Abstract
HIV Self Tests (HIVST) have the potential to increase testing among young adults. However, little is known about high-risk young adults‘ perception of the HIVST as a risk reduction tool and how they would use the HIVST in their everyday lives. Our study sought to examine these factors. Twenty-one ethnically diverse participants (ages 18–24) used the HIVST at our study site, completed surveys, and underwent an in-depth interview. Descriptive statistics were used to analyze the survey responses, and interview data were coded using constructs from the Information-Motivation-Behavioral skills model. Information deficits included: how to use the HIVST and the “window period” for sero-conversion. Motivations supporting HIVST use included: not needing to visit the clinic, fast results, easy access, and use in non-monogamous relationships. Behavioral skills discussed included: coping with a positive test, handling partner violence after a positive test, and accessing HIV services. These findings can inform the use of the HIVST for improving HIV testing rates and reducing HIV risk behavior.
Keywords: HIV Self Tests, Prevention, Information-Motivation-Behavioral skills (IMB), IMB model, High-Risk, Youth
INTRODUCTION
In the United States (US), the HIV epidemic disproportionately affects racial, ethnic and sexual minority populations, especially in their youth. Youth and young adults make up a greater number of newly HIV-infected individuals in the US versus their older counterparts (1). Among those aged 13 to 24, 75% of infections occur in men who have sex with men (MSM) (2). Of the nearly 21,000 infections estimated to occur each year among African Americans, 34% are among young people aged 13 to 24 (3). Latino youth continue to experience an increase in the rate of diagnoses of HIV and account for approximately 20% of new HIV diagnoses among youth aged 13 to 24 (4).
HIV-infected youth are less likely than HIV-infected adults to be aware of their status, particularly those at high-risk for acquiring HIV such as MSM, African Americans and Latinos (5). Despite reports that youth know where to get an HIV test, testing rates among youth remain low. The CDC estimated that in 2010, about 50% of youth aged 13 to 24 with HIV in the United States were unaware of their infection, compared to 12.8% in the overall population. In the same year, only 35% of young adults aged 18 to 24 had been tested for HIV. Nationwide, only 12.9% of high school students had ever been tested for HIV (6). Studies have shown that 50% to 60% of young HIV-infected MSM aged 18 to 24 are unaware of their infection (7). Lack of HIV testing contributes to this unawareness. Although the CDC recommends testing for HIV every 12 months for persons at high-risk for infection, over 35% of young MSM have not been tested in the past year (8). All of these populations remain at high-risk for acquiring HIV, and knowing their HIV status is fundamental to linking them to care and secondary prevention (9).
When properly used, HIV testing can be a gateway to treatment, care, and prevention (5). Specifically, the HIV Self-Test (HIVST) has been publicized for its potential to improve the identification of those who do not know they are infected by increasing access to HIV testing (10, 11). In 2012, the FDA approved the first rapid HIVST (OraQuick test, OraSure Technologies, Bethlehem, PA), allowing an individual to find out his/her HIV status in as short as twenty minutes without the presence of a healthcare provider (12). The HIVST may be of particular relevance to racial, ethnic and sexual minority young adults who are most likely to be affected by the disease and least likely to be tested (13). However, we know very little about young adults‘ perceptions of the HIVST and their behavioral intention to use the test. The potential uses of this technology by youth need to be better understood in order to develop and promote programs that eliminate the current disparity in HIV detection and incidence among high-risk youth and young adults.
The goal of this study was to understand young adults‘ perceptions of the use of the HIVST as a screening and behavioral intervention tool. Towards this goal, we sought to: understand young adults‘ knowledge of HIV and the HIVST, elicit their motivations for using HIVST, and identify behavioral intentions to use the HIVST as a prevention strategy.
METHODS
Theoretical Framework
Our study was guided by the Information-Motivation-Behavioral skills (IMB) model, a conceptual model developed to guide thinking about complex health behaviors. The IMB model hypothesizes that if a person is provided adequate information, motivation, and behavioral skills and has the self-efficacy to act, then there is an increased likelihood that they will fulfill and maintain healthful behaviors and achieve the desired outcome. The IMB model has been used to guide health behavior intervention development by eliciting targeted end-users‘ information, motivation, and behavioral skills through the use of questionnaires, surveys, or other methods (14). Behavior-specific and group-specific interventions can then be designed to achieve behavioral goals. Finally, evaluation-outcome research can assess whether the intervention produced the desired effect on remediating information, motivation, and behavioral skill deficits that are likely causes of the original faulty health behavior (14–16).
