Abstract
Study Objectives:
Obstructive sleep apnea (OSA) promotes myocardial electrical instability and may predispose to nocturnal sudden cardiac death. We evaluated whether hypobaric hypoxia during altitude travel further impairs cardiac repolarization in patients with OSA, and whether this is prevented by acetazolamide, a drug known to improve oxygenation and central sleep apnea at altitude.
Methods:
Thirty-nine OSA patients living < 600 m, discontinued continuous positive airway pressure therapy during studies at 490 m and during two sojourns of 3 days at altitude (2 days at 1860 m, 1 day at 2590 m). During one altitude sojourn, patients took acetazolamide, during the other placebo, or vice versa, according to a randomized, double-blind crossover design. Twelve-lead electrocardiography and pulse oximetry (SpO2) were recorded during nocturnal polysomnography. Heart rate corrected mean QT intervals during the entire night (meanQTc) and during 1 min of the night with the longest meanQTc (maxQTc) were determined.
Results:
At 490 m the median nocturnal SpO2 was 93%, medians of meanQTc and maxQTc were 420 ms and 478 ms. At 2590 m, on placebo, SpO2 was lower (85%), and meanQTc and maxQTc were prolonged to 430 ms and 510 ms (P < 0.02 vs. 490 m, all corresponding comparisons). At 2590 m on acetazolamide, median SpO2 was increased to 88% (P < 0.05 vs. placebo), meanQTc was reduced to 427 ms (P < 0.05 vs. placebo), whereas maxQTc remained increased at 502 ms (P = ns vs. placebo).
Conclusions:
At 2590 m OSA patients experienced cardiac repolarization disturbances in association with hypoxemia. Prolongation of meanQTc at altitude was prevented and hypoxemia was improved by acetazolamide, whereas maxQTc remained increased suggesting imperfect protection from repolarization disturbances.
Clinical Trial Registration:
ClinicalTrials.gov ID: NTC-00714740. URL: www.clinicaltrials.gov
Citation:
Latshang TD, Kaufmann B, Nussbaumer-Ochsner Y, Ulrich S, Furian M, Kohler M, Thurnheer R, Saguner AM, Duru F, Bloch KE. Patients with obstructive sleep apnea have cardiac repolarization disturbances when travelling to altitude: randomized, placebo-controlled trial of acetazolamide. SLEEP 2016;39(9):1631–1637.
Keywords: sleep apnea, cardiac arrhythmias, cardiac repolarization, sudden cardiac death, altitude
Significance.
Obstructive sleep apnea (OSA) is a highly prevalent disorder associated with considerable cardiovascular morbidity and mortality. The current randomized placebo-controlled trial demonstrates that patients with OSA who discontinued continuous positive airway pressure (CPAP) therapy during a stay at moderate altitude suffer from disturbed cardiac repolarization with a prolongation of the QTc interval and greater dispersion, suggesting an increase in the risk of malignant arrhythmias. Because acetazolamide prevents prolongation of the mean QTc interval, the drug might be beneficial for OSA patients who are unable to use CPAP therapy during altitude travel. The results are important because they might have an effect on the clinical practice and because the study provides novel insights into the pathophysiology of cardiac repolarisation and control of breathing.
