Abstract
Objective
Although psychoeducation has been found effective for improving the life functioning of patients with schizophrenia in high income countries, there have been relatively few studies of schizophrenia psychoeducation adapted for low and middle-income countries (LMIC), particularly in Southeast Asia. The present study assessed effects of the Family Schizophrenia Psychoeducation Program (FSPP) among Vietnamese patients and their families on the patients’ (1) quality of life and (2) medication non-compliance, and the family and patients’ (3) stigma towards schizophrenia, and (4) consumer satisfaction.
Method
This intervention study involved 59 patients, and their families, from the Da Nang Psychiatric Hospital, randomly assigned to treatment (n=30) or control (n=29) conditions. Control subjects received services as usual (antipsychotic medication); treatment group subjects received the FSPP as well. Blind-rater assessments were conducted at T1 immediately after project enrollment (prior to participating in the FSPP) and at T2 six months later.
Results
There were significant treatment effects on: (1) quality of life, (2) stigma, (3) medication compliance, and (4) consumer satisfaction, with all effects favoring the treatment group. Effect sizes were moderate to large.
Conclusions
This psychoeducation program appears to reduce stigma, improve quality of life and medication compliance, and increase consumer satisfaction of Vietnamese patients with schizophrenia and their families, beyond the effects of antipsychotic medication. It involves relatively little cost, and it may be useful for it or equivalent programs to be implemented in other hospitals in Viet Nam, and potentially other low-income Asian countries to improve the lives of patients with schizophrenia.
Keywords: Psychoeducation, schizophrenia, stigma, quality of life, medication compliance, Vietnam
1. INTRODUCTION
Schizophrenia is a chronic disorder with a prevalence of a little less than 1 % of the general population across the world (Jablensky, 2000). In addition to its core symptoms of delusions, etc., the disorder is associated with life functioning impairment in a variety of domains (e.g., occupational functioning; social functioning) as well as social stigma (Galuppi et al., 2012). Many of these negative secondary effects, however, often are the result of misunderstandings by patients and their families about schizophrenia as a medical disorder, rather than inherent to the disorder. For instance, families with a member with schizophrenia sometimes believe that it is best for the patient to rest at home, rather than having a job, developing social relationships outside the family, etc. As a consequence, the patient’s life becomes restricted and their life functioning and quality of life are diminished. However, the reality is that if the patient is successfully treated, he or she can have a relatively fulfilling life with a career, their own family, etc. (Gaebel, 2011).
In high income Western countries, psychoeducation is used to help patients with schizophrenia achieve such better outcomes. Psychoeducation provides patients and families with accurate information about schizophrenia, about the potential for patients with schizophrenia to lead productive lives when successfully treated, and reduces stigma (Kulhara et al., 2009); psychoeducation also has been found to increase medication compliance among patients with schizophrenia (Rummel-Kluge et al., 2008). Unfortunately, use of psychoeducation is not widespread in Asia, in particular in Southeast Asian countries like Viet Nam. In fact, to the best of our knowledge, at the time of the present study there were no schizophrenia psychoeducation programs being provided in Viet Nam. Therefore, the purposes of the present study were to (a) develop a schizophrenia psychoeducation program adapted for Viet Nam, and (b) to conduct an initial randomized evaluation of the program to determine if a full scale evaluation would be justified. Outcomes included patient and family reports for (1) stigma towards schizophrenia, and the patients’ (2) quality of life, (3) medication compliance, and (4) consumer satisfaction with the program. The research study was conducted at the Da Nang (Viet Nam) Psychiatric Hospital from March, 2014 to July, 2015 and was sponsored by the U.S. National Institutes of Health. The trial was registered with ClinicalTrials.gov (DPH20140818).
