Abstract
BACKGROUND:
Emergencies such as road traffic accidents (RTAs), acute myocardial infarction (AMI) and cerebrovascular accident (CVA) are the most common causes of death and disability in India. Robust emergency medicine (EM) services and proper education on acute care are necessary. In order to inform curriculum design for training programs, and to improve the quality of EM care in India, a better understanding of patient epidemiology and case burden presenting to the emergency department (ED) is needed.
METHODS:
This study is a retrospective chart review of cases presenting to the ED at Kerala Institute of Medical Sciences (KIMS), a private hospital in Trivandrum, Kerala, India, from November 1, 2011 to April 21, 2012 and from July 1, 2013 to December 21, 2013. De-identified charts were systematically sampled and reviewed.
RESULTS:
A total of 1 196 ED patient charts were analyzed. Of these patients, 55.35% (n=662) were male and 44.7% (n=534) were female. The majority (67.14%, n=803) were adults, while only 3.85% (n=46) were infants. The most common chief complaints were fever (21.5%, n=257), renal colic (7.3%, n=87), and dyspnea (6.9%, n=82). The most common ED diagnoses were gastrointestinal (15.5%, n=185), pulmonary (12.3%, n=147), tropical (11.1%, n=133), infectious disease and sepsis (9.9%, n=118), and trauma (8.4%, n=101).
CONCLUSION:
The patient demographics, diagnoses, and distribution of resources identified by this study can help guide and shape Indian EM training programs and faculty development to more accurately reflect the burden of acute disease in India.
KEY WORDS: Emergency care systems, Emergency department, Education, Acute care, Emergency department utilization
INTRODUCTION
Road traffic accidents (RTAs), acute myocardial infarctions (AMIs) and cerebrovascular accidents (CVAs) are the most commonly cited causes of death and disability in India.[1] Emergency medicine (EM) services—acute medical care that is delivered within the first few hours of the onset of treatable acute conditions,[2,3] can help better manage the most commonly presenting Indian injuries and diseases to ensure better clinical outcomes. Despite the acceptance of EM as a specialty in many high-income countries, India has lagged in developing specialty training to address the needs of the presenting disease burden.
The World Health Organization (WHO) estimates in their 2013 report on road safety that India experiences 18.9 traffic-related deaths per 100 000 people and that globally India accounts for 10% of all road-related fatalities.[4] Despite having only 1% of total motor vehicles in the world, India accounts for 6% of the global burden of RTAs.[5] Compared to traffic-related deaths in other low and middle income neighboring countries, India’s incidence of RTAs is alarmingly high and is projected to increase by 2020.[4] According to the Indian NGO, SaveLIFE Foundation, in 2013 there was one road death approximately every four minutes in India,[6] resulting in 377 fatalities every day from RTAs. In addition to Indian road traffic mortality, there were 1 287 unintentional injuries per day from RTAs.[6] Despite global advancements in road safety and injury prevention, Indian fatalities from RTAs have consistently increased every year, from 18.1% in 2002 to 24.4% in 2011.[7] The severity of RTAs, measured in terms of persons killed per 100 accidents, has also increased, from 20.8 to 28.6 in 2011.[7] While engineers have designed safer roads and cars, many common safety habits and features—the “4Es”-Enforcement, Engineering, Education and Encouragement—still lack wide adoption in India.[7]
Cardiovascular disease (CVD) is also increasing in India, especially in urban areas.[8,9] A recent study in India found that almost 80 percent of all study participants had two or more risk factors for CVD.[10] Unlike high-income countries where only 67% of deaths from CVD occur after the age 70, in India 52% of deaths from CVD occur in people under 70 years of age. Eighty percent of the world’s heart disease occurs in low and middle income countries,[11] and with a population of 1.2 billion people and GDP per person of $1,630 in 2014,[12] India will bear a significant portion of the world’s CVD. Managing medical CVD-induced emergencies, such as AMIs and CVAs, will place enormous strain of emergency services.
Despite the effectiveness of emergency care, poor access to emergency medical services remains a problem in low- and middle-income countries.[2] In India there is little understanding and research[13] as to what specific knowledge base and skillsets are required to provide appropriate emergency care. While the core concepts of EM are internationally universal, the application of these concepts must be adapted to practice realities, legislation and culture of individual countries.[14] The Medical Council of India formally recognized EM as a specialty in 2009 and the National Board of Examinations created the Diplomate of the National Board for EM residencies in 2013. However, increasing urbanization and rapidly changing disease patterns will require significant research to inform the continued development of Indian EM. A better understanding of the unique demographics and presenting illnesses of Indian ED patients can inform curriculum development and associated learning activities for Indian EM residencies and other associated training programs. This paper describes one private, peri-urban hospital’s emergency department (ED) patient population and associated burden of disease, offers a model for collecting and analyzing emergency department data in other hospitals in India, and provides data to inform EM curricula.
