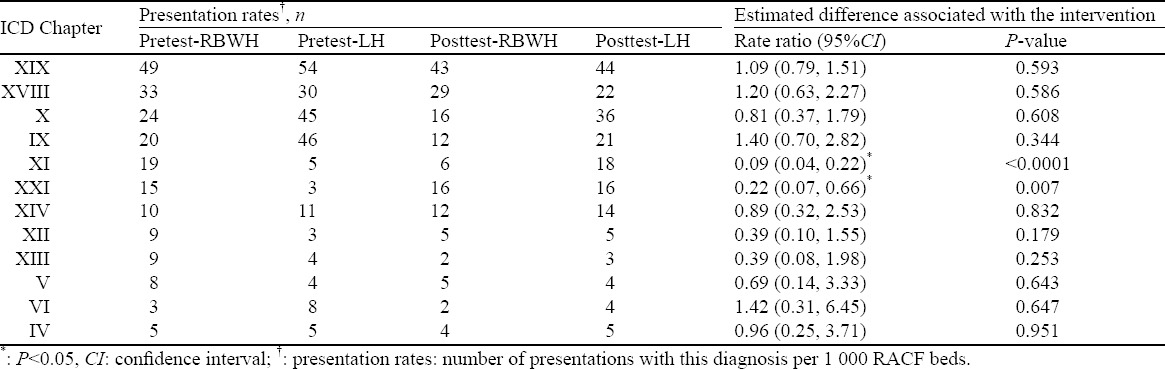
Results of the change in presentation rates associated with implementation of the intervention for each of the identified top diagnoses on ED presentation are illustrated in Table 4. Due to the HiNH intervention, significant decreases were found in the presentation rates with the following presenting diagnoses by RACF residents, including Chapter XI: digestive diseases [ratio (95%CI): 0.09 (0.04, 0.22), P<0.0001] and Chapter XXI: factors influencing health status and contact with health services [ratio (95%CI): 0.22 (0.07, 0.66), P=0.007]. After intervention, there were more RACF patients presenting to the ED with diagnoses of Chapter XIX: injury and poisoning, Chapter XVIII: symptoms, signs and abnormal clinical and laboratory findings, Chapter IX: circulatory diseases, and Chapter VI: nervous diseases; and there were fewer patients with diagnoses falling into Chapter X: respiratory diseases, Chapter XIV: genitourinary disease, Chapter XII: skin and subcutaneous tissue [0.39 (0.20, 0.75), P=0.005], Chapter XIII: musculoskeletal system and connective tissue [0.38 (0.15, 0.96), P=0.040], and Chapter V: mental and behavioral disorders, and Chapter IV: endocrine, nutritional and metabolic diseases. However all of the above did not reach statistical significance.
Table 4.
Comparison of presentation rates by each of the top diagnosis chapters
DISCUSSION
Our study has evaluated the demographics and clinical characteristics of RACF patients presenting to the two hospital EDs in Queensland Australia (one with the HiNH intervention and the other without), in order to improve the understanding of pattern of ED use by RACF residents and the possible influence of the HiNH intervention.
In the present study, RACF residents constituted 2.3% and 1.6% of the total presentations in the two hospitals. Although the percentages are not considerable, these presentations take up a disproportionately large share of acute care resources.[14,15] ED presentations per RACF resident bed per year in the two hospitals ranged from 0.6 to 0.9 over the studied periods. This is consistent with previous studies which found 0.1–1.5 ED transfers per RACF resident/bed per year.[7] Our data showed a substantial decrease (–25.1%) in the ED presentation rate in RBWH when implementing the HiNH intervention from pre- to post-intervention period, decreased by twice as much as that in LH without the intervention. This indicates that the HiNH intervention is likely to reduce unnecessary or avoidable ED presentations from RACFs. Previous studies have similar findings, supporting that 7%–48% of transfers from RACF to ED are considered inappropriate or avoidable if the availability of GPs and access to alternative primary and community care are improved.[16–18]
Our analysis indicates that most RACF residents visiting the ED are aged between 75–94 years, female, and triaged at scale 3 to 5 (relatively low acuity). The majority of them arrived at the ED on weekdays and during normal business hours. There is no peak at weekends. Although EDs operate 24 hours a day, there may be reduced access to senior ED staff and radiology or specialist consultations outside of normal working hours.[6] Almost half of RACF residents presenting to the ED are admitted to the hospital, a consistent finding as one prior study.[15] From three-month pre- to post-intervention period, the likelihood of admissions via the ED decreased by 7.1% in RBWH while increased by 17.5% in LH. This finding may be associated with the HiNH implementation aimed at discharging patients back to their usual residency for alternative acute care to be provided and continued at RACFs. Though the acute hospital services in Australia are of high quality, they are not always in the best interest of RACF residents.[16] Discharging them back to the RACF enables more suitable nursing care to meet their special needs and reduces their susceptibility to hospital-acquired adverse events such as medication errors, falls, infections, delirium, iatrogenic complications, or unnecessary invasive treatment.[5,6]
Consistently in both hospitals before and after the intervention period, the number one reason for ED presentations by RACF residents is Chapter XIX: injury and poisoning, contributing to over one fifth of all visits. This finding is consistent with those reported elsewhere.[11,12,14,17,19] We assume the high rate of injury and poisoning leading to ED attendances may be because such illnesses themselves have high incidence rate and they are potentially more treatable than others or would result in more clinical deteriorations, which thus decreases the threshold for ED utilization. Presentations to the ED also tend to occur in patients with diagnosis of Chapter X: respiratory diseases, which consistently serve as the top three reasons in all groups. However, diagnoses in Chapter X: respiratory diseases, such as pneumonia, are considered as potentially preventable in previous studies.[14,20] These results provide vital messages for designing interventions to improve access to medical care for these most common diagnoses leading to ED presentations from RACFs (such as injury and poisoning, and respiratory diseases), hence reducing the unnecessary ED utilization for these conditions. Besides, Chapter XVIII: symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified also ranked high as the top three reasons in three of the four comparison groups. This is not surprising, owing to the reality that priority of ED care is often to stabilize patient illness and this may sometimes compromise the work on accurate diagnosis.[19]