2. Methods
2.1 Study site, participants, and sampling
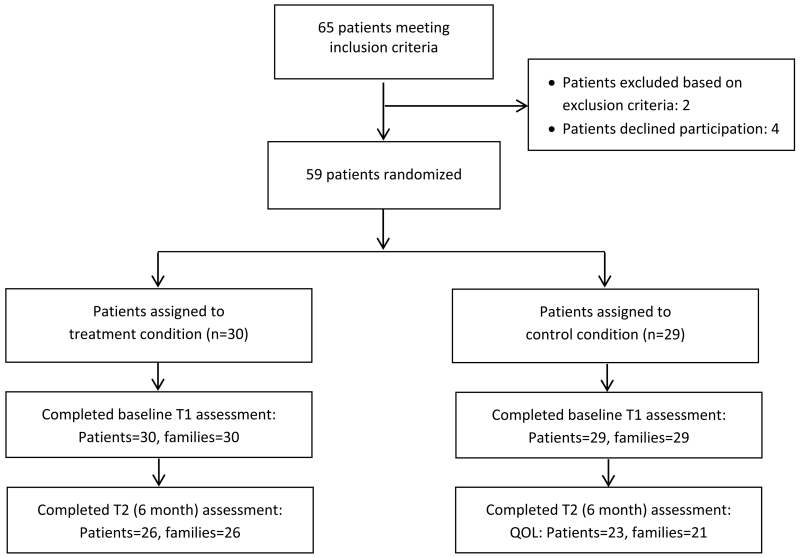
Study participants were recruited from the Danang Psychiatric Hospital, the primary mental health facility in central Viet Nam and the third largest psychiatric hospital in the country. Study inclusion criteria were: (a) an ICD-10 diagnosis of schizophrenia (F20.x); (b) no more than 3 prior psychiatric hospitalizations including the current one; (c) a duration of less than three years for their schizophrenia; (d) age between 18-30 years; (e) the family living within 50 kilometers of the hospital (in order that follow-up interviews which took place in the patient’s home be feasible). Exclusion criteria were suicidal ideation. Study consent was obtained from both the patient and the patient’s family. Families were informed about the study and recruited after the intake session at the hospital; patients were informed about the study and recruited after their psychosis was controlled with medication, typically about two weeks after entering the hospital. A total of 65 patients met the inclusion criteria, 2 met the exclusion criteria (see Figure 1); 63 families and patients were informed about the study, and 59 were interested in participating, consented to the study, and were randomized to condition (intervention group n=30 patients and their families; control group n=29). All patients randomized to condition completed the baseline assessment. The study was approved by the hospital’s US FWA IRB (#00011251).
Fig. 1.
Patient recruitment, enrollment, and retention.
2.2 Control and intervention conditions
The control group received services as usual, which consisted of psychotropic medication selected and monitored by the patient’s hospital physician. The intervention group received the Family Schizophrenia Psychoeducation Program (FSPP), as well as medication. The FSPP was developed based on review and adaptation of similar programs used in other countries (e.g., Kung et al., 2012) followed by several months of pilot testing and modification in the hospital. One of the primary cultural modifications involves the program, throughout its course, strongly emphasizing the potential capabilities of the family member with schizophrenia, and the dangers of “spoiling” the family member. In Viet Nam, out of their concern and desire to be supportive, families often reduce the responsibilities and expectations for a family member with a disability, including schizophrenia. The consequence is, of course, that the family member does not develop their capabilities, their life becomes restricted, and their quality of life actually diminishes.
The program consists of three sessions of approximately 1.5 hours duration that take place in the hospital. Sessions include both the family members staying with the patient as well as the patient. (In Viet Nam, a family member(s) typically stays with in-patients receiving acute care at or near the hospital during the patient’s stay.) Sessions are interactive, with the hospital staff providing information but also facilitating discussion with the family and patient. Because of the complexity of scheduling multiple families, the program is provided to individual families rather than in a group. Sessions were conducted by a hospital psychiatrist, two psychologists and two nurses. Sessions typically are provided over a period of a week and a half.
Session 1: The first session discusses schizophrenia as a medical condition, what it is and what its symptoms are, what is known about the medical / biological causes of schizophrenia, and what treatments for schizophrenia are, and the prognosis including the potential for the patient to have a full life with their own family, etc. if successfully treated. Because stigma reduction may be one way to increase patient quality of life (Sibidz et al., 2010), this session also discusses stigma, its causes, and how stigma is inaccurate and harmful.
Session 2: The second session discusses how the family can be supportive of the patient, including the importance of not “spoiling” him or her and of having reasonable expectations for the patient, the kinds of skills that are useful for this, the difficulties in living with a patient with schizophrenia, and how to resolve these difficulties. It also discusses problem-solving challenges and solutions that arise in families with a member with schizophrenia.
Session 3: The third session focuses on how to help the patient reintegrate into the community and have a “normal life”. It discusses realistic social goals for the patient (that they can have friends, a job, etc.), and the challenges and skills useful in achieving these goals.