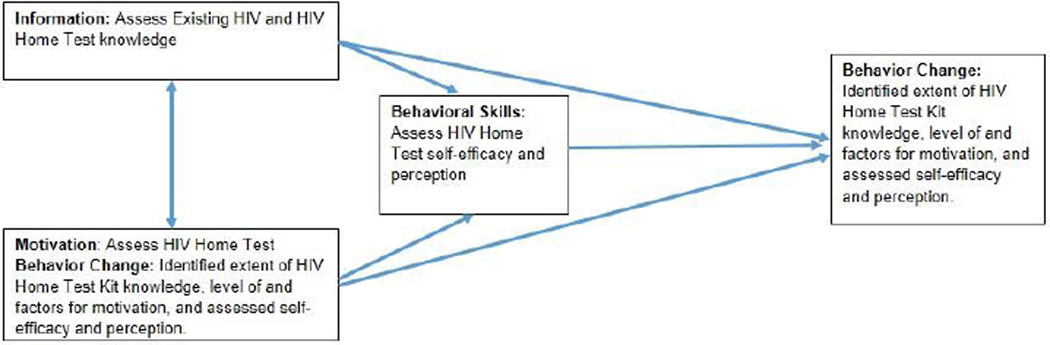
The goal of our research was to examine young adults‘ use of the HIVST, which included knowledge, motivation, and efficacy to execute distinct behaviors. To achieve this goal, data collection instruments were identified specifically for each construct of the IMB model. Mixed methods analyses of surveys and in-depth qualitative interviews were used. We collected demographics, HIVST information, HIV knowledge, attitudes, self-efficacy, and intentions to use the HIVST. The IMB constructs (i.e., information, motivation, behavioral skills), and how they were operationalized in our study is illustrated in Figure 1. We adapted instruments from their original tools to specifically measure perceptions related to HIVST use. All original scales were chosen for their core generalizability and malleability so that the original terms and concepts (i.e., smoking and condoms) could be replaced by and measure “HIV Self Tests”. Measurement tools are described in Table 1.
Figure 1.
IMB Constructs Tied to Study Activities
Table 1.
Questionnaire modeled to the IMB model
| Construct | Instrument | Description | Mean (S.D.) | Scale |
|---|---|---|---|---|
| Information | HIV-Knowledge Questionnaire – HIV-KQ-18 (17) | Measures knowledge about HIV disease and how it is transmitted | 13.22 (2.56) | Min: 0 Max: 18 |
| HIVST Information Scale (18) | Assesses understanding of the limitations of the test | 10.67 (4.69) | Min: 0 Max: 18 |
|
| Motivation | Peer Influence and Perceived Social Norms (19, 20) | Assesses the importance of approval of adolescent and family referents for HIVST use | Brother and Sister: 4.19 (0.87) | Min: 1 (Strongly Discouraging) Max: 5 (Strongly Encouraging) |
| Mother: 4.14 (0.96) | ||||
| Father: 4.10 (1.09) | ||||
| Recent sex partner: 4.00 (1.0) | ||||
| Other friends: 3.76 (1.04) | ||||
| Intention to use HIVST Scale (21) | Assesses intent and willingness to use HIVST | Use HIVST to test themselves: 3.43 (0.81) | Min: 1 (Very Unlikely) Max: 4 (Very Likely) |
|
| Use HIVST to test a sexual partner: 3.33 (0.97) | ||||
| Perceived susceptibility (22) | Assesses feelings of vulnerability or susceptibility to HIV | 1.71 (0.845) | Min: 1 (Strongly Disagree) Max: 4 (Strongly Agree) |
|
| HIV-Antibody Testing Attitude Scale (HTAS) (23) | Measures attitudes about HIV testing | 3.97 (0.431) | Min: 1 (Strongly Disagree) Max: 5 (Strongly Agree) |
|
| Behavioral Skills | HIVST Self-Efficacy Adapted from (24) | Measures self-efficacy for use of HIVST | Use the HIVST correctly: 4.29 (0.72) | Min: 1 (Very Unsure) Max: 5 (Very Sure) |
| Understand the results of the HIVST: 4.44 (0.63) | ||||
| Talk about using the HIVST with any sexual partner: 4.24 (0.77) | ||||
| Talk about using the HIVST if they were unsure of their partner's feelings about it: 4.00 (1.05) | ||||
| Say no to sex if their partner refused to take an HIV test: 4.19 (1.21) | ||||
| Talk about using the HIVST with a potential sexual partner before they started to hug and kiss: 3.14 (1.24) | ||||
| Talk a partner into taking an HIVST before they have sexual intercourse: 3.62 (1.43) | ||||
| Perceived Effectiveness and Difficulty of Discussing the HIV Test with Partners (25) Adapted from (26) | Measures perceived ability to discuss HIVST results with partners | Keep a supply of HIVST in their home: 1.71, (0.85) | Min: 1 (Very Easy to Do) Max: 4 (Very Hard to Do) |
|
| Easy to carry HIVST when going out: 2.00 (1.05) | ||||
| Raising the idea of using HIVST with a partner: 1.52 (0.68) | ||||
| Ask a partner to take HIVST: 1.45 (0.61) | ||||
| Showing a partner how to use HIVST: 1.43 (0.60) | ||||
| Use HIVST when partner is under the influence of alcohol or drugs: 2.33, (1.07) | ||||
| Use HIVST with a partner when they are under the influence of alcohol or drugs: 2.10, (1.17) | ||||
| Avoid receptive anal intercourse with a partner who refuses to take HIVST: 1.71, (0.78) | ||||
| Avoid insertive anal intercourse with a partner who refuses to take HIVST: 1.70 (0.73) | ||||
| Handle a violent situation that occurred as a result of using or proposing to use a HIVST: 1.90 (0.85) |
Study Procedures
Procedures
The study took place from January to June of 2014. We secured approval from the Columbia University Medical Center Institutional Review Board and obtained a Certificate of Confidentiality from the National Institutes of Health. We recruited participants by posting fliers in bars, dance clubs, community events and community-based organizations where young adults congregate. Participants were recruited through purposive sampling. Inclusion criteria were: ability to speak English or Spanish, HIV-negative or unknown status, unprotected vaginal or anal intercourse (receptive or insertive) in the prior year with a partner of unknown or discordant HIV status, and willing to take an HIV test at our study site.
