Abstract
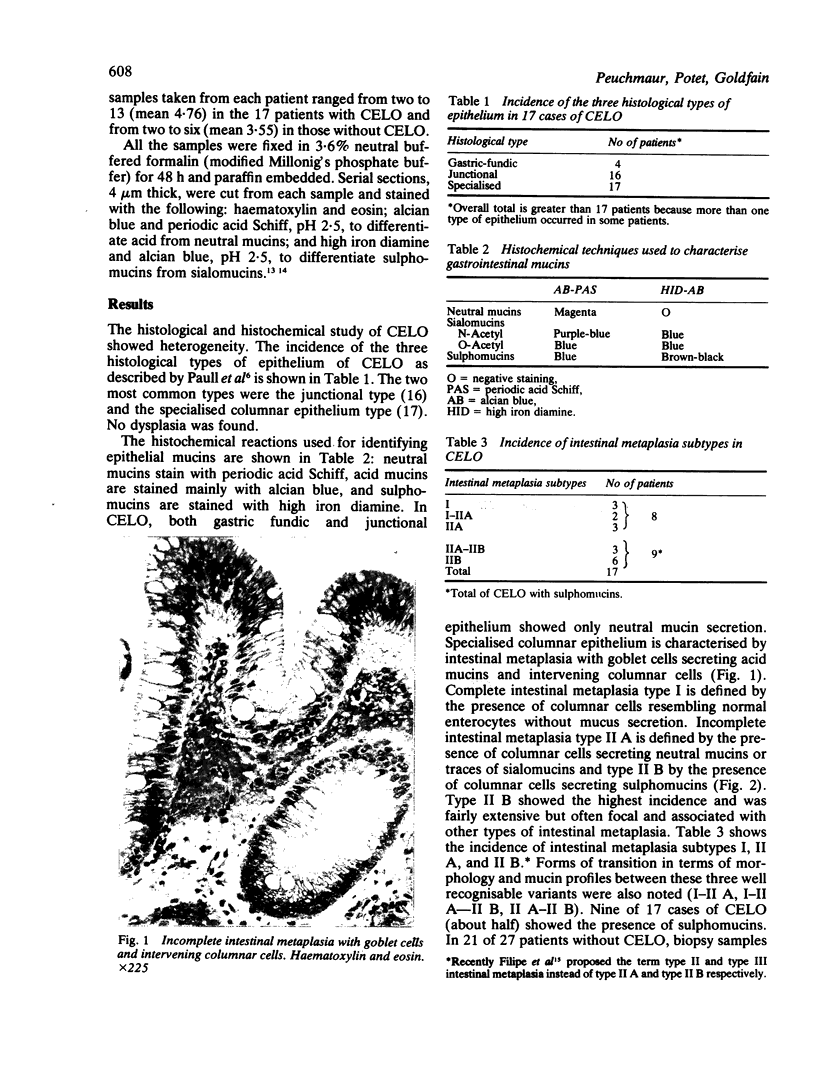
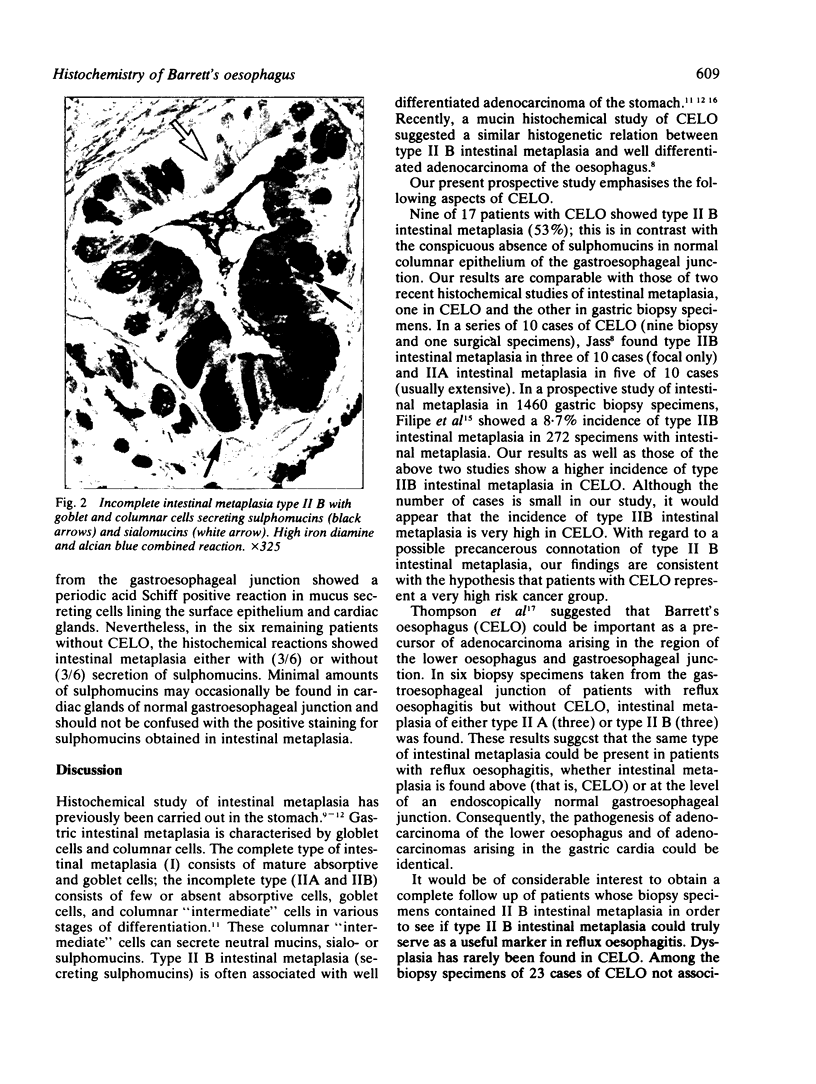
Columnar epithelium-lined oesophagus (CELO) is an acquired disorder associated with a high incidence of cancer. CELO consists of three histological types of epithelium: gastric-fundic, junctional, and specialised columnar, the last resembling intestinal metaplasia of the stomach. In a previous study of CELO an incompletely differentiated variant of intestinal metaplasia secreting sulphomucins (type II B) was found. This was shown to be associated with well differentiated adenocarcinoma, as in the stomach. The purpose of this paper has been to define by histochemistry the mucin profile of CELO in 17 patients and to compare it with the mucin profile of the gastroesophageal junction in 27 patients without CELO. In CELO a specialised columnar epithelium was always found and type II B intestinal metaplasia (with sulphomucins) showed the highest incidence (53%). In normal subjects, this type of intestinal metaplasia was found in only three of 27 cases. Type II B intestinal metaplasia has often been considered as a precancerous lesion or as an equivalent of dysplasia; consequently, its high incidence in our study on CELO raises the question of whether this lesion should be considered a high risk condition for adenocarcinoma of the lower oesophagus.
Full text
PDF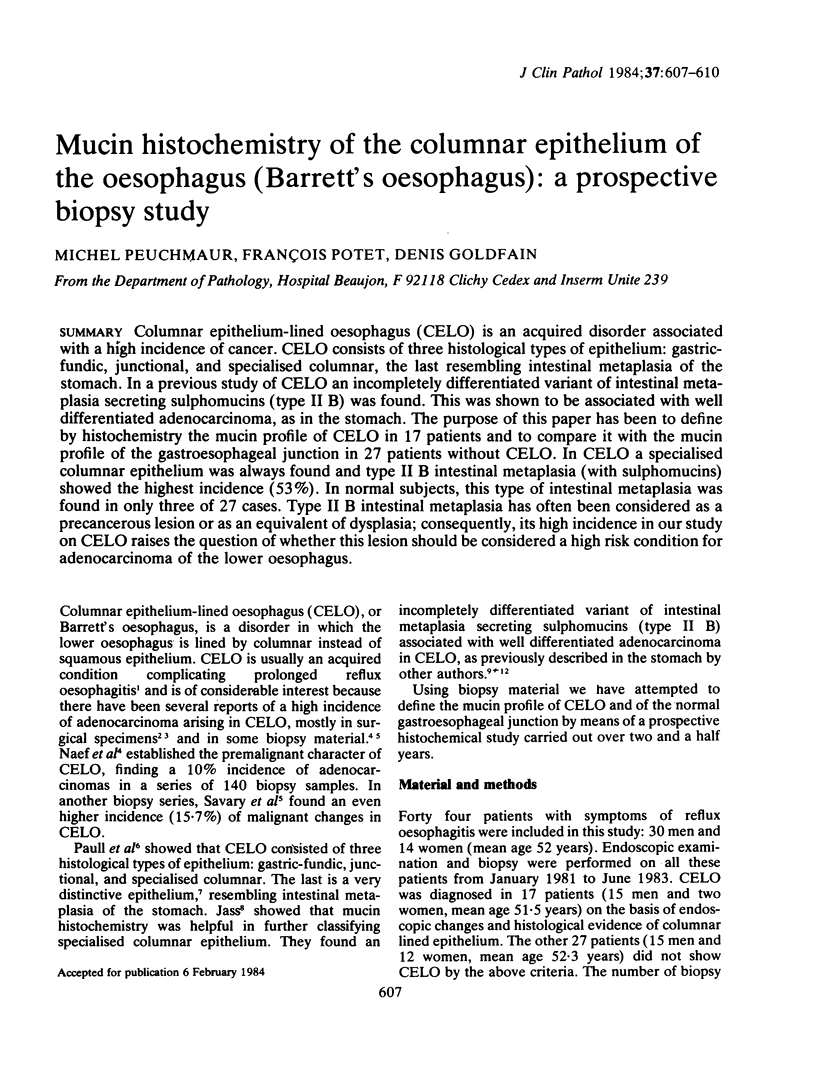

