Abstract
Objectives
To determine how often hospitalized older patients principally diagnosed with pneumonia, chronic obstructive pulmonary disease (COPD), or heart failure (HF) are concurrently treated for two or more of these acute cardiopulmonary conditions.
Design
Retrospective cohort study.
Setting
368 US hospitals in the Premier research database
Participants
Patients ≥65 years-old principally hospitalized with pneumonia, COPD, or HF in 2009 or 2010.
Measurements
Proportion of diagnosed episodes of pneumonia, COPD, or HF concurrently treated for two or more of these acute cardiopulmonary conditions during the first two hospital days.
Results
Among 91,709 diagnosed pneumonia hospitalizations, 32% received treatment for two or more acute cardiopulmonary conditions (18% received treatment for HF, 18% received treatment for COPD, and 4% received treatment for both HF and COPD). Among 41,052 diagnosed COPD hospitalizations, 19% received treatment for two or more acute cardiopulmonary conditions (all of which involved additional HF treatment). Among 118,061 diagnosed HF hospitalizations, 38% received treatment for two or more acute cardiopulmonary conditions (34% received treatment for pneumonia, 9% received treatment for COPD, and 5% received treatment for both pneumonia and COPD).
Conclusion
Hospitalized older patients diagnosed with pneumonia, COPD, or HF are frequently treated for two or more acute cardiopulmonary conditions, suggesting that clinical syndromes often fall between traditional diagnostic categories. Research is needed to evaluate the risks and benefits of real-world treatment for the many older patients whose presentations elicit diagnostic uncertainty or concern for coexisting acute conditions.
Keywords: Hospital medicine, pharmacoepidemiology, comorbidity, pulmonary diseases, cardiovascular disease
INTRODUCTION
Treatment guidelines,1-3 clinical textbooks,4-6 and investigations7-10 most often consider treatment during hospitalization from the perspective of a distinct disease or condition. Yet in practice, hospitalized patients are complex11 and may simultaneously receive multiple treatments that bridge traditional disease-specific categories due to concurrent illness, diagnostic uncertainty, or other reasons. Indeed, prior work has shown that patients hospitalized with a principal diagnosis of heart failure (HF) frequently receive concurrent therapies for pneumonia, acute asthma, or exacerbated chronic obstructive pulmonary disease (COPD), often for the entirety of hospitalization.12
Yet we do not know if this observation represents findings specific to heart failure or instead signals a more generalizable pattern among patients hospitalized with the most common cardiorespiratory illnesses. On the one hand, HF may be the quintessential syndrome that exemplifies uncertain treatment boundaries, as presenting symptoms are often non-specific13,14 and may therefore be interpreted as resulting from respiratory or other illnesses. However, it may instead be that the most common acute cardiac and pulmonary conditions exhibit significant pathophysiologic overlap,15,16 are often concomitantly present,17-19 or are difficult to distinguish from one another in real world practice.13,14,20,21 Concurrent treatment may therefore be common in typical clinical practice. This question is important as large numbers of patients may have acute exacerbations that arise from two or more distinct conditions and therefore benefit little from scientific evidence focused on the treatment of single diseases. In particular, few studies and no large trials have tested treatment strategies in patients presenting with indistinct clinical syndromes or concomitant acute conditions, the treatment of which may work at cross-purposes.
We therefore sought to determine the frequency with which patients hospitalized with diagnoses of pneumonia, COPD, or HF are concurrently treated with therapies for two or more of these acute cardiopulmonary conditions, all of which frequently arise as exacerbations of underlying chronic illness. These three conditions are among the most common reasons for hospitalization among older persons and are a focus of quality improvement in the Medicare program.22 If concurrent treatment is frequently present, this finding would demonstrate that empiric practice diverges significantly from narrowly focused disease taxonomies and evidence that prevail in medical education and the medical literature. This finding would also provide strong evidence that many hospitalized patients have acute illnesses that are difficult to categorize and largely unstudied. There would be great need to understand the effectiveness and safety of real-world therapeutic strategies that cross disease-specific boundaries in this complex population.
Accordingly, we examined a large database of hospitalizations in the US to primarily investigate whether older patients hospitalized with a principal diagnosis of pneumonia or COPD frequently receive concurrent treatment for HF and/or each other. As a secondary analysis, we sought to quantify the expected additional risk of major adverse hospital outcomes associated with treatment for two or more acute cardiopulmonary conditions. We focused on treatment patterns in older persons, as they are the most medically complex age group,11,23,24 the most likely to present in a non-specific manner,25 and the most likely to experience adverse effects of treatment.26
METHODS
Data source and study sample
We conducted a retrospective cohort study using the Premier research database, a voluntary, fee-supported database developed and maintained by Premier, Inc., for measuring quality and healthcare utilization. The Premier database contains information on approximately one-fifth of all US discharges from 2000 to the present. The database contains standard hospital discharge files as well as date-stamps of all billed items, including procedures, medications, and diagnostic services at the individual patient level. Drug utilization information is available by day of stay and includes strength, quantity, and dosing.
We created two disease-specific cohorts of patients 65 years and older who were hospitalized in 2009 or 2010 with a principal discharge diagnosis of pneumonia or COPD. To provide further perspective on patterns of concurrent treatment and in-hospital outcomes of patients in these two cohorts, we also created a comparator cohort of patients 65 years and older hospitalized in 2009 or 2010 with a principal discharge diagnosis of HF. Cohorts were defined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes used by the Centers for Medicare & Medicaid Services in hospital quality measurement.22,27,28 The pneumonia cohort was defined using ICD-9-CM codes 480.xx, 481, 482.0, 482.1, 482.2, 482.30, 482.31, 482.32, 482.39, 482.4x, 482.8x, 482.9, 483.xx, 485, 486, 487.0, and 488.11. The COPD cohort was defined using ICD-9-CM codes 491.21, 491.22, 491.8, 491.9, 492.8, 493.2xx, and 496. The HF cohort was defined using ICD-9-CM codes 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, and 428.xx. We excluded hospitalizations involving transfer from another hospital or that had an unknown admission source, as information about treatment before hospitalization was unavailable. We also excluded hospitalizations with a pediatric attending in order to concentrate on care patterns of physicians who treat adults. Although administrative codes specifically identify syndromes of pneumonia, COPD, and HF,29-32 we sought to further increase the likelihood that these conditions were present by requiring hospitalizations to be at least two days in duration and demonstrate evidence of disease-specific treatment during the first two hospital days. Accordingly, pneumonia hospitalizations required treatment with antibiotics, COPD hospitalizations required treatment with corticosteroids, and HF hospitalizations required treatment with intravenous or oral loop diuretics, intravenous vasodilators, or intravenous positive inotropes.
