Abstract
Substantial data demonstrate that the early‐life environment, including in utero, plays a key role in later life disease. In particular, maternal stress during pregnancy has been linked to adverse behavioural and emotional outcomes in children. Data from human cohort studies and experimental animal models suggest that modulation of the developing epigenome in the foetus by maternal stress may contribute to the foetal programming of disease. Here, we summarise insights gained from recent studies that may advance our understanding of the role of the placenta in mediating the association between maternal mood disorders and offspring outcomes. First, the placenta provides a record of exposures during pregnancy, as indicated by changes in the placental trancriptome and epigenome. Second, prenatal maternal mood may alter placental function to adversely impact foetal and child development. Finally, we discuss the less well established but interesting possibility that altered placental function, more specifically changes in placental hormones, may adversely affect maternal mood and later maternal behaviour, which can also have consequence for offspring well‐being.
Keywords: maternal mood, prenatal stress, foetal programming, placenta, hormones
Introduction
Pregnancy can be a challenging time in a woman's life, during which she may experience many changes in her circumstances. Pregnancy can also be a time of vulnerability to perinatal mental illnesses, including depression, stress and postnatal psychosis 1. In the UK, it is estimated that maternal mood disorders, either prenatally or in the immediate period after birth, affect approximately one in five women, and is therefore one of the most common conditions of pregnancy. These disorders affect women of all ethnicities, nationalities and social strata 2. In addition to the distress that this causes women and their families, mental health disorders are one of the leading causes of death during pregnancy and the year after birth 1. Of equal concern is an additional consequence for her child's well‐being, with an increased risk of adverse behavioural and metabolic outcomes following exposure to maternal prenatal stress 3. Thus, a greater understanding of both the causes and the consequences of prenatal maternal stress and mood disorders is imperative.
Foetal programming by maternal stress
Prenatal stress at its broadest level includes major life event stress, catastrophic disasters, chronic stress, daily hassles, perceived stress or pregnancy‐specific anxiety along with related symptoms of depression or general anxiety during pregnancy 4. Both animal and human studies indicate that maternal prenatal stress is associated with an increased risk of adverse emotional, behavioural and cognitive outcomes in the offspring, a subject that has been reviewed extensively 5, 6. Several studies, including the large Avon Longitudinal Study of Parents and Children (ALSPAC) cohort, allow for multiple confounders, including prenatal paternal and postnatal maternal mood. The findings from such studies indicate that the increased risk for adverse outcomes in the offspring is programmed in utero by the maternal emotional state, in least in part 7. If the mother is in the top 15% of a normal population for prenatal symptoms of anxiety or depression, her child has double the risk of a probable mental disorder, raised from approximately 6–12% at the age of 13 years 7. However, it is clear that not all children are affected equally by exposure to maternal stress, and also the effects of prenatal stress on child development are inconsistent. Recent data suggest that this may partly be a result of a gene/environment interplay, including the interaction between prenatal maternal anxiety and the child with respect to the genes for brain‐derived neurotrophic factor (BDNF) 8 and catechol‐O‐methyltransferase (COMT) (O'Donnell and Glover, unpublished data), during the development of emotional and cognitive outcomes, respectively.
The role of the placenta in mediating foetal programming
Placental function is important both for optimal foetal growth and maternal health 9. The placenta is a transient organ of pregnancy that transports nutrients and oxygen to the growing foetus and removes waste products. Additionally, the placenta functions to mitigate the mother's immune response to her semi‐allogeneic foetus and manufactures large quantities of hormones that flood the maternal system to induce the adaptations required for a successful pregnancy 10. An optimally functioning placenta can provide protection to the foetus against some forms of prenatal adversity. For example, the placental enzyme 11β‐hydroxysteroid dehydrogenase 2 (HSD11B2) regulates foetal exposure to maternal cortisol by converting it to inactive cortisone. Thus, the placenta is able to partially protect the foetus against elevated maternal cortisol levels. However, there is evidence that placental function may be affected by prenatal stress 11, 12, 13, 14, 15. Both endogenous and synthetic glucocorticoids have been shown to impact a variety of placental functions, including vascularisation, apoptosis and nutrient transport, in a range of animal models and human studies 16, 17, 18, 19, 20. Moreover, there is evidence that other maternal factors, such as catecholamines 21, may transfer the effects of maternal stress to the foetus by altering placental function. Consequently, suboptimal placental function induced by the maternal state may contribute to altered and, in our environment, poorer outcomes for children 22. Prenatal anxiety is associated with both lower expression and activity of placental HSD11B2 14, potentially mitigating the protective role that this enzyme usually plays, and theoretically exposing the foetus to higher cortisol levels. Foetal glucocorticoid exposure is also regulated by the placental glucocorticoid (GR; NR3C1) and mineralocorticoid (MR; NR3C2) receptors. Placental NR3C1 and NR3C2 expression is higher among depressed compared to nondepressed new mothers, providing another mechanism for the programming of adverse offspring outcomes 15. Alterations in the expression of genes for placental corticotrophin‐releasing hormone [pCRH; which stimulates the production of cortisol via the hypothalamic‐pituitary‐adrenal (HPA) axis], monoamine oxidase A (MAOA; which metabolises serotonin into 5‐hydroxyindoleacetic acid) and placental serotonin transporter (SLC6A4; which transports the neurotransmitter serotonin) and P‐glycoprotein have also been linked to prenatal stress 11, 23, 24, 25. Interestingly, very recent evidence suggests that the associations between prenatal maternal mood and placental gene expression may be different in Caucasian and non‐Caucasian populations (Capron and Glover, unpublished data). Thus, alterations in the expression of a number of genes in the placenta may mediate aspects of foetal programming associated with prenatal stress (Fig. 1); however, these findings may have ethnic specificities.