FSPP training and supervision
Hospital staff providing the program received 20 hours of training over eight days, provided by TNT and LTT. The training consisted of (a) initial review of the purpose, goals and structure of the program, (b) discussion of the program, led by the trainers, (c) role-play practice with the trainers and trainees, (d) practice with volunteer patients and their families. In this project staff met weekly for supervision, which lasted about 1 hour, provided by TNT.
2.3 Outcome measures and procedures
Data were collected at two time points. The first (T1) was in the hospital as soon as possible after study consent was obtained (prior to intervention group participants beginning FSPP), and the second (T2) was six months later, in the family’s home. All scales were scored as the mean of the component items for ease in interpretability, so that mean scores would be on the same scale as the items.
Quality of Life (QOL) was assessed using the Quality of Life Enjoyment and Satisfaction Questionnaire (Endicott et al., 1993). It assesses patients’ QOL in five areas: general activities, physical activities, emotional functioning, recreational activities, and social relationships. It has 59 items rated on a 1 to 5 Likert scale, with higher scores indicating higher QOL. In the present study the total score was used. The timeframe for the measure at T1 was for QOL the one week prior to the patient’s hospitalization and for T2 for the one week prior to the six-month assessment.
Stigma towards schizophrenia was assessed using the Stigma Towards Schizophrenia scale developed for Vietnamese patients based on other international stigma scales (Corrigan, 2013; Saldivia et al., 2014). This scale has 9 items (e.g., People with schizophrenia cannot be successful in anything in life) rated on a scale ranging from 0 to 3, with higher scores indicating higher levels of agreement with stigma attitudes towards schizophrenia. This scale was rated by the patient and the family member taking care of the patient at the hospital.
Medication non-compliance was assessed using Dunja et al.’s (2007) medication compliance inventory, adapted for Viet Nam. This scale has 8 items (e.g., How often do you stop taking your medication because of side-effects) rated on a 0 to 2 frequency scale, with higher scores indicating higher non-compliance. This measure was collected at T2 but not at T1 because at that point the patient was still in the hospital receiving medication, supported by the hospital.
Consumer satisfaction was assessed using a scale developed for this study. This scale has 4 items (e.g., What was the quality of the treatment and support services at the hospital) rated on a 1 to 4 scale, with a higher scores indicating higher satisfaction. This measure was collected at T2 but not T1 because at that point the hospital services had not been completed.
2.4 Statistical analysis
One-way analysis of variance were used to assess group differences on baseline levels of outcome variables (e.g., stigma) and continuous demographic variables via SAS 9.5 Proc Glm. A logistic model was used to assess group differences on gender via SAS Proc Glimmix. Analyses of covariance via SAS Proc Glm were used for outcome analyses, with T2 scores as the dependent variable, and T1 scores and variables upon which the groups differed at baseline as covariates (however, there were no T1 differences; see Results below). Because there were no T1 baseline scores for consumer satisfaction or medication compliance (since the T1 assessment occurred during the hospitalization before treatment was completed), analysis of variance without baseline scores were used to analyze these variables.
3. Results
3.1 Baseline analyses
The groups differed significantly on none of the demographic or outcome variables at baseline (all p>.10); therefore, none of these variables were included as covariates. We also compared participants with T2 data to those without T2 data (i.e., participants who had attrited) on the baseline variables. One of the 18 analyses, family-reported stigma, was significant (F[1,57] = 9.40, p<.005), with families missing T2 data reporting higher levels of stigma than families not missing T2 data (1.09 vs. .60, respectively).
3.2 Outcome analyses
Table 2 reports results of the outcome analyses. The effect of treatment was significant for patient-report QOL and marginally significant for family-report QOL; the other five analyses all were significant, with all results favoring the treatment group. Effect sizes (see Table 2) were moderate (R2=.08, family-reported QOL) to large (R2=.22, patient-reported consumer satisfaction). Also, because we hypothesize that reduction in stigma is one of the mechanisms through which the FSPP increases patient quality of life, we conducted a second set of ANCOVA assessing QOL, controlling for T2 stigma (for patient-report QOL, T2 patient-report stigma; for family-report QOL, T2 family-report stigma). In both of these analyses, the effect of treatment became non-significant (both p>.10) with the addition of these terms in the model.
Table 2.