Treatments studied
For each hospitalization, we noted treatment with commonly used therapies for pneumonia, COPD, and HF. For pneumonia, we identified treatment with antibiotics from pharmacologic classes used to treat both community-acquired and hospital-acquired pneumonia including penicillins, cephalosporins, fluoroquinolones, macrolides, vancomycin, tetracyclines, aminoglycosides, and carbapenems. For COPD, we identified daily corticosteroid treatments within a dose range of 20mg to 80mg of oral prednisone or 120mg to 800mg of intravenous prednisone equivalents, as has been done previously.33 For HF, we identified treatment with (1) intravenous loop diuretics, (2) intravenous vasodilators including nitroglycerin, nitroprusside, and nesiritide or (3) intravenous positive inotropes including dobutamine, dopamine, and milrinone. To increase the likelihood that antibiotics and corticosteroids were intended for respiratory illness, we used ICD-9-CM present-on-admission diagnosis codes to exclude hospitalizations with evidence of common infections besides pneumonia or inflammatory, allergic, or autoimmune conditions other than COPD, as has been done previously.12 To increase the likelihood that intravenous diuretics were intended for HF, we used ICD-9-CM present-on-admission diagnosis codes to exclude hospitalizations with evidence of cirrhosis or ascites.12
Definitions of concurrent treatment
For the pneumonia cohort, concurrent treatment was defined as the receipt of antibiotics plus intravenous diuretics, intravenous vasodilators, intravenous inotropes or corticosteroids during the first two hospital days. For the COPD cohort, concurrent treatment was defined as the receipt of corticosteroids plus intravenous diuretics, intravenous vasodilators or intravenous inotropes during the first two hospital days. Antibiotic treatment was not used to define concurrent treatment in the COPD cohort, as guidelines for the inpatient management of COPD recommend that antibiotics be administered to most patients.2 As a result, treatment with antibiotics in this cohort cannot reliably identify concerns for concurrent infection. For the HF cohort, concurrent treatment was defined as the receipt of oral or intravenous diuretics, intravenous vasodilators or intravenous inotropes plus antibiotics or corticosteroids during the first two hospital days.
Outcomes
Our primary outcome was the proportion of hospitalizations with a principal discharge diagnosis of pneumonia, COPD, or HF that received concurrent treatment for two or more of these acute cardiopulmonary conditions during the first two hospital days.
Secondary outcomes for each disease cohort included the adjusted odds of admission to an intensive care unit (ICU), late intubation (intubation two or more days after admission), and in-hospital death among patients receiving concurrent treatment for two or more acute cardiopulmonary conditions.
Statistical analyses
For our primary analysis, we calculated summary statistics for categorical variables using frequencies and percentages. We used chi-square tests for comparisons of treatment groups. For these analyses, we included all hospitalizations meeting inclusion criteria rather than one random hospitalization per patient since our intent was to study prevailing treatment patterns during hospitalization for common cardiopulmonary conditions. In addition, our data does not include all repeat hospitalizations, only those to the discharging hospital. We therefore could not identify repeat hospitalizations to all other hospitals inside and outside of the Premier network. For our secondary analysis, we used hierarchical logistic regression to calculate adjusted odds ratios and corresponding 95% confidence intervals (CI) for the outcomes of ICU admission, late intubation, and in-hospital mortality. In all models, the referent group consisted of patients who received treatment for only the singular acute cardiopulmonary condition corresponding to the principal discharge diagnosis. As above, we used all hospitalizations when calculating the adjusted odds of ICU admission and late intubation. However, we used one random hospitalization per patient when calculating the adjusted odds of in-hospital mortality to ensure that death could only occur once per patient. We adjusted for patient age, patient sex, and Elixhauser comorbidities34 in all models. Elixhauser comorbidities are identified using secondary discharge diagnosis codes for conditions that were present prior to admission, unrelated to the primary reason for hospitalization, and not a complication of hospital care. These comorbidities were identified with software provided by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (versions 3.4-3.6 for federal fiscal years 2009-2011, respectively).34 All statistical tests were 2-sided, and significance was indicated by p-values less than 0.05. Analyses were conducted with SAS 9.2 (SAS Institute Inc., Cary, NC).
The Yale University Human Investigation Committee reviewed the study protocol and determined that it was not considered Human Subjects Research as defined by the Office of Human Research Protections.
RESULTS
Our final study cohorts were comprised of 91,709 hospitalizations for pneumonia, 41,052 hospitalizations for COPD, and 118,061 hospitalizations for HF from 368 hospitals. These cohorts were comprised of 83,964, 33,864, and 92,910 unique patients, respectively.
Patient characteristics are presented in Table 1. The majority of patients were 75 years of age and older and were women. Comorbidities were common. Fluid and electrolyte disorders were most frequent in the pneumonia cohort (39%), depression was most common in the COPD cohort (15%), and both diabetes and renal failure were most common in the HF cohort (44% in both cases). Comorbidities were generally more common among hospitalizations of patients receiving treatment for two or more acute cardiopulmonary conditions in the COPD cohort, with particular differences noted for the prevalence of diabetes and renal failure (Table 2). Differences in the prevalence of comorbidities by treatment strategy were less frequent and pronounced in the pneumonia and HF cohorts (Table 2).
