Abstract
Objective:
To determine the predictive and diagnostic value of thorax trauma severity score (TTSS) in a population of thoracic trauma patients admitted to a secondary level trauma center.
Methods:
A Retrospective analysis of patients admitted over a period of two years with IDC-9 codes related to thoracic trauma was undertaken. The association of TTSS with complications and mortality was evaluated. We also determined the predictive value of TTSS using receiver operating characteristic curve (ROC).
Results:
238 patients with thoracic trauma, mostly middle-aged (62.2 ± 15 years), were included. The main mechanisms of injury were falls and traffic accidents. Thirty-three patients had important extra-thoracic injuries, but only 9 presented an ISS> 15. The average ISS was 3 ± 5; Morbidity was 2.5% and mortality was 2.1% as a result of thoracic injury and these patients had significantly higher TTSS values. Each score component was analyzed separately, showing significant association with complications and mortality. The area under the curve for TTSS was significant for predicting complications (0.848) and mortality (0.856) values. TTSS with a cut off value of 8 points had a sensitivity of 66% and specificity of 94% to predict complications and 80% sensitivity and 94% specificity for predicting mortality.
Conclusions:
The TTSS is an appropriate and feasible tool to predict the development of complications or mortality in a population of mostly mild thoracic trauma.
Key Words: Thorax Trauma Severity Score (TTSS), Thoracic Trauma, Mortality, Morbidity, Predictive value
Introduction
Early and accurate evaluation of the severity level in thoracic trauma is important for correct treatment, from predicting intensive care need, to future complications [1]. Currently, there is no scale in general use that does this, thus highlighting the need for a precise scale in the evaluation of thoracic trauma. Scales such as the ISS (Injury Severity Score) [2] or the TRISS (Trauma Injury Severity Score) [3] are widely used, but these being global poly-trauma scales, they underestimate isolated thoracic trauma. Other scales specific to the thorax such as the Abbreviated Injury Scale (AIStorax) [4] or Lung Injury Scale [5], rely solely on anatomical findings. Classically, it has been considered that the presence of 3 or more rib fractures or fracture of the first rib is associated with greater severity. The association of parameters such as age, mechanism and severity of injury with the development of pulmonary complications is still under study. In 2000, Pape et al described the Thorax Trauma Severity Score (TTSS), a scale that included both anatomical and functional [6] parameters. The purpose of the scale was to help emergency medical evaluation in identifying trauma patients at risk of pulmonary complications, using parameters available during the initial evaluation which could be applied in primary and secondary level hospitals. This scale has recently been validated for predicting mortality [7], but the study does not establish a cutoff point beyond which intensive care unit (ICU) admission or the need for mechanical ventilation could be indicated, data which we believe would be useful. The aim of our study was to describe the performance and to set the prognostic ability of TTSS in our thoracic trauma population, characterized mainly by low grade injuries.
Material and Methods
Study populationIn this retrospective, single-center, observational study we identified patients treated in our secondary level trauma hospital (Hospital Universitario de Torrevieja), Emergency Department and coded for diagnoses related with thoracic trauma, over a two years period (2012-2013). Codes from the International Classification of Diseases, 9th Revision (ICD-9): 807 (fractured rib(s), sternum, larynx and trachea), 860 (traumatic pneumothorax and haemothorax), 861 (heart and lung injury), 862 (damage to other intra-thoracic organs), 875 (open wound of the chest (wall)), 876 (open wound on the back), 959.11 (other traumas of the chest wall), 959.19 (other trauma in other trunk sites) and 959.8 (trauma of other specified sites, including multiple), were used as inclusion criteria. Pediatric patients (<14 years) and coding errors in the patient’s medical history were excluded. The institutional review board and the medical ethics committee of our center approved the study protocol before inclusion of the patients. As this was a retrospective study, we did not required informed written consents to be obtained from the patients.