All study activities were conducted in a private study room at the Columbia Community Partnership for Health. Participants completed a written informed consent form. Following the consent process, we used a think-aloud protocol, video observations, questionnaires, and in-depth interviews to examine study participants‘ use of the HIVST. Results from the think-aloud protocol are reported in “Do High-Risk Young Adults Use the HIV Home Test Appropriately?” (27)
Participants were asked to use the OraQuick Rapid HIV 1&2 home test (12) in the presence of a research team member. OraQuick is an antibody test that involves self-collection of a mouth swab and testing an oral fluid sample for HIV antibodies. The test gives results in 20 to 40 minutes, comes with step-by-step instructions on how to perform it at home, is 99% accurate, and is FDA-approved. Once the participant indicated that s/he had completed the HIVST procedures, the study team member asked the participant for his/her interpretation of the results. Following the procedures, participants completed surveys (Table 1) through Qualtrics, a secure, web-based application designed to support data capture for research studies.
Participants were interviewed after they used the HIVST and completed all of the questionnaires. The interviewer was a Latina who had a master‘s degree in public health and a medical degree from a foreign university. She received training from the research team members in how to conduct interviews and focus groups, and coded qualitative data as part of her work on multiple federally funded research projects. The interview consisted of a series of open-ended questions designed to understand their experiences using the test. Interview questions were developed based on the three constructs of the IMB model (i.e., information, motivation, and behavioral skills) with the goal of unearthing participant HIV testing proficiencies within the specified construct. Questions related to the “Information” construct provided an indication of participants‘ basic knowledge about HIV, HIV Self Testing, and other strategies for positive and healthful behaviors. Questions for the “Motivation” construct discussed and assessed personal attitudes towards HIV, HIV testing, use of HIVST, perceived social support from partner or family and friends, and the participants' subjective norms or perception of others‘ HIV testing and HIVST use. Lastly, questions for the “Behavioral Skills” construct provided an understanding of the specific behavioral tools or strategies needed to perform positive and healthful behaviors, such as increased testing for HIV, enlisting social support, and strategies for healthful self-regulation.
Participant Description
We interviewed twenty-one minority young adults aged 18 to 24 (M = 21.25, S.D. = 1.49) who reported having had one or more unprotected sexual encounters with a partner of unknown HIV status. Sixteen participants reported being male, 3 reported being female, 1 reported being transgeder male, 1 reported being transgender female and 2 reported being gender-queer. Eighty-six percent (N =18) of our participants had a history of anal intercourse. Nine participants reported being Black/ African American, 1 was Asian, 1 was American Indian/ Alaska Native and 10 were of Latino/ Hispanic origin. Almost all of our participants (N =19) spoke English; one participant spoke Spanish and one used American Sign Language to communicate.
Analysis
Three research staff members administered quantitative surveys via Qualtrics and conducted qualitative in-depth interviews during one-on-one sessions. Quantitative data were analyzed using descriptive statistics with SPSS. The qualitative data was manually coded using word review and annotation tools by two doctorally prepared researchers. Coded excerpts were then extracted from the word document and organized into an excel database. Codes and related excerpts were reviewed by a second rater, and final codes and related excerpts were agreed upon by both raters.
RESULTS
Table 1 presents a summary of the quantitative results, and is followed by relevant excerpts from interview data. Results are organized by the IMB constructs.
Information
Information and Standard HIV Testing
Our findings about knowledge of HIV testing support common findings that most youth know about HIV testing, where to get tested, and have been tested at least once in their life, but don‘t get tested frequently enough due to misperceptions of risk and barriers such as social stigma and economic limitations (28). We used 2 questionnaires to measures knowledge and each had a scale of 0 (none correct) to 18 (perfect score). On the HIV-Knowledge Questionnaire, participants had a mean score of 13.22 (S.D. 2.56). On the HIVST Information Scale, participants had a mean score of 10.67 (S.D. 4.69). All participants had some knowledge of HIV testing, including where to get tested and generally what testing would involve (See Table 1, Instrument: HIV-Knowledge Questionnaire – HIV-KQ-18).
