Abstract
This study assessed the in vitro antibacterial activity of combinations of amikacin and doxycycline or tigecycline against multidrug-resistant E. coli isolates. Twenty-four different pulsotypes, including 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant, 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-E. coli isolates were collected. All 24 isolates were susceptible to amikacin and tigecycline. Only 30% of ESBL and 50% of carbapenem-resistant E. coli were susceptible to doxycycline. Both of the NDM-E. coli had a MIC of 64 μg/ml. The checkerboard method showed that for the ESBL- and carbapenem-resistant E. coli, the synergistic effects of amikacin/doxycycline were 80% and 90%, respectively. For the two KPC- and two NDM-E. coli, the FIC index of amikacin/doxycycline were 0.5/0.375 and 0.5/0.281, respectively. For the ESBL- and carbapenem-resistant E. coli isolates, the combinations of amikacin and doxycycline exhibited synergistic activities against 80%, and 80% and 10% vs 60%, and 80% and 10% of the isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. The synergistic effect seems to be similar for doxycycline and tigecycline based combinations with amikacin. In conclusion, the antibacterial activity of doxycycline can be enhanced by the addition of amikacin and is observed against most multidrug-resistant E. coli isolates.
Escherichia coli, a Gram-negative rod, can cause protean human infections, such as gastroenteritis, urinary tract infections, peritonitis, pneumonia and septicemia. The administration of appropriate antibiotics dependent upon susceptibility pattern is life-saving for the treatment of severe E. coli infections. However, the emergence of antibiotic-resistant E. coli has limited the therapeutic options available to physicians1,2. The production of β-lactamase is the most common mechanism of bacterial resistance to β-lactam. Among various antibiotic-resistant mechanisms, extended-spectrum β-lactamase (ESBL)- and carbapenemase-producing Enterobacteriaceae are spreading mostly as nosocomial pathogens worldwide, and the serious concern is that ESBL- and carbapenemase-producing Enterobacteriaceae are typically resistant to most of the currently available antibiotics1,3. To overcome this critical clinical condition, severe multi-drug resistant (MDR) bacterium infection, antimicrobial combination therapy with in vitro synergistic effect may be a better treatment option compared with monotherapy4,5,6,7,8. However, specific relevant investigations are scarce that guide the determination of the most appropriate combination antimicrobial therapy options.
Tigecycline, polymyxins, carbapenems, aminoglycosides, fluoroquinolones, fosfomycin, rifampicin, ampicillin-sulbactam, piperacillin-tazobactam, and tetracyclines (minocycline and doxycycline) are common antibiotics that have been used in combinations9,10,11. Although colistin, tigecycline, and some aminoglycosides remain most likely to be active in vitro against carbapenem-hydrolyzing β-lactamases producing Enterobacteriaceae, current data do not reliably support the use of these agents as monotherapy for systemic infections2. Antimicrobial combination therapy with these agents exhibiting synergistic effects might also be of benefit, and the investigation of further effective therapeutic regimens with various antibiotic combinations is warranted. However, most studies have been conducted to determine the in vitro activity of combination therapy against Klebsiella pneumoniae carbapenemase (KPC)-producing Klebsiella pneumoniae4,5,6,7. Enhanced activity was noted following treatment with doxycycline combined with amikacin against KPC-producing K. pneumoniae isolates in a recent study7; however, other in vitro studies of the combination effect of an aminoglycoside-amikacin with doxycycline or tigecycline against multi-drug resistant E. coli are rare. The goal of this study was to assess the in vitro antibacterial activity of the combinations of an aminoglycoside (amikacin) and doxycycline or tigecycline against ESBL-, carbapenem-resistant, New Delhi Metallo-beta-lactamase (NDM)- and KPC-producing E. coli isolates.
Materials and Methods
The collection of clinical isolates
Twenty-four different pulsotypes E. coli including 10 ESBL, 10 CRE, 2 KPC and 2 NDM strains were collected from the Department of Bacteriology at Chi Mei Medical Center between May 1, 2012 and April 30, 2014. Ethics approval was obtained from the Institution Review Board of the Chi Mei Medical Center. All of the methods were carried out in accordance with the relevant guidelines, and informed consent was obtained from all subjects. The isolates were stored at −80 °C in Protect Bacterial Preservers (Technical Service Consultants Limited, Heywood, UK) before use. ESBL was tested for use with both cefotaxime and ceftazidime, alone and in combination with clavulanic acid. An increase in the zone diameter of ≥5 mm for either antimicrobial agent tested in combination with clavulanic acid over that when tested alone indicates that the isolate is an ESBL producer12, excluding carbapenem resistant strains. Carbapenem resistance is defined as resistance to imipenem, meropenem, doripenem, or ertapenem. The carriage of KPC or NDM was confirmed by polymerase chain reaction (PCR) sequence analysis13. Species confirmation was performed by standard biochemical methods, on a VITEK 2 automated system (bioMérieux, Marcy l’Etoile, France).
In vitro susceptibility
Standard powders of amikacin and doxycycline were obtained from Sigma, St Louis, MO. Tigecycline by Pfizer (New York, NY). MIC determinations and susceptibility interpretation criteria followed the CLSI and FDA standards14,15. The minimum inhibitory concentrations (MICs) of the drugs were measured by broth microdilution in freshly prepared Mueller-Hinton broth (Oxoid, Basingstoke, UK) with 25 μg/mL of calcium and 12.5 μg/mL of magnesium (CAMHB), as recommended by the CLSI guidelines14,16. E. coli ATCC 25922 was included as the control strain in each run of MIC measurements.
The in vitro antibacterial activity of antibiotic combinations assessed by the broth method
The in vitro determination of the inhibitory effect of combination regimens followed the time-killing method was defined by the CLSI17. In brief, bacterial suspensions were diluted to concentrations 5.0×105 colony-forming units (CFU)/mL in fresh Mueller–Hinton broth. Drug concentrations of amikacin, tigecycline and doxycycline were adjusted to those of 1xMIC, 1/2xMIC, and 1/4xMIC. Each drug alone and the combination of amikacin and tigecycline or doxycycline were tested. Bacterial counts were measured at 24 h by enumerating the colonies in 10-fold serially diluted specimens of 100 μL aliquots plated on the nutrient agar (Difco Laboratories, Sparks, MD) at 37 °C.