After implementing the HiNH intervention, there were significant decreases in the numbers of ED visits with the following two of the top presenting complaints, i.e., Chapter XI: digestive diseases and Chapter XXI: factors influencing health status and contact with health services. This may indicate the current HiNH scheme has certain effect on reducing ED visits from RACFs out of the above presenting diagnoses. The HiNH intervention aims at increasing RACF staff’s capacity and confidence in providing with a wider range of acute interventions, such as wound management, parenteral antibiotics or common end of life procedures such as syringe driver management, avoiding emergency presentation and hospital admission. Prior studies also support that some hospital-type care could be alternatively undertaken in the RACFs.[6] However this study also found no significant changes in ED visits under the HiNH scheme with all other top presenting diagnoses, e.g, Chapter XIX: injury and poisoning, Chapter X: respiratory diseases, and Chapter IX: circulatory diseases. This is consistent with findings from one prior study demonstrating that a number of ED presentations from RACFs are still considered appropriate and necessary.[16] This might be owing to the important roles that the ED takes in caring for certain acute illness conditions. For instance, EDs have capacity in providing suitable observations and in performing complex procedures, and are much better equipped with medical facilities such as X-ray facility, all of which are not yet available at RACFs under current circumstances. Enhanced access to care for such conditions might be possible at RACFs, however, requires further careful consideration and planning.
There are limitations to this study. First, this study relied on data from the electronic administrative database of the Australian public hospitals, where the complete clinical records were not yet available. Other important information, such as GP consultation, resource utilization at the ED (e.g., lab and radiological investigations) and co-morbidities of patients, were not evaluated in this study. Second, we included all eligible ED presentations in two hospitals for a three-month period before and after the intervention. However the distribution and pattern of ED visits might vary over the course of the year. It is still unclear how the time of a year would affect the findings.
In conclusion, knowledge regarding patterns of ED presentations by RACF residents is crucial for optimizing the way that the scarce and costly healthcare resources are used as well as ensuring that patients receive the right care in the most appropriate settings. The current study adds to our knowledge in this area. Presentations to the EDs from RACFs tend to occur in patients with diagnosis of Chapter XIX: injury and poisoning and Chapter X: respiratory diseases, which remain consistently among the three most common reasons for ED visits. Emphasis on preventing RACF residents from visiting the ED for injury and poisoning-related and respiratory illnesses could be considered to further improve design of the HiNH program. Organising and delivering ED care to RACF residents represents a complex area for health policy, but alternative care models such as the Hospital in the Nursing Home may assist with reducing acute resource use by this frail population in certain aspects, for instance, decreasing the number of RACF residents visiting EDs for diagnoses of Chapter XI: digestive diseases and Chapter XXI: factors influencing health status and contact with health services.
ACKNOWLEDGEMENTS
This research project is funded by the Queensland Emergency Medicine Research Foundation (QEMRF) (Project ID: QEMRF-PORJ-2009-014, Title: A Comprehensive Evaluation of a Hospital in Nursing Home Program in Three Queensland Hospitals). The funder was not involved in study design, data collection, data analysis, manuscript preparation, and publication decisions. The authors also acknowledge the support from the School of Public Health and Social Work at Queensland University of Technology, the Royal Brisbane and Women’s Hospital, and the Logan Hospital.
Footnotes
Funding: This research project is funded by the Queensland Emergency Medicine Research Foundation (QEMRF) (Project ID: QEMRF-PORJ-2009-014, Title: A Comprehensive Evaluation of a Hospital in Nursing Home Program in Three Queensland Hospitals).
Ethical approval: The study was reviewed and approved by the Ethical Review Committee of the Queensland University of Technology, Brisbane Australia (Reference No.: 1000000457).
Conflicts of interest: None declared.