Table 1. Characteristics of Patients in Pneumonia, Chronic Obstructive Pulmonary Disease, and Heart Failure Cohorts.
| Pneumonia cohort (91,709 hospitalizations) N (%) |
Chronic obstructive pulmonary disease cohort (41,052 hospitalizations) N (%) |
Heart failure cohort (118,061 hospitalizations) N (%) |
|
|---|---|---|---|
| Age in years | |||
| 65-74 | 28,615 (31) | 19,753 (48) | 32,395 (27) |
| 75-84 | 36,042 (39) | 15,622 (38) | 46,119 (39) |
| 85+ | 27,052 (30) | 5,677 (14) | 39,547 (34) |
| Sex | |||
| Female | 48,048 (52) | 23,476 (57) | 63,180 (54) |
| Male | 43,661 (48) | 17,576 (43) | 54,881 (46) |
| Comorbidities | |||
| Peripheral vascular disease | 9,034 (10) | 4,148 (10) | 17,713 (15) |
| Hypertension | 64,884 (71) | 28,706 (70) | 84,004 (71) |
| Diabetes with and without complications | 29,388 (32) | 12,929 (31) | 51,924 (44) |
| Obesity | 6,124 (7) | 4,200 (10) | 14,207 (12) |
| Chronic pulmonary disease | 48,689 (53) | --- | 46,470 (39) |
| Renal failure | 20,271 (22) | 5,834 (14) | 52,034 (44) |
| Fluid and electrolyte disorders | 35,732 (39) | 10,444 (25) | 35,877 (30) |
| Deficiency anemias | 29,150 (32) | 7,866 (19) | 40,976 (35) |
| Liver disease | 525 (1) | 195 (0) | 652 (1) |
| Depression | 12,012 (13) | 5,988 (15) | 11,755 (10) |
Table 2. Characteristics of Patients Receiving and Not Receiving Concurrent Treatment for Two or More Acute Cardiopulmonary Conditions among Pneumonia, Chronic Obstructive Pulmonary Disease, and Heart Failure Cohorts.
| Pneumonia cohort | Chronic obstructive pulmonary disease cohort |
Heart failure cohort | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Concurrent treatment (29,768 hospitalizations) N (%) |
No concurrent treatment (61,941 hospitalizations) N (%) |
Concurrent treatment (7,759 hospitalizations) N (%) |
No concurrent treatment (33,293 hospitalizations) N (%) |
Concurrent treatment (44,505 hospitalizations) N (%) |
No concurrent treatment (73,556 hospitalizations) N (%) |
|
| Age in years | ||||||
| 65-74 | 9,879 (33) | 18,736 (30) | 3,180 (41) | 16,573 (50) | 12,066 (27) | 20,329 (28) |
| 75-84 | 11,808 (40) | 24,234 (39) | 3,177 (41) | 12,445 (37) | 17,413 (39) | 28,706 (39) |
| 85+ | 8,081 (27) | 18,971 (31) | 1,402 (18) | 4,275 (13) | 15,026 (34) | 24,521 (33) |
| Sex | ||||||
| Female | 15,671 (53) | 32,377 (52) | 4,242 (55) | 19,234 (58) | 23,942 (54) | 39,238 (53) |
| Male | 14,097 (47) | 29,564 (48) | 3,517 (45) | 14,059 (42) | 20,563 (46) | 34,318 (47) |
| Comorbidities | ||||||
| Peripheral vascular disease |
3,181 (11) | 5,853 (9) | 966 (12) | 3,182 (10) | 6,822 (15) | 10,891 (15) |
| Hypertension | 20,987 (71) | 43,897 (71) | 5,738 (74) | 22,968 (69) | 31,539 (71) | 52,465 (71) |
| Diabetes with and without complications |
10,191 (34) | 19,197 (31) | 3,147 (41) | 9,782 (29) | 19,555 (44) | 32,369 (44) |
| Obesity | 2,570 (9) | 3,554 (6) | 1,274 (16) | 2,926 (9) | 5,384 (12) | 8,823 (12) |
| Chronic pulmonary disease |
19,978 (67) | 28,711 (46) | -- | -- | 22,922 (52) | 23,548 (32) |
| Renal failure | 7,270 (24) | 13,001 (21) | 1,853 (24) | 3,981 (12) | 19,027 (43) | 33,007 (45) |
| Fluid and electrolyte disorders |
11,197 (38) | 24,535 (40) | 2,183 (28) | 8,261 (25) | 14,806 (33) | 21,071 (29) |
| Deficiency anemias |
9,528 (32) | 19,622 (32) | 1,982 (26) | 5,884 (18) | 16,220 (36) | 24,756 (34) |
| Liver disease | 158 (1) | 367 (1) | 32 (0) | 163 (0) | 238 (1) | 414 (1) |
| Depression | 3,884 (13) | 8,128 (13) | 1,050 (14) | 4,938 (15) | 4,757 (11) | 6,998 (10) |
Hospitalizations in all three cohorts frequently had secondary discharge diagnosis codes identifying other cardiopulmonary conditions that were potentially present as acute illnesses during hospitalization. Among diagnosed pneumonia hospitalizations, 46% and 31% had secondary diagnosis codes for COPD and HF, respectively. Among diagnosed COPD hospitalizations, 19% and 29% had secondary diagnosis codes for pneumonia and HF. Among diagnosed HF hospitalizations, 14% and 35% had secondary diagnosis codes for pneumonia and COPD.