Definitions
Synergy was defined as a ≥2-log10 decrease in the CFU/ml between the combination and its most active constituent after 24 h and the number of surviving organisms in the presence of the combination must be ≥2 log10 CFU/ml below the starting inoculum. Bacteriostatic activities were defined as the presence of ≥2 log10, but <3 log10 reductions, and bactericidal activities were defined as the presence of ≥3 log10 reductions in the CFU/mL at 24 h, relative to the initial inoculum17. All experiments were performed in duplicate.
The in vitro antibacterial activity of antibiotic combinations assessed by the checkerboard method
To evaluate the effect of the combinations, the fractional inhibitory concentration (FIC) was calculated for each combination by the broth microdilution technique as recommended by the CLSI and as previously described14,18,19. Briefly, the 96-well microdilution plates were inoculated with each test organism to yield the appropriate density (105 CFU/ml) in 100 μl of Mueller-Hinton broth (MHB) and incubated at 35 °C in ambient air for 24 h. One well with no antibiotic was used as a positive growth control on each plate. The plates were read for visual turbidity, and the results were recorded at 35 °C in ambient air using a magnifying mirror reader after 24 h of incubation, as turbidity in the wells indicated the growth of the microorganism. The MIC was determined as the well in the microtiter plate with the lowest drug concentration at which there was no visible growth. The following formulas were used to calculate the FIC index: FIC of drug A = MIC of drug A in combination/MIC of drug A alone, FIC of drug B = MIC of drug B in combination/MIC of drug B alone, and FIC index = FIC of drug A + FIC of drug B. Synergy was defined as a FIC index ≤0.5, indifference was defined as a FIC index >0.5 but ≤4, and antagonism was defined as a FIC index >420. All drug combinations were performed repeatedly to validate the data.
The detection of β-Lactamase genes
Plasmid DNA was extracted as templates and polymerase chain reaction (PCR) was used to amplify CTX-M, TEM, IMI, IMP, VIM, KPC, OXA and NDM using specific primers as previously published21,22,23. For AmpC genes, the following primers were used: (a) CMY-2-forward (TTT TCA AGA ATG CGC CAG GC), CMY-2-reverse (CTG CTG CTG ACA GCC TCT TT); and (b) DHA-1-forward (CTG ATG AAA AAA TCG TTA TC) and DHA-1-reverse (ATT CCA GTG CAC TCA AAA TA). For SHV genes, the following primers were used: (a) SHV-forward (GAT CCA CTA TCG CCA GCA GG) and SHV-reverse (ACC ACA ATG CGC TCT GC TTT G); and (b) SHV-12-forward (ATG CGT TAT ATT CGC CTG TG) and SHV-12-reverse (TTAGCGTTGCCAGTGCTCG). Amplicons were purified with PCR clean-up kits (Roche Diagnostics, GmbH, Penzberg, Germany) and were sequenced on an ABI PRISM3730 sequencer analyzer (Applied Biosystems, Foster City, CA, USA).
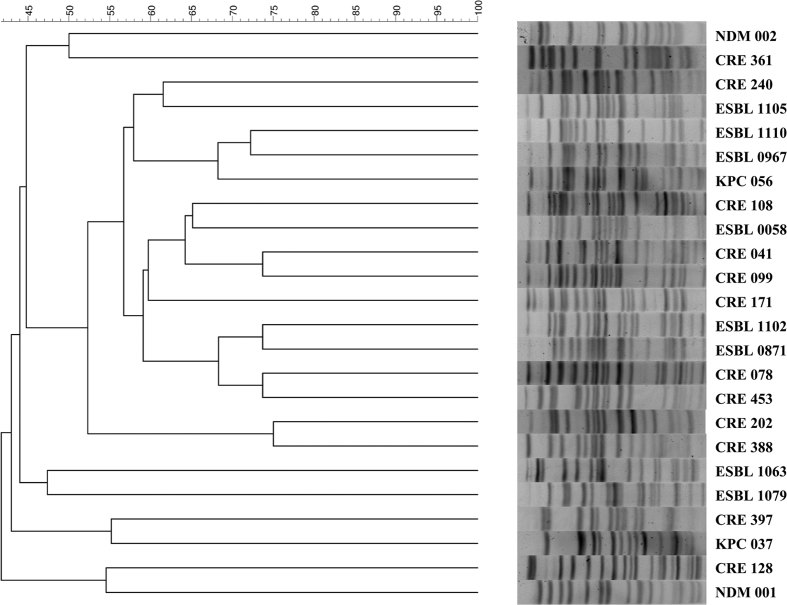
Pulsed-field gel electrophoresis
PFGE was performed as described previously24 with a CHEF DR II apparatus (Bio-Rad Laboratories, Hercules, Calif.). In brief, the DNA in the plugs was digested with XbaI, and electrophoresis was performed in a 1% agarose gel (in 0.5x TBE [Tris-borate-EDTA] buffer). The electrophoretic conditions used were as follows: initial switch time, 2.0 s; final switch time, 35.0 s; run time, 21 h; gradient, 6 V/cm; angle, 120°; and temperature, 14 °C. The bacteriophage lambda ladder pulsed-field grade (PFG) and low-range PFG molecular weight markers were loaded onto all gels. The PFGE patterns were visually examined and interpreted according to the criteria of Tenover et al.25. The similarities of the PFGE profiles of each strain were compared using a Dice coefficient at 1.0% of tolerance and 0.8% of optimization.
Results
Figure 1 shows the PFGE profile of the enrolled 10 ESBL-, 10 carbapenem-resistant-, two KPC-2 producing and 2 NDM- E. coli isolates (one was NDM-1, and the other was NDM-5), and all of them had different PFGE profiles. Table 1 shows their MIC values and the susceptible rates of amikacin, doxycycline, and tigecycline. All of the 24 E. coli isolates were susceptible to amikacin and tigecycline. However, only 30% of ESBL E. coli and 50% of carbapenem-resistant E. coli were susceptible to doxycycline. For doxycycline, both of the NDM positive E. coli had MICs of 64 μg/ml, and in contrast, both KPC-producing E. coli had MIC values ≤ 2 μg/ml.