METHODS
The study is a retrospective chart review of records from cases that presented to the ED at the Kerala Institute of Medical Sciences (KIMS), a 600-bed, private hospital located in Trivandrum, Kerala from November 1, 2011 to April 21, 2012, and from July 1, 2013 to December 21, 2013. The study period was chosen over two years in order to minimize seasonal variation of patient epidemiology and to avoid a period of transition of medical record keeping format from paper to electronic. This study was approved by the Boston University Institutional Review Board as well as by the Medical Superintendent at KIMS.
The primary outcomes included the mode of arrival, chief complaint, diagnosis group, and disposition. Secondary outcomes included procedures, diagnostic studies performed, and consultants involved in ED care. Demographics collected included patient gender and age group. Frequencies and percentages were calculated for all variables.
A total of 1 529 ED records were systematically sampled from KIMS over the study period. Two research assistants collected data from paper and electronic medical records and entered it into a password-protected Excel template. All records were treated equally; in order to preserve randomization, records with low data quality or missing information were included in the data collection process. Ultimately 333 ED records were excluded due to large amounts of missing data. All analysis was performed using SAS 9.3 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
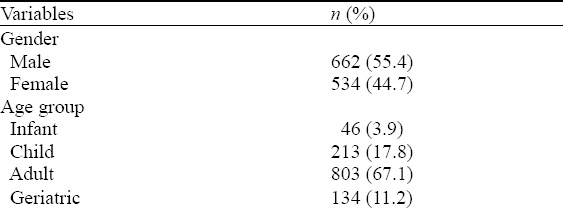
A total of 1 196 ED patient charts were analyzed. Of these patients, 55.4% (n=662) were male and 44.7% (n=534) were female. Table 1 shows the ages of the patients seen: the majority (67.1%, n=803) of the patients were adults, while only 3.9% (n=46) were infants.
Table 1.
Gender and age distribution
Mode of arrival
The majority of patients (52.5%, n=625) presented on their own accord, while 13.4% (n=159) of cases were referred. Only 7.5% (n=89) of patients came by ambulance.
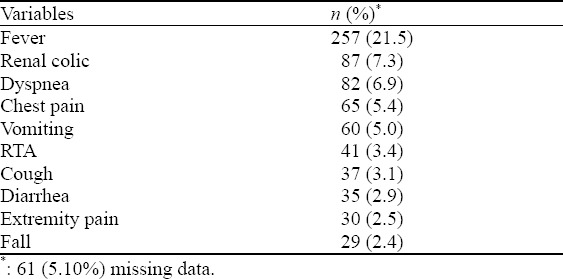
Chief complaint
The most common chief complaints were fever (21.5%, n=257), renal colic (7.3%, n=87), and dyspnea (6.9%, n=82), as shown in Table 2.
Table 2.
Chief complaints
ED diagnosis
The most common ED diagnosis categories were gastrointestinal (15.5%, n=185), pulmonary (12.3%, n=147), tropical (11.1%, n=133), infectious disease and sepsis (9.9%, n=118), and trauma (8.4%, n=101). Tropical diagnoses included endemic vector-borne infectious diseases such as malaria, dengue, and leptospirosis.
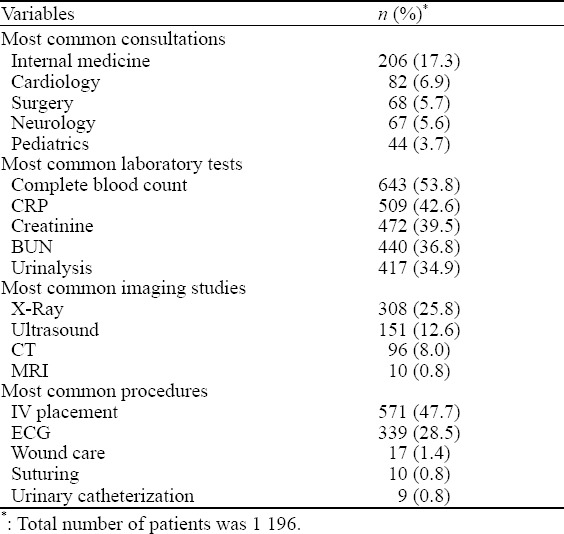
ED resource utilization
ED procedures were performed on 58.9% (n=704) of patients. The most common procedures were intravenous catheter (IV) placement (47.7%, n=571) and electrocardiography (ECG) (28.5%, n=339), as shown in Table 3. The most common tests requested were complete blood count (CBC) (53.8%, n=643) and X-rays (25.8%, n=308), as shown in Table 3. The most commonly requested consultations were internal medicine, cardiology and surgery.