Mean (and SD) for dependent variables at T1 and T2
| Dependent variable | Group | T1 | T2 | F(df), R2,p |
|---|---|---|---|---|
| Patient-report QOL (range: 1-5) |
FSPP Group C Group |
3.69 (0.61) 3.49 (0.53) p > .19 |
3.95 (0.60) 3.55 (0.65) |
F(1,46)=4.32*, R2=.09 |
| Family-report QOL (range: 1- 5) |
FSPP Group C Group |
3.04 (0.55) 3.05 (0.41) p > .97 |
3.81 (0.45) 3.53 (0.67) |
F(1,44)=3.87+, R2=.08 |
| Patient-report stigma (range: 0-3) |
FSPP Group C Group |
0.89 (0.53) 0.85 (0.48) p > .76 |
0.39 (0.35) 0.71 (0.54) |
F(1,45)=6.67*, R2=.13 |
| Family-report stigma (range: 0-3) |
FSPP Group C Group |
0.63 (0.45) 0.73 (0.54) p > .45 |
0.24 (0.26) 0.53 (0.44) |
F(1,44)=9.36**, R2=.18 |
| Medication non-compliance (range: 0-2) |
FSPP Group C Group |
0.29 (0.24) 0.59 (0.50) |
F(1,47)=7.65**, R2=.14 | |
| Patient-report consumer satisfaction (range: 1-4) |
FSPP Group C Group |
3.60 (0.37) 3.14 (0.52) |
F(1,46)=12.82***, R2=.22 | |
| Family-report consumer satisfaction (range: 1-4) |
FSPP Group C Group |
3.72 (0.40) 3.42 (0.46) |
F(1,45)=5.91*, R2=.12 |
FSPP Group = Psychoeducation group. C Group = Control group. QOL = Quality of Life measure.
p < 0.10;
p < 0.05;
p < 0.01;
p < 0.001.
No T1 differences were significant, all p>.10.
3.3 Patient comments on the utility of the program
We also asked participants to comment on what they found most helpful or useful about the FSPP. The most frequent comments centered around the importance of having realistic expectations for the family member with schizophrenia (e.g., “Before this program, I thought that because my son was ill, he should rest and not work in order to reduce stress that was making his illness worse. After the program, our family realized that he needs to work in a way that is compatible with his actual strength, and that this will help him become healthier”). Participants also commented on the importance of understanding the biological causes of schizophrenia (e.g., “We learned that this illness schizophrenia is not due to ghosts or a bad family or because our child is lazy but because of medical biological causes like other illnesses. So now we know what we can do to help”). Families also commented on having better understanding of stigma, and the difficulties of more general stigma in society (e.g., “We now see that schizophrenia is an illness and not something that is our daughter’s or family’s fault about which we should be ashamed. We also understand that the rest of the community does not always understand this and that we have to be strong for our daughter”).
4. Discussion
The goal of the Family Schizophrenia Psychoeducation Program (FSPP) at the Da Nang Psychiatric Hospital is to increase patient quality of life, by providing families with: (1) accurate information about schizophrenia as a medical disorder, (2) information about realistic expectations about what an individual with schizophrenia can do, and (3) skills to support the member with schizophrenia have as normal a life as possible. As part of these goals, the program seeks to reduce stigma towards schizophrenia, to increase patient quality of life.
At the baseline assessment (T1) there were no differences between the groups on any of the demographic and outcome variables. Six months later, participants in the FSPP showed significantly greater improvement than the control group on 6 of 7 outcome variables, and a marginally significant effect on the 7th. Effect sizes were moderate to large, ranging from R 2=.08 (family-report of patient QOL) to R2=.22 (patient-report of consumer satisfaction.
Our primary outcome was the patient’s quality of life (QOL). Patient-report QOL showed a significant treatment effect, and family-report showed a marginally significant effect, both favoring the FSPP group. One possible explanation why the effect of the FSSP on patient-report QOL was significant but for family-report QOL only marginally significant is that the apparent FSSP effects on family-report QOL may have been reduced due to limitations in the family’s understanding or awareness of the patient’s QOL. In support of this possibility, a variety of research suggests that families tend to under-estimate the quality of life of family members who are medical patients (e.g., Schulz et al., 2013; Tang, 2006). Thus, apparent program effects may have been reduced for family-report QOL due to such effects.
