Abstract
Objectives:
Recent studies have recognized that signs of functional disability in schizophrenia are evident in early phases of the disorder, and, as a result, can potentially serve as vulnerability markers of future illness. However, functional measures in the psychosis prodrome have focused exclusively on real-world achievements, rather than on the skills required to carry-out a particular real-world function (ie, capacity). Despite growing evidence that diminished capacity is critical to the etiology of the established disorder, virtually no attention has been directed towards assessing functional capacity in the pre-illness stages. In the present study, we introduce the Map task, a measure to assess functional capacity in adolescent and young-adult high-risk populations.
Methods:
The Map task was administered to 609 subjects at Clinical High-Risk (CHR) for psychosis and 242 Healthy Controls (HCs) participating in the North American Prodrome Longitudinal Study (NAPLS2). Subjects were required to efficiently complete a set of specified errands in a fictional town.
Results:
CHR participants showed large impairments across major indices of the Map task, relative to the HCs. Most importantly, poor performance on the Map task significantly predicted conversion to psychosis, even after adjusting for age, IQ, clinical state, and other potential confounders.
Conclusions:
To the best of our knowledge, the Map task is one of the first laboratory-based measures to assess functional capacity in high-risk populations. Functional capacity deficits prior to the onset of psychosis may reflect a basic mechanism that underlies risk for psychosis. Early intervention targeting this domain may help to offset risk and independently improve long-term outcome.
Key words: prodromal, role functioning, disability, prediction, CHR, NAPLS
Introduction
Functional disability is now a well-established component of chronic psychotic disorders, especially schizophrenia, and represents a major health concern in its own right.1–3 A complex construct, functional disability generally refers to an inability to be independently self-sustaining in the community. Especially when combined with social isolation, as is often the case, functional disability is highly resistant to treatment even when the more dramatic positive symptoms markedly improve with treatment. It has only been recently recognized that signs of functional disability are evident prior to the onset of psychosis, and are not wholly caused by emerging illness. As a result, early impaired functioning may represent a new class of vulnerability indicators of future psychosis,2 previously unstudied and most likely complementary to neurocognitive predictors.4
In prodromal research targeting pre-illness youth at risk, achievement has been measured in several projects using the Global Functioning: Social (GF:S) and Role (GF:R) scales, and early social deficits in particular, appear to be predictors of future illness.5–7 The 2 matched scales are clinical measures reflecting real-world functioning as reported by patients and/or relatives.8 Several recent studies have reported that social skills appear to be biologically related traits9–11 associated with increased vulnerability to the development of psychosis11–18 and are a major component of functional disability.14,19 Role functioning in prodromal individuals has been measured in terms of adjustment to school in adolescents and to early employment in older individuals. While impaired role (school/employment) functioning has not been as predictive of psychosis as social functioning,13,20–22 role deficits have been shown to be core aspects of long-term disability.23 In some cases, role functioning appears to be highly susceptible to environmental determinants, such as economic factors and access to educational resources.24
Due to the variability in role achievement, functional capacity may be a more valid predictor of psychosis at this phase of illness. The distinction between functional capacity vs achievement, 2 major components of functional disability, is particularly salient to the vulnerability issue. “Capacity” refers to one’s true ability to perform in the real world and “achievement,” to the extent to which capacity is translated into real-world accomplishments.25 Patients with chronic psychosis have been found to be highly impaired in both achievement and capacity.26 Of the 2 constructs, achievement is the more quantifiable and is typically measured using attainment of real life milestones or accomplishments.27 Functional capacity, on the other hand, is a more abstract construct referring to the actual ability to sustainably adapt to the demands of society. Capacity measures typically involve standardized paper and pencil assessments in a laboratory setting that simulate limited but real-world scenarios.28 While chronically ill adult patients have been shown to have major impairments in both capacity and achievement, this is less clear for individuals at Clinical High-Risk (CHR) for psychosis.
However, despite substantial evidence that diminished capacity is a key barrier to good functional outcomes in adult patients with schizophrenia, virtually no attention has been directed towards capacity in the pre-illness stages or the extent to which deficits in capacity precede or parallel the decline in achievement often reported during the prodromal stage.29 Although several functional capacity measures have been developed, eg, the UCSD Performance-Based Skills Assessment (UPSA30–33), they are designed to test adult skill sets in highly impaired chronically ill schizophrenia or bipolar patients, and are not appropriate for younger at-risk individuals either in content or difficulty level.
