Abstract
Main goal in the management of patients with severe traumatic brain injury (TBI) is control of intracranial pressure (ICP). Decompressive craniectomy is an accepted technique for control of refractory intracranial hypertension in patients with severe TBI. Because of high complication rate after decompressive craniectomy, new techniques such as basal cisternostomy have developed. We herein report a case of severe TBI in a 13-year-old boy treated by cisternostomy. The patient was admitted following a motor vehicle accident. Brain CT scan showed diffuse brain edema, left frontal contusion and posterior interhemispheric subdural hematoma. The patient underwent ICP monitoring. Subsequently, with 26 mmHg mean-value of ICP, he was treated surgically by cisternostomy technique. A progressive improvement of the neurological conditions in the following hours. After 5 days the boy was discharged and in the 3-months follow-up he was completely recovered. Cisternostomy could be an appropriate alternative to decompressive craniectomy for management of intracranial hypertension in patietns with sever TBI.
Key Words: Severe traumatic brain injury, Intracranial hypertension, Cisternostomy, Outcome
Introduction
The subarachnoid cisterns are spaces within the subarachnoid space where the pia mater and arachnoid membrane are not in close approximation. These spaces are filled with the cerebrospinal fluid [1]. Opening of the basal cisterna for evacuation of the cerebrospinal fluid is a well-recognized and effective method for brain relaxation in microneurosurgical approaches to the skull base especially in microvascular surgery [2, 3]. Traumatic brain injury (TBI) is the leading cause of mortality and morbidity in children worldwide. An important goal of TBI treatment is to avoid the secondary injuries to the traumatized brain. Mortality in children with severe TBI is often the result of a refractory intracranial hypertension [4]. Meticulous control of intracranial pressure (ICP) can improved outcome of patients after TBI [5]. Decompressive craniectomy remain the surgical technique of choice for management of refractory intracranial hypertension in patients with TBI [6,7]. But the complications following decompressive craniectomy and also cranioplasty cause the neurosurgeons to search for new ways of controlling intracranial hypertension in TBI [8-11]. Recently basal cisternostomy has been introduced for management of ICP in TBI with acceptable success rate [12]. We herein present management of intracranial hypertension following severe TBI in child with cisternostomy.
Case Report
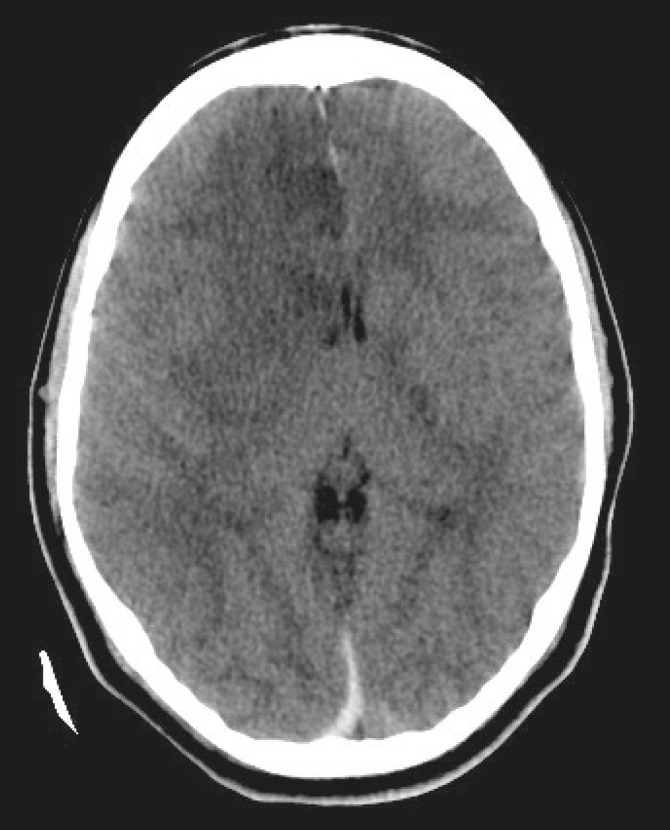
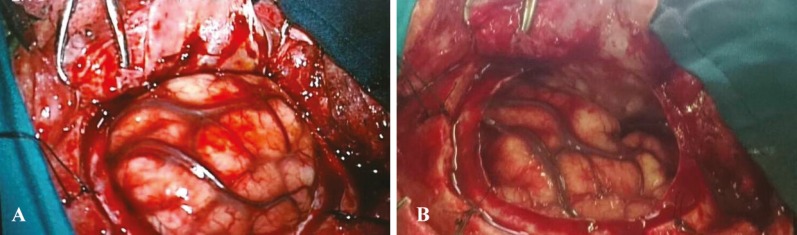
A 13-year-old boy referred to our center by emergency service following multiple trauma due to a Motor-vehicle accident; his father and brothers expired in the same accident. On arrival, he had GCS 6/15 (M: 4; V: 1; E: 1), bilateral sluggish papillary response to the light and significant respiratory distress due to severe lung contusion. He had fractures in both lower extremities long bones and severe facial injury because of mid-facial trauma. The brain CT-Scan revealed generalized brain edema, left frontal contusion and posterior interhemispheric subdural hematoma (Figure 1). The patient was transferred to the operating room and a ventriculostomy catheter for closed monitoring of ICP was inserted. His average ICP in a 24-hour period was 26 mmHg despite receiving medical therapies for intracranial hypertension. Thus, we reassessed the patient condition and decided to control his intracranial hypertension by a surgical technique. It was decided to insert a draining catheter in the basal cisterna to evacuate the cerebrospinal fluid (CSF). The patient was placed in supine position with his head slightly turned to the left. Supraorbital craniotomy was carried out and the dura was opened on the base of the orbital rim. We observed severe cerebral edema that was resistant to all methods of neuroanesthesia (Figure 