Study protocol The TTSS specification uses 5 parameters: patient's age; number of rib fractures; pleural involvement (haemo/pneumothorax); presence and degree of pulmonary contusion and PaO2/FiO2, each scored on a scale of 0 to 5 points, with 0 representing normal function; absence of injury or age <30 years and 5 representing severity or age > 70 years. The TTSS is calculated by adding each of the values, with a minimum of 0 and a maximum of 25 (Table 1) [6]. The medical records of patients were reviewed to determine the values of distinct qualitative and quantitative variables consisting of: each of the parameters of the TTSS scale; patient sex; mechanism of injury; AIS and ISS scale values; associated injuries; hospital stay; ICU stay; need for mechanical ventilation; admission; complications and mortality. Chest X-rays of each patient included in the study were reviewed individually by one of the authors to confirm findings described in the medical records.
Table 1.
Thorax Trauma Severity Score (Pape et al.) [6].
| Grade | PaO2/FiO2 | Rib Fractures | Lung Contusion | Pleura | Age (years) | POINTS |
|---|---|---|---|---|---|---|
| 0 | > 400 | 0 | No | No | < 30 | 0 |
| I | 300-400 | 1-3 | Unilobar unilateral | Pneumothorax | 30-41 | 1 |
| II | 200-300 | 3-6 | unilobar bilateral or bilobar unilateral | Haemothorax or haemo/pneumothorax unilateral | 42-54 | 2 |
| III | 150-200 | > 3 bilateral | bilateral < 2 lobules | Haemothorax or haemo/pneumothorax bilateral | 55-70 | 3 |
| IV | <150 | Flail chest | Bilateral ≥ 2 lobules | Tension pneumothorax | > 70 | 5 |
Statistical analysis Statistical analysis was performed with statistical package for social sciences (SPSS Inc. for Mac, IBM Corporation Inc. Chicago, IL. USA). Data are presented as mean ± SD and proportions as appropriate. Mann-Whitney and Chi-Square tests were used for association analysis between categorical variables. Diagnostic test characteristics for mortality and complications were calculated from the ROC curves. A two-sided P values of less than 0.05 was considered statistically significant.
Results
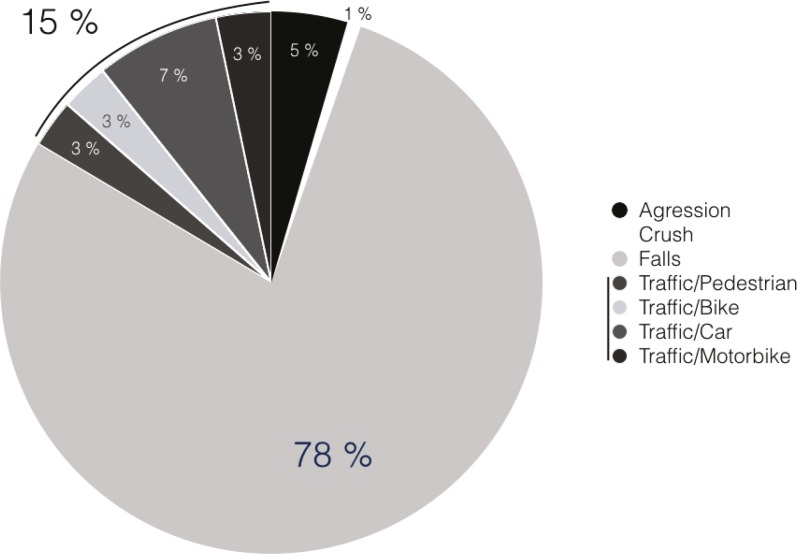
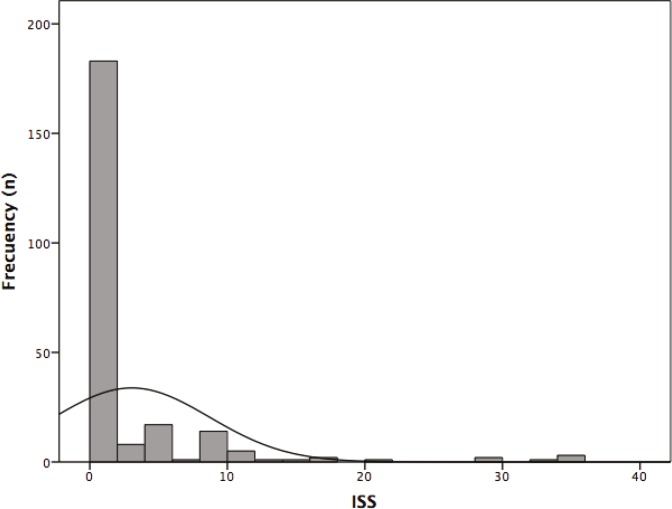
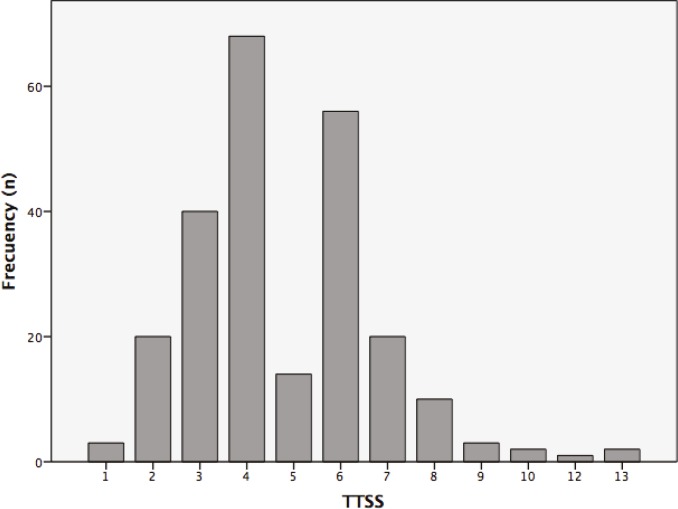
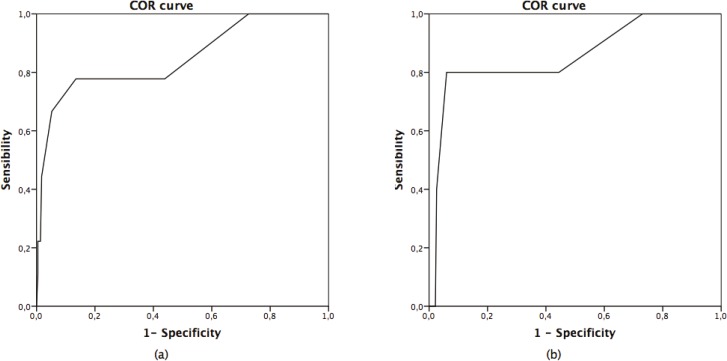
During the study period, 137,738 emergency patients were admitted in our general emergency department. Of these, only 239 met the inclusion criteria. Patients were mostly male (160; 66.9%) with a mean age of 62.2±15.9 years (range 24-92 years). Only 42 patients (17.6%) were coded poly-trauma care on admission (ACS triage) and 33 patients (13.8%) had associated extra-thoracic injuries that were clinically relevant. The majority of cases were as a result of accidental falls (> 3 meters in patients younger than 65 years, < 3 meters in older) (190; 79.5%) or traffic accidents (36; 15%) Figure 1. The most frequent diagnoses were rib fractures (single in 133 patients, multiple in 79 patients); haemothorax (8 patients); pneumothorax (6 patients); or pulmonary contusions (5 patients). Other diagnoses included fractures of the collarbone, sternum or scapula and haemomediastinum and partial aortic rupture in two patients. Regarding the severity of injuries, patients had mostly mild trauma, with an average AIST of 1.28±0.6 (AIST 1: 82.4%, AIST 2 and 3: 8.4%, AIST 4 and 5: 