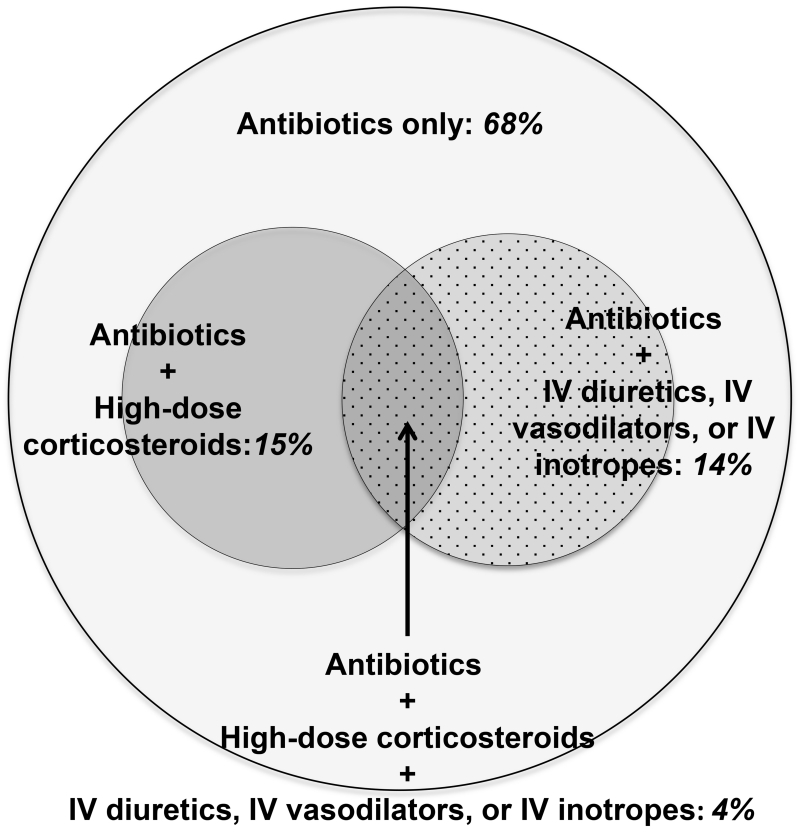
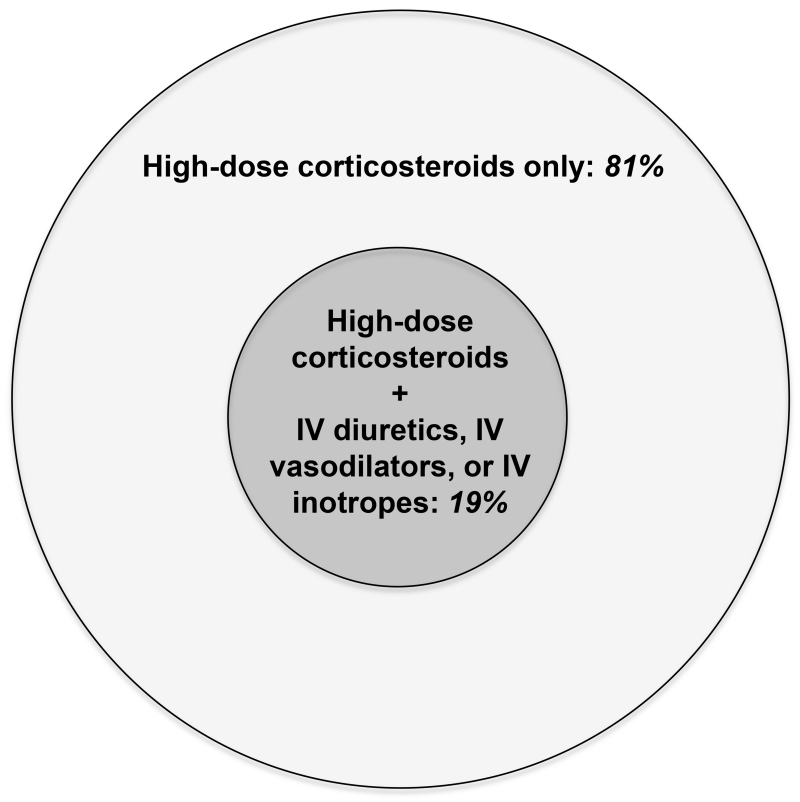
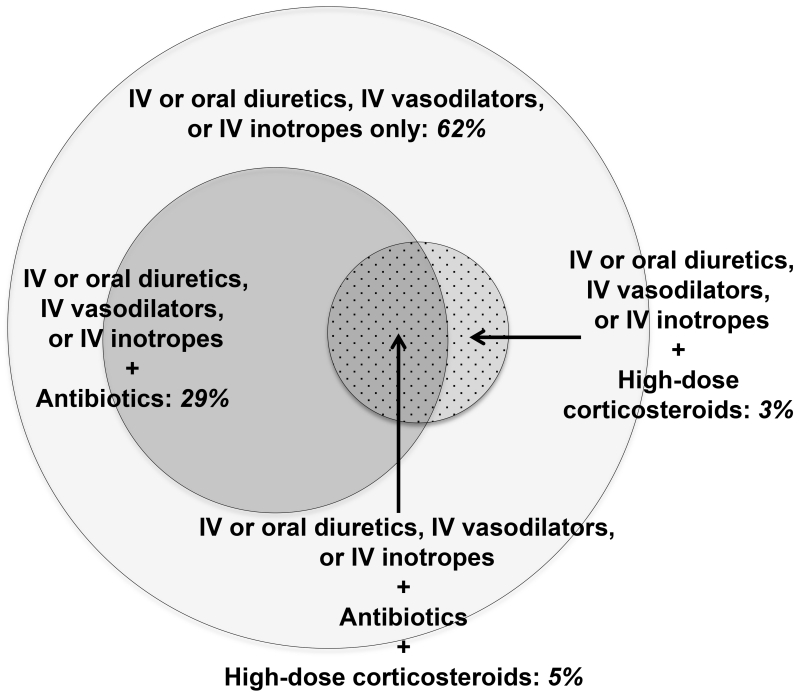
Concurrent treatment for two or more acute cardiopulmonary conditions was common across cohorts (Table 3). Among diagnosed pneumonia hospitalizations, 32% received concurrent treatment (18% received treatment for HF, 18% received treatment for COPD, and 4% received treatment for both HF and COPD). Among diagnosed COPD hospitalizations, 19% received concurrent treatment (all of which involved additional HF treatment). Among diagnosed HF hospitalizations, 38% received concurrent treatment (34% received treatment for pneumonia, 9% received treatment for COPD, and 5% received treatment for both pneumonia and COPD). The overlap of treatment groups in each study cohort is shown in Figure 1.