To address this gap in prodromal research, we sought to develop a laboratory-based measure analogous to role capacity measures used with chronic adult patients, but that addressed skills much more complex than those characteristically assessed in florid patients. The task had to go beyond school performance to determine if an individual is able to conduct basic everyday tasks. The resulting Map task, unlike existing role capacity measures, is free of potential confounds such as social interaction and does not require mastery of any adult level tasks (ie, check writing, money management) making it age-appropriate for adolescents. It can be administered and scored easily and reliably and is suitable for use with less impaired at-risk adolescents and young adults. The Map task was inspired by errand-planning tasks developed for the Office of Naval Research to study planning processes34 that were later adapted for use with children.35,36 The task requires participants to complete a list of errands in a timely and efficient manner stressing the ability to simultaneously process multiple instructions, thus measuring a narrowly defined set of specific skills required to carry out a particular real-world function, in this case, the ability to complete a set of errands on a shopping trip.
The goals of the current study were to evaluate the validity of the Map task as a new risk factor for psychosis that reflects functioning rather than clinical components of illness. Specific goals of the study were to: (1) Determine whether CHR individuals show impairments on the Map task compared to Healthy Controls (HCs); (2) Determine whether poor performance on the Map task is predictive of conversion to psychosis and; (3) Establish that the predictive association between impaired functional capacity as measured by the Map task and psychosis is independent of the contributions of other potentially explanatory variables such as intellectual deficits, clinical symptoms, and role achievement.
Materials and Methods
Sample Description
Data was collected as part of the larger North American Prodrome Longitudinal Study (NAPLS2) sample (N = 1044), a multisite prospective study that is funded by the National Institute of Mental Health.37 The NAPLS2 sample consists of 764 CHR subjects and 280 HC participants. Subjects were collected at the 8 NAPLS2 sites located at Emory University, Harvard University, University of Calgary, UCLA, UCSD, UNC at Chapel Hill, Yale University, and the Zucker Hillside Hospital in New York. Recruitment efforts varied at the 8 sites and primarily resulted from direct referrals, referrals from community professionals, and direct advertising in the community and on the internet.38
Participants were identified as CHR based on criteria derived from the Scale of Prodromal Symptoms (SOPS39–41). Inclusion criteria were based on one of the following: (1) attenuated positive symptoms (APS), defined by the onset or worsening in the past year of 1 or more moderate to severe attenuated positive symptoms (scores of 3–5 on the SOPS 0–6 scale); (2) genetic risk and deterioration (GRD), defined as having a first-degree relative with an Axis I psychotic disorder or having an Axis II diagnosis of Schizotypal Personality Disorder and a 30% decline in functioning in the past year; or (3) Brief intermittent psychotic symptoms (BIPS), having 1 psychotic level symptom (score of 6 on SOPS) that is brief and spontaneously remits. CHR and HCs between the ages of 12–35 were eligible to participate.
Exclusion criteria for all participants included: (1) any Axis I Schizophrenia-spectrum diagnosis; (2) non-English speaking; (3) a medical or neurological disorder; (4) estimated IQ < 70; (5) significant head injury; or (6) severe substance abuse. HCs were additionally excluded if they had a first-degree relative with a diagnosed Axis I psychotic disorder.
Because the Map task was introduced in Year 2 of the NAPLS study, a somewhat reduced sample completed the task, consisting of CHR: N = 609 and HC: N = 242 (see supplementary figure 1). All procedures were approved by the Institutional Review Board (IRB) at each site. Written informed consent (with assent from participants <18) was obtained from all participants.
The Map Task
The Map task was administered as part of a comprehensive baseline assessment (see Addington38 for details). Participants were first read a set of instructions and then asked to complete specified errands by plotting their route on an 11×14 inch color map of a fictional town. The instructions contained specific details regarding how and in what order the errands needed to be completed, with emphasis placed on planning the most efficient route possible. Streets were displayed on the map that were lined with icons of businesses, offices and municipal buildings to simulate a typical town, including a hospital, various clothing and grocery stores, a post office, library, museum, firehouse, and apartments.
Participants were given a pen and instructed to draw the route on the map that they would take through town to complete the errands as efficiently and quickly as possible. Some errands could be completed at more than 1 location giving the participant the opportunity to choose the best location, eg, which of 3 gas stations to go to. In addition, while there were sufficient choices for subjects to vary in efficiency, the instructions logically dictated when many of the errands should be completed. For example, participants were instructed to enter and exit the town via specific streets. After entering town and parking the car, the participant was expected to visit the bank to withdraw money. Without money, none of the errands that followed could be completed.
The Map task generated 4 outcome indices: (1) Completion time; (2) Total blocks travelled; (3) Total target errands completed (out of 14 possible); and (4) Total errors. Errors resulted from: visiting an unnecessary location; failure to use a door to enter or exit a location; incorrect use of a shortcut and for ordering errors. Ordering errors violated specific instructions and represented illogical planning (eg, going to the Gas Station before getting one’s car from the Parking Lot, going shopping before withdrawing money at the Bank, visiting the Post Office before purchasing the card that had to be mailed).