INTRODUCTION
Obstructive sleep apnea (OSA) is a highly prevalent sleep-related breathing disorder with prevalence rates of 5% to 19 % of the adult population in Western countries.1–3 OSA is characterized by repetitive interruption of airflow through the pharyngeal airway during sleep, leading to oxygen desaturations, fragmented sleep, and excessive daytime sleepiness. Patients with OSA are at increased risk of hypertension and vascular dysfunction4–7 and there is evidence that OSA is associated with cardiac arrhythmias and sudden cardiac death, especially in the early morning hours.8–12 Approximately 50% of patients with symptomatic OSA have cardiac arrhythmias during sleep, mostly associated with an episode of obstructive apnea.13 Intermittent hypoxia caused by OSA is assumed to promote cardiac arrhythmias by producing oxidative stress, systemic inflammation, and increased sympathetic activity.6 Withdrawal of continuous positive airway pressure (CPAP) in patients with OSA7 and simulated obstructive apnea in healthy subjects14 are associated with QTc prolongation, suggesting that the cardiac arrhythmia in OSA patients may be mediated by disturbances of cardiac repolarization.8
Many patients with OSA travel to altitude for professional or recreational activities. We have previously shown that altitude exposure aggravates nocturnal hypoxemia and exacerbates sleep apnea in OSA patients, and may therefore further increase the risk of cardiac repolarization disturbances and arrhythmia.15 Although nocturnal CPAP therapy may improve oxygen saturation and sleep apnea, many OSA patients prefer to discontinue this treatment during altitude travel because carrying a CPAP device is inconvenient and electrical power is not always available. Acetazolamide therapy in combination with CPAP, or as the sole treatment if CPAP is not feasible, confers some benefit to OSA patients during altitude travel because it improves nocturnal oxygen saturation, sleep apnea, and subjective sleep quality.16,17 However, whether acetazolamide therapy may reduce or prevent disturbances of cardiac repolarization and arrhythmias in OSA patients staying at altitude has not been studied. Therefore, the purpose of the current study was to perform a randomized, placebo-controlled trial evaluating the hypotheses that (1) cardiac repolarization as reflected by a prolonged QTc interval is disturbed in OSA patients during a stay at altitude, and (2) that the altitude-induced QTc prolongation is prevented by acetazolamide therapy.
METHODS
Study Design
This randomized, placebo-controlled, double-blind crossover trial evaluated the effects of a 3-day altitude sojourn on indices of cardiac repolarization in OSA patients discontinuing their long-term CPAP therapy; in addition, the efficacy of acetazolamide in preventing the effects of altitude on cardiac repolarization was tested. As described in detail previously,16 the trial included two altitude sojourns of 3 days each, one with acetazolamide, the other with placebo treatment, or vice versa, according to a randomized crossover design, separated by a 2-w washout period at < 600m (see next section). The study was approved by the institutional ethics committee, registered at clinicaltrials.gov NCT00714740, and all patients gave written informed consent. The primary outcomes of the trial (apnea-hypopnea index and nocturnal oxygen saturation) are reported in detail elsewhere,16 and the data on cardiac repolarization, the focus of the current report, have not been published previously.
Setting and Participants
Baseline studies were carried out at the University Hospital in Zurich, Switzerland (490 m, barometric pressure 717 mmHg), altitude measurements were performed in the Swiss mountain resorts Davos Schatzalp (1860 m, barometric pressure 607 mmHg) and Davos Jakobshorn (2590 m, barometric pressure 554 mmHg). We invited OSA patients of both sexes, age 20 to 80 y, on successful CPAP therapy for more than 3 mo and living at an altitude below 600 m, to participate in our study. The diagnosis of OSA was based on an elevated apnea-hypopnea index (AHI) and symptoms of excessive daytime sleepiness documented in the medical records, prior to the start of CPAP therapy. Study inclusion required more than 15 oxygen desaturations per hour (> 3% SpO2 dips) during a current ambulatory pulse oximetry performed at the end of a 4-night period without CPAP in Zurich. In addition, polysomnography at 490 m had to show an AHI > 10 events/h with predominant obstructive events.
Randomization and Interventions
Participants were randomized to one of four sequences of altitude exposure and to two sequences of drug treatment according to a nested, balanced block design, i.e., they spent 1 day/night each at the following altitudes:
sequence A: 490, 1860, 1860, 2590 m – 2 w low altitude washout – 1860, 1860, 2590 m;
sequence B: 490, 1860, 2590, 1860 m – 2 w low altitude washout – 1860, 2590, 1860 m;
sequence C: 1860, 1860, 2590 m – 2 w low altitude washout – 1860, 1860, 2590, 490 m;
sequence D: 1860, 2590, 1860 m – 2 w low altitude washout – 1860, 2590, 1860, 490 m.16
During the first altitude sojourn patients took acetazolamide and during the second sojourn placebo, or vice-versa, according to randomization. Polysomnography and 12-lead electrocardiography (ECG) monitoring were assessed in the night at 490 m, in the second night at 1860 m and in the night at 2590 m. Patients chose among available study time slots without being aware of the order of altitude exposure assigned to them. The order of treatment with acetazolamide (2 × 250 mg/d) and placebo during the two altitude sojourns was randomized by letting participants select a medication set from a box containing several identically looking sets of study drugs. Patients and investigators were blinded to the study treatment until completion of data analysis.