2A). Then, through microscopic subfrontal approach, we exposed the basal cisterna. After gentle and careful subfrontal retraction of the brain, we opened the suprachiasmatic, carotido-oculomotor and sylvian (medial part) cisterna and evacuated a significant amount of CSF. After that, brain was relaxed (Figure 2B). We then inserted a ventriculostomy catheter in the suprachiasmatic and planum sphenoidale, passed it through the dura and skin, and connected it to a ventriculostomy bag. After closure of the dura, his bone was fixed at the site and the patient was transferred to ICU for ICP monitoring. The cistsernostomy system was on draining valve. After 48 hours of ICP monitoring, the mean ICP was 14 mmHg and the CT-scan revealed decreased edema (Figure 3). Thus the ventriclostomy and cisternostomy catheters were removed. One day after the operation, the patient’s GCS improved and after 5 days he was completely conscious. He was finally discharged from the hospital with GCS of 13/15. On 3-month follow-up, he had excellent neurological recovery. He had a Glasgow outcome score (GOS) of 4.
Fig. 1.
The initial brain CT-Scan of the patient demonstrating generalized brain edema, left frontal contusion and posterior interhemispheric subdural hematoma
Fig. 2.
A ) The initial intraoperative image of the brain after opening of the dura following a supralateral craniotomy demonstrating severe edema; B) Intraoperative image of the brain after opening of the basal cisterna and evacuation of significant amount of CSF demonstrating brain relaxation
Fig. 3.
Postoperative brain CT-Scan demonstrating relaxed brain with decreased edema along with pneumocephalus and a ventriculostomy catheter placed in basal cisterna
Discussion
Currently, management of patients with TBI based in ICP values is considered the method of choice [5]. Decompressive craniectomy is also considered the surgical method of choice in patients with severe TBI [7,8]. But complications after decompressive craniectomy and cranioplasty encourage the trauma surgeons to think about new methods of intracranial hypertension management [9-11]. All neurosurgeons accept the concept that evacuation of CSF from the basal cisterns is an effective method for achieving a relaxed brain during a microsurgical approach [1, 4]. Cherian and Munakomi [12] presented cisternostomy as a new method for the control of ICP in TBI that could replace decompressive craniectomy [12-14]. Avoidance from complications of decompressive surgery and cranioplasty are two critical reasons that encourage and satisfy neurosurgeons to utilize cisternostomy for control of ICP in patients with TBI. But the use of this technique needs good understanding of neuroanatomy of the basal cisterns and also enough experience in microsurgical anatomy [15]. In their technique they remove anterior and posterior clinoid processes and opens all basal cisterns including inter-optic cistern, optico-carotid, lateral carotid, interpeduncular and prepontine [15]. By using cisternostomy technique, we can decrease morbidities associated with removal of the bone flap in decompressive craniectomy and also the need for doing cranioplasty after that. In the current case, we did not remove the clinoid process and got the access to the basal cisterns through subfrontal approach by gentle brain retraction. We opened suprachiasmatic, carotido-oculomotor and sylvian (medial part) cisterna and drained significant amount of CSF which resulted in gross intraoperative brain relaxation and controlled ICP postoperatively. The outcome of the patient was excellent in 3-month follow-up. This is in concordance with previous reports of management of ICP in TBI patients utilizing basal cisternostomy. In conclusion, basal cisternostomy is an appropriate, effective, safe and feasible surgical method for management of severe TBI. Further clinical series and randomized clinical trials are required to shed light of its short- and long-term efficacy in management of patients with severe TBI.