Table 3. Concurrent Treatments for Two or More Acute Cardiopulmonary Conditions Received by Pneumonia, Chronic Obstructive Pulmonary Disease, and Heart Failure Cohorts.
| Pneumonia cohort (91,709 hospitalizations) N (%) |
Chronic obstructive pulmonary disease cohort (41,052 hospitalizations) N (%) |
Heart failure cohort (118,061 hospitalizations) N (%) |
|
|---|---|---|---|
| Any concurrent treatment | 29,768 (32) | 7,759 (19) | 44,505 (38) |
| Antibiotics | N/A | N/A | 40,457 (34) |
| Corticosteroids | 16,959 (18) | N/A | 10,380 (9) |
|
Intravenous diuretics,
Intravenous vasodilators or Intravenous positive inotropes |
16,404 (18) | 7,759 (19) | N/A |
Figure 1. Concurrent Treatments for Two or More Acute Cardiopulmonary Conditions Received by Pneumonia, Chronic Obstructive Pulmonary Disease, and Heart Failure Cohorts.
Data is shown for pneumonia, chronic obstructive pulmonary disease (COPD), and heart failure cohorts in panels A, B, and C, respectively. Concurrent treatment for pneumonia cannot be determined during hospitalization for COPD, as antibiotic treatment is part of guideline-recommended therapy for COPD. Figure is drawn to scale. COPD: chronic obstructive pulmonary disease; IV: intravenous.
Concurrent treatment was also present among diagnosed pneumonia, COPD, and HF hospitalizations without a secondary diagnosis code for the other two cardiopulmonary conditions. Among pneumonia hospitalizations without secondary diagnosis codes for COPD or HF, 17% received concurrent treatment for two or more acute cardiopulmonary conditions. Among COPD hospitalizations without secondary diagnosis codes for pneumonia or HF, 9% received concurrent treatment. Among HF hospitalizations without secondary diagnosis codes for pneumonia or COPD, 24% received concurrent treatment.
Concurrent treatment was higher among hospitalizations in which the principal admission diagnosis differed from the principal discharge diagnosis compared with hospitalizations in which the principal admission and discharge diagnoses were the same. Among 71,253 hospitalizations with both a documented principal admission diagnosis and a principal discharge diagnosis of pneumonia, the rate of concurrent treatment was 29.2% if the principal admission diagnosis was pneumonia and 35.4% if the principal admission diagnosis was not pneumonia. Among 31,866 hospitalizations with both a documented principal admission diagnosis and a principal discharge diagnosis of COPD, the rate of concurrent treatment was 15.7% if the principal admission diagnosis was COPD and 21.7% if the principal admission diagnosis was not COPD. Among 90,225 hospitalizations with both a documented principal admission diagnosis and a principal discharge diagnosis of HF, the rate of concurrent treatment was 32.7% if the principal admission diagnosis was HF and 42.9% if the principal admission diagnosis was not HF.
Patients concurrently treated for two or more acute cardiopulmonary conditions were substantially more likely to experience adverse outcomes. Among hospitalizations for diagnosed pneumonia, observed rates of ICU admission, late intubation, and in-hospital death were respectively 19%, 6%, and 7% among patients receiving concurrent treatment and 9%, 3%, and 3% among patients treated just for pneumonia. Among hospitalizations for diagnosed COPD, observed rates of ICU admission, late intubation, and in-hospital death were respectively 15%, 6%, and 4% among patients receiving concurrent treatment and 7%, 3%, and 2% among patients treated just for COPD. Among hospitalizations for diagnosed HF, observed rates of ICU admission, late intubation, and in-hospital death were respectively 20%, 4%, and 4% among patients receiving concurrent treatment and 13%, 2%, and 3% among patients treated just for HF (p<0.001 for all).
The adjusted odds of adverse outcomes were between 60% and 138% higher among patients receiving concurrent treatment in pneumonia, COPD, and HF cohorts (Table 4). For example, among patients hospitalized for diagnosed pneumonia, concurrent treatment was associated with a 133% (odds ratio [OR] = 2.33, 95% confidence interval [CI] = 2.23-2.43) greater odds of ICU admission, 124% (OR = 2.24, 95% CI = 2.09-2.39) greater odds of late intubation, and 138% (OR = 2.38, 95% CI = 2.22-2.54) greater odds of in-hospital death.
Table 4. Adjusted In-hospital Outcomes among Hospitalizations Receiving Concurrent Treatment for Two or More Acute Cardiopulmonary Conditions in Pneumonia, Chronic Obstructive Pulmonary Disease, and Heart Failure Cohorts.
| Pneumonia cohort (91,709 hospitalizations) Odds ratio with concurrent treatment (95% CI) |
Chronic obstructive pulmonary disease cohort (41,052 hospitalizations) Odds ratio with concurrent treatment (95% CI) |
Heart failure cohort (118,061 hospitalizations) Odds ratio with concurrent treatment (95% CI) |
|
|---|---|---|---|
| Intensive care unit admission | 2.33 (2.23, 2.43) | 2.27 (2.10, 2.46) | 1.61 (1.55, 1.66) |
| Late intubation | 2.24 (2.09, 2.39) | 2.10 (1.87, 2.36) | 1.60 (1.50, 1.71) |
| In-hospital mortality | 2.38 (2.22, 2.54) | 2.09 (1.81, 2.42) | 1.61 (1.49, 1.73) |
Models were adjusted for age (categorized as 65 to <75 years, 75 to <85 years, 85+ years), sex, peripheral vascular disease, hypertension, diabetes, obesity, chronic pulmonary disease, renal failure, fluid and electrolyte disorders, deficiency anemias, liver disease, depression, and treatment for two or more acute cardiopulmonary conditions. For analyses of mortality, we randomly selected one hospitalization per patient (Pneumonia N=83,964; COPD N=33,864; Heart failure N=92,910).