0.4%) and a mean ISS of 3±5.6 (range 1-35 points) estimated at admission. Only 9 patients (3.7%) had an ISS >15. Figure 2 shows the distribution of the population according to their ISS severity. The average hospital stay of patients was 1.5±4.3 days (range 0-45 days) and 17 patients (7.1%) required admission to the ICU with an average stay of 0.46±3.2 days (0-45 days). Eight of these patients (3.3%) required mechanical ventilation. Six of the total number of patients had complications (2.5%) and 5 patients died (2.1%). Complications reported were pneumonia; secondary pneumothorax; persistent haemothorax; Adult Respiratory Distress Syndrome (ARDS) or empyema. Neither the poly-trauma activation code nor the presence of relevant extra-thoracic injuries, were significantly associated with the presence of complications or mortality. The average TTSS of patients was 4.8±1.9 points. Figure 3 shows the frequency histogram of patient scores. When performing the nonparametric Mann-Whitney test significant differences in the values of TTSS were found to be substantially higher in patients who had complications (p=0.001) or died (p=0.005). Analyzing separately each of the variables of the scale, it was observed that there were significant associations between the presence of complications and the points scored by age (p=0.012); PaO2/FiO2 index (p<0.001); by the number of rib fractures (p<0.001); pulmonary contusion (p<0.001) and pleural involvement (p<0.001). The variables also showed significant association with mortality: age (p=0.02); rib fractures (p<0.001); pulmonary contusion (p=0.001) and pleural involvement (p<0.001). PaO2/FiO2 points index was close to statistical significance (p=0.07). ROC curves were used to estimate the sensitivity and specificity of the TTSS scale versus prediction of complications and mortality. The area under the curve shows a value of 0.848 (p<0.001) for complications and a value of 0.856 (p=0.006) for mortality (Figure 4 A and B, respectively).
Fig. 1.
Mechanism of injury distribution in our study population
Fig. 2.
Injury Severity Scoredistribution in the study population
Fig. 3.
TTSS points of the study population
Fig. 4.
ROC Curve analysis for complications (a) and mortality (b) prediction. Area under the curve showed a value of 0.848309 for complications and 0.855983 for mortality
Analyzing separately the 9 patients with ISS >15, only 4 of this patients had TTSS >8 (44%), probably reflecting the importance of other extra-thoracic injuries in the severity of the patients. Three (33%) had major complications and 2 of them (22%) died (one pedestrian with haemomediastinum and aortic rupture, TTSS 13 points; and the patient with the crush syndrome, TTSS 4 points). The patient in this group with major complications was a 45yo male after car accident with 4 rib fractures, haemothorax and pulmonary contusion, TTSS 13 and developing pneumonia and catheter related sepsis). Taking out of the analysis this 9 severe poly-trauma patients, mortality increases from 0.4 to 33% in patients with TTSS >8, and complications from 1.3 to 33%, although small simple size precludes us from any significant statistic analysis. Using Bayes' theorem, for an estimated cumulative incidence of 2.5% in case of complications and 2.1% for death, and from the sensitivity and specificity estimates with 8 scale points as a cutoff, we calculated positive and negative predictive values (PPV, NPV) for complications and mortality in patients with thoracic trauma (Table 2).