Figure 1.
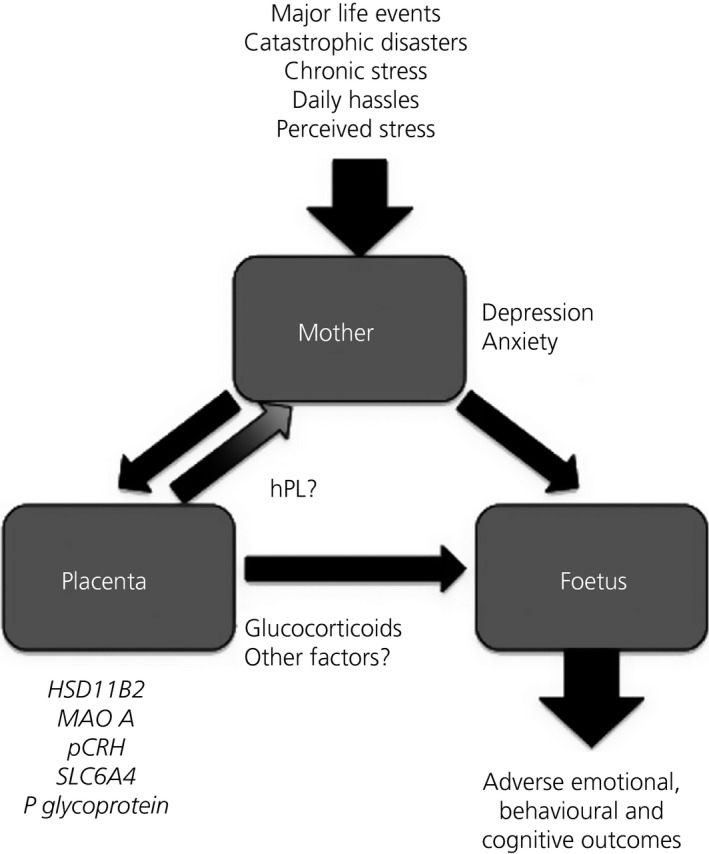
The role of the placenta in prenatal stress. Prenatal stress can influence the placental and foetal transcriptomes and epigenomes, which may contribute to adverse outcomes for children. Dysfunctional placental signalling may also influence maternal mood during pregnancy and maternal behaviour in the postnatal period, further contributing to adverse outcomes.
Maternal stress and epigenetic changes in the placenta
Although it is clear that there are changes in the expression of genes in the placenta in relation to prenatal stress exposure, the mechanisms underpinning these changes are unclear. One possibility is the epigenetic deregulation of gene expression. Epigenetics describes the marks or tags that are added or removed from DNA sequence and the histones that regulate gene expression in a manner heritable through cell division. Such marks may be altered by exposure to stress during prenatal development, a period when the epigenome is rapidly changing 26. Animal research demonstrates that maternal stress can induce epigenetic changes in the placenta. DNA methylation changes have been reported in the promoter region of Hsd11B2 12 and altered chromatin methylation has been linked to the gene for O‐linked‐N‐acetylglucosamine transferase (Ogt) 27. Such alterations may be mediated by sex‐specific changes in the placental epigenetic machinery 28. In humans, maternal anxiety has been linked to greater placental methylation of HSD11B2, whereas maternal depression (but not anxiety) has been associated with increased placental methylation of NR3C1 29. Recent research with mothers in a conflict‐ridden region of the Democratic Republic of Congo has reported that higher levels of war trauma and chronic stress were associated with DNA methylation levels in multiple placental genes involved in HPA axis regulation, including CRH, CRHBP, NR3C1 and FKBP5 30. Stress‐linked variation in DNA methylation was observed in placental tissue, as well as maternal and umbilical cord blood. However, similar to Jensen Pena et al. (12), the effects at individual CpG sites differed between tissues. The majority of CpG sites identified were situated in transcription factor binding regions, and several were associated with offspring birth weight 30. Similar effects of maternal war trauma and chronic stress have been observed with placental BDNF methylation 31. Considering that many affected CpG sites bind transcription factors, as well as the associations with mRNA levels or offspring birth weight, this suggests that stress‐linked variation in placental methylation may have functional consequences for offspring outcomes.