DISCUSSION
Through study of a database containing approximately one-fifth of all acute care hospitalizations in the United States, we found that older patients hospitalized with the principal diagnoses of pneumonia, COPD, or HF regularly receive concurrent treatment for two or more of these acute cardiopulmonary conditions. This high frequency of treatment for multiple acute illnesses in the typical care of hospitalized older adults reveals shortcomings with our prevailing use of disease definitions and treatment pathways that consider clinical presentation, diagnosis, and treatment from the perspective of a single distinct condition.35 Our findings also suggest that many older adults hospitalized with the most common clinical syndromes have disease presentations that fall between traditional diagnostic categories. These people have rarely been studied in clinical trials, which overwhelmingly test interventions among patients with narrow and well-defined phenotypes. A new research agenda is therefore needed that evaluates the risks and benefits of real-world treatment strategies for the many patients whose presentations elicit diagnostic uncertainty or concern for coexisting acute conditions, the treatment of which may produce conflicting results.
Despite the frequency of concurrent treatment of two or more acute conditions and the complex clinical syndromes motivating these strategies, neither have been major foci of investigation. With over 550,000 yearly hospitalizations for pneumonia, 450,000 yearly hospitalizations for COPD, and 650,000 yearly hospitalizations for HF among older persons in the US alone,36 we estimate that over half a million elderly Americans receive treatment for multiple acute cardiopulmonary conditions during hospitalization. Yet data from large disease-specific registries37 and other observational studies38-41 have not demonstrated these typical practice patterns across conditions, as they have focused on reporting treatments for singular diseases. Analogously, major clinical trials of hospitalized patients have described only a limited breadth of the broad range of treatments likely received by enrolled subjects.7-10 Studies have overwhelmingly focused on patients with conditions that are distinct and singular rather than fuzzy and multiple.
As a result, little high quality data exist to guide everyday treatment decisions for patients who do not have one distinct illness. For example, little is known about the potential benefits and harms of concurrent treatment in cases of diagnostic uncertainty. Yet this is a common scenario when caring for complex elderly patients. Similarly, little is known about the comparative effectiveness of complex therapeutic strategies involving multiple medications. Only recently has the treatment of acute illness in the setting of chronic disease become a research priority.42 At a more basic level, the medical literature is largely silent on patients presenting with non-traditional clinical syndromes. Who are these patients, and how large is this group? What complex phenotypes are most common and consequential for outcomes? Can we reliably diagnose these patients? What are the consequences for reimbursement and quality measurement of labeling them with one principal discharge diagnosis? And what is even meant by “acute” illness when complex syndromes resulting in hospitalization often arise from the exacerbation of background diseases? These understandings are particularly important for elderly persons who frequently have multiple chronic conditions,11,24 geriatric syndromes,43 and non-specific findings at presentation.44
The motivations for broad approaches to treatment are likely diverse. It may be that hospitalized older patients often have multiple, distinct, acute conditions. In support of this hypothesis, we found that older patients hospitalized with pneumonia, COPD, or HF often had secondary diagnosis codes for the other cardiopulmonary conditions, some of which may be present as concurrent acute illnesses. Previous literature on patients hospitalized with myocardial infarction has shown that up to 20 percent have co-existing non-cardiac conditions such as pneumonia, gastrointestinal bleeding, and sepsis at admission.17,45 Research has also shown that pneumonia can trigger decompensated HF, arrhythmia, and acute coronary syndromes.18,19,46 It is also possible that concurrent treatment results from diagnostic uncertainty. In support of this perspective, we found that rates of concurrent treatment were higher when the principal admission diagnosis differed from the principal discharge diagnosis. It would not be surprising if diagnostic uncertainty is common in real world practice, as shortness of breath is common to many cardiac and pulmonary conditions, and no pathognomonic findings or diagnostic tests consistently differentiate them from one another.20,47
The markedly higher rate of adverse outcomes among patients treated for two or more acute cardiopulmonary syndromes likely relates to multiple factors including poorer chronic health, higher illness acuity, concurrent illnesses, or adverse effects from the treatments themselves. In support of these hypotheses, we found patients receiving concurrent treatment to be more complex with more chronic conditions than patients receiving treatment only for their principal diagnosis. Similarly, we found that concurrently treated patients often have secondary discharge diagnoses for other cardiopulmonary conditions, suggesting that concurrent acute illnesses were present at times. There is also theoretical concern about adverse drug effects, as all studied drug classes including loop diuretics,48 antibiotics,49 and corticosteroids50 can cause direct harms to older persons and may work at cross-purposes. For example, loop diuretics and corticosteroids may have opposing effects on sodium excretion.
The many outstanding questions suggest that researchers and funders develop a dedicated research agenda to better understand and treat older patients without a single distinct condition on admission to the hospital. Initial work should prospectively examine older patients hospitalized with common symptoms such as shortness of breath or delirium to better understand how often their histories, physical examination findings, and initial testing results suggest uncertainty in diagnosis or multiple concomitant illnesses. Follow-up studies should examine how clinicians process this data to assign diagnoses and make treatment decisions, especially in settings of diagnostic uncertainty. Ultimately, comparative effectiveness studies using large databases of electronic health records can be used to examine the benefits and harms of different treatment combinations. These studies may require natural language processing and advanced statistical methods to identify patients without stereotypical presentations and create comparable populations to examine differences in outcomes by treatment.
Findings should be interpreted in the context of the following limitations. We could not ascertain reasons for concurrent treatment, the assessment of which will require more detailed clinical information including further descriptions of chronic health status and illness acuity at hospital presentation. In addition, we could not determine if the use of multiple treatments directly contributed to adverse patient outcomes or was simply associated with administration to sicker patients. Finally, we may have misclassified some patients due to our use of administrative data to identify patients with pneumonia, COPD, and HF. However, as we found that treatments are multiple and extend across disease-specific boundaries regardless of diagnosis, our conclusions would not change if patients moved among study cohorts.