In order to control for age-related change in performance on the Map task, raw scores from each of the 4 indices were transformed into standard Z-scores using the age-stratified means and SDs of the HC group. When applicable, indices were reverse-scored so that lower scores reflected worse performance relative to the HCs. An overall Map Capacity Score was calculated by averaging the performance on errands, errors, and time. The overall Map composite was then re-standardized using the mean and SD of the HC group.
Clinical Measures
Axis I diagnoses were assessed by the Structured Clinical Interview for DSM-IV (SCID-I42). Prodromal symptoms were assessed by the Structured Interview for Prodromal Syndromes (SIPS) and the companion Scale of Prodromal Symptoms (SOPS39–41). Total scores for each subscale (positive, negative, disorganized, and general) were calculated. Total negative symptom scores were determined by adding items 2 through 5, excluding items 1 (social anhedonia) and 6 (deterioration in role) due to the overlap in the functioning measures. Social and role functioning was assessed using the GF:Social and GF:Role scales.8 The GF:Social scale assesses peer relationships, peer conflict, age-appropriate intimate relationships, and involvement with family members. The GF:Role scale rates performance and amount of support needed in one’s specific role (ie, school, work).8 The Global Assessment of Functioning Scale (GAF) assessed clinical symptoms, social and role functioning on one global scale. 43
Statistical Analysis
All analyses were conducted using SPSS 16.0 (SPSS Inc). Comparisons of demographic and clinical characteristics were performed with Student’s t test for continuous variables and chi-square test for categorical variables.
The Spearman’s rho coefficient was used to determine the relationship between the Map task indices and demographic, clinical, and IQ measures. Group differences (CHR vs HC; Converter vs Non-Converter) were assessed with multivariate analysis of covariance (MANCOVA) with group as between subject factors and Map index scores (Blocks, Errors, Errands, Time) as within-subject factors, co-varying for baseline age, current and premorbid IQ. Individual ANCOVAs were used to examine differences in the overall Map Capacity Score between the groups (CHR vs HC; Converter vs Non-Converter), co-varying for baseline age, current and premorbid IQ.
To determine whether the impairments on the Map task could predict conversion to psychosis, independent of the contributions of clinical symptoms, intellectual performance, and role functioning (ie, achievement), a Cox proportional hazards model was constructed with the Map Capacity Score, adjusting for baseline age, Total SIPS-Positive, baseline GAF and GF:Role scores, and current and premorbid IQ scores. Bootstrap resampling with replacement (B = 10 000 samples) was used to internally validate the final prediction model.44 These analyses were conducted using data for those subjects who had either developed a psychotic disorder within the study period or who had been followed at least 24 months without developing psychotic symptoms. Missing data was imputed using mean values for Completion Time (missing 3 values) and IQ (missing 15 values) prior to use in all analyses.
Results
Sample Characteristics
Table 1 summarizes baseline demographic and clinical characteristics of the study sample. HC and CHR subjects differed significantly on baseline age and years of education, but not on gender or race. The HC subjects were older and had more years of education and higher premorbid and current IQs than the CHR subjects. As expected, the CHR subjects reported higher scores on all of the SIPS subscales, and lower scores on the functioning measures than the HC subjects, indicating impairment.
Table 1.
Baseline Demographic and Clinical Data and Statistics
| Healthy Controls (N = 242) | CHR (N = 609) | t/χ2 | P Value | |
|---|---|---|---|---|
| Age, y | 19.77±4.80 | 18.55±4.35 | 3.42 | <.001 |
| Education, y | 12.67±3.64 | 11.27±2.83 | 5.35 | <.001 |
| Sex, N male (%) | 126 (52.1) | 352 (57.8) | 2.31 | .13 |
| Race, N Caucasian (%) | 133 (54.96) | 352 (57.80) | 0.570 | .450 |
| Premorbid IQ | 108.30±16.30 | 105.15±16.56 | 2.50 | .013 |
| Current IQ | 111.14±14.03 | 103.83±15.09 | 6.48 | <.001 |
| Scale of prodromal symptoms | ||||
| Positive | 1.02±1.63 | 11.94±3.86 | −57.90 | <.001 |
| Negative | 1.46±2.30 | 11.83±5.96 | −36.44 | <.001 |
| Disorganized | 0.63±1.17 | 5.16±3.08 | −30.88 | <.001 |
| General | 1.30±2.16 | 9.25±4.22 | −35.90 | <.001 |
| GAF score | 83.41±10.76 | 48.38±10.74 | 42.83 | <.001 |
| Global Functioning: Social Scale | 8.87±0.928 | 6.22±1.54 | 30.61 | <.001 |
| Global Functioning: Role Scale | 8.53±1.39 | 5.97±2.16 | 20.46 | <.001 |
| Baseline medicationa | ||||
| No medication | — | 372 (61.1) | — | — |
| Anti-psychotics | — | 120 (19.7) | — | — |
| Anti-depressants | — | 156 (25.6) | — | — |
| Anxiolytic | — | 42 (6.9) | — | — |
| Mood stabilizer | — | 21 (3.4) | — | — |
Note: CHR, Clinical High-Risk; GAF, Global Assessment of Functioning Scale.
aFive CHR subjects were missing medication information for the baseline testing.