Maternal stress and epigenetic changes in offspring
Experimental animal models have demonstrated that early‐life stress can leave a mark on the offspring epigenome, with alterations reported in offspring exposed to prenatal stress 28, maternal separation 32 and low levels of maternal postnatal care 33. In humans, variation in CpG methylation in umbilical cord blood at NR3C1 has been associated with prenatal maternal anxiety 34 and depressive symptoms 29, 35. Also in cord blood, CpG methylation at both NR3C1 and CRH is associated with maternal experiences of war trauma and chronic stress 30. The NR3C1 and CRH CpG sites identified in these studies are the same as those linked to pre‐eclampsia in cord blood 36 or prenatal exposure to inter‐partner violence in offspring venous blood 37. In animal models, methylation at the NR3C1 sites affects NGFI‐A binding 38. These may be sites for which DNA methylation is particularly sensitive to several stress‐linked phenotypes. Prenatal maternal chronic stress and war trauma is associated with BDNF methylation in cord blood at birth 31 and prenatal depression has been associated with DNA methylation at the BDNF promoter region in buccal cells at 2 months of age 39. BDNF plays an essential role in brain development and has been linked to psychiatric risk 40, thus suggesting that BDNF DNA methylation may be an important target for future investigation. Maternal cortisol and self‐reported depressive and anxiety symptoms have also been associated with altered DNA methylation of the imprinted genes IGF2 and GNASXL 41. However, it is important to note that, across both rodent and human studies, there are tissue specific associations of prenatal stress and DNA methylation. These differences may reflect the different physiological functions of each tissue or differences in the epigenetic status of certain tissues at the time of exposure. Nonetheless, it is clear that the maternal stress can impact both the placental and the foetal epigenomes to alter gene expression.
The programming of maternal mood by the placenta
Although considerable data from both animal models and human studies support changes in the placenta and foetus in response to maternal stress, which may then contribute to the programming of neurodevelopmental changes in offspring, few studies have explored a placental origin for maternal mood disorders. Pituitary prolactin and the placental lactogens are a group of evolutionarily and functionally‐related hormones important in pregnancy. Human placental lactogen (hPL) is produced by the placental syncytiotrophoblast and secreted into the maternal circulation, replacing prolactin as the main lactogenic hormone during pregnancy 42. Numerous studies highlight a functional role for these hormones and their shared receptor (prolactin receptor; PRLR) in the onset of maternal behaviours in rodents and, in the case of prolactin and PRLR, also maternal neurogenesis 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53. In humans, these hormones may contribute to suppression of anxiety‐related behaviours during pregnancy 54. Decreased serum prolactin levels have been reported in human mothers with postnatal depression 55, 56, whereas increased levels of prolactin have been associated with low anxiety scores during pregnancy 57. Impaired hPL production has also been associated with adverse infant outcomes such as foetal growth restriction 58, 59. Thus, the altered placental expression of the genes for placental lactogen could contribute to both maternal mood disorders and adverse outcomes (Fig. 1).