Because it can have a major impact on QOL (Collins et al., 2012), a primary target of the FSPP is stigma. We found that the FSPP significantly reduced both patient- and family-report stigma; in fact, the effect of the program on stigma was larger than on quality of life (i.e., R2=.13, .18, vs. .09, .08). Further, we found that the effects of the FSSP on QOL became non-significant when we controlled for T2 stigma, suggesting that stigma may have been one of the mediators of FSSP effects. We also found that FSPP participants reported better medication compliance than control participants, of obvious importance since medication compliance is one of the most important predictors of successful treatment of schizophrenia and improved quality of life (Dunja et al., 2007). Finally, participants in the FSPP group reported higher consumer satisfaction compared to participants in the control group. Although it does not directly relate to quality of life or patient functioning, consumer satisfaction is important because it may be related to increased treatment compliance in the present and in the future, and the patient may return more quickly for services if there is a relapse (e.g., Sterk et al., 2013). Positive attitudes towards the mental health center also may serve as constructive advertising for other families considering seeking mental health services from the center.
There are several limitations of the study that should be considered. First, the sample size was relatively small, and the study was implemented in only one site. The sample size was, however, large enough to produce statistically significant effects, but it still will be important in future research to include multiple sites and a larger sample to increase the generalizability of findings. A second limitation is that although as often happens in this region of the world (e.g., Dang et al., 2015; Weiss et al., 2014) the study participation rate was high (>93%), loss to attrition in the study (19%) was higher than ideal, although only 1 of 18 tests comparing dropouts to non-dropouts at T1 was significant, which is at about the chance level (.05). Third, this study intentionally focused on individuals with relatively recent onset schizophrenia; thus the applicability of results to individuals with more long-term schizophrenia is unclear. This does suggest that at least at present, it will be important to use this program relatively early in the course of the disease, to increase the likelihood that the positive effects of program found here will be replicated with new samples. It also suggests that in the future it will be worthwhile to modify and evaluate a version of the program for individuals with more long-term schizophrenia. Finally, although there is some empirical evidence (e.g., Ran et al., 2015) and our six month outcome timeframe suggests that FSSP effects may be durable, it will be useful in future research to include a longer outcome timeframe.
In conclusion, similar to studies in high income countries (e.g., Kung et al., 2012), we found that our Family Schizophrenia Psychoeducation Program adapted for Viet Nam appears to reduce stigma, and improve quality of life and medication compliance of Vietnamese patients with schizophrenia. It involves relatively few resources and it may be useful for it or equivalent programs to be implemented in other hospitals across Viet Nam, and potentially in other similar Asian countries, to improve the lives of patients with schizophrenia.
Table 1.
Baseline demographic characteristic of randomized participants
| Psychoeducation group | Control group | p1 | |
|---|---|---|---|
| Male (%) | 48.6 % | 51.4 % | .67 |
| Mean age in years (SD) | 24.87 (5.11) | 23.69 (4.37) | .35 |
| Education (High school graduate) (%) | 26.7 % | 27.6 % | .94 |
| Mean number of hospitalizations (SD) | 1.53 (0.78) | 1.72 (0.65) | .31 |
| Mean years of schizophrenia (SD) | 1.58 (1.13) | 1.99 (1.06) | .16 |
p for group difference between Psychoeducation and Control groups.
HIGHLIGHTS.
Few studies of schizophrenia psychoeducation have been conducted in Southeast Asia.
This study assessed the Family Schizophrenia Psychoeducation Program in Vietnam.
Effects were found on quality of life, stigma, medication compliance, consumer satisfaction.
Effect sizes were moderate to large.
It may be useful for such programs to be implemented in Viet Nam and other Asian countries.
Acknowledgements
All authors had full access to all of data and take responsibility for data integrity and accuracy of data analysis. The authors gratefully thank the participating patients and families for their involvement in the study, and the funding sources for their support.
Funding
This study was funded by the U.S. National Institutes of Health Fogarty International Center, NIH Office of the Director, and National Institute of Mental Health (R25 TW009337; D43TW009089).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
TNN & LTT adapted and finalized the Psychoeducation Program. BW was responsible for the research study design. TNN was responsible for research implementation, with support from BW and LTT. BW was responsible for data analysis. TNN was responsible for production of the initial Vietnamese version of the manuscript, with support from TNN & BW. TNN & BW were responsible for production of this English version of the manuscript, with BW having final responsibility. All authors reviewed and approved the final version of this manuscript.
Conflict of interest
All authors declare they have no conflict of interest.