Figure 1. The PFGE profile of the enrolled 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant-(CRE), 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-producing E. coli isolates.
Table 1. The MIC values and susceptibility rates of amikacin, doxycycline, and tigecycline against 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant-(CRE), 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-producing E. coli isolates.
| Antibiotics | ESBL (N=10) |
CRE (N=10) |
KPC |
NDM |
MIC breakpoint |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC range | susceptible % | MIC range | susceptible % | KPC 037 | KPC 056 | NDM-1 | NDM-2 | S | I | R | |
| Amikacin | 2~16 | 100 | 2~16 | 100 | 8 | 2 | 8 | 2 | ≤16 | 32 | ≥64 |
| Doxycycline | 1~16 | 30 | 2~16 | 50 | 1 | 2 | 64 | 64 | ≤4 | 8 | ≥16 |
| Tigecycline | 0.12~1 | 100 | 0.5~1 | 100 | 0.5 | 0.25 | 1 | 0.25 | ≤2 | 4 | ≥8 |
| Cefazolin | >128 | 0 | >128 | 0 | >128 | >128 | >128 | >128 | ≦2 | 4 | ≧8 |
| Cefmetazole | ≦2~128 | 70 | >128 | 0 | 8 | 4 | >128 | 16 | ≦16 | 32 | ≧64 |
| Cefotaxime | 8~128 | 100 | 32~128 | 0 | 128 | 2 | >128 | >128 | ≦1 | 2 | ≧4 |
| Cefpirome | ≦2~16 | 30 | ≦2~128 | 20 | 4 | ≦2 | 128 | 16 | ≦2 | 4~8a | ≧16 |
| Doripenem | ≦0.06 | 100 | 1~4 | 30 | 8 | 1 | 16 | 1 | ≦1 | 2 | ≧4 |
| Ertapenem | ≦0.06~0.12 | 100 | 4~64 | 0 | 8 | 32 | 32 | 8 | ≦0.5 | 1 | ≧2 |
| Imipenem | 0.25~1 | 100 | 2~16 | 0 | 8 | 4 | 64 | 8 | ≦1 | 2 | ≧4 |
| Merapenem | ≦0.06 | 100 | 1~4 | 20 | 8 | 2 | 16 | 2 | ≦1 | 2 | ≧4 |
aSusceptible-Dose Dependent (SDD).
The ESBL and carbapenemase genes detected among the clinical isolates are presented in Table 2. For ten ESBL E. coli isolates, genes encoding CTX-M were detected for all isolates. Additionally, genes encoding TEM and CMY were detected for three and two isolates, respectively. For ten carbapenem-resistant E. coli isolates, genes encoding CMY were detected for all isolates. However, genes encoding CTX-M and TEM were detected for four and two isolates, respectively. For two KPC-producing E. coli isolates, genes encoding CMT, TEM, and CTX-M were detected for one isolate. For two NDM positive E. coli isolates, both had the gene encoding CMT and TEM, and one had the KPC-2 gene.
Table 2. The extended-spectrum β-lactamase and carbapenemase genes detected among 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant-(CRE), 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-producing E. coli isolates.
| isolates | CMY | TEM | CTX-M | KPC | NDM | othersa | |
|---|---|---|---|---|---|---|---|
| ESBL E. coli | |||||||
| ESBL 0041 | 2 | 1 | 14 | — | — | — | |
| ESBL 0171 | — | — | 27 | — | — | — | |
| ESBL 0871 | — | — | 14 | — | — | — | |
| ESBL 0967 | — | — | 27 | — | — | — | |
| ESBL 1063 | — | — | 24 | — | — | — | |
| ESBL 1079 | — | 1 | 15 | — | — | — | |
| ESBL 1102 | 2 | — | 15 | — | — | — | |
| ESBL 1105 | — | 1 | 24 | — | — | — | |
| ESBL 1110 | — | — | 174 | — | — | — | |
| ESBL 0058 | — | — | 27 | — | — | — | |
| CR E. coli | |||||||
| CRE 078 | 2 | — | — | — | — | — | |
| CRE 099 | 2 | — | — | — | — | — | |
| CRE 108 | 2 | — | 15 | — | — | — | |
| CRE 128 | 2 | — | 14 | — | — | — | |
| CRE 202 | 2 | — | — | — | — | — | |
| CRE 240 | 2 | — | 14 | — | — | — | |
| CRE 361 | 2 | 1 | — | — | — | — | |
| CRE 388 | 2 | 1 | — | — | — | — | |
| CRE 397 | 42 | — | 14,15 | — | — | — | |
| CRE 453 | 2 | — | — | — | — | — | |
| KPC E. coli | |||||||
| KPC 037 | 2b | 1 | 3 | KPC-2 | — | — | |
| KPC 056 | — | — | — | KPC-2 | — | — | |
| NDM E. coli | |||||||
| NDM 001 | 2 | 1 | — | KPC-2 | NDM-1 | — | |
| NDM 002 | 2 | 1 | — | — | NDM-5 | — | |
aIncluding SHV, DHA, VIM, IMP, OXA48.
bInsertion.
The results of the checkerboard methods are shown in Table 3. For the ESBL E. coli, the FIC50/90 of doxycycline and the tigecycline-based combination were 0.375/0.563 and 0.5/0.563, respectively. The synergistic effects of amikacin/doxycycline and amikacin/tigecycline were 80% and 60%, respectively. For carbapenem-resistant E. coli, the FIC50/90 of doxycycline and the tigecycline-based combination were 0.375/0.5, and 0.5/0.563, respectively. The synergistic effects of amikacin/doxycycline and amikacin/tigecycline were 90% and 80%, respectively. For both, there was no antagonism among the two combinations. For the two KPC E. coli and the two NDM E. coli, the FIC index values of amikacin/doxycycline were 0.5/0.375 and 0.5/0.281, respectively, and the FIC index values of amikacin/tigecycline were 0.375/0.5 and 0.265/0.312, respectively.