Contributors: XH, BL, RP and ST initiated the study conception and designed the study. LF, JZ, JS and KD assisted with study design and data analysis. LF drafted the manuscript. All authors contributed to the revision and final approval of the manuscript.
REFERENCES
- 1.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–36.e1. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 3.Nasim MU, Mistry C, Harwood R, Kulstad E, Tommaso L. An attending physician float shift for the improvement of physician productivity in a crowded emergency department. World J Emerg Med. 2013;4:10–14. doi: 10.5847/wjem.j.issn.1920-8642.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fan L, Lukin W, Zhao J, Sun J, Hou X-Y. Interventions targeting the elderly population to reduce emergency department utilisation: a literature review. Emerg Med J. 2015;32:738–743. doi: 10.1136/emermed-2014-203770. [DOI] [PubMed] [Google Scholar]
- 5.Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing. 2014 doi: 10.1093/ageing/afu117. afu117. [DOI] [PubMed] [Google Scholar]
- 6.Briggs R, Coughlan T, Collins R, O’Neill D, Kennelly S. Nursing home residents attending the emergency department: clinical characteristics and outcomes. QJM-Int J Med. 2013 doi: 10.1093/qjmed/hct136. hct136. [DOI] [PubMed] [Google Scholar]
- 7.O’Connell B, Hawkins M, Considine J, Au C. Referrals to hospital emergency departments from residential aged care facilities: Stuck in a time warp. Contemp Nurse. 2013;45:228–233. doi: 10.5172/conu.2013.45.2.228. [DOI] [PubMed] [Google Scholar]
- 8.Arendts G, Howard K. The interface between residential aged care and the emergency department: a systematic review. Age Ageing. 2010;39:306–312. doi: 10.1093/ageing/afq008. [DOI] [PubMed] [Google Scholar]
- 9.Arendts G, Popescu A, Howting D, Quine S, Howard K. ‘They never talked to me about…’: Perspectives on aged care resident transfer to emergency departments. Australas J Ageing. 2015;34:95–102. doi: 10.1111/ajag.12125. [DOI] [PubMed] [Google Scholar]
- 10.Buja A, Fusco M, Furlan P, Bertoncello C, Baldovin T, Casale P, et al. Referral patterns in elderly emergency department visits. Ann Ist Super Sanita. 2013;49:395–401. doi: 10.4415/ANN_13_04_13. [DOI] [PubMed] [Google Scholar]
- 11.Jones JS, Dwyer PR, White LJ, Firman R. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997;4:908–915. doi: 10.1111/j.1553-2712.1997.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 12.Finucane P, Wundke R, Whitehead C, Williamson L, Baggoley C. Profile of people referred to an emergency department from residential care. Aust N Z J Med. 1999;29:494–499. doi: 10.1111/j.1445-5994.1999.tb00749.x. [DOI] [PubMed] [Google Scholar]
- 13.Keskinoğlu P, İnan F. Analysis of emergency department visits by elderly patients in an urban public hospital in Turkey. JCGG. 2014;5:127–131. [Google Scholar]
- 14.Gruneir A, Bell CM, Bronskill SE, Schull M, Anderson GM, Rochon PA. Frequency and pattern of emergency department visits by long-term care residents-a population-based study. J Am Geriatr Soc. 2010;58:510–517. doi: 10.1111/j.1532-5415.2010.02736.x. [DOI] [PubMed] [Google Scholar]
- 15.Wang HE, Shah MN, Allman RM, Kilgore M. Emergency department visits by nursing home residents in the United States. J Am Geriatr Soc. 2011;59:1864–1872. doi: 10.1111/j.1532-5415.2011.03587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finn JC, Flicker L, Mackenzie E, Jacobs IG, Fatovich DM, Drummond S, et al. Interface between residential aged care facilities and a teaching hospital emergency department in Western Australia. Med J Aust. 2006;185:296. doi: 10.5694/j.1326-5377.2006.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 17.Arendts G, Dickson C, Howard K, Quine S. Transfer from residential aged care to emergency departments: an analysis of patient outcomes. Intern Med. 2012;42:75–82. doi: 10.1111/j.1445-5994.2010.02224.x. [DOI] [PubMed] [Google Scholar]
- 18.Bergman H, Carfield AM. Appropriateness of patient transfer from a nursing home to an acute-care hospital: a study of emergency room visits and hospital admissions. J Am Geriatr Soc. 1991;39:1164–1168. doi: 10.1111/j.1532-5415.1991.tb03568.x. [DOI] [PubMed] [Google Scholar]
- 19.Hou X-Y, Tollo S, FitzGerald G. What health problems overcrowd hospital emergency departments in Queensland and has this changed over time?: a case study of two hospitals in Queensland 2001–2009. Australas Epidemiol. 2011;18:10. [Google Scholar]
- 20.Loeb M, Carusone SC, Goeree R, Walter SD, Brazil K, Krueger P, et al. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia. JAMA. 2006;295:2503–2510. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]