Assessments
Participants were monitored with a 12-lead surface Holter ECG device during time in bed (Getemed, CardioDay ECG analyses software V2.2.0).18,19 According to international standards,20 the device recorded all leads simultaneously during the entire night, identified the lead with the longest QT intervals and averaged the values every five heartbeats. The QT intervals automatically determined by the software in this way was validated visually.
The corrected QT interval was calculated by the Bazett formula (QTc = QT interval divided by the square root of the RR interval).21,22 Mean values of QTc computed for the entire night (meanQTc), and mean QTc computed for the minute of the night with highest (maxQTc) and lowest values (minQTc) and the difference between these (max-minQTc) as a measure of variability were determined. QT dispersion among the simultaneously recorded 12 leads was computed as the difference in QT interval in the lead with the longest QT interval minus the corresponding value in the lead with the shortest QT interval.20 This analysis was performed for periods in the early morning (05:00–06:00) when the longest QT intervals were expected. Supraventricular and ventricular arrhythmias and bradycardia events (heart rate < 50/min for > 4 beats) were scored. Polysomnographic sleep studies comprised standard neurophysiologic measurements,17,23 calibrated respiratory inductance plethysmography,24 diaphragmatic surface electromyography to differentiate obstructive from central apneas/hypopneas, transcutaneous PCO2 (PtcCO2)25, airflow and pulse oximetry. Morning examinations included measurements of blood pressure, pulse oximetry and body weight.
Outcomes
The main outcome of the current analysis was the QTc interval duration. Secondary outcomes included the number of nocturnal arrhythmia events, heart rate, arterial oxygen saturation by pulse oximetry and the AHI. A sample size estimation performed in relation to the primary outcomes of the main study (AHI and the mean nocturnal oxygen saturation) suggested that at least 44 patients should be randomized.16
Statistical Analysis
As most variables were not normally distributed, data are summarized as medians and quartiles. Analyses of drug effects were conducted on an intention-to-treat principle with missing values substituted by corresponding values on the alternative drug assuming no effect of acetazolamide. Effects of altitude and acetazolamide were evaluated by Friedman analysis of variance followed by post hoc analysis with Wilcoxon matched pairs tests as appropriate. Effects of interventions (altitude exposure, acetazolamide therapy) were further quantified by median differences with 95 % confidence intervals.17 Multivariable, random-effects, generalized least-square regression models were adapted to the mean QTc interval (which was normally distributed) to assess the effects of treatment when controlling for potential confounders including time of the night spent with oxygen saturation < 90% as a measure of sustained hypoxia at altitude, AHI, age, and sex. Two-sided tests applying a Bonferroni correction were applied and P < 0.05 was considered statistically significant.17
RESULTS
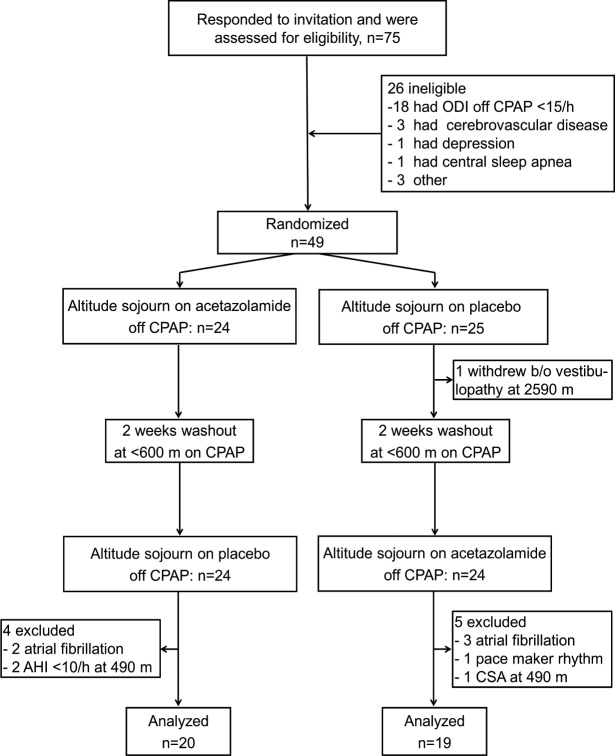
Of 75 screened patients, 49 met inclusion criteria and were randomized (Figure 1). One patient withdrew from the study after the first night at 2590 m because of an acute peripheral vestibulopathy. Data from three patients had to be excluded according to the predefined criteria, because polysomnography at 490 m revealed an obstructive AHI < 10 events/h in two patients and predominant central sleep apnea in one patient.16 Five had to be excluded because of atrial fibrillation and one because of a pacemaker rhythm that prevented reliable QTc measurement. Table 1 shows the characteristics of the 39 participants (36 men, 3 women) included into the analyses.