Table 3. The results of the checkerboard method of amikacin-based combinations with doxycycline and tigecycline against 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant-(CRE), 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-producing E. coli isolates.
| ESBL | CRE | KPC | NDM | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| range | FIC50 | FIC90 | S | I | A | range | FIC50 | FIC90 | S | I | A | FIC | FIC | FIC | FIC | |
| Amikacin/Doxycycline | 0.25~0.625 | 0.375 | 0.563 | 80 | 20 | 0 | 0.25~0.563 | 0.375 | 0.5 | 90 | 10 | 0 | 0.5 | 0.375 | 0.5 | 0.281 |
| Amikacin/Tigecycline | 0.31~0.75 | 0.5 | 0.563 | 60 | 40 | 0 | 0.375~0.563 | 0.5 | 0.563 | 80 | 20 | 0 | 0.375 | 0.5 | 0.265 | 0.312 |
S, I, R: Synergy (%), Indifference (%), Antagonism (%).
The in vitro activities of the combination of amikacin and doxycycline at the drug concentrations of 1xMIC, 1/2xMIC and 1/4x MIC against each isolate are shown in Table 4. For ESBL E. coli, the reduction of CFU at 24 hours ranged from 2.99 to 4.2, 0.05–4.2, and 0.29–4.08 log10, at concentrations of 1x, 1/2x and 1/4xMIC, respectively. The combinations of amikacin and doxycycline exhibited bactericidal effects against 90%, 70%, and 10% of the tested isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. These combinations were synergistic against 80%, 80%, and 10% of the isolates at the concentrations of 1x, 1/2x and 1/4xMIC, respectively. For carbapenem-resistant E. coli isolates, the reduction of CFU at 24 hours ranged from 0.28 to 3.79, 0.23–3.53 and 0.73–2.00 log10, at concentrations of 1x, 1/2x and 1/4xMIC, respectively. The combinations of amikacin and doxycycline exhibited bactericidal effects against 90%, 50%, and 10% of the tested isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. These combinations were synergistic against 60%, 80%, and 10% of the isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. For KPC E. coli, at the concentration of the 1x MIC combination, one of two strains had a synergistic effect, and the reduction of the CFU at 24 hours compared to the initial inoculum was 3.79 log10 and was −3.94 compared to most active antibiotic. At the concentration of 1/2x MIC, both strains had synergistic effects, and the reduction of the CFU at 24 hours compared to the initial inoculum was 3.79/2.10 log10 and was 6.45/4.49 compared to the most active antibiotic. Both strains had synergistic effects. The NDM strain combinations of amikacin and doxycycline were not performed because the MIC of doxycycline was too high.
Table 4. The log change (log10 CFU/ml) from the starting inoculum and the most active single agent after 24 h of incubation with different concentrations of antibiotics combinations including 1x, 1/2x and 1/4x MICs of amikacin, doxycycline and tigecycline for 10 extended-spectrum β-lactamase (ESBL)-, 10 carbapenem-resistant-, 2 New Delhi Metallo-beta-lactamase (NDM)- and 2 Klebsiella pneumoniae carbapenemase (KPC)-producing E. coli isolates.
| (a) ESBL | Synergism(%) | -cidal/ -static(%)a | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Colony changes (log10 CFU/mL) at 24 h | |||||||||||||
| ESBL0041 | ESBL0058 | ESBL0171 | ESBL0871 | ESBL0967 | ESBL1063 | ESBL1079 | ESBL1102 | ESBL1105 | ESBL1110 | ||||
| 1xAMK+1xDOX | vs. initial inoculum | −3.76 | −4.08 | −3.73 | −3.82 | −4.20 | −3.88 | −3.79 | −2.99 | −3.51 | −3.73 | 80 | 90/10 |
| vs. most active drug | −2.51 | 0.00 | −5.83 | −3.81 | −2.66 | −3.44 | −1.73 | −2.90 | −3.93 | −4.90 | |||
| 1/2xAMK+1/2xDOX | vs. initial inoculum | −3.76 | −4.08 | 0.82 | −2.62 | −4.20 | −3.88 | −3.79 | −0.05 | −3.51 | −3.73 | 80 | 70/10 |
| vs. most active drug | −5.83 | −6.81 | −2.22 | −5.00 | −6.95 | −6.15 | −6.34 | −2.98 | −5.92 | −6.76 | |||
| 1/4xAMK+1/4xDOX | vs. initial inoculum | 0.00 | −4.08 | 3.09 | 1.60 | −0.54 | 0.06 | 1.76 | 3.24 | −1.51 | −0.29 | 10 | 10/0 |
| vs. most active drug | −2.94 | −6.70 | 0.48 | −1.59 | −3.07 | −1.66 | −1.32 | 0.00 | −5.00 | −3.55 | |||
| 1xAMK+1xTGC | vs. initial inoculum | −3.64 | −3.56 | −3.60 | −3.51 | −3.51 | −3.70 | −3.45 | −2.18 | −3.68 | −3.72 | 50 | 90/10 |
| vs. most active drug | −2.60 | −0.9 | −2.53 | −2.34 | −1.00 | 0.00 | −4.87 | 1.51 | −1.83 | −3.34 | |||
| 1/2xAMK+1/2xTGC | vs. initial inoculum | −3.64 | −3.56 | −3.60 | −3.51 | −3.51 | −3.70 | −2.07 | −3.68 | −3.68 | −3.72 | 100 | 90/10 |
| vs. most active drug | −5.95 | −5.90 | −5.86 | −7.00 | −6.34 | −5.90 | −5.12 | −4.86 | −3.51 | −3.81 | |||
| 1/4xAMK+1/4xTGC | vs. initial inoculum | 3.16 | 3.44 | −0.87 | 3.21 | −0.64 | 0.78 | 3.25 | −1.27 | −3.68 | −3.41 | 20 | 20/0 |
| vs. most active drug | 0.16 | 0.55 | −4.24 | 0.30 | −3.69 | −1.97 | 0.80 | −4.33 | −6.41 | −6.54 | |||
| (b) CRE | |||||||||||||
| Colony changes (log10 CFU/mL) at 24 h | Synergism(%) | -cidal/ -static(%)a | |||||||||||
| CRE078 | CRE099 | CRE108 | CRE128 | CRE202 | CRE240 | CRE361 | CRE388 | CRE397 | CRE453 | ||||