Preknowledge of the HIVST
In the quantitative assessment, participants demonstrated an average level of knowledge about HIV, but a below average understanding of the HIVST and its limitations (See Table 1, Instrument: HIVST Information Scale). Similar to the findings in the quantitative assessment, during interviews most participants reported not having any prior knowledge of the HIVST before participating in the study. Many expressed surprise about the availability of an HIV test for use outside of a clinical setting. Others were surprised that they didn‘t have to take a blood test. When asked if they had heard about the rapid HIVST recently approved by the FDA, typical responses included:
“No I haven't. And most of them are drawing blood. So I thought it would be that one.”
---- ----
“Actually, no, I haven‘t. I didn‘t know they sell this at home. I thought you‘d have to go find a van or go into little clinics and be like I need to get an HIV test, which is really weird because you don‘t know who is listening.”
Some participants expressed knowledge of the HIVST before participating in our study. They had heard about it from TV or other forms of media (social media, magazine, etc.), had some professional involvement in HIV prevention or health care, or were informed by a healthcare provider.
“I work in HIV prevention…I knew you could, but did not have knowledge of it until after I came…about a month or so after I did my first test, an organization came in and was expressing the benefits and I guess the necessity of wanting to take your own HIV test.”
---- ----
“I‘ve seen a commercial, but I didn‘t think it was real because I didn‘t…I was thinking that you had to report it, like whether you‘re positive or negative. I was thinking, how is that going to be done if you‘re at home because somebody could just throw it away. So, I didn‘t think it was really out there. Once I saw the commercial, I just browsed on the internet, but it was like $60, so I was like I wouldn‘t ever have one of those.”
---- ----
“I only heard that it was new, rather, but I never really knew where to buy it from or if I can buy it right now. All I know is that there was possibly an HIV home test…Around, people talk about it. I could have possibly saw it in newspapers. I'm not sure if I read about it or not. But I did know that it was coming out.”
Motivation
Motivation and Standard HIV testing
Peer influence and perceived social norms have been identified as highly influential factors that motivate people to get tested for HIV, along with a history of sexually transmitted infection and risk awareness (8, 28). Our findings on youths‘ motivations to use the HIVST confirm existing research.
Peer Influence and Perceived Social Norms in HIVST Use
Approval of peer, intimate partner, and family referents for HIVST use was an important motivating factor. Overall, participants reported that those who they most closely interacted with would support their use of the HIVST. The majority of participants reported that all of the following categories of people would encourage them to use the HIVST: mother (76.5%), best friend (70.6%), most recent sex partner (70.6%), father (64.7%), siblings (64.7%), and other friends (58.9%). (See Table 1, Instrument: Peer Influence and Perceived Social Norms).
Intention To Use HIVSTs
Most participants said they would definitely use the HIVST kit (57.1%) or that it was likely (33.3%). Similarly, most participants responded that they would definitely use HIVST to test any sexual partners (57.1%) or with intimate partners (28.6%) (See Table 1, Instrument: Intention to use HIVST Scale). Additionally, when asked how much they would be willing to spend to purchase an HIVST in their interview, most participants indicated they wouldn‘t spend more than $20. This highlighted the importance of cost as a barrier or facilitator of HIVST use, and clarified that motivation to use the HIVST may be mitigated by cost.
R: It depends on the cost, and I feel like it should be free instead of charging anybody because there‘s a better way to protect a lot of people from…who is very private, who don‘t want to go to the doctors, that they can get some kind of knowledge of it. So, I feel like it should be free for everyone.
M: Let‘s say it costs $50, would that be a problem?
R: Yes.
M: What do you think would be normal?
R: Like $10, $15, or probably lower because I feel like it‘s too much to pay $50 to get a rapid test. I could go to the doctor free and get blood work free.”
---- ----
M: And what should be the cost of this?
R: I would go in the range between $5 and $8, around there. You pay like $7.75 and you get an AIDS test.
M: So $50 would be?
R: That‘s too much. Fifty dollars, I don‘t think anybody… Well some people would do it. But then again, that goes to disadvantage to people that can‘t afford to pay $50 for it. You know what I mean? I think, like with the pregnancy test, to have dollar ones, two, three dollars. I think it would be most prominent for them to put it at a low number than a higher number. So it enables, it puts it out to more people. More people have the access to it, you know.
Based on our findings, participants did not report susceptibly to HIV. Low perceived susceptibility to HIV may be associated with low testing rates in general (See Table 1, Instrument: Perceived susceptibility). However, attitudes towards HIV-antibody testing were favorable among our participants (See Table 1, Instrument: HIV-Antibody Testing Attitude Scale (HTAS)).