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Namazi Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Conflict of Interest: None declared.
Note
Please cite this paper as: Masoudi MS, Rezaee E, Hakiminejad HA, Tavakoli M, Sadeghpoor T. Cisternostomy for Management of Intracranial Hypertension in Severe Traumatic Brain Injury; Case Report and Literature Review. Bull Emerg Trauma. 2016;4(3):161-164.
References
- 1.Yasargil MG, Kasdaglis K, Jain KK, Weber HP. Anatomical observations of the subarachnoid cisterns of the brain during surgery. J Neurosurg. 1976;44(3):298–302. doi: 10.3171/jns.1976.44.3.0298. [DOI] [PubMed] [Google Scholar]
- 2.Vale FL, Bradley EL, Fisher WS 3rd. The relationship of subarachnoid hemorrhage and the need for postoperative shunting. J Neurosurg. 1997;86(3):462–6. doi: 10.3171/jns.1997.86.3.0462. [DOI] [PubMed] [Google Scholar]
- 3.Mura J, Figueiredo EG, Carmona P, Palma-Fellemberg A, de Faria JW. The anterior ventriculo-cisternostomy: the pioneers' work revisited. J Neurol Surg A Cent Eur Neurosurg. 2013;74(3):146–51. doi: 10.1055/s-0032-1330122. [DOI] [PubMed] [Google Scholar]
- 4.Ghajar J. Traumatic brain injury. Lancet. 2000;356(9233):923–9. doi: 10.1016/S0140-6736(00)02689-1. [DOI] [PubMed] [Google Scholar]
- 5.Rahmanian A, Haghnegahdar A, Ghaffarpasand F. Effects of Intracranial Pressure Monitoring on Outcome of Patients with Severe Traumatic Brain Injury; Results of a Historical Cohort Study. Bull Emerg Trauma. 2014;2(4):151–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006;104(4):469–79. doi: 10.3171/jns.2006.104.4.469. [DOI] [PubMed] [Google Scholar]
- 7.Alvis-Miranda H, Castellar-Leones SM, Moscote-Salazar LR. Decompressive Craniectomy and Traumatic Brain Injury: A Review. Bull Emerg Trauma. 2013;1(2):60–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Ho B, Ooi M, Yinn C, Sheikh M, Muhamad A, Jallo M. Complications of Decompressive Craniectomy. JHN Journal. 2012;7(1) [Google Scholar]
- 9.Honeybul S, Ho KM. Long-term complications of decompressive craniectomy for head injury. J Neurotrauma. 2011;28(6):929–35. doi: 10.1089/neu.2010.1612. [DOI] [PubMed] [Google Scholar]
- 10.Khalili H, Omidvar A, Ghaffarpasand F, Yadollahikhales G. Cranioplasty Results after Application of Anti-adhesive Films (OrthoWrap) in Traumatic Decompressive Craniectomy. Bull Emerg Trauma. 2016;4(1):24–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Zanaty M, Chalouhi N, Starke RM, Clark SW, Bovenzi CD, Saigh M, et al. Complications following cranioplasty: incidence and predictors in 348 cases. J Neurosurg. 2015;123(1):182–8. doi: 10.3171/2014.9.JNS14405. [DOI] [PubMed] [Google Scholar]
- 12.Cherian I, Yi G, Munakomi S. Cisternostomy: Replacing the age old decompressive hemicraniectomy? Asian J Neurosurg. 2013;8(3):132–8. doi: 10.4103/1793-5482.121684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherian I. Basal cisternostomy–Is it a panacea for traumatic brain swelling? Journal of College of Medical Sciences-Nepal. 2012;8(1):1–6. [Google Scholar]
- 14.Cherian I, Bernardo A, Grasso G. Cisternostomy for Traumatic Brain Injury: Pathophysiologic Mechanisms and Surgical Technical Notes. World Neurosurg. 2016;89:51–7. doi: 10.1016/j.wneu.2016.01.072. [DOI] [PubMed] [Google Scholar]
- 15.Cherian I, Grasso G, Bernardo A, Munakomi S. Anatomy and physiology of cisternostomy. Chin J Traumatol. 2016;19(1):7–10. doi: 10.1016/j.cjtee.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]