Figure 1.
Patient flow. AHI, apnea-hypopnea index; b/o, because of; CPAP, continuous positive airway pressure; CSA, predominant central sleep apnea; ODI, oxygen desaturation index.
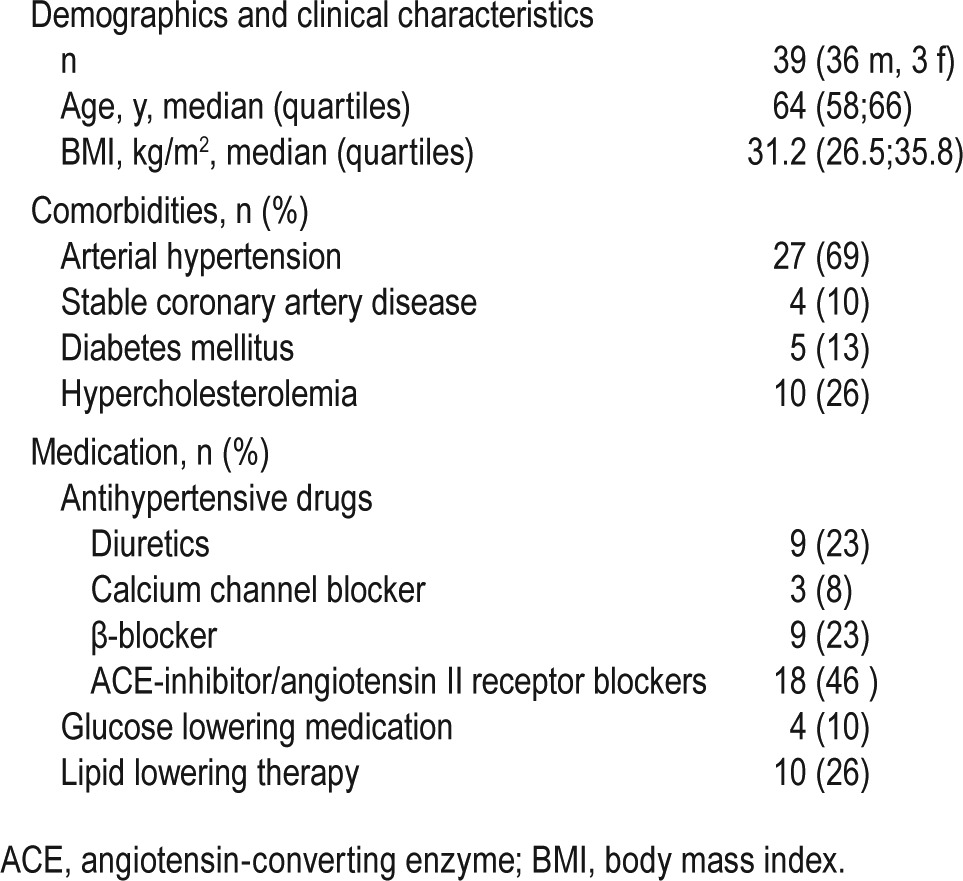
Table 1.
Characteristics of patients.