Imprinted genes, foetal programming and maternal mood disorders
Imprinted genes are expressed from one parental allele through epigenetic marking in the germline 60. Imprinted genes are known to regulate foetal growth, placental development, adult behaviour and metabolism 61. These multifunctional roles and the flexibility of epigenetic marks have led to the suggestion that imprinted genes may contribute to the foetal programming of adverse outcomes 62. Numerous studies have reported the aberrant expression of imprinted genes in the placenta in relation to foetal growth restriction and low birth weight 63. Altered expression of imprinted genes in the placenta has also been linked to infant neurobehavioral developmental outcomes 64, 65. Recently, imprinted genes have been highlighted as key regulators of the endocrine lineages that express placental hormones in rodents 66. This newly defined function suggests that the aberrant expression of imprinted genes in the placenta could contribute to the mispriming of maternal behaviour, at least in rodents, by modulating exposure of the maternal brain to key placental hormones such as the placental lactogens. If the function of imprinted genes in regulating the endocrine lineage was conserved across species, aberrant imprinting could help to explain the co‐occurrence of low birth weight with prenatal mood disorders, which has been reported in a number of studies 67, 68, 69, 70, 71, 72, 73. Epigenetic changes in cord blood DNA at imprinted loci have been associated with depressed maternal mood during pregnancy 74 and with maternal stress 41, 75. One study reported changes in DNA methylation in both cord blood DNA and placental DNA at an imprinted locus 76. Although it is generally presumed that such changes occur in response to prenatal adversity with the focus primarily concerning offspring outcomes, it is possible that such changes contribute to altered maternal mood by changing the endocrine function of the placenta (Fig. 1). Consistent with this hypothesis, recent data have identified a significant association between both symptoms of prenatal depression and clinically diagnosed depression with placental expression of both an imprinted gene and placental lactogen, a hormone predicted to be regulated by this gene 77. Determining the cause and effect relationships in human studies of pregnancy is challenging. However, very recent work utilising a novel rodent model suggests that imprinted genes in the placenta can influence both the maternal neural transcriptome during pregnancy and maternal behaviour in the early postnatal period (Creeth et al., in preparation), comprising data that support a causal relationship.
Summary and outlook
In summary, the placenta plays a key role in supporting a successful healthy pregnancy. The placenta can provide a record of prenatal adversity, including maternal stress. Changes in placental function, potentially driven by epigenetic processes, may impact neurodevelopmental outcomes for children and both mental and metabolic health into adulthood. Importantly, placental dysfunction may also contribute to maternal mood disorders, either during pregnancy and/or in the immediate postnatal period, by exposing the mother to abnormal levels of placental hormones. At present, most women experiencing heightened levels of prenatal depression, stress and anxiety are undetected and untreated. The potential clinical implications of maternal prenatal mood on foetal and child neurodevelopment are substantial. The provision of better emotional care for all pregnant women and enhanced identification and support for women at particularly high risk of maternal mood disorders will help not only them, but also their children, and potentially subsequent generations.
References
- 1. Jones I, Chandra PS, Dazzan P, Howard LM. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post‐partum period. Lancet 2014; 384: 1789–1799. [DOI] [PubMed] [Google Scholar]
- 2. Atif N, Lovell K, Rahman A. Maternal mental health: the missing ‘m’ in the global maternal and child health agenda. Semin Perinatol 2015; 39: 345–352. [DOI] [PubMed] [Google Scholar]
- 3. Glover V, O'Donnell K, O'Connor TG, Ramchandani P, Capron L. Prenatal anxiety and depression, fetal programming and placental function. Psychoneuroendocrinology 2015; 61: 3–4.26383279 [Google Scholar]