Table 3.
ED resource utilization
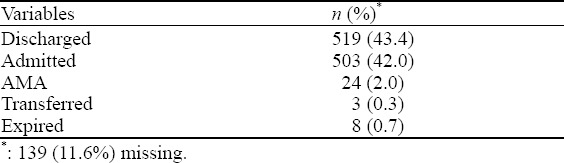
Disposition
The admission rate of patients at KIMS was 42% (Table 4), much higher than the 11.9% admission rate in the Unites States.[15]
Table 4.
Disposition
DISCUSSION
A thorough literature search for comparable papers showing a systematic sample of ED patient epidemiology or resource utilization in India did not reveal any similar studies. This paper provides baseline documentation on emergency department disease burden and resource utilization in an Indian emergency department. Analysis of the data in this study reveals some differences between India and the US. These differences suggest that the acute conditions addressed in EM curriculum and training in India may be somewhat different from those in the United States (U.S.) or other countries.
Patient epidemiology
A comparison with U.S. ED statistics from the National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Tables[15] provides some interesting observations about the differences in Indian versus U.S. ED epidemiology. As most Indians pay for medical services out-of-pocket and are not protected by insurance or legislation like The Emergency Medical Treatment and Labor Act (EMTALA) that require the ED to treat them, Indian self-referral patterns are much different than in the U.S. The ED is a medical resource of last resort in India and as such, the acuity of patients presenting to the ED is typically higher than in the U.S. Another important difference with the U.S. is the frequency of infectious disease as a presenting condition in the ED.
Chief complaints
In India the majority of chief complaints for EM visits are due to tropical diseases, cardiac complaints and trauma. Fever, usually indicative of an infectious disease, was the number one chief complaint. Renal colic was the second chief complaint in this study, supporting prior hypotheses that climate, type of food and dietary practice may play a role in the development of kidney stones. Based on the frequency of these two chief complaints, EM faculty training and EM curriculum should emphasize managing infectious disease emergencies and episodes of acute renal colic.
Procedures
In both the U.S. and this particular Indian ED, IV placement was the most frequent emergency procedure.[15] However, the Indian ED provided more procedures for acute and minor trauma care (ECG, wound care and suturing) than U.S. emergency departments, where the top procedures after IV placement were splint wraps, suturing, and nebulization.
As the Diplomate of the National Board (DNB) in Emergency Medicine is introduced and physicians pursue post-graduate degrees in this new Indian specialty, it may be beneficial to reflect on this study’s findings in order to develop programming to prepare Indian EM doctors for the types of patients and pathology they are most likely to see. In the U.S. Model of the Clinical Practice of Emergency Medicine[16] and the American Board of Emergency Medicine Qualifying Exam, the epidemiology of disease burden is used to determine the relative importance of acute conditions for their curricula and exam. In the U.S. where cardiovascular and trauma emergencies predominate, the examiners emphasize cardiovascular (10%) and trauma emergencies (10%).[17] Because of the prevalence of infectious and tropical disease in India, it would seem prudent to develop curriculum, training programs and examinations that emphasize the clinical pathological spectrum of infectious disease and antibiotic selection.
The EM DNB was formally launched in 2014 and the working curriculum[18] is based on U.S. and U.K. curricula and Indian EM residency programs that started in private hospitals prior to its introduction. As this paper demonstrates, the epidemiology and case burden of patients seen in Indian EDs is different from programs that were developed for more established EDs in high-income countries. The Indian EM curriculum needs to reflect infectious and tropical disease that is indigenous to the subcontinent, as well as prioritize preparing doctors for acute care trauma care and the management of cardiovascular and neurological emergencies. A review of curricula based on the epidemiology of acute conditions from this study and future studies should result in development of practical and relevant training programs. The authors also recommend that if funding permits, this study be extended to a medical trust, a government medical college, and a rural emergency medicine department in India to more fully describe, better understand, and prepare clinical staff for the wide variety of patients that present to Indian EDs for acute care.