Comparison of HIVST with Clinical Testing
A few participants raised concerns about the accuracy of the HIVST. Concerns focused on the perception that blood tests in clinics were more accurate than HIVST. Some participants said that they would prefer using the HIVST over going to a clinic or getting tested by a health care provider, since it was simple to use and faster than waiting for the test results from the health care provider. This would save them time and money because they wouldn‘t have to travel to a hospital or clinic.
M: …How did this test compare to other tests you‘ve had in the past, other HIV tests and other medical tests? Did you like it more, did you like it less, was it simpler, was it more complicated?
R: It was more simpler because usually when you do an intake with a counselor or a doctor, they ask you a lot of personal things and it‘s a lot of time being wasted. The Home rapid test, I know my sexual history, so I don‘t have to ask any questions. I can just perform the test and it‘s less time and it‘s at a place where I feel secure at.
M: What about the swabbing of the mouth? Is that better? Was that the same as the other tests you‘ve had in the past?
R: A couple of times I got tested when they would swab my gums. They usually would swab too rough sometimes. So, once again, for me this proves to be better, more beneficial because I know my body and I know what pressure to put on my gums.”
---- ----
M: So you like this way of testing, as opposed to getting pricks and taking blood.
R: I actually kind of like the blood a little bit better. I just feel like it‘s a little bit more accurate, but I wouldn‘t know. I'm not into that type of thing. So I don‘t know. I just think anything with blood is a little bit more accurate.
Facilitators
Participants highlighted several advantages of the HIVST, including ease of use, privacy, and speed.
“It‘s quick. You can do it anywhere. You have to just go by yourself and somewhere they have it, like a pharmacy. Just get it. It‘s quick. It‘s only a little swab. There‘s no blood even involved.”
---- ----
“It would have been a different experience just because I am in a secure place, my home, and I am not around people who I feel are going to breach my confidentiality. I really don‘t feel that comfortable around doctors and counselors, so just to be in my home, a place that I feel secure at and be able to take a test like this, it makes me feel good.”
Barriers
The participants also identified disadvantages to the HIVST, particularly cost and lack of immediate and direct contact with a medical professional in case of a positive diagnosis. Tied to this was a fear that others may resort to suicide in the event of a positive test result as well as violence by their intimate partner.
“Let‘s say a person is mentally ill…they suffer from depression or something…and they so happen to…happen to come up positive…they have nobody to talk to at that point in time. They can do anything. They can harm themselves. They can probably harm the people that they feel gave it to them or they can do harm to themselves, or both. They have no trained medical professional to guide them through their chaos, so I think that‘s one of the disadvantages.”
---- ----
“If the test comes back positive, it could get violent.”
Behavioral Skills
An Adolescent and Young Adult HIVST Self-Efficacy Scale
Behavioral skills were assessed using an “Adolescent and Young Adult HIVST Self-Efficacy Scale” (24) and a “Perceived Effectiveness and Difficulty of Discussing the HIV Test with Partners” (25, 26) assessment. Participants strongly indicated that they could: use the HIVST correctly, understand the results of the HIVST, talk about using the HIVST with a potential sexual partner, talk about using the HIVST if they were unsure of their partner's feelings about it, and say no to sex if their partner refused to take an the HIVST. Participants were less certain they could talk about using the HIVST with a potential sexual partner before they started to hug and kiss, or talk a partner into taking a HIVST before they have sexual intercourse. Participants felt least confident they could use the HIVST if drinking beer, wine or other liquor, indicating that substance use could be a significant barrier to HIVST use (See Table 1, Instrument: HIVST Self-Efficacy).
Perceived Effectiveness and Difficulty of Discussing the HIVST with Partners
Most participants indicated that it would be easy to keep a supply of HIVST in their home and easy to carry the HIVST when they go out. Participants felt less confident about judging whether a sexual partner could become violent over taking the HIVST, using the HIVST when their partner is under the influence of alcohol or drugs, and using the HIVST with a partner when they are under the influence of alcohol or drugs. Even so, participants indicated that they could handle a violent situation that occurred as a result of using or proposing to use the HIVST.
Timing is also a critical factor to use. Participants felt they could raise the issue of taking the HIVST with a potential partner: as soon as they made contact, while chatting online, in a bar or club, on the telephone, in person before anything sexual happened, and while =fooling around‘ but before penetration (See Table 1, Instrument: Perceived Effectiveness and Difficulty of Discussing the HIV Test with Partners).
Ease of use
Some participants‘ expressed initial feelings of tribulation with performing the HIVST for the first time. After having used the HIVST, most participants reported feeling more comfortable using it on their own and reported feeling confident that they could follow the instructions that were provided with the HIVST without being supervised.
M: Tell me, how are you feeling after the test?