- 4. Glover V. Prenatal stress and its effects on the fetus and the child: possible underlying biological mechanisms. Adv Neurobiol 2015; 10: 269–283. [DOI] [PubMed] [Google Scholar]
- 5. Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev 2005; 29: 237–258. [DOI] [PubMed] [Google Scholar]
- 6. Talge NM, Neal C, Glover V; Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health . Antenatal maternal stress and long‐term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry 2007; 48: 245–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Donnell KJ, Glover V, Barker ED, O'Connor TG. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol 2014; 26: 393–403. [DOI] [PubMed] [Google Scholar]
- 8. O'Donnell KJ, Glover V, Holbrook JD, O'Connor TG. Maternal prenatal anxiety and child brain‐derived neurotrophic factor (BDNF) genotype: effects on internalizing symptoms from 4 to 15 years of age. Dev Psychopathol 2014; 26: 1255–1266. [DOI] [PubMed] [Google Scholar]
- 9. John R, Hemberger M. A placenta for life. Reprod Biomed Online 2012; 25: 5–11. [DOI] [PubMed] [Google Scholar]
- 10. Glynn LM, Sandman CA. Prenatal origins of neurological development: a critical period for fetus and mother. Curr Dir Psychol Sci 2011; 20: 384–389. [Google Scholar]
- 11. Blakeley PM, Capron LE, Jensen AB, O'Donnell KJ, Glover V. Maternal prenatal symptoms of depression and down regulation of placental monoamine oxidase A expression. J Psychosom Res 2013; 75: 341–345. [DOI] [PubMed] [Google Scholar]
- 12. Jensen Pena C, Monk C, Champagne FA. Epigenetic effects of prenatal stress on 11beta‐hydroxysteroid dehydrogenase‐2 in the placenta and fetal brain. PLoS ONE 2012; 7: e39791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mairesse J, Lesage J, Breton C, Breant B, Hahn T, Darnaudery M, Dickson SL, Seckl J, Blondeau B, Vieau D, Maccari S, Viltart O. Maternal stress alters endocrine function of the feto‐placental unit in rats. Am J Physiol Endocrinol Metab 2007; 292: E1526–E1533. [DOI] [PubMed] [Google Scholar]
- 14. O'Donnell KJ, Bugge Jensen A, Freeman L, Khalife N, O'Connor TG, Glover V. Maternal prenatal anxiety and downregulation of placental 11beta‐HSD2. Psychoneuroendocrinology, 2012; 37: 818–826. [DOI] [PubMed] [Google Scholar]
- 15. Reynolds RM, Pesonen AK, O'Reilly JR, Tuovinen S, Lahti M, Kajantie E, Villa PM, Laivuori H, Hamalainen E, Seckl JR, Raikkonen K. Maternal depressive symptoms throughout pregnancy are associated with increased placental glucocorticoid sensitivity. Psychol Med 2015; 45: 2023–2030. [DOI] [PubMed] [Google Scholar]
- 16. Audette MC, Challis JRG, Jones RL, Sibley CP, Matthews SG. Synthetic glucocorticoid reduces human placental system a transport in women treated with antenatal therapy. J Clin Endocrinol Metabol 2014; 99: E2226–E2233. [DOI] [PubMed] [Google Scholar]
- 17. Hewitt DP, Mark PJ, Waddell BJ. Glucocorticoids prevent the normal increase in placental vascular endothelial growth factor expression and placental vascularity during late pregnancy in the rat. Endocrinology 2006; 147: 5568–5574. [DOI] [PubMed] [Google Scholar]
- 18. Vaughan OR, Fisher HM, Dionelis KN, Jefferies EC, Higgins JS, Musial B, Sferruzzi‐Perri AN, Fowden AL. Corticosterone alters materno‐fetal glucose partitioning and insulin signalling in pregnant mice. J Physiol 2015; 593: 1307–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Waddell BJ, Hisheh S, Dharmarajan AM, Burton PJ. Apoptosis in rat placenta is zone‐dependent and stimulated by glucocorticoids. Biol Reprod 2000; 63: 1913–1917. [DOI] [PubMed] [Google Scholar]
- 20. Wyrwoll CS, Seckl JR, Holmes MC. Altered placental function of 11beta‐hydroxysteroid dehydrogenase 2 knockout mice. Endocrinology 2009; 150: 1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rakers F, Bischoff S, Schiffner R, Haase M, Rupprecht S, Kiehntopf M, Kuhn‐Velten WN, Schubert H, Witte OW, Nijland MJ, Nathanielsz PW, Schwab M. Role of catecholamines in maternal‐fetal stress transfer in sheep. Am J Obstet Gynecol 2015; 213: 684.e681‐689.. [DOI] [PubMed] [Google Scholar]
- 22. O'Donnell K, O'Connor TG, Glover V. Prenatal stress and neurodevelopment of the child: focus on the HPA axis and role of the placenta. Dev Neurosci 2009; 31: 285–292. [DOI] [PubMed] [Google Scholar]