We found that older patients hospitalized with the principal diagnoses of pneumonia, COPD, or HF are regularly treated for two or more of these acute cardiopulmonary conditions. These findings indicate that disease presentation and treatment are often more expansive than specialists, textbooks, and disease-focused research have acknowledged. Researchers and funders must help close this gap between typical clinical practice and traditional teaching through studies and eventual practice guidelines that better account for the complexities of disease presentation in older adults, including the presence of concurrent acute illnesses, as well as the potential benefits and harms of different treatment strategies in settings of diagnostic uncertainty. With the ultimate goal of precision medicine, the resulting knowledge will help tailor complex treatment regimens to the large and poorly studied group of hospitalized older patients with indistinct clinical syndromes and multiple acute conditions.
ACKNOWLEDGMENTS
Funding sources: This project was supported by grant DF10-301 from the Patrick and Catherine Weldon Donaghue Medical Research Foundation in West Hartford, CT; grant UL1 RR024139-06S1 from the National Center for Advancing Translational Sciences in Bethesda, MD; and a John A. Hartford Foundation Center of Excellence Career Development Award to Dr. Dharmarajan through Yale University. Dr. Dharmarajan is additionally supported by grant K23AG048331-02 from the National Institute on Aging and the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. Dr. Lagu is supported by grant K01HL114745-03 from the National Heart, Lung, and Blood Institute. Dr. Krumholz is supported by grant 1U01HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not represent the official views of the Patrick and Catherine Weldon Donaghue Medical Research Foundation, National Center for Advancing Translational Sciences, John A. Hartford Foundation, National Institute on Aging, American Federation for Aging Research, or National Heart, Lung, and Blood Institute.
Sponsor’s role: The sponsors had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; in the preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Footnotes
Prior Presentation: These data were presented in part at the Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke Scientific Sessions of the American Heart Association; May 15-17, 2013; Baltimore, Maryland.
Conflict of interest: Dr. Dharmarajan is a member of a scientific advisory board for Clover Health. Dr. Dharmarajan, Ms. Strait, Dr. Lindenauer, and Dr. Krumholz work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Krumholz is the chair of a cardiac scientific advisory board for UnitedHealth. Dr. Krumholz is the recipient of research grants from Medtronic and Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing.
1. Kumar Dharmarajan: Employment or affiliation: works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: member of a scientific advisory board for Clover Health; Patents: no; Personal relationship: no
2. Kelly M. Strait: Employment or affiliation: works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
3. Mary E. Tinetti: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
4. Tara Lagu: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
5. Peter K. Lindenauer: Employment or affiliation: works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
6. Joanne Lynn: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
7. Michelle R. Krukas: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
8. Frank R. Ernst: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
9. Shu-Xia Li: Employment or affiliation: no; Grants/funds: no; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: no; Patents: no; Personal relationship: no
10. Harlan M. Krumholz: Employment or affiliation: works under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures; Grants/funds: recipient of research grants from Medtronic and Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing; Honoraria: no; Speaker forum: no; Consultant: no; Stocks: no; Royalties: no; Expert testimony: no; Board member: chair of a cardiac scientific advisory board for UnitedHealth; Patents: no; Personal relationship: no
Authors’ contributions:
Study concept and design: Dharmarajan, Krumholz
Acquisition of data: Krumholz
Analysis and interpretation of data: Dharmarajan, Strait, Tinetti, Lagu, Lindenauer, Lynn, Krukas, Ernst, Li, Krumholz
Drafting of the manuscript: Dharmarajan
Critical revision of the manuscript for important intellectual content: Dharmarajan, Strait, Tinetti, Lagu, Lindenauer, Lynn, Krukas, Ernst, Li, Krumholz
Statistical analysis: Strait
Obtained funding: Dharmarajan, Krumholz
Administrative, technical, or material support: Krumholz
Study supervision: Krumholz
At the time this research was performed, Michelle R. Krukas and Frank R. Ernst were associated with Premier Research Services, Premier, Inc., Charlotte, NC.
REFERENCES
- 1.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease (GOLD) [Accessed February 27, 2015];Global strategy for the diagnosis, management and prevention of COPD. 2011 Available at: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Feb21.pdf.
- 3.Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: Developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 4.Donowitz GR. Acute pneumonia. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Churchill Livingstone Elsevier; Philadelphia, PA: 2010. pp. 891–916. [Google Scholar]
- 5.Shapiro SD, Reilly JJ, Rennard SI. Chronic bronchitis and emphysema. In: Mason RJ, Broaddus VC, Martin TR, et al., editors. Murray and Nadel’s Textbook of Respiratory Medicine. 5th ed. Saunders Elsevier; Philadelphia, PA: 2010. pp. 919–967. [Google Scholar]
- 6.Teerlink JR. Diagnosis and management of acute heart failure. In: Libby P, Bonow RO, Mann DL, Zipes DP, editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 8th ed. Saunders Elsevier; Philadelphia, PA: 2008. pp. 583–610. [Google Scholar]
- 7.File TM, Jr., Segreti J, Dunbar L, et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin versus ceftriaxone and/or cefuroxime axetil in treatment of adults with community-acquired pneumonia. Antimicrob Agents Chemother. 1997;41:1965–1972. doi: 10.1128/aac.41.9.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: A randomized trial. JAMA. 2003;290:2588–2598. doi: 10.1001/jama.290.19.2588. [DOI] [PubMed] [Google Scholar]
- 9.Niewoehner DE, Erbland ML, Deupree RH, et al. Department of Veterans Affairs Cooperative Study Group Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1999;340:1941–1947. doi: 10.1056/NEJM199906243402502. [DOI] [PubMed] [Google Scholar]