R: I am happy, of course, I am HIV negative. It was my first time doing it by myself. I haven‘t got HIV tested in a few months, but it‘s my first time doing it by myself so it was really interesting. I learned how to…being able to do it myself by the instructions and stuff. It was really exciting.
M: How do you think you would have felt if you had done this at home?
R: At home? I think I still would have been a little lost. I was kind of lost, but the instructions helped me. I think I would be happy to take this by myself at home.
Self-efficacy using the HIVST
Participants also felt confident that they would be able to use the HIVST with a sexual partner and for prevention. They were interested in finding out the HIV status of their sexual partners if it were unknown to them and would use the HIVST with partners if given the opportunity.
M: Now I am going to ask you about a few situations in which you may use the HIVST. Please tell me one scenario in which you would use this test.
R: I will use this test before seeing any sexual partners. I would let them use it and I use it before anything first.
Negotiating Use of HIVST with sexual partner(s)
Participants felt that they would be able to negotiate use of the test with partners. Though some expressed reservations and concerns of violence, many participants said that they felt they would be able to communicate with their partner effectively about the HIVST.
“If I was having sex with a partner that I usually have sex with and I wanted to know their status before we continue to have sexual relations, I would have him take the test. If it was something that I knew on a regular…if it was a stranger, I don‘t know…not a stranger, but somebody I don‘t really know, I wouldn‘t be able to be like take a test because that would just seem awkward to me.”
DISCUSSION
HIVST is a tool that may help to improve HIV testing rates and promote risk reduction behaviors (29). There has been some research on the HIVST, and while people report being likely to use the technology, uptake has been low (30–33). A recent study was conducted with young Black MSM and transgender women and found that although the HIVST is available, there are many barriers to its use (34). Despite these findings there has been limited research to understand youth and young adults‘ perception on the use of the HIVST as a tool for health behavior change. More specifically, our work was focused on some of the contextual factors that influence participants‘ use of the HIVST. Our study specifically examined emotional and behavioral reactions, encouragement by others to use the test (35), and plans to use the information to get appropriate treatment, if applicable.
Now that the HIVST is available over the counter, the importance of understanding the potential for its use by sexually active young adults is fundamental. Yet use of the HIVST by untrained young adults is still not well understood, and this study helps to fill this gap in the literature. To better understand how young adults would use the HIVST, we used the IMB model to guide our study design. For the “information” construct, we identified several gaps in participants‘ knowledge. Many participants did not know that the HIVST was available or how to use it. Participants‘ understanding of HIV was average and their understanding of the HIVST was low, even after using the test; however, we found that participants did understand their clinical options for testing. Participants also identified several advantages of the HIVST over clinical testing: ease of use, privacy, speed of test results, and access.
For the “motivation” construct, we identified motivating factors such as importance of the approval of peers, intimate partners, and family referents, which were all important to HIVST use. Also, it should be noted that sibling relationships were the most impactful. Of particular importance was the indication that participants were motivated and confident to use the HIVST on themselves and with sexual partners. When asked to compare the HIVST to the clinical test, participants felt more motivated to use the HIVST to find out their HIV status. Both perceived advantages and disadvantages were discussed and though accessibility, speed of results, and increased privacy were seen as advantages, while cost and lack of support during a positive test result were repeatedly identified as significant barriers to use.
Also, regarding cost, participants indicated that they wouldn‘t be willing to spend a lot of money for the test. Twenty dollars seem to be the common maximum threshold. Conversely, the right cost was also indicated as possibly being a facilitator of HIVST use. Youth and young adults are often economically limited. In turn, some participants thought that the best thing would be to make the HIVST free so that it could be accessible to people for whom cost is a detrimental barrier.
In terms of “behavioral skills”, participants were confident in their ability to use the HIVST again at home without study staff or clinical supervision. Their self-efficacy to use the test was strong, as well as their self-efficacy to test partners of unknown status, which has been reported as a viable prevention strategy (35). Participants also indicated that it would be easy to keep a supply of rapid HIVST in their home. Many of these findings are promising in terms of HIV treatment and prevention. According to HIV prevention strategies highlighted by the CDC, an increase in HIV testing—as is provided with HIVST—could have a significant effect of lowering the disproportionate risk level and burden of HIV on youth and young adults.
Future Work
Considering our findings, HIVST has the potential to minimize the current gap in HIV incidence that exists among youth and young adults with their adult counterparts, particularly for underserved, minority youth and young adults with limited access to health care. Future work should incorporate the barriers to HIVST kit use, data on primary/steady partners, number of partners, or condom use as they relate to decision-making around HIVST use. This study identified a very small sub-population (n=4) of participants who had never been tested. Future work could explore if the HIVST can play a particularly important role for these individuals.