At the time of testing, 61.1% of the CHR subjects that received the Map task were not receiving any medication, 19.7% were receiving antipsychotics, 25.6% anti-depressants, 6.9% anxiolytics, and 3.4% mood stabilizers. In addition, there was no relationship between medication type and performance on any of the Map task indices (rs < .10).
Map Task Group Comparison
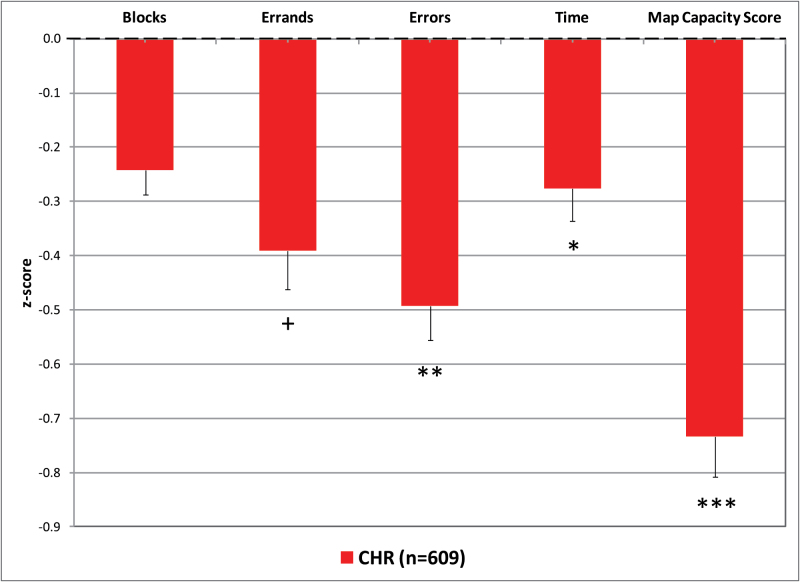
Figure 1 displays the mean performance across the 4 Map indices for the CHR group, relative to the HCs. The CHR group showed significant impairments (P < .05) on all 4 of the Map indices, with mild-to-moderate deficits seen on Blocks, Errands, and Completion Time and large impairments on Errors (see supplementary table S1 for details). Baseline age was a significant covariate (F 4, 845 = 9.69, P < .001).The CHR group also displayed a large impairment on the overall Map Capacity Score (M = −0.73, SD = 1.83), indicating a general deficit on the task relative to the performance of HCs (M = 0.00, SD = 1.00).
Fig. 1.
Map task performance (z-score ± SEM) of the Clinical High-Risk group relative to the Healthy Control (HC) group (mean set to 0, SD set to 1). Note: + P = .05; *P < .05; **P < .01; ***P < .001. Dotted line represents performance of HC group.
Correlations Between Map Task Indices and Demographic, Clinical, and IQ Measures
In HC subjects, 3 Map task indices were significantly correlated with demographic and clinical measures as follows: (1) Blocks correlated with SIPS Negative total score; (2) Errors correlated with SIPS Negative total score, GF:Role and GAF score; and (3) Map Capacity Score significantly correlated with GF:Role (supplementary table S2).
In CHR subjects, the Map task indices significantly correlated with demographic and clinical measures as follows: (1) Blocks correlated GF:Role; (2) Errands correlated with GF:Role; (3) Errors correlated with SIPS Negative total score, GF:Role, and GAF score; (4) Completion time correlated with IQ; and (5) Map Capacity Score correlated with GF:Social and GF:Role and GAF score (supplementary table S3). IQ as measured by the WASI Vocabulary and Block Design subtests was correlated with Blocks, Errands, Errors, and the Map Capacity Score.