Results of ECG recordings and polysomnography are summarized in Tables 1, 2, and 3 and Figures 2 and 3. Baseline studies without CPAP at 490 m revealed median values of meanQTc of 420 ms, maxQTc of 478 ms, max-minQTc (QTc variability) of 82 ms and QT dispersion of 35 ms, which lies in the normal range for both men and women.26 At 1860 m and 2590 m on placebo the QTc intervals were significantly prolonged (meanQTc 436 ms and 430 ms; maxQTc 499 ms and 510 ms, respectively) compared to corresponding values at 490 m (Table 2, Figure 2). Moreover, the measures of QT variability (max-minQTc) and of QT dispersion were also significantly larger at 2590 m than at 490 m (Table 2). On acetazolamide at 1860 m and 2590 m, meanQTc were significantly shorter (422 ms and 427 ms) than on placebo at corresponding altitude, and similar to the values at 490m, while maxQTc remained prolonged (494 ms and 502 ms). Acetazolamide decreased the meanQTc by −6 ms (95% CI, −2 ms to −12 ms) at 1860 m and by −10 ms (95% confidence interval [CI], 0 to −12 ms) at 2590 m and it decreased QT dispersion by −12 ms (95% CI, −6 ms to −22 ms) at 1860 m and by −25 ms (95% CI, −21 to −37 ms) at 2590 m (Figure 3).
Table 2.
Results of electrocardiography monitoring and polysomnography (n = 39).
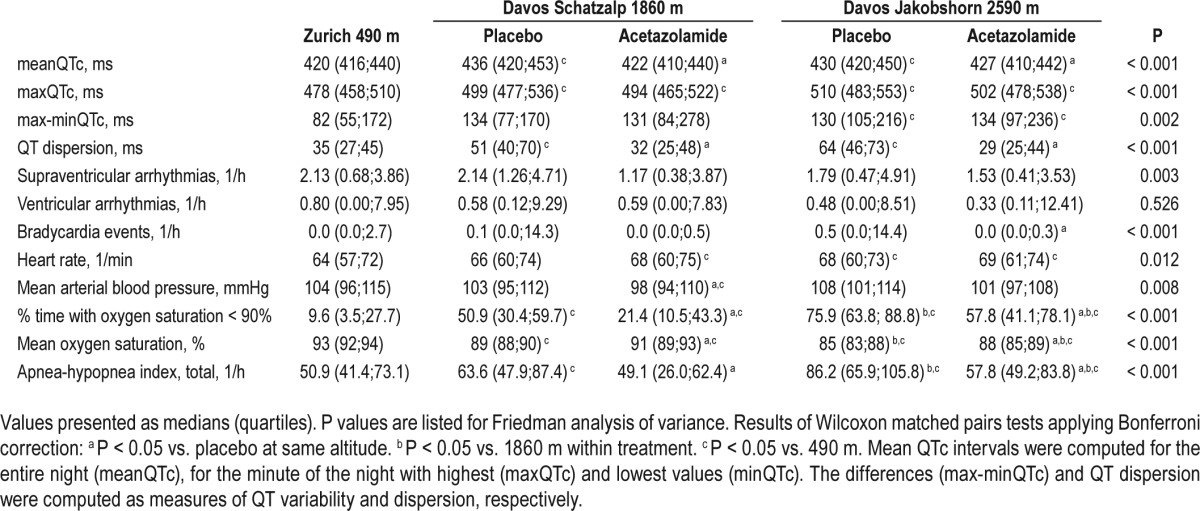
Table 3.
Regression analysis of the effect of altitude and acetazolamide on the mean QTc interval (dependent variable).
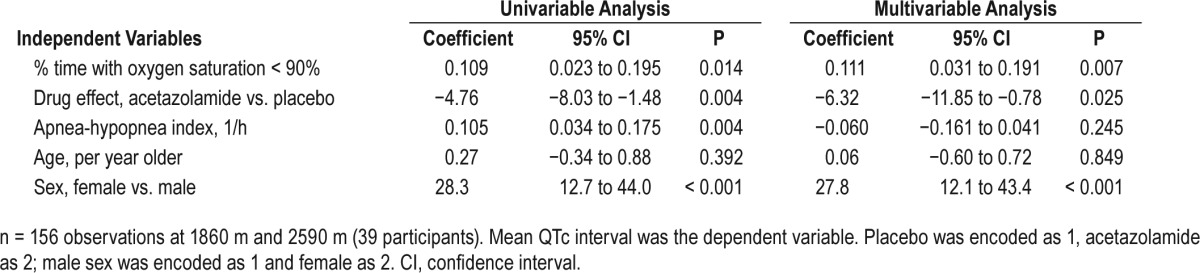
Figure 2.