Table 2.
Sensibility, specificity and predictive values of a TTSS ≥ 8 points for complications and mortality prediction
| Complications | Mortality | ||
|---|---|---|---|
| CI 95% Sensibility | 0.66 ± 0.41 | CI95% Sensibility | 0.80 ± 0.35 |
| CI 95% Specificity | 0.94 ± 0.03 | CI95% Specificity | 0.94 ± 0.03 |
| CI 95% Positive Predictive Value | 0.22 ± 0.19 | CI95% Positive Predictive Value | 0.22 ± 0.61 |
| CI 95% Negative Predictive Value | 0.99 ± 0.01 | CI95% Negative Predictive Value | 0.99 ± 0.01 |
CI: Confidence Interval
Discussion
The creation of scales is a basic requirement in the epidemiology of trauma and is needed to predict the morbidity and mortality of these patients [8]. Scales most commonly used in trauma combine anatomical and physiological parameters. The addition of other factors, such as patient co-morbidity, age, or differences in immune status or genetic predispositions, make the task of creating a universally applicable and accepted scale extremely difficult. A scale should be accurate, reliable and specific. The robustness of a scale for trauma depends on, among other factors, the composition of the study population. The validation process includes the use of a population different from the original one. The observed variation in morbidity and mortality between different centers or countries may reflect differences in the severity of injuries in individual patient characteristics or quality of treatment, but it could also reflect inaccuracies or actual mistakes in the scale used to synthesize information [9,10]. Several studies have correlated pulmonary complications with thoracic extension [11,12] trauma. Recently developed rating scales to predict lung failure in trauma patients, such as Lung Organ Failure Score (LOFS), which includes variables such as sex; age; severity of injury; chest or head, predict the need for urgent surgery (s) and volumes of fluid resuscitation for severe trauma patients [1]. This particular study of almost 6,000 patients on the Trauma Registry of the German Trauma Society (DGU), included patients with ISS>15 and predicted which patients would develop complications for entry into intensive care. The limitations of the study are the fact that it is retrospective; based on parameters which are difficult to quantify during the initial resuscitation or imprecise estimates that could have affected the results. The TTSS is a specific scale for thoracic trauma, originally conceived for patients with severe blunt trauma (AIS>2, ISS>18) but with more than 48 hours survival [6]. The scale has been validated in other severe trauma groups [7]. One possible weakness of the scale however is the difficulty of assessing the significance of other associated trauma in the analysis of the results. The possible influence of the presence of associated injuries on mortality in relation to the scale scores in these patients, is difficult to assess. While it is known that the severity of thoracic injury in poly-traumatized patients represents a gravity factor [13], it is difficult to establish how far thoracic injury may affect the development of (DRSA) [14]. Interestingly, in our study