Prediction of Conversion to Psychosis
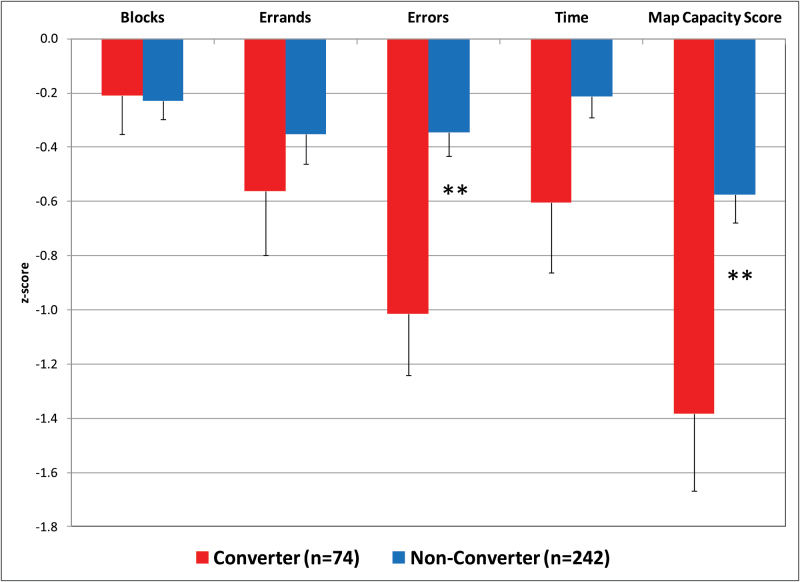
As shown in Figure 2, relative to the HCs, Converters and Non-Converters showed similar impairments on Blocks and Errands (P > .05). However, Converters showed large impairments on Errors (M = −1.01, SD = 1.97) and the Map Capacity Score (M = −1.38, SD = 2.45; see supplementary table S4 for more details) compared to the performance of Non-Converters (Errors: M = −0.35, SD = 1.00, Cohen’s d [effect size] = 0.35; Map Capacity Score: M = −0.57, SD = 1.63, Cohen’s d = 0.45). At a cut-point of −0.5 SD, the Map Capacity Score has a Positive Predictive Value of 30%, Negative Predictive Value of 81%, sensitivity of 50% and a specificity of 64%.
Fig. 2.
Map task performance (z-score ± SEM) for Clinical High-Risk (CHR) Converters vs CHR Non-Converters. Note: *P < .05; **P < .01. ***P < .001.
The Map Capacity Score significantly predicted conversion to psychosis (Overall model χ2 = 23.59, df = 2, P < .001). As shown in table 2, even when adjusting for baseline age, Total SIPS-Positive, baseline GAF and GF:Role scores, and current and premorbid IQ scores the Map Capacity Score continued to predict conversion to psychosis. The bootstrap approximation with 10 000 iterations yielded bias-corrected and accelerated CIs, which demonstrated the robustness of the Map Capacity Score to predict psychosis because zero is not between the lower and upper bound (Map Capacity Score: 95% CI: (−0.416) to (−0.061), P = .009; Age: 95% CI: (−0.107) to (−0.004), P = .12; Positive Symptoms: 95% CI: (0.046) to (0.187), P = .001; GAF: 95% CI: (−0.028) to (0.024), P = .93; Current IQ: 95% CI: (−0.024) to (0.014), P = .594; Premorbid IQ: 95% CI: (−0.005) to (0.033), P = .14; GF:Role: 95% CI: (−0.199) to (0.054), P = .257).
Table 2.
Predicting Conversion to Psychosis With the Map Capacity Score
| Conversion to Psychosis | |||||
|---|---|---|---|---|---|
| β | SE | Wald | Hazard Ratio (95% CI) | P Value | |
| Map Capacity Score | −.23 | 0.10 | 5.436 | 0.792 (0.650–0.963) | .02 |
| Baseline age | −.05 | 0.03 | 1.928 | 0.956 (0.897–1.019) | .165 |
| SIPS total positive | .11 | 0.03 | 11.179 | 1.116 (1.047–1.191) | .001 |
| Global Assessment of Functioning | −.001 | 0.01 | 0.007 | 0.999 (0.973–1.025) | .932 |
| Current IQ | −.01 | 0.01 | 0.234 | 0.995 (0.976–1.015) | .629 |
| Premorbid IQ | .01 | 0.01 | 2.071 | 1.013 (0.995–1.031) | .15 |
| GF: Role | −.07 | 0.07 | 1.185 | 0.930 (0.815–1.06) | .276 |
Note: SIPS, Structured Interview for Prodromal Syndromes; GF, Global Functioning.
Discussion
To the best of our knowledge, the Map task is one of the first laboratory measures specifically designed to assess a young person’s basic capacity to function in society, ie, to measure capacity to carry-out age-appropriate skills that lead to independent community living. From this perspective capacity provides the foundation for what can actually be achieved. This is comparable to the comparison between IQ (capacity) vs grades at school (achievement). In terms of applications to high-risk populations and early interventions, this study yielded 3 main findings. First, CHRs, in general, performed poorly on the task relative to HCs. Second, CHR individuals who later developed psychosis were more impaired on several aspects of the task when compared to subjects who did not develop psychosis, suggesting that functional capacity may serve as a marker of impending psychosis. Lastly, and especially important to supporting marker potential, performance on the Map task was predictive of conversion to psychosis, independent of intellectual deficits, clinical symptoms, and role achievement. This suggests that functional capacity may represent a basic biologically-based trait that has the potential to predict psychosis.