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berenson M. M., Riddell R. H., Skinner D. B., Freston J. W. Malignant transformation of esophageal columnar epithelium. Cancer. 1978 Feb;41(2):554–561. doi: 10.1002/1097-0142(197802)41:2<554::aid-cncr2820410223>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Bremner C. G., Lynch V. P., Ellis F. H., Jr Barrett's esophagus: congenital or acquired? An experimental study of esophageal mucosal regeneration in the dog. Surgery. 1970 Jul;68(1):209–216. [PubMed] [Google Scholar]
- Haggitt R. C., Tryzelaar J., Ellis F. H., Colcher H. Adenocarcinoma complicating columnar epithelium-lined (Barrett's) esophagus. Am J Clin Pathol. 1978 Jul;70(1):1–5. doi: 10.1093/ajcp/70.1.1. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. A variant of intestinal metaplasia associated with gastric carcinoma: a histochemical study. Histopathology. 1979 May;3(3):191–199. doi: 10.1111/j.1365-2559.1979.tb02996.x. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. Sulphomucins and precancerous lesions of the human stomach. Histopathology. 1980 May;4(3):271–279. doi: 10.1111/j.1365-2559.1980.tb02921.x. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. The mucin profiles of normal gastric mucosa, intestinal metaplasia and its variants and gastric carcinoma. Histochem J. 1981 Nov;13(6):931–939. doi: 10.1007/BF01002633. [DOI] [PubMed] [Google Scholar]
- Jass J. R. Mucin histochemistry of the columnar epithelium of the oesophagus: a retrospective study. J Clin Pathol. 1981 Aug;34(8):866–870. doi: 10.1136/jcp.34.8.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jass J. R. Role of intestinal metaplasia in the histogenesis of gastric carcinoma. J Clin Pathol. 1980 Sep;33(9):801–810. doi: 10.1136/jcp.33.9.