- 23. Glynn LM, Davis EP, Sandman CA. New insights into the role of perinatal HPA‐axis dysregulation in postpartum depression. Neuropeptides 2013; 47: 363–370. [DOI] [PubMed] [Google Scholar]
- 24. Ponder KL, Salisbury A, McGonnigal B, Laliberte A, Lester B, Padbury JF. Maternal depression and anxiety are associated with altered gene expression in the human placenta without modification by antidepressant use: implications for fetal programming. Dev Psychobiol 2011; 53: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang T, Chen M, Yan Y‐E, Xiao F‐Q, Pan X‐L, Wang H. Growth retardation of fetal rats exposed to nicotine in utero: possible involvement of CYP1A1, CYP2E1, and P‐glycoprotein. Environ Toxicol 2009; 24: 33–42. [DOI] [PubMed] [Google Scholar]
- 26. Seckl JR, Holmes MC. Mechanisms of disease: glucocorticoids, their placental metabolism and fetal ‘programming’ of adult pathophysiology. Nat Clin Pract Endocrinol Metab 2007; 3: 479–488. [DOI] [PubMed] [Google Scholar]
- 27. Howerton CL, Morgan CP, Fischer DB, Bale TL. O‐GlcNAc transferase (OGT) as a placental biomarker of maternal stress and reprogramming of CNS gene transcription in development. Proc Natl Acad Sci USA 2013; 110: 5169–5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mueller BR, Bale TL. Sex‐specific programming of offspring emotionality after stress early in pregnancy. J Neurosci 2008; 28: 9055–9065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Conradt E, Lester BM, Appleton AA, Armstrong DA, Marsit CJ. The roles of DNA methylation of NR3C1 and 11beta‐HSD2 and exposure to maternal mood disorder in utero on newborn neurobehavior. Epigenetics 2013; 8: 1321–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kertes DA, Kamin H, Hughes DA, Rodney N, Bhatt SS, Mulligan CJ. Prenatal maternal stress predicts methylation of genes regulating the hypothalamic‐pituitary‐adrenocortical system in mothers and newborns in the Democratic Republic of Congo. Child Dev 2016; 87: 61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kertes DA, Bhatt SS, Kamin HS, Rodney NC, Hughes DA, Mulligan CJ. Prenatal maternal stress and BDNF methylation in newborns. Dev Psychobiol 2015; 57(1): S19. [Google Scholar]
- 32. Kundakovic M, Champagne FA. Early‐life experience, epigenetics, and the developing brain. Neuropsychopharmacology 2015; 40: 141–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Szyf M, Weaver IC, Champagne FA, Diorio J, Meaney MJ. Maternal programming of steroid receptor expression and phenotype through DNA methylation in the rat. Front Neuroendocrinol 2005; 26: 139–162. [DOI] [PubMed] [Google Scholar]
- 34. Hompes T, Izzi B, Gellens E, Morreels M, Fieuws S, Pexsters A, Schops G, Dom M, Van Bree R, Freson K, Verhaeghe J, Spitz B, Demyttenaere K, Glover V, Van den Bergh B, Allegaert K, Claes S. Investigating the influence of maternal cortisol and emotional state during pregnancy on the DNA methylation status of the glucocorticoid receptor gene (NR3C1) promoter region in cord blood. J Psychiatr Res 2013; 47: 880–891. [DOI] [PubMed] [Google Scholar]
- 35. Oberlander TF, Weinberg J, Papsdorf M, Grunau R, Misri S, Devlin AM. Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics 2008; 3: 97–106. [DOI] [PubMed] [Google Scholar]
- 36. Hogg K, Blair JD, McFadden DE, von Dadelszen P, Robinson WP. Early onset pre‐eclampsia is associated with altered DNA methylation of cortisol‐signalling and steroidogenic genes in the placenta. PLoS ONE 2013; 8: e62969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Radtke KM, Ruf M, Gunter HM, Dohrmann K, Schauer M, Meyer A, Elbert T. Transgenerational impact of intimate partner violence on methylation in the promoter of the glucocorticoid receptor. Transl Psychiatry 2011; 1: e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zhang TY, Labonte B, Wen XL, Turecki G, Meaney MJ. Epigenetic mechanisms for the early environmental regulation of hippocampal glucocorticoid receptor gene expression in rodents and humans. Neuropsychopharmacology 2013; 38: 111–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Braithwaite EC, Kundakovic M, Ramchandani PG, Murphy SE, Champagne FA. Maternal prenatal depressive symptoms predict infant NR3C1 1F and BDNF IV DNA methylation. Epigenetics 2015; 10: 408–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boulle F, van den Hove DL, Jakob SB, Rutten BP, Hamon M, van Os J, Lesch KP, Lanfumey L, Steinbusch HW, Kenis G. Epigenetic regulation of the BDNF gene: implications for psychiatric disorders. Mol Psychiatry 2012; 17: 584–596. [DOI] [PubMed] [Google Scholar]