Overall, the Map task was effective in differentiating CHR subjects, in general, from HCs, with the CHR group scoring significantly lower than the HC group on several the Map task indices, suggesting capacity problems are characteristics of risk for psychosis. CHR subjects made mistakes on simple instructions, such as entering or exiting the town using the wrong street, entering extra stores not on the list, and not entering/exiting the stores through the indicated door. The overall Capacity Score, which takes into account 3 of the major Map task indices, indicates a general deficiency of functional capacity in the CHR group that may be comparable to a general index of impaired neurocognitive performance.
Of perhaps more importance, the Map Capacity Score significantly predicted conversion to psychosis, above and beyond the contributions of baseline attenuated positive symptoms. In addition, this relationship was not an artifact of IQ deficits or clinical symptoms, as the Map Capacity Score predicted psychosis even when controlling for intellectual performance. Of particular interest, while CHR Converters showed similar performance on hits, ie, Errands, compared to Non-Converters, they made significantly more Errors. This suggests that the Map task taps into a specific domain of real-life functioning, the ability to stay on target and screen out irrelevant stimuli/tasks. Past work from our group has shown that true-positive individuals (ie, Converters) consistently have lower social functioning and lower, but inconsistent, role achievement scores, as measured in several populations using the GF scales, relative to Non-Converters many years before onset of psychosis.8 The current study extends these findings by indicating that true-positive subjects have a larger deficit in their “capacity” to perform everyday tasks and that this separate dimension of functioning may serve, in its own right, as an early developmental marker of eventual illness.
This is the first prodromal study, to our knowledge, to focus on the capacity of role functioning as being distinctly different than social skills, where role represents a broader adjustment to life demands than just school or work performance. Moreover, our findings indicate that efficient functioning in a real-world situation, while depending on cognition/IQ, may also involve a broader skill set. Measures such as the Map are “neurofunctional,” as they involve a substantial neurocognitive component, but are measuring skill sets critical for carrying out everyday activities, such as taking the bus to school, going to a restaurant, getting a driver’s license, or in the case of the Map task, carrying out a shopping trip. While these tasks involve IQ, working memory, declarative memory, processing speed, etc., functional capacity can be considered midway between complex real-world behaviors and the more reductionistic cognitive building blocks. Along this progression from cognition→capacity→achievement, achievement is multi-determined and subject to considerable environmental input and thus difficult to assess, while capacity is closer to biological and genetic causation. These vulnerability or risk factors are comparable to neurocognitive risk factors but are tapping a different domain of impairment involving more complex behaviors than cognitive processes. For example, if an individual wants to go to a restaurant, the ability to plan this event, obtain the reservations, and organize the trip, would all be capacity; going to the restaurant would be the achievement.
Overall, this preliminary assessment of the Map task provides encouraging results for the widespread use of this measure in prodromal research. There was virtually no relationship between Map indices and clinical symptoms in the CHR group, supporting the assertion that ability to perform at school or work are problems that are not determined by positive symptoms.15 In contrast, the Map Capacity Score was significantly correlated with role achievement,8 at comparable levels to correlations reported between the UPSA and other measures of global functioning such as the GAF.45 Ideally, a measure of functional capacity would test skills in an actual real-world situation or setting (ie, at a grocery store46). However, practical and logistical issues limit the ability to utilize a real-world setting. Moreover, current functional capacity measures are typically designed to assess skills that are more relevant for an adult population, such as writing a check,30 which can be particularly problematic for CHR research that involves adolescents and young adults. The Map task circumvents some of these issues by recreating an age-appropriate experience of planning and carrying out a series of errands. The current findings suggest that the Map task is sufficiently challenging for healthy adolescent populations, eliminating the possibility of ceiling effects on performance, and is sensitive enough to differentiate between clinical and healthy populations. Of the indices generated by the Map task, as indicated above, errors are most informative. It should be noted that based on the current findings scoring of the blocks travelled has been eliminated from the standard Map administration since it proved to be very labor intensive and did not differentiate between any of the CHR groups.