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsukura N., Suzuki K., Kawachi T., Aoyagi M., Sugimura T., Kitaoka H., Numajiri H., Shirota A., Itabashi M., Hirota T. Distribution of marker enzymes and mucin in intestinal metaplasia in human stomach and relation to complete and incomplete types of intestinal metaplasia to minute gastric carcinomas. J Natl Cancer Inst. 1980 Aug;65(2):231–240. [PubMed] [Google Scholar]
- Naef A. P., Savary M., Ozzello L. Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett's esophagus with 12 adenocarcinomas. J Thorac Cardiovasc Surg. 1975 Nov;70(5):826–835. [PubMed] [Google Scholar]
- Paull A., Trier J. S., Dalton M. D., Camp R. C., Loeb P., Goyal R. K. The histologic spectrum of Barrett's esophagus. N Engl J Med. 1976 Aug 26;295(9):476–480. doi: 10.1056/NEJM197608262950904. [DOI] [PubMed] [Google Scholar]
- SPICER S. S. DIAMINE METHODS FOR DIFFERENTIALING MUCOSUBSTANCES HISTOCHEMICALLY. J Histochem Cytochem. 1965 Mar;13:211–234. doi: 10.1177/13.3.211. [DOI] [PubMed] [Google Scholar]
- Skinner D. B., Walther B. C., Riddell R. H., Schmidt H., Iascone C., DeMeester T. R. Barrett's esophagus. Comparison of benign and malignant cases. Ann Surg. 1983 Oct;198(4):554–565. doi: 10.1097/00000658-198310000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson J. J., Zinsser K. R., Enterline H. T. Barrett's metaplasia and adenocarcinoma of the esophagus and gastroesophageal junction. Hum Pathol. 1983 Jan;14(1):42–61. doi: 10.1016/s0046-8177(83)80045-8. [DOI] [PubMed] [Google Scholar]
- Trier J. S. Morphology of the epithelium of the distal esophagus in patients with midesophageal peptic strictures. Gastroenterology. 1970 Apr;58(4):444–461. [PubMed] [Google Scholar]