- 41. Vangeel EB, Izzi B, Hompes T, Vansteelandt K, Lambrechts D, Freson K, Claes S. DNA methylation in imprinted genes IGF2 and GNASXL is associated with prenatal maternal stress. Genes Brain Behav 2015; 14: 573–582. [DOI] [PubMed] [Google Scholar]
- 42. Newbern D, Freemark M. Placental hormones and the control of maternal metabolism and fetal growth. Curr Opin Endocrinol Diabetes Obes 2011; 18: 409–416. [DOI] [PubMed] [Google Scholar]
- 43. Augustine RA, Grattan DR. Induction of central leptin resistance in hyperphagic pseudopregnant rats by chronic prolactin infusion. Endocrinology 2008; 149: 1049–1055. [DOI] [PubMed] [Google Scholar]
- 44. Trujillo ML, Spuch C, Carro E, Senaris R. Hyperphagia and central mechanisms for leptin resistance during pregnancy. Endocrinology 2011; 152: 1355–1365. [DOI] [PubMed] [Google Scholar]
- 45. Bridges RS, Freemark MS. Human placental lactogen infusions into the medial preoptic area stimulate maternal behavior in steroid‐primed, nulliparous female rats. Horm Behav 1995; 29: 216–226. [DOI] [PubMed] [Google Scholar]
- 46. Bridges RS, Robertson MC, Shiu RP, Sturgis JD, Henriquez BM, Mann PE. Central lactogenic regulation of maternal behavior in rats: steroid dependence, hormone specificity, and behavioral potencies of rat prolactin and rat placental lactogen I. Endocrinology 1997; 138: 756–763. [DOI] [PubMed] [Google Scholar]
- 47. Walker TL, Vukovic J, Koudijs MM, Blackmore DG, Mackay EW, Sykes AM, Overall RW, Hamlin AS, Bartlett PF. Prolactin stimulates precursor cells in the adult mouse hippocampus. PLoS ONE 2012; 7: e44371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rolls A, Schori H, London A, Schwartz M. Decrease in hippocampal neurogenesis during pregnancy: a link to immunity. Mol Psychiatry 2008; 13: 468–469. [DOI] [PubMed] [Google Scholar]
- 49. Lucas BK, Ormandy CJ, Binart N, Bridges RS, Kelly PA. Null mutation of the prolactin receptor gene produces a defect in maternal behavior. Endocrinology 1998; 139: 4102–4107. [DOI] [PubMed] [Google Scholar]
- 50. Moltz H, Lubin M, Leon M, Numan M. Hormonal induction of maternal behavior in the ovariectomized nulliparous rat. Physiol Behav 1970; 5: 1373–1377. [DOI] [PubMed] [Google Scholar]
- 51. Bridges RS, DiBiase R, Loundes DD, Doherty PC. Prolactin stimulation of maternal behavior in female rats. Science 1985; 227: 782–784. [DOI] [PubMed] [Google Scholar]
- 52. Shingo T, Gregg C, Enwere E, Fujikawa H, Hassam R, Geary C, Cross JC, Weiss S. Pregnancy‐stimulated neurogenesis in the adult female forebrain mediated by prolactin. Science 2003; 299: 117–120. [DOI] [PubMed] [Google Scholar]
- 53. Larsen CM, Grattan DR. Prolactin, neurogenesis, and maternal behaviors. Brain Behav Immun 2012; 26: 201–209. [DOI] [PubMed] [Google Scholar]
- 54. Torner L, Toschi N, Pohlinger A, Landgraf R, Neumann ID. Anxiolytic and anti‐stress effects of brain prolactin: improved efficacy of antisense targeting of the prolactin receptor by molecular modeling. J Neurosci 2001; 21: 3207–3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Abou‐Saleh MT, Ghubash R, Karim L, Krymski M, Bhai I. Hormonal aspects of postpartum depression. Psychoneuroendocrinology 1998; 23: 465–475. [DOI] [PubMed] [Google Scholar]
- 56. Groer MW, Morgan K. Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology 2007; 32: 133–139. [DOI] [PubMed] [Google Scholar]
- 57. Asher I, Kaplan B, Modai I, Neri A, Valevski A, Weizman A. Mood and hormonal changes during late pregnancy and puerperium. Clin Exp Obstet Gynecol 1995; 22: 321–325. [PubMed] [Google Scholar]
- 58. Dutton PJ, Warrander LK, Roberts SA, Bernatavicius G, Byrd LM, Gaze D, Kroll J, Jones RL, Sibley CP, Froen JF, Heazell AE. Predictors of poor perinatal outcome following maternal perception of reduced fetal movements–a prospective cohort study. PLoS ONE 2012; 7: e39784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Roh CR, Budhraja V, Kim HS, Nelson DM, Sadovsky Y. Microarray‐based identification of differentially expressed genes in hypoxic term human trophoblasts and in placental villi of pregnancies with growth restricted fetuses. Placenta 2005; 26: 319–328. [DOI] [PubMed] [Google Scholar]