In conclusion, the Map task adds to the newly emerging set of measures of functional capacity, a construct gaining attention as critical to the etiology of psychosis and therefore to prevention. Our findings have extended this notion to the early stages of the illness and suggest that functional capacity is primary to achievement in the real-world and therefore may constitute a new marker of impending illness. Future research should examine the potential of a multi-variable functional profile consisting of a range of capacity and achievement measures to provide the most accurate method to predict long-term prognosis. In turn, the complexity of functional deficits is likely to contribute unique information for developing more optimal preventive interventions.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
Supported by grants from the National Institute of Mental Health: U01 MH081984 to J.A.; U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to L.J.S.; R01 MH60720, U01 MH082022, and K24 MH76191 to K.S.C.; U01 MH081902 to T.D.C.; P50 MH066286 (Prodromal Core) to C.E.B.; grant U01 MH082004 to D.O.P.; U01 MH081988 to E.F.W.; RO1 MH076989-01 to D.H.M.; U01 MH082022 to S.W.W.; U01 MH081857 and MH61523 to B.A.C.; the Zucker Hillside Hospital NIMH Advanced Center for Intervention and Services Research for the Study of Schizophrenia MH 074543-01 to John M. Kane, M.D. REC received funding from the Brain and Behavior Research Foundation (NARSAD): Young Investigator Grant 19740 and the Let the Sun Shine Run/Walk, Cold Spring, MN. No funding agency had any role in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Supplementary Material
Acknowledgments
The authors would like to thank the NAPLS2 study participants and the entire NAPLS2 and RAP program staff for their time and effort. In particular, we would like to thank Bill Stone, Ruth Olsen, Lauren Baskir-Quinones and Gary Brucato for their assistance in carrying out the study and Rob Perry for his graphic design. T.D.C. reports that he is a consultant to the Los Angeles County Department of Mental Health and to Boehringer Ingelheim Pharmaceuticals. D.H.M. reports that he is a consultant to Boehringer Ingelheim Pharmaceuticals. S.W.W. reports that during the last 36 months he has received investigator-initiated research funding support from Pfizer and sponsor-initiated research funding support from Auspex and Teva. He has consulted to Merck, Biomedisyn (unpaid), and Boehringer Ingelheim. He has also served as an unpaid consultant to DSM-5. He has been granted US patent no. 8492418 B2 for a method of treating prodromal schizophrenia with glycine agonists and has received royalties from Oxford University Press. P.D.H. has received grants/research support from The Stanley Medical Research Foundation and Takeda, and has served as a consultant for Allergan, Boehringer Ingelheim, Forum Pharma, Lundbeck, Otsuka America, Sanofi, Sunovion, and Takeda Pharma.
References
- 1. Harvey PD. Assessment of everyday functioning in schizophrenia. Innov Clin Neurosci. 2011;8:21–24. [PMC free article] [PubMed] [Google Scholar]
- 2. Harvey PD. Disability in schizophrenia: contributing factors and validated assessments. J Clin Psychiatry. 2014;75:15–20. [DOI] [PubMed] [Google Scholar]
- 3. Harvey PD. Direct measurement of disability. Psychiatry (Edgmont). 2009;6:43–46. [PMC free article] [PubMed] [Google Scholar]
- 4. Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 2012;11:73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meyer EC, Carrión RE, Cornblatt BA, et al. ; NAPLS group The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr Bull. 2014;40:1452–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Niendam TA, Bearden CE, Johnson JK, et al. Neurocognitive performance and functional disability in the psychosis prodrome. Schizophr Res. 2006;84:100–111. [DOI] [PubMed] [Google Scholar]
- 7. Schlosser DA, Jacobson S, Chen Q, et al. Recovery from an at-risk state: clinical and functional outcomes of putatively prodromal youth who do not develop psychosis. Schizophr Bull. 2012;38:1225–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cornblatt BA, Auther AM, Niendam T, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carrión RE, Cornblatt BA, McLaughlin D, et al. Contributions of early cortical processing and reading ability to functional status in individuals at clinical high risk for psychosis. Schizophr Res. 2015;164:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schreiner MJ, Karlsgodt KH, Uddin LQ, et al. Default mode network connectivity and reciprocal social behavior in 22q11.2 deletion syndrome. Soc Cogn Affect Neurosci. 2014;9:1261–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karlsgodt KH, Niendam TA, Bearden CE, Cannon TD. White matter integrity and prediction of social and role functioning in subjects at ultra-high risk for psychosis. Biol Psychiatry. 2009;66:562–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Addington J, Cornblatt BA, Cadenhead KS, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168:800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. 2008;99:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carrión RE, McLaughlin D, Goldberg TE, et al. Prediction of functional outcome in individuals at clinical high risk for psychosis. JAMA Psychiatry. 2013;70:1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cornblatt BA, Carrión RE, Addington J, et al. Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38:1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tarbox SI, Addington J, Cadenhead KS, et al. Premorbid functional development and conversion to psychosis in clinical high-risk youths. Dev Psychopathol. 2013;25:1171–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Velthorst E, Nieman DH, Linszen D, et al. Disability in people clinically at high risk of psychosis. Br J Psychiatry. 2010;197:278–284. [DOI] [PubMed] [Google Scholar]