| 1xAMK+1xDOX | vs. initial inoculum | −3.53 | −3.51 | −3.48 | −3.78 | −3.51 | −3.15 | −3.79 | −3.76 | −3.00 | −0.28 | 60 | 90/0 |
| vs. most active drug | 0.00 | −2.78 | −2.56 | 0.00 | −1.45 | −5.04 | −3.99 | −3.60 | −3.54 | −0.09 | |||
| 1/2xAMK+1/2xDOX | vs. initial inoculum | −3.53 | −2.73 | −2.33 | −0.78 | −3.51 | −3.45 | −3.01 | −3.46 | −2.15 | −0.23 | 80 | 50/30 |
| vs. most active drug | −5.41 | −4.12 | −5.13 | −2.45 | −6.20 | −5.15 | −5.56 | −5.68 | −5.55 | −3.70 | |||
| 1/4xAMK+1/4xDOX | vs. initial inoculum | −0.73 | 2.05 | 2.7 | 2.73 | 3.35 | 1.97 | 1.92 | −1.03 | −2.00 | 3.47 | 10 | 0/10 |
| vs. most active drug | −1.57 | −1.44 | −0.37 | −0.45 | 0.44 | −0.38 | 0.92 | −1.71 | −5.28 | 0.00 | |||
| 1xAMK+1xTGC | vs. initial inoculum | −3.53 | −3.20 | −3.82 | −3.68 | −3.51 | −3.45 | −3.79 | −3.76 | −3.60 | −1.12 | 30 | 90/0 |
| vs. most active drug | 0.00 | −2.49 | −0.30 | −1.89 | −1.45 | −1.08 | −2.56 | −2.90 | −0.78 | −2.84 | |||
| 1/2xAMK+1/2xTGC | vs. initial inoculum | −3.53 | −2.00 | −3.82 | −3.68 | −3.51 | −2.54 | −3.79 | −3.76 | −3.60 | −2.45 | 100 | 70/30 |
| vs. most active drug | −7.00 | −5.09 | −3.79 | 6.34 | −6.38 | −4.24 | −5.51 | −3.66 | −5.95 | −5.80 | |||
| 1/4xAMK+1/4xTGC | vs. initial inoculum | 1.61 | 3.3 | −1.56 | 2.02 | 1.70 | 3.13 | 2.76 | 2.74 | −0.30 | 3.17 | 0 | 0/0 |
| vs. most active drug | 0.77 | −0.14 | −4.12 | −0.16 | −1.05 | 0.79 | 1.76 | 2.06 | −3.62 | 0.04 | |||
| (c) KPC/NDM | |||||||||||||
| KPC | NDM | ||||||||||||
| Colony changes (log10 CFU/mL) at 24 h | synergism (%) | -cidal/-static (%)a | Colony changes (log10 CFU/mL) at 24 h | synergism (%) | -cidal/-static (%)a | ||||||||
| KPC 037 | KPC 056 | NDM 001 | NDM 002 | ||||||||||
| 1xAMK+1xDOX | vs. initial inoculum | −3.79 | −3.79 | 50 | 100/0 | ND | ND | ND | ND | ||||
| vs. most active drug | −0.30 | −3.94 | ND | ND | |||||||||
| 1/2xAMK+1/2xDOX | vs. initial inoculum | −3.79 | −2.10 | 100 | 50/50 | ND | ND | ND | ND | ||||
| vs. most active drug | −6.45 | −4.49 | ND | ND | |||||||||
| 1/4xAMK+1/4xDOX | vs. initial inoculum | 3.14 | 1.79 | 0 | 0/0 | ND | ND | ND | ND | ||||
| vs. most active drug | −0.01 | −1.18 | ND | ND | |||||||||
| 1xAMK+1xTGC | vs. initial inoculum | −3.73 | −3.53 | 0 | 100/0 | −4.00 | −3.68 | 50 | 100/0 | ||||
| vs. most active drug | −1.82 | −1.58 | −2.38 | 0.00 | |||||||||
| 1/2xAMK+1/2xTGC | vs. initial inoculum | −3.73 | −3.53 | 100 | 100/0 | −4.00 | −3.68 | 100 | 100/0 | ||||
| vs. most active drug | −2.56 | −6.15 | −6.45 | −6.68 | |||||||||
| 1/4xAMK+1/4xTGC | vs. initial inoculum | 3.00 | −0.33 | 0 | 0/0 | 2.68 | −0.93 | 0 | 0/0 | ||||
| vs. most active drug | 0.18 | −3.53 | 0.10 | −3.90 | |||||||||
-cidal refers to the bactericidal effect and -static refers to the bacteriostatic effect. ND refers to not done.
a-cidal refers to bactericidal effect and -static refers to bacteriostatic effect. ND refers to not done.
The in vitro activities of combinations of amikacin and tigecycline at the drug concentrations of 1xMIC, 1/2xMIC and 1/4x MIC against each isolate are also shown in Table 4. For ESBL-E. coli, the reduction of CFU at 24 hours ranged from 2.18 to 3.72, 1.77–3.72 and 0.87–3.68 log10, at concentrations of 1x, 1/2x and 1/4xMIC, respectively. The combinations of amikacin and tigecycline exhibited bactericidal effects against 90%, 90%, and 20% of the tested isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. These combinations were synergistic against 50%, 100%, and 20% of the isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. For carbapenem-resistant E. coli, the reduction of CFU at 24 hours ranged from 1.12 to 3.82, 2.00–3.82 and 0.30–1.56 log10, at concentrations of 1x, 1/2x and 1/4xMIC, respectively. The combinations of amikacin and tigecycline exhibited bactericidal effects against 90%, 70%, and 0% of the tested isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. These combinations were synergistic against 30%, 100%, and 0% of the isolates at concentrations of 1x, 1/2x and 1/4xMIC, respectively. For KPC E. coli, at the combined concentrations of 1x MIC and 1/4 x MIC, both two strains have no synergistic effect. At the combined concentration of 1/2x MIC, both strains had synergistic effects and with a value of 2.56/6.15 log10 compared to most active antibiotic. The reduction of CFU at 24 hours compared to the initial inoculum was 3.73/3.53 log10, exhibiting a bactericidal effect. One of the two NDM strains at the combined concentration of 1x MIC had a synergistic effect, and the reduction of CFU at 24 hours compared to the initial inoculum was 4.00 log10 was −2.38/0 log10 compares to the most active antibiotic. At the combined concentration of 1/2x MIC, both strains had a synergistic effect, and the reduction of CFU at 24 hours compared to the initial inoculum was 4.00/3.68 log10 and was 6.45/6.58 log10 compared to the most active antibiotic. However, no synergistic effect was noted at the combined 1/4 x MIC.