the previous activation of a poly-trauma code or the presence of relevant extra-thoracic injuries, like head, limbs or abdomen AIS>2, were not significantly associated with complications or mortality, the first reflecting an over-triage policy, stated by the low frequency of strictly defined poly-trauma patients (ISS>15: 3.7%) in our series. In line with other studies, the TTSS values were significantly higher in patients with complications or mortality. Taken individually, increasing scale score variables also show significant association with complications and mortality. It seems obvious that age or pulmonary parenchymal lesions are more important parameters for predicting mortality than rib fractures. On the other hand, the old "per se" is influenced by confounding factors not taken into account by the scale, such as the presence of co-morbidities or propensity to develop complications. An association between age and increased risk of rib fractures has been demonstrated against pulmonary contusion [6], and other studies have confirmed that it is not possible to establish a correlation between the number of rib fractures and underlying pulmonary injury or its progression [15-17]. Our work aimed to assess the applicability, reliability and precision of the TTSS scale in predicting complications and mortality and study its performance in our local thoracic trauma population, which is characterized by a low prevalence of severe trauma. In our study, the ROC curves allowed us to calculate the predictive values as an indicator for monitoring these patients and establish a cutoff at 8 points on the scale, below which it is highly unlikely for complications or mortality to occur, and above that, although >8 gives no relevant positive prediction (0,22) neither for complications nor for mortality, the probability multiplied per 10 to the probability estimated for both complications and mortality to occur in our population. In non-severe patients according to ISS, there is a clear tendency in patients with >8 score points to show more complications and mortality, although not reaching statistical significancy due to small number of patients. It is well known that elderly patients with apparently minor trauma attending to mechanism can hide lesions or scape our attention in the initial assessment. Half of our patients were older than 65 years and nearly 70% minor falls (<3 mts). According to the score and our results, a 71yo patient with 2 rib fractures and minimum unilateral haemothorax reaches the 8 cutpoint, and can be allocated in the patient at risk of complications or mortality group, indicating a better surveillance for the patient is needed.Our study has, however, some limitations due to its retrospective nature and the sample size on which the results are based. Accurate prospective and larger population studies are needed to support our findings. In conclusion, TTSS has a high correlation with the occurrence of complications or mortality in patients with thoracic trauma in a population with mostly minor trauma, making it a useful tool to predict the development of complications or mortality in patients admitted to Emergency Department with a thoracic trauma. A cut-off level of 8 points in TTSS can be use to classify patients for careful observation.
Conflict of Interest: None declared.