- 18. Velthorst E, Nelson B, Wiltink S, et al. Transition to first episode psychosis in ultra high risk populations: does baseline functioning hold the key? Schizophr Res. 2013;143:132–137. [DOI] [PubMed] [Google Scholar]
- 19. Lin A, Wood SJ, Nelson B, et al. Neurocognitive predictors of functional outcome two to 13 years after identification as ultra-high risk for psychosis. Schizophr Res. 2011;132:1–7. [DOI] [PubMed] [Google Scholar]
- 20. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nieman DH, Ruhrmann S, Dragt S, et al. Psychosis prediction: stratification of risk estimation with information-processing and premorbid functioning variables. Schizophr Bull. 2014;40:1482–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alderman T, Addington J, Bearden C, et al. Negative symptoms and impaired social functioning predict later psychosis in Latino youth at clinical high risk in the North American prodromal longitudinal studies consortium. Early Interv Psychiatry. 2015;9:467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Harvey PD, Heaton RK, Carpenter WT, Jr, Green MF, Gold JM, Schoenbaum M. Functional impairment in people with schizophrenia: focus on employability and eligibility for disability compensation. Schizophr Res. 2012;140:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harvey PD, Helldin L, Bowie CR, et al. Performance-based measurement of functional disability in schizophrenia: a cross-national study in the United States and Sweden. Am J Psychiatry. 2009;166:821–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harvey PD, Velligan DI, Bellack AS. Performance-based measures of functional skills: usefulness in clinical treatment studies. Schizophr Bull. 2007;33:1138–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harvey PD, Sabbag S, Prestia D, Durand D, Twamley EW, Patterson TL. Functional milestones and clinician ratings of everyday functioning in people with schizophrenia: overlap between milestones and specificity of ratings. J Psychiatr Res. 2012;46:1546–1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: relevance to persons with schizophrenia. Schizophr Res. 2004;72:53–67. [DOI] [PubMed] [Google Scholar]
- 29. Cornblatt BA, Carrión RE, Auther A, et al. Psychosis prevention: a modified clinical high risk perspective from the Recognition and Prevention (RAP) Program. Am J Psychiatry. 2015;172:986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. [DOI] [PubMed] [Google Scholar]
- 31. Mausbach BT, Bowie CR, Harvey PD, et al. Usefulness of the UCSD performance-based skills assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. J Psychiatr Res. 2008;42:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mausbach BT, Depp CA, Bowie CR, et al. Sensitivity and specificity of the UCSD Performance-based Skills Assessment (UPSA-B) for identifying functional milestones in schizophrenia. Schizophr Res. 2011;132:165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mausbach BT, Harvey PD, Pulver AE, et al. Relationship of the Brief UCSD Performance-based Skills Assessment (UPSA-B) to multiple indicators of functioning in people with schizophrenia and bipolar disorder. Bipolar Disord. 2010;12:45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hayes-Roth B, Cammarata S, Goldin SE, Hayes-Roth F, Rosenschein S, Thorndyke PW. Human Planning Processes: DTIC Document. Santa Monica, CA: RAND Corporation; 1980. [Google Scholar]
- 35. Pea RD, Hawkins J. Planning in a chore-scheduling task. In: Friedman SL, Scholnick EK, Cocking RR, eds. Blueprints for Thinking: The Role of Planning in Cognitive Development. New York, NY: Cambridge University Press; 1987:273–302. [Google Scholar]
- 36. Rogoff B, Gauvain M, Gardner W. The development of children’s skills in adjusting plans to circumstances. In: Friedman SL, Scholnick EK, Cocking RR, eds. Blueprints for Thinking: The Role of Planning in Cognitive Development. New York, NY, US: Cambridge University Press; 1987:303–320. [Google Scholar]
- 37. Addington J, Cadenhead KS, Cannon TD, et al. North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Addington J, Cadenhead KS, Cornblatt BA, et al. North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophr Res. 2012;142:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. [DOI] [PubMed] [Google Scholar]
- 40. Miller TJ, McGlashan TH, Rosen JL, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. [DOI] [PubMed] [Google Scholar]
- 41. Miller TJ, McGlashan TH, Woods SW, et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q Winter. 1999;70:273–287. [DOI] [PubMed] [Google Scholar]
- 42. First M, Spitzer R, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). In: Biometrics Research. New York, NY: New York State Psychiatric Institute; 1995. [Google Scholar]
- 43. Hall RC. Global assessment of functioning. A modified scale. Psychosomatics. 1995;36:267–275. [DOI] [PubMed] [Google Scholar]
- 44. Sauerbrei W, Schumacher M. A bootstrap resampling procedure for model building: application to the Cox regression model. Stat Med. 1992;11:2093–2109. [DOI] [PubMed] [Google Scholar]
- 45. Green MF, Nuechterlein KH, Kern RS, et al. Functional co-primary measures for clinical trials in schizophrenia: results from the MATRICS Psychometric and Standardization Study. Am J Psychiatry. 2008;165:221–228. [DOI] [PubMed] [Google Scholar]
- 46. Hamera E, Brown CE. Developing a context-based performance measure for persons with schizophrenia: the test of grocery shopping skills. Am J Occup Ther. 2000;54:20–25. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.