Discussion
Antibiotic combination therapy has become the possible resolution for the treatment of severe multidrug resistant organism infections, and various antibiotic combination regimens for treating multidrug resistant E. coli have been recommended based on in vitro and in vivo studies. However, research investigating the in vitro antibacterial activity of the combinations of an aminoglycoside (amikacin) and tigecycline or doxycycline against multidrug-resistant E. coli isolates is scarce. This is the first study to assess this type of combined antibiotic regimen against multidrug-resistant E. coli, including ESBL-, carbapenem-resistant, NDM- and KPC-producing E. coli isolates. Based on this in vitro study, we have several significant findings. Most important, although tigecycline and amikacin displayed greater in vitro activities against multidrug-resistant E. coli than doxycycline, the synergistic effect seems to be similar between the combination of doxycycline and amikacin and the combination of tigecycline plus amikacin. As doxycycline is safe, inexpensive, and almost universally availability, further large in vitro and in vivo studies are warranted to clarify its role as a new adjunctive therapy to improve the outcomes of multidrug-resistant E. coli infections.
Although doxycycline is a cheap antimicrobial agent, it exhibits a broad spectrum of activity against different pathogens, including Gram-negative bacteria, and remains as a useful or even drug of choice in the treatment of many infectious diseases26,27. Even in this era of the increasing prevalence of multidrug-resistant organism infections, doxycycline is efficacious against multidrug-resistant A. baumannii28, Pseudomonas aeruginosa29, and Stenotrophomonas maltophilia30. In this first study investigating the in vitro activity of doxycycline against multidrug-resistant E. coli, we found that most clinical isolates, including seven (70%) ESBL-, five (50%) carbapenem-resistant and two (100%) NDM - E. coli, were not susceptible to doxycycline. However, even sub-inhibitory concentrations of an aminoglycoside combined with doxycycline can exhibit synergistic activities against more than 80% of tested isolates. For this combination, using 1/2xMIC of doxycycline (2 μg/mL, which is achievable in serum) produces the best synergism7,31. Therefore, our findings indicate the potential role of doxycycline-containing combinations in the management of multidrug-resistant E. coli infections.
Tigecycline, the first glycylcycline, exhibits potent activity against a wide range of clinically significant gram-positive and gram-negative bacteria, including multidrug-resistant strains (e.g., oxacillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci, and ESBL-producing Enterobacteriaceae), and anaerobes (e.g., Bacteroides spp)32. Like several previous studies33,34,35, we found that the MIC values of tigecycline against all tested isolates remained low (≤1 μg/mL), and all of the tested isolates were susceptible to tigecycline. However, in vitro activity does not equate to an in vivo response, and the current suggested dosage of tigecycline for adults only achieves low serum concentrations; therefore, tigecycline cannot be recommend for the treatment of bloodstream infections, even those caused by so called “tigecycline-susceptible” isolates. To overcome this barrier to the treatment of critical conditions and the emergent tigecycline-resistant strains, tigecycline-containing combinations have been proposed as possible solutions. In this study, we found that using 1/2xMIC of tigecycline (0.5 μg/mL) in combination with sub-inhibitory concentrations of an aminoglycoside, synergism can be achieved for all of the 24 tested isolates. However, if we use 1/4xMICs of tigecycline (0.25 μg/mL) in combination with 1/4xMICs of an aminoglycoside, synergism was found for only two of the tested isolates. A previous study showed that the serum attainable concentration of tigecycline was only 0.38 and 0.93 μg/mL after a single dose injection of 50 mg and 100 mg tigecycline, respectively36. Therefore, if we formulate tigecycline-containing combination regimens based on the recommended dosages (100 mg loading, followed by 50 mg every 12 h), we can obtain the synergistic effect with tigecycline and amikacin despite low serum levels of tigecycline (<1 μg/mL).
In this study, we found an unusual association between NDM-1 and KPC-2 in one E. coli isolates, and it is the first detection of this combination in Taiwan. As previously reported37, this isolate should be multi-drug resistant against most antibiotics, excluding tigecycline. Previous studies only found this double carbapenemase-producer in K. pneumoniae, E. cloacae, Citrobacter freundii and Enterobacter hormaechei isolates from Brazil, Pakistan, China, and India38,39,40,41,42. However, we did not find the mutation of outer membrane porin (Omp) in KPC or NDM-producing isolates. As previous reports43,44,45, we found that the mutation of OmpA, OmpC, or OmpF was only presented in carbapenem-resistant strains. Overall, all of these findings indicate the worldwide emergence of double, or even multiple, carbapenemase-producing bacteria among Enterobacteriacae, including in Taiwan.
Finally, recent studies46,47 showed that the different resistance mechanisms of multidrug-resistant organisms may influence the synergistic effects of combination therapy. For carbapenem-resistant K. pneumoniae, Laishram et al.46 found that isolates producing NDM carbapenemase alone showed significantly more synergy than isolates producing OXA-48-like carbapenemase. Furthermore, Hong et al.47 found that clinical isolates of KPC-producing K. pneumoniae with high porin expression were more responsive to a combination of colistin-doripenm-ertapenem than isolates with low expression (100% [8/8] vs 0% [0/4]; p = 0.002). In this study of limited clinical isolates, we did not assess whether the MDR E. coli with different resistant mechanisms had different responses to antibiotic combination therapy. However, further investigations are warranted to clarify this issue.
In conclusion, despite the lower susceptible rate of doxycycline, the antibacterial activity of such an ancient antimicrobial agent can be enhanced by the addition of amikacin. The synergistic effect of such combinations seems to be as effective as the tigecycline/amikacin combination against most multidrug-resistant E. coli isolates, and warrants further in vivo investigation to confirm their therapeutic efficacy.