- 10.Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805. doi: 10.1056/NEJMoa1005419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition--multimorbidity. JAMA. 2012;307:2493–2494. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dharmarajan K, Strait KM, Lagu T, et al. Acute decompensated heart failure is routinely treated as a cardiopulmonary syndrome. PLoS One. 2013;8:e78222. doi: 10.1371/journal.pone.0078222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delerme S, Ray P. Acute respiratory failure in the elderly: Diagnosis and prognosis. Age Ageing. 2008;37:251–257. doi: 10.1093/ageing/afn060. [DOI] [PubMed] [Google Scholar]
- 14.Ray P, Birolleau S, Lefort Y, et al. Acute respiratory failure in the elderly: Etiology, emergency diagnosis and prognosis. Crit Care. 2006;10:R82. doi: 10.1186/cc4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barr RG, Bluemke DA, Ahmed FS, et al. Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med. 2010;362:217–227. doi: 10.1056/NEJMoa0808836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells JM, Washko GR, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367:913–921. doi: 10.1056/NEJMoa1203830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lichtman JH, Spertus JA, Reid KJ, et al. Acute noncardiac conditions and in-hospital mortality in patients with acute myocardial infarction. Circulation. 2007;116:1925–1930. doi: 10.1161/CIRCULATIONAHA.107.722090. [DOI] [PubMed] [Google Scholar]
- 18.Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: A systematic review and meta-analysis of observational studies. PLoS Med. 2011;8:e1001048. doi: 10.1371/journal.pmed.1001048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: Incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125:773–781. doi: 10.1161/CIRCULATIONAHA.111.040766. [DOI] [PubMed] [Google Scholar]
- 20.Hawkins NM, Petrie MC, Jhund PS, et al. Heart failure and chronic obstructive pulmonary disease: Diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009;11:130–139. doi: 10.1093/eurjhf/hfn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jorge S, Becquemin MH, Delerme S, et al. Cardiac asthma in elderly patients: Incidence, clinical presentation and outcome. BMC Cardiovasc Disord. 2007;7:16. doi: 10.1186/1471-2261-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services . Medicare Hospital Quality Chartbook 2013: Performance Report on Outcome Measures. Centers for Medicare & Medicaid Services; Washington, DC: 2013. [Google Scholar]
- 23.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 24.Guiding principles for the care of older adults with multimorbidity: An approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60:E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Emmett KR. Nonspecific and atypical presentation of disease in the older patient. Geriatrics. 1998;53:50–52. 58–60. [PubMed] [Google Scholar]
- 26.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–351. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Lindenauer PK, Normand SL, Drye EE, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6:142–150. doi: 10.1002/jhm.890. [DOI] [PubMed] [Google Scholar]
- 28.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 29.Quan H, Li B, Saunders LD, et al. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441. doi: 10.1111/j.1475-6773.2007.00822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Birman-Deych E, Waterman AD, Yan Y, et al. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 31.Skull SA, Andrews RM, Byrnes GB, et al. ICD-10 codes are a valid tool for identification of pneumonia in hospitalized patients aged > or = 65 years. Epidemiol Infect. 2008;136:232–240. doi: 10.1017/S0950268807008564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lacasse Y, Daigle JM, Martin S, et al. Validity of chronic obstructive pulmonary disease diagnoses in a large administrative database. Can Respir J. 2012;19:e5–9. doi: 10.1155/2012/260374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lindenauer PK, Pekow PS, Lahti MC, et al. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303:2359–2367. doi: 10.1001/jama.2010.796. [DOI] [PubMed] [Google Scholar]
- 34.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. JAMA. 2005;294:716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 36.Agency for Healthcare Research and Quality [Accessed June 1, 2015];HCUPnet: national and regional estimates on hospital use for all patients from the HCUP National Inpatient Sample (NIS) Available at: http://www.hcupnet.ahrq.gov/HCUPnet.jsp.
- 37.Yancy CW, Lopatin M, Stevenson LW, et al. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: A report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol. 2006;47:76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 38.Kollef MH, Shorr A, Tabak YP, et al. Epidemiology and outcomes of health-care-associated pneumonia: Results from a large US database of culture-positive pneumonia. Chest. 2005;128:3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 39.Fry AM, Shay DK, Holman RC, et al. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. 2005;294:2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 40.Jasti H, Mortensen EM, Obrosky DS, et al. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis. 2008;46:550–556. doi: 10.1086/526526. [DOI] [PubMed] [Google Scholar]
- 41.Almagro P, Cabrera FJ, Diez J, et al. Comorbidities and short-term prognosis in patients hospitalized for acute exacerbation of COPD: The EPOC en Servicios de medicina interna (ESMI) study. Chest. 2012;142:1126–1133. doi: 10.1378/chest.11-2413. [DOI] [PubMed] [Google Scholar]
- 42.Arnett DK, Goodman RA, Halperin JL, et al. AHA/ACC/HHS strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions: From the American Heart Association, American College of Cardiology, and US Department of Health and Human Services. Circulation. 2014;130:1662–1667. doi: 10.1161/CIR.0000000000000128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55:780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jarrett PG, Rockwood K, Carver D, et al. Illness presentation in elderly patients. Arch Intern Med. 1995;155:1060–1064. [PubMed] [Google Scholar]
- 45.Lichtman JH, Fathi A, Radford MJ, et al. Acute, severe noncardiac conditions in patients with acute myocardial infarction. Am J Med. 2006;119:843–850. doi: 10.1016/j.amjmed.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 46.Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264–274. doi: 10.1001/jama.2014.18229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Le Jemtel TH, Padeletti M, Jelic S. Diagnostic and therapeutic challenges in patients with coexistent chronic obstructive pulmonary disease and chronic heart failure. J Am Coll Cardiol. 2007;49:171–180. doi: 10.1016/j.jacc.2006.08.046. [DOI] [PubMed] [Google Scholar]
- 48.Cleland JG, Coletta A, Witte K. Practical applications of intravenous diuretic therapy in decompensated heart failure. Am J Med. 2006;119:S26–36. doi: 10.1016/j.amjmed.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 49.Gleckman RA. Antibiotic concerns in the elderly. A clinician’s perspective. Infect Dis Clin North Am. 1995;9:575–590. [PubMed] [Google Scholar]
- 50.Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81:1361–1367. doi: 10.4065/81.10.1361. [DOI] [PubMed] [Google Scholar]