Note
Please cite this paper as: Martinez Casas I, Amador Marchante MA, Paduraru M, Fabregues Olea AI, Nolasco A, Medina JC. Thorax Trauma Severity Score: Is it reliable for Patient’s Evaluation in a Secondary Level Hospital?. Bull Emerg Trauma. 2016;4(3):150-155.
References
- 1.Wutzler S, Wafaisade A, Maegele M, Laurer H, Geiger EV, Walcher F, et al. Lung Organ Failure Score (LOFS): probability of severe pulmonary organ failure after multiple injuries including chest trauma. Injury. 2012;43(9):1507–12. doi: 10.1016/j.injury.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 2.Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96. [PubMed] [Google Scholar]
- 3.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method Trauma Score and the Injury Severity Score. J Trauma. 1987;27(4):370–8. [PubMed] [Google Scholar]
- 4.Committee on Medical Aspects of Automotive Safety. Rating the severity of tissue damage I The abbreviated scale. JAMA. 1971;215(2):277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 5.Moore EE, Malangoni MA, Cogbill TH, Shackford SR, Champion HR, Jurkovich GJ, et al. Organ injury scaling IV: Thoracic vascular, lung, cardiac, and diaphragm. J Trauma. 1994;36(3):299–300. [PubMed] [Google Scholar]
- 6.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49(3):496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Aukema TS, Beenen LF, Hietbrink F, Leenen LP. Validation of the Thorax Trauma Severity Score for mortality and its value for the development of acute respiratory distress syndrome. Open Access Emerg Med. 2011;3:49–53. doi: 10.2147/OAEM.S22802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tamim H, Al Hazzouri AZ, Mahfoud Z, Atoui M, El-Chemaly S. The injury severity score or the new injury severity score for predicting mortality, intensive care unit admission and length of hospital stay: experience from a university hospital in a developing country. Injury. 2008;39(1):115–20. doi: 10.1016/j.injury.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35(4):347–58. doi: 10.1016/S0020-1383(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 10.Meredith JW, Evans G, Kilgo PD, MacKenzie E, Osler T, McGwin G, et al. A comparison of the abilities of nine scoring algorithms in predicting mortality. J Trauma. 2002;53(4):621–8. doi: 10.1097/00005373-200210000-00001. discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 11.Edens JW, Chung KK, Pamplin JC, Allan PF, Jones JA, King BT, et al. Predictors of early acute lung injury at a combat support hospital: a prospective observational study. J Trauma. 2010;69( Suppl 1):S81–6. doi: 10.1097/TA.0b013e3181e44a32. [DOI] [PubMed] [Google Scholar]
- 12.Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, et al. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51(2):223–8. doi: 10.1097/00005373-200108000-00003. discussion 9-30. [DOI] [PubMed] [Google Scholar]
- 13.Gaillard M, Herve C, Mandin L, Raynaud P. Mortality prognostic factors in chest injury. J Trauma. 1990;30(1):93–6. doi: 10.1097/00005373-199001000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Miller PR, Croce MA, Kilgo PD, Scott J, Fabian TC. Acute respiratory distress syndrome in blunt trauma: identification of independent risk factors. Am Surg. 2002;68(10):845–50. discussion 50-1. [PubMed] [Google Scholar]
- 15.Tyburski JG, Collinge JD, Wilson RF, Eachempati SR. Pulmonary contusions: quantifying the lesions on chest X-ray films and the factors affecting prognosis. J Trauma. 1999;46(5):833–8. doi: 10.1097/00005373-199905000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Abbasi HR, Mousavi SM, Taheri Akeri A, Niakan MH, Bolandparvaz S, Paydar S. Pattern of Traumatic Injuries and Injury Severity Score in a Major Trauma Center in Shiraz, Southern Iran. Bull Emerg Trauma. 2013;1(2):81–85. [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmad Ganie F, Lone H, Lone GN, Wani MH, Singh Sh, Dar AM, Wani N, wani Sh N, Nazeer N. Lung Contusion: A Clinico-Pathological Entity with Unpredictable Clinical Course. Bull Emerg Trauma. 2013;1(1):7–16. [PMC free article] [PubMed] [Google Scholar]