Additional Information
How to cite this article: Lai, C.-C. et al. The role of doxycycline in the therapy of multidrug-resistant E. coli – an in vitro study. Sci. Rep. 6, 31964; doi: 10.1038/srep31964 (2016).
Footnotes
Author Contributions H.-J.T. is the guarantor of this manuscript, C.-C.L., C.-C.C., H.-L.H. and Y.-C.C. contributed to the conception and design of the study, C.-C.C. and H.-J.T. analysed and interpreted the data, C.-C.L. and H.-J.T. drafted the manuscript. All authors reviewed the manuscript.
References
- Kanj S. S. & Kanafani Z. A. Current concepts in antimicrobial therapy against resistant gram-negative organisms: extended-spectrum beta-lactamase-producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and multidrug-resistant Pseudomonas aeruginosa. Mayo Clin. Proc. 86, 250–259, doi: 10.4065/mcp.2010.0674 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falagas M. E., Karageorgopoulos D. E. & Nordmann P. Therapeutic options for infections with Enterobacteriaceae producing carbapenem-hydrolyzing enzymes. Future Microbiol. 6, 653–666, doi: 10.2217/fmb.11.49 (2011). [DOI] [PubMed] [Google Scholar]
- Doi Y. & Paterson D. L. Carbapenemase-producing Enterobacteriaceae. Semin. Respir. Crit. Care Med. 36, 74–84, doi: 10.1055/s-0035-1544208 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkotou O. et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin. Microbiol. Infect 17, 1798–1803, doi: 10.1111/j.1469-0691.2011.03514.x (2011). [DOI] [PubMed] [Google Scholar]
- Qureshi Z. A. et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob. Agents Chemother. 56, 2108–2113, doi: 10.1128/aac.06268-11 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumbarello M. et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin. Infect Dis. 55, 943–950, doi: 10.1093/cid/cis588 (2012). [DOI] [PubMed] [Google Scholar]
- Tang H. J. et al. Colistin-sparing regimens against Klebsiella pneumoniae carbapenemase-producing K. pneumoniae isolates: Combination of tigecycline or doxycycline and gentamicin or amikacin. J. Microbiol. Immunol. Infect. (in press) (2016). [DOI] [PubMed]
- Tzouvelekis L. S., Markogiannakis A., Piperaki E., Souli M. & Daikos G. L. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin. Microbiol. Infect 20, 862–872, doi: 10.1111/1469-0691.12697 (2014). [DOI] [PubMed] [Google Scholar]
- Izadpanah M. & Khalili H. Antibiotic regimens for treatment of infections due to multidrug-resistant Gram-negative pathogens: An evidence-based literature review. J. Res. Pharm. Pract. 4, 105–114, doi: 10.4103/2279-042x.162360 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamma P. D., Cosgrove S. E. & Maragakis L. L. Combination therapy for treatment of infections with gram-negative bacteria. Clin. Microbiol. Rev. 25, 450–470, doi: 10.1128/cmr.05041-11 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollef M. H., Golan Y., Micek S. T., Shorr A. F. & Restrepo M. I. Appraising contemporary strategies to combat multidrug resistant gram-negative bacterial infections–proceedings and data from the Gram-Negative Resistance Summit. Clin. Infect. Dis. 53 Suppl 2, S33–55; quiz S56–38, doi: 10.1093/cid/cir475 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing, 9th informational supplement. M100-S24. National Committee for Clinical Laboratory Standards, Wayne, Pa. (2014). [Google Scholar]
- Ma L. et al. Updated molecular epidemiology of carbapenem-non-susceptible Escherichia coli in Taiwan: first identification of KPC-2 or NDM-1-producing E. coli in Taiwan. BMC infect. Dis. 13, 599, doi: 10.1186/1471-2334-13-599 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- CLSI. Performance standards for antimicrobial susceptibility testing. Document M100-S24. Wayne, PA CLSI. (2014). [Google Scholar]
- Brown S. D. & Traczewski M. M. Comparative in vitro antimicrobial activity of tigecycline, a new glycylcycline compound, in freshly prepared medium and quality control. J. Clin. Microbiol. 45, 2173–2179, doi: 10.1128/jcm.02351-06 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- CLSI. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically—Eighth Edition Approved Standard M07-A9. CLSI, Wayne, PA, USA. (2009). [Google Scholar]
- National Committee for Clinical Laboratory Standards. Methods for determining bactericidal activity of antimicrobial agents; approved guideline. Document M26-A. Wayne, PA NCCLS. (1999). [Google Scholar]
- Eliopoulos G. M. & a. R. C. M. Jr. In V. Lorian. Antibiotics in laboratory medicine, 4th ed. The Williams & Wilkins Co., Baltimore, Md. Antimicrobial combinations. 330–396 (1996).