Limitation
The small sample size of this study is a limitation. The fact that the HIVST was already being marketed means that pre-knowledge of the HIVST kit was more likely. Even so, the scores on HIVST knowledge were quite low. All participants were recruited in New York City, a highly urban metropolitan area where access to HIV testing and/or HIVST is easier than in rural areas, thus limiting the generalizability of these findings to areas where the HIVST may be of greater use.
Participants used the HIVST kit under the supervision of a trained professional. Though their subsequent reflections on HIVST use are a good measure of their efficacy in using the HIVST, we did not measure effectiveness in the real world. Thus, future work should allow youth and young adults to use the HIVST kits at home and report their experiences.
Conclusion
The goal of this work was to understand high-risk young adults‘ knowledge, perceptions, and use of the HIVST. Our participants had little previous knowledge of the HIVST. However, once aware, likelihood and self-efficacy to use the HIVST for self-testing, partner testing, and as a prevention strategy was high. Nonetheless, the high cost of the test was identified as a barrier that would make it unlikely for many of our study participants to use the HIVST in their everyday lives. The HIVST is now widely available, and increased education around using the HIVST could strengthen youths‘ awareness of the HIVST and self-efficacy for testing themselves and their partners for HIV, which could subsequently increase HIV testing among this high-risk population and decrease their disproportionate burden of disease.
REFERENCES
- 1.Centers for Disease C, Prevention. Vital signs: HIV infection, testing, and risk behaviors among youths - United States. MMWR Morb Mortal Wkly Rep. 2012;61(47):971–976. [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention (CDC) [cited 2015 October 12];CDC - HIV Among Youth - Age - Risk - HIV/AIDS. 2012 Available from: http://www.cdc.gov/hiv/risk/age/youth/index.html?s_cid=tw_std0141316.
- 3.Center for Disease Control and Prevention (CDC) [cited 2015 Sept 11];HIV among African American Youth. 2014 Available from: http://www.cdc.gov/nchhstp/newsroom/docs/CDC-Youth-AAs-508.pdf.
- 4.Center for Disease Control and Prevention (CDC) HIV among Latinos Fact Sheet. 2011
- 5.Center for Disease Control and Prevention (CDC) [cited 2015 October 13];HIV Testing in the United States Atlanta, GA. 2015 Available from: http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-testing-us-508.pdf.
- 6.Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, et al. Youth risk behavior surveillance--United States, 2013. MMWR Surveill Summ. 2014;63(Suppl 4):1–168. [PubMed] [Google Scholar]
- 7.Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J, et al. HIV Infection and Awareness among Men Who Have Sex with Men–20 Cities, United States, 2008 and 2011. PLoS ONE. 2013;8(10):e76878. doi: 10.1371/journal.pone.0076878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooley LA, Wejnert C, Rose CE, Paz-Bailey G. Increases in Recent HIV Testing Among Men Who Have Sex With Men Coincide With the Centers for Disease Control and Prevention's Expanded Testing Initiative. Clinical Infectious Diseases. 2015;60(3):483–485. doi: 10.1093/cid/ciu851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Philbin MM, Tanner AE, DuVal A, Ellen J, Kapogiannis B, Fortenberry JD. Linking HIV-positive adolescents to care in 15 different clinics across the United States: Creating solutions to address structural barriers for linkage to care. AIDS care. 2014;26(1) doi: 10.1080/09540121.2013.808730. 10.1080/09540121.2013.808730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balán IC, Carballo-Diéguez A, Frasca T, Dolezal C, Ibitoye M. The Impact of Rapid HIV Home Test Use with Sexual Partners on Subsequent Sexual Behavior among Men Who Have Sex with Men. AIDS Behav. 2014;18(2):254–262. doi: 10.1007/s10461-013-0497-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibitoye M, Frasca T, Giguere R, Carballo-Diéguez A. Home Testing Past, Present and Future: Lessons Learned and Implications for HIV Home Tests. AIDS Behav. 2014;18(5):933–949. doi: 10.1007/s10461-013-0668-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orasure Technologies. OraQuick® Advance Rapid HIV-1/2 Antibody Test Customer Letter. Bethlehem, PA: OraSure Technologies; 2005. Apr, [Google Scholar]
- 13.Schnall R, Carballo-Diéguez A, Larson E. Can the HIV Home Test Promote Access to Care? Lessons Learned from the In-home Pregnancy Test. AIDS Behav. 2014;18(12):2496–2498. doi: 10.1007/s10461-014-0798-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiene SM, Fisher WA, Shuper PA, Cornman DH, Christie S, MacDonald S, et al. Understanding HIV transmission risk behavior among HIV-infected South Africans receiving antiretroviral therapy: An Information—Motivation—Behavioral Skills Model analysis. Health Psychology. 2013;32(8):860–868. doi: 10.1037/a0030554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrer RA, Morrow KM, Fisher WA, Fisher JD. Toward an information–motivation–behavioral skills model of microbicide adherence in clinical trials. AIDS Care. 2010;22(8):997–1005. doi: 10.1080/09540121003623719. [DOI] [PubMed] [Google Scholar]