References
- Collins RL, Wong EC, Cerully JL, Schultz D, Eberhart NK. Interventions to Reduce Mental Health Stigma and Discrimination. The RAND Corporation; Santa Monica, CA, USA: 2012. [PMC free article] [PubMed] [Google Scholar]
- Corrigon P. Toolkit for Evaluating Programs Meant to Erase the Stigma of Mental Illness. Illinois Institute of Technology; Chicago, IL, USA: 2013. [Google Scholar]
- Dang MH, Weiss B, Trung LT. Mental health functioning and functional impairment among a nationally representative sample of Vietnamese children. Social Psychiatry and Psychiatric Epidemiology. 2015;51:39–47. doi: 10.1007/s00127-015-1114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunja D, Pozgain I, Filakovic P. Psychoeducation and compliance in the treatment of patients with schizophrenia. Coll. Antropol. 2007;31:1111–1115. [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacol Bull. 1993;29:321–326. [PubMed] [Google Scholar]
- Gaebel W. Schizophrenia: Current Science and Clinical Practice. Wiley-Blackwell; Hoboken, New Jersey, USA: 2011. [Google Scholar]
- Galuppi A, Turola MC, Mazzoni P. Quality of life and personal and social functioning: New targets in schizophrenia treatment. In: Sumiyoshi T, editor. Schizophrenia Research: Recent Advances. Nova Science Publishers; Hauppauge, NY, USA: 2012. pp. 45–59. [Google Scholar]
- Jablensky A. Epidemiology of schizophrenia: The global burden of disease and disability. Eur. Arch. Psychiatry Clin. Neurosci. 2000;250:274–285. doi: 10.1007/s004060070002. [DOI] [PubMed] [Google Scholar]
- Kulhara P, Chakrabarti S, Avasthi A, Sharma A, Sharma S. Psychoeducational intervention for caregivers of Indian patients with schizophrenia: A randomized-controlled trial. Acta Psychiatrica Scandinavica. 2009;119(6):472–483. doi: 10.1111/j.1600-0447.2008.01304.x. [DOI] [PubMed] [Google Scholar]
- Kung WW, Tseng Y, Wang Y, Hsu P, Chen D. Pilot study of ethnically sensitive family psychoeducation for Chinese American patients with schizophrenia. Social Work in Mental Health. 2012;10:384–408. [Google Scholar]
- Ran MS, Chan CLW, Ng SM, Guo LT, Xiang MZ. The effectiveness of psychoeducational family intervention for patients with schizophrenia in a 14-year follow-up study in a Chinese rural area. Psychol Med. 2015;45(10):2197–2204. doi: 10.1017/S0033291715000197. [DOI] [PubMed] [Google Scholar]
- Rummel-Kluge C, Schuster T, Peters S, Kissling W. Partial compliance with antipsychotic medication in common in patients with schizophrenia. Aust N Z J Psychiatry. 2008;42:382–388. doi: 10.1080/00048670801961107. [DOI] [PubMed] [Google Scholar]
- Saldivia S, Runte-Geidel A, Grandón P, Torres-González F, Xavier M, Antonioli C, King M. The Maristán stigma scale: A standardized international measure of the stigma of schizophrenia and other psychoses. BMC Psychiatry. 2014:14. doi: 10.1186/1471-244X-14-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Cook TB, Beach SR, Lingler JH, Martire LM, Monin JK, Czaja SJ. Magnitude and causes of bias among family caregivers rating Alzheimer disease patients. The American Journal of Geriatric Psychiatry. 2013;21:14–25. doi: 10.1016/j.jagp.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibitz I, Amering M, Unger A, Seyringer ME, Bachmann A, Schrank B, et al. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. European Psychiatry. 2011;26:28–33. doi: 10.1016/j.eurpsy.2010.08.010. [DOI] [PubMed] [Google Scholar]
- Sterk B, van Rossum IW, Muis M, de Haan L. Priorities, satisfaction and treatment goals in psychosis patients: An online consumer’s survey. Pharmacopsychiatry. 2013;46:88–93. doi: 10.1055/s-0032-1327732. [DOI] [PubMed] [Google Scholar]
- Tang ST. Concordance of quality-of-life assessments between terminally ill cancer patients and their primary family caregivers in Taiwan. Cancer Nurs. 2006;29:49–57. doi: 10.1097/00002820-200601000-00009. [DOI] [PubMed] [Google Scholar]
- Weiss B, Dang M, Trung L, Nguyen MC, Thuy NTH, Pollack A. A nationally-representative epidemiological and risk factor assessment of child mental health in Vietnam. International Perspectives in Psychology: Research, Practice, Consultation. 2014;3:139–153. doi: 10.1037/ipp0000016. [DOI] [PMC free article] [PubMed] [Google Scholar]