- 60. Surani MA. Imprinting and the initiation of gene silencing in the germ line. Cell 1998; 93: 309–312. [DOI] [PubMed] [Google Scholar]
- 61. Peters J. The role of genomic imprinting in biology and disease: an expanding view. Nat Rev Genet 2014; 15: 517–530. [DOI] [PubMed] [Google Scholar]
- 62. Keverne EB. Epigenetically regulated imprinted genes and foetal programming. Neurotox Res 2010; 18: 386–392. [DOI] [PubMed] [Google Scholar]
- 63. Moore GE, Ishida M, Demetriou C, Al‐Olabi L, Leon LJ, Thomas AC, Abu‐Amero S, Frost JM, Stafford JL, Chaoqun Y, Duncan AJ, Baigel R, Brimioulle M, Iglesias‐Platas I, Apostolidou S, Aggarwal R, Whittaker JC, Syngelaki A, Nicolaides KH, Regan L, Monk D, Stanier P. The role and interaction of imprinted genes in human fetal growth. Philos Trans R Soc Lond B Biol Sci 2015; 370: 20140074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Marsit CJ, Lambertini L, Maccani MA, Koestler DC, Houseman EA, Padbury JF, Lester BM, Chen J. Placenta‐imprinted gene expression association of infant neurobehavior. J Pediatr 2012; 160: 854–860 e852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Green BB, Kappil M, Lambertini L, Armstrong DA, Guerin DJ, Sharp AJ, Lester BM, Chen J, Marsit CJ. Expression of imprinted genes in placenta is associated with infant neurobehavioral development. Epigenetics 2015; 10: 834–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. John RM. Epigenetic regulation of placental endocrine lineages and complications of pregnancy. Biochem Soc Trans 2013; 41: 701–709. [DOI] [PubMed] [Google Scholar]
- 67. Berkowitz GS, Wolff MS, Janevic TM, Holzman IR, Yehuda R, Landrigan PJ. The World Trade Center disaster and intrauterine growth restriction. JAMA 2003; 290: 595–596. [DOI] [PubMed] [Google Scholar]
- 68. Henrichs J, Schenk JJ, Roza SJ, van den Berg MP, Schmidt HG, Steegers EA, Hofman A, Jaddoe VW, Verhulst FC, Tiemeier H. Maternal psychological distress and fetal growth trajectories: the Generation R Study. Psychol Med 2010; 40: 633–643. [DOI] [PubMed] [Google Scholar]
- 69. Khashan AS, McNamee R, Abel KM, Pedersen MG, Webb RT, Kenny LC, Mortensen PB, Baker PN. Reduced infant birthweight consequent upon maternal exposure to severe life events. Psychosom Med 2008; 70: 688–694. [DOI] [PubMed] [Google Scholar]
- 70. Paarlberg KM, Vingerhoets AJ, Passchier J, Dekker GA, Heinen AG, van Geijn HP. Psychosocial predictors of low birthweight: a prospective study. Br J Obstet Gynaecol 1999; 106: 834–841. [DOI] [PubMed] [Google Scholar]
- 71. Pritchard CW, Teo PY. Preterm birth, low birthweight and the stressfulness of the household role for pregnant women. Soc Sci Med 1994; 38: 89–96. [DOI] [PubMed] [Google Scholar]
- 72. Steer RA, Scholl TO, Hediger ML, Fischer RL. Self‐reported depression and negative pregnancy outcomes. J Clin Epidemiol 1992; 45: 1093–1099. [DOI] [PubMed] [Google Scholar]
- 73. Uguz F, Sahingoz M, Sonmez EO, Karsidag C, Yuksel G, Annagur BB, Annagur A. The effects of maternal major depression, generalized anxiety disorder, and panic disorder on birth weight and gestational age: a comparative study. J Psychosom Res 2013; 75: 87–89. [DOI] [PubMed] [Google Scholar]
- 74. Liu Y, Murphy SK, Murtha AP, Fuemmeler BF, Schildkraut J, Huang Z, Overcash F, Kurtzberg J, Jirtle R, Iversen ES, Forman MR, Hoyo C. Depression in pregnancy, infant birth weight and DNA methylation of imprint regulatory elements. Epigenetics 2012; 7: 735–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Vidal AC, Benjamin Neelon SE, Liu Y, Tuli AM, Fuemmeler BF, Hoyo C, Murtha AP, Huang Z, Schildkraut J, Overcash F, Kurtzberg J, Jirtle RL, Iversen ES, Murphy SK. Maternal stress, preterm birth, and DNA methylation at imprint regulatory sequences in humans. Genet Epigenet 2014; 6: 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Chen J, Li Q, Rialdi A, Mystal E, Ly J, Finik J, Davey T, Lambertini L, Nomura N. Influences of maternal stress during pregnancy on the epi/genome: comparison of placenta and umbilical cord blood. J Depress Anxiety 2014; 3: 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Janssen AB, Capron LE, O'Donnell K, Tunster SJ, Ramchandani PG, Heazell AEP, Glover V, John RM. Maternal prenatal depression is associated with decreased placental expression of the imprinted gene PEG3. Psychological Medicine 2016; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]