- 16.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21(2):177–186. [PubMed] [Google Scholar]
- 17.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ventuneac A, Carballo-Diéguez A. HIV Home Test information. 2008 [Unpublished]. In press. [Google Scholar]
- 19.Urberg KA, Shiang-Jeou S, Liang J. Peer influence in adolescent cigarette smoking. Addictive Behaviors. 1990;15(3):247–255. doi: 10.1016/0306-4603(90)90067-8. [DOI] [PubMed] [Google Scholar]
- 20.Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: testing the Information-Motivation-Behavior Skills (IMB) model. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2006;38(1):18–25. doi: 10.1016/j.jadohealth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Carballo-Diéguez A, Ventuneac A. Intention to use HIV Home Test. 2007 [Unpublished]. In press. [Google Scholar]
- 22.Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM) Health Educ Q. 1990;17(1):53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- 23.Boshamer CB, Bruce KE. A scale to measure attitudes about HIV-antibody testing: Development and psychometric validation. AIDS Education and Prevention. 1999;11(5):400–413. [PubMed] [Google Scholar]
- 24.Hanna KM. An adolescent and young adult condom self-efficacy scale. J Pediatr Nurs. 1999;14(1):59–66. doi: 10.1016/S0882-5963(99)80061-X. [DOI] [PubMed] [Google Scholar]
- 25.Ventuneac A, Carballo-Diéguez A. Perceived Effectiveness and Difficulty of Discussing HIV Test with Partners Scale. 2007 [Unpublished]. In press. [Google Scholar]
- 26.Misovich SJ, Fisher WA, Fisher JD. A measure of AIDS prevention information, motivation, and behavioral skills. In: Davis WLY CM, Bauserman R, Schreer G, Davis SL, et al., editors. Sexually related measures: A compendium. Newbury Park, CA: Sage; 1998. pp. 328–337. [Google Scholar]
- 27.Schnall R, John R, Carballo-Dieguez A. Do High-Risk Young Adults Use the HIV Self-Test Appropriately? Observations from a Think-Aloud Study. AIDS Behav. 2015:1–10. doi: 10.1007/s10461-015-1240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schnall R, Rojas M, Travers J. Understanding HIV testing behaviors of minority adolescents: a health behavior model analysis. J Assoc Nurses AIDS Care. 2015;26(3):246–258. doi: 10.1016/j.jana.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carballo-Diéguez A, Frasca T, Dolezal C, Balan I. Will Gay and Bisexually Active Men at High Risk of Infection Use Over-the-Counter Rapid HIV Tests to Screen Sexual Partners? Journal of sex research. 2012;49(4):379–387. doi: 10.1080/00224499.2011.647117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marlin RW, Young SD, Bristow CC, Wilson G, Rodriguez J, Ortiz J, et al. Piloting an HIV self-test kit voucher program to raise serostatus awareness of high-risk African Americans, Los Angeles. BMC Public Health. 2014;14:1226. doi: 10.1186/1471-2458-14-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pant Pai N, Sharma J, Shivkumar S, Pillay S, Vadnais C, Joseph L, et al. Supervised and Unsupervised Self-Testing for HIV in High- and Low-Risk Populations: A Systematic Review. PLoS Medicine. 2013;10(4):e1001414. doi: 10.1371/journal.pmed.1001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eaton L, Driffin D, Smith H, Conway-Washington C, White D, Cherry C. Black Men Who Have Sex with Men, Sexual Risk-Taking, and Willingness to Use Rapid Home HIV Tests. Prev Sci. 2015;16(2):321–329. doi: 10.1007/s11121-014-0496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mackellar DA, Hou SI, Whalen CC, Samuelsen K, Sanchez T, Smith A, et al. Reasons for not HIV testing, testing intentions, and potential use of an over-the-counter rapid HIV test in an internet sample of men who have sex with men who have never tested for HIV. Sex Transm Dis. 2011;38(5):419–428. doi: 10.1097/OLQ.0b013e31820369dd. [DOI] [PubMed] [Google Scholar]
- 34.Frye V, Wilton L, Hirshfield S, Chiasson MA, Usher D, Lucy D, et al. “Just Because It's Out There, People Aren't Going to Use It.” HIV Self-Testing Among Young, Black MSM, and Transgender Women. AIDS Patient Care and STDs. 2015;29(11):617–624. doi: 10.1089/apc.2015.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ventuneac A, Carballo-Diéguez A, Leu C-S, Levin B, Bauermeister J, Woodman-Maynard E, et al. Use of a Rapid HIV Home Test to Screen Sexual Partners: An Evaluation of its Possible Use and Relative Risk. AIDS Behav. 2009;13(4):731–737. doi: 10.1007/s10461-009-9565-7. [DOI] [PMC free article] [PubMed] [Google Scholar]