- JA M. Synergy testing: broth microdilution checkerboard and broth macrodilution methods, p. 5.18.1–5.18.23. In Eisenberg H. D. (ed.), Clinical microbiology procedures handbook. American Society for Microbiology, Washington, D.C. (1992). [Google Scholar]
- White R. L., Burgess D. S., Manduru M. & Bosso, J. A. Comparison of three different in vitro methods of detecting synergy: time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 40, 1914–1918 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Queenan A. M. & Bush K. Carbapenemases: the versatile beta-lactamases. Clin. Microbiol. Rev. 20, 440–458 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckert C. et al. Dissemination of CTX-M-type beta-lactamases among clinical isolates of Enterobacteriaceae in Paris, France. Antimicrob. Agents Chemother. 48, 1249–1255 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poirel L., Revathi G., Bernabeu S. & Nordmann P. Detection of NDM-1-producing Klebsiella pneumoniae in Kenya. Antimicrob. Agents Chemother. 55, 934–936, doi: 10.1128/aac.01247-10 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejrnaes K. et al. Pulsed-field gel electrophoresis typing of Escherichia coli strains from samples collected before and after pivmecillinam or placebo treatment of uncomplicated community-acquired urinary tract infection in women. J. Clin. Microbiol. 44, 1776–1781, (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenover F. C. et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol 33, 2233–2239 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler T., Winkler C., Wege K. & Schmechel H. Doxycycline–the forgotten antibiotic. Med. Klin. (Munich). 95, 629–631 (2000). [DOI] [PubMed] [Google Scholar]
- Zhanel G. G. et al. The glycylcyclines: a comparative review with the tetracyclines. Drugs 64, 63–88 (2004). [DOI] [PubMed] [Google Scholar]
- Falagas M. E., Vardakas K. Z., Kapaskelis A., Triarides N. A. & Roussos N. S. Tetracyclines for multidrug-resistant Acinetobacter baumannii infections. Int. J. Antimicrob. Agents. 45, 455–460, doi: 10.1016/j.ijantimicag.2014.12.031 (2015). [DOI] [PubMed] [Google Scholar]
- Timurkaynak F. et al. In vitro activities of non-traditional antimicrobials alone or in combination against multidrug-resistant strains of Pseudomonas aeruginosa and Acinetobacter baumannii isolated from intensive care units. Int. J. Antimicrob. Agents. 27, 224–228, doi: 10.1016/j.ijantimicag.2005.10.012 (2006). [DOI] [PubMed] [Google Scholar]
- Wood G. C., Underwood E. L., Croce M. A., Swanson J. M. & Fabian T. C. Treatment of recurrent Stenotrophomonas maltophilia ventilator-associated pneumonia with doxycycline and aerosolized colistin. Ann. Pharmacother. 44, 1665–1668, doi: 10.1345/aph.1P217 (2010). [DOI] [PubMed] [Google Scholar]
- Hirsch E. B. & Tam V. H. Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection. J. Antimicrob. Chemother. 65, 1119–1125, doi: 10.1093/jac/dkq108 (2010). [DOI] [PubMed] [Google Scholar]
- Doan T. L., Fung H. B., Mehta D. & Riska P. F. Tigecycline: a glycylcycline antimicrobial agent. Clin. Ther. 28, 1079–1106, doi: 10.1016/j.clinthera.2006.08.011 (2006). [DOI] [PubMed] [Google Scholar]
- Xu A. et al. National epidemiology of carbapenem-resistant and extensively drug-resistant Gram-negative bacteria isolated from blood samples in China in 2013. Clin. Microbiol Infect. doi: 10.1016/j.cmi.2015.09.015 (2016). [DOI] [PubMed] [Google Scholar]
- Ozkok S. et al. In vitro susceptibility of tigecycline against multidrug-resistant gram-negative strains: Etest versus agar dilution. Chemother. 60, 151–156, doi: 10.1159/000375440 (2014). [DOI] [PubMed] [Google Scholar]
- Chen Y. H. et al. Trends in the susceptibility of clinically important resistant bacteria to tigecycline: results from the Tigecycline in vitro Surveillance in Taiwan study, 2006 to 2010. Antimicrob. Agents Chemother. 56, 1452–1457, doi: 10.1128/aac.06053-11 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meagher A. K., Ambrose P. G., Grasela T. H. & Ellis-Grosse E. J. Pharmacokinetic/pharmacodynamic profile for tigecycline-a new glycylcycline antimicrobial agent. Diagn. Microbiol. Infect. Dis. 52, 165–171, doi: 10.1016/j.diagmicrobio.2005.05.006 (2005). [DOI] [PubMed] [Google Scholar]
- Meletis G., Chatzidimitriou D. & Malisiovas N. Double- and multi-carbapenemase-producers: the excessively armored bacilli of the current decade. Eur. J. Clin. Microbiol. Infect. Dis. 34, 1487–1493, doi: 10.1007/s10096-015-2379-9 (2015). [DOI] [PubMed] [Google Scholar]
- Pereira P. S. et al. Coproduction of NDM-1 and KPC-2 in Enterobacter hormaechei from Brazil. Microbial. Drug Resist. 21, 234–236, doi: 10.1089/mdr.2014.0171 (2015). [DOI] [PubMed] [Google Scholar]
- Quiles M. G. et al. Unusual association of NDM-1 with KPC-2 and armA among Brazilian Enterobacteriaceae isolates. Braz. J. Med. Biol. Res. 48, 174–177, doi: 10.1590/1414-431x20144154 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattar H., Toleman M., Nahid F. & Zahra R. Co-existence of bla and bla in clinical isolates of Klebsiella pneumoniae from Pakistan. J. Chemother. 1973947814y0000000223, doi: 10.1179/1973947814y.0000000223 (2014). [DOI] [PubMed] [Google Scholar]
- Kumarasamy K. & Kalyanasundaram A. Emergence of Klebsiella pneumoniae isolate co-producing NDM-1 with KPC-2 from India. J. Antimicrobial. Chemother. 67, 243–244, doi: 10.1093/jac/dkr431 (2012). [DOI] [PubMed] [Google Scholar]
- Poirel L., Heritier C., Spicq C. & Nordmann P. In vivo acquistion of high-level resistance to imipenem in Escherichia coli. J. Clin. Microbiol. 42, 3831–3833 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L. et al. Updated molecular epidemiology of carbapenem-non-susceptible Escherichia coli in Taiwan: first identification of KPC-2 or NDM-1-producing E. coli in Taiwan. BMC Infect. Dis. 13, 599 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia J. H. et al. Emergence of carbapenem-resistant Escherichia coli in Taiwan: resistance due to combined CMY-2 production and porin deficiency. J. Chemother. 21, 621–626 (2009). [DOI] [PubMed] [Google Scholar]
- Feng J. et al. Coexistence of a novel KPC-2-encoding MDR plasmid and an NDM-1-encoding pNDM-HN380-like plasmid in a clinical isolate of Citrobacter freundii. J. Antimicrobial. Chemother. 70, 2987–2991, doi: 10.1093/jac/dkv232 (2015). [DOI] [PubMed] [Google Scholar]
- Laishram S. et al. Determination of synergy between sulbactam, meropenem and colistin in carbapenem-resistant Klebsiellapneumoniae and Acinetobacter baumannii isolates and correlation with the molecular mechanism of resistance. J. Chemother. 2015 Oct 2:1973947815Y0000000079. [Epub ahead of print]. [DOI] [PubMed]
- Hong J. H. et al. Characterization of porin expression in Klebsiella pneumoniae Carbapenemase (KPC)-producing K. pneumoniae identifies isolates most susceptible to the combination of colistin and carbapenems. Antimicrob. Agents Chemother. 57, 2147–2153 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]