Limitations
The authors acknowledge that there were some limitations to conducting this study. These limitations include the fact that there was some data missing; this finding highlights the importance of consistent record keeping and uniform terminology. This is a single, private hospital site in south India, therefore the results should not be generalized to other hospitals or settings; rather, the results are a source of preliminary data that should be built upon if time and funding permits. The authors recommend that this study be conducted in hospitals outside southern India (North, East and West) and at public hospitals as their case burden is different than that of private hospitals.
In conclusion, the patient demographics and diagnosis list generated by this study can help guide and shape Emergency Medicine programs and faculty development in India to more accurately reflect the burden of disease. Unlike high-income countries, India requires a different emphasis on key skills that reflect infectious disease, trauma and the care of CVA and neurological emergencies. The findings should also be utilized to inform key stakeholders including the National Board of Examinations, and funders of Emergency Medicine development in India.
Footnotes
Funding: None.
Ethical approval: This study was approved by the Boston University Institutional Review Board as well as by the Medical Superintendent at KIMS.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Clark EG proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.Arora P, Bhavnani A, Kole T, Curry C. Academic emergency medicine in India and international collaboration. Emerg Med Australas. 2013;25:294–296. doi: 10.1111/1742-6723.12110. [DOI] [PubMed] [Google Scholar]
- 2.Periyanayagam U, Dreifuss B, Hammerstedt H, Chamberlainc S, Nelsonc S, Boscoc KJ, et al. Acute care needs in a rural sub-saharan African emergency center: a retrospective analysis. African J Emerg Med. 2012;2:151–158. [Google Scholar]
- 3.David SS, Vasnaik M, T VR. Emergency medicine in India: why are we unable to ‘walk the talk’? Emerg Med Australas. 2007;19:289–295. doi: 10.1111/j.1742-6723.2007.00985.x. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Road Safety Prevention. Secondary Road Safety Prevention. http://www.searo.who.int/india/topics/road_safety_and_injury_prevention/en/
- 5.Joshipura MK, Shah HS, Patel PR, Divatia PA, Desai PM. Trauma care systems in India. Injury. 2003;34:686–692. doi: 10.1016/s0020-1383(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 6.SaveLifeFoundation. Secondary. http://savelifefoundation.org/wp-content/uploads/2014/10/2013-Fact-Sheet_October1.pdf .
- 7.Oestern HJ, Garg B, Kotwal P. Trauma care in India and Germany. Clin Orthop Relat Res. 2013;471:2869–2877. doi: 10.1007/s11999-013-3035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nag T, Ghosh A. Cardiovascular disease risk factors in Asian Indian population: A systematic review. J Cardiovasc Dis Res. 2013;4:222–228. doi: 10.1016/j.jcdr.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Heart Federation. Secondary. http://www.world-heart-federation.org/press/releases/detail/article/reasons-for-indias-growing-cardiovascular-disease-epidemic-pinpointed-in-largest-ever-risk-factor/
- 10.Sekhri T, Kanwar RS, Wilfred R, Chugh P, Chhillar M, Aggarwal R, et al. Prevalence of risk factors for coronary artery disease in an urban Indian population. BMJ Open. 2014;4:005346. doi: 10.1136/bmjopen-2014-005346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HealthLine. Secondary. http://www.healthline.com/health/heart-disease/statistics-1 .
- 12.World Bank. Secondary. http://data.worldbank.org/indicator/NY.GDP.PCAP.CD .
- 13.Aggarwal P, Banga A, Kurukumbi M, Gupta M. Emergency physicians and emergency medicine: an imminent need in India. Natl Med J India. 2001;14:257–259. [PubMed] [Google Scholar]
- 14.Pothiawala S, Anantharaman V. Academic emergency medicine in India. Emerg Med Australas. 2013;25:359–364. doi: 10.1111/1742-6723.12095. [DOI] [PubMed] [Google Scholar]
- 15.CDC. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. 2011 [Google Scholar]
- 16.American Board of Emergency Medicine. Model of the Clinical Practice of Emergency Medicine. Secondary Model of the Clinical Practice of Emergency Medicine. https://http://www.abem.org/public/docs/default-source/publication-documents/2013-em-model—website-documentD861F66050B0.doc?sfvrsn=4 .
- 17.American Board of Emergency Medicine. Qualifying Examination Description and Content Specifications. Secondary Qualifying Examination Description and Content Specifications. https://http://www.abem.org/public/emergency-medicine-%28em%29-initial-certification/qualifying-examination/qualifying-examination-description-and-content-specificiations .
- 18.National Board of Examiners. Guidelines for Competency Based Training Programme in DNB- Emergency Medicine. 2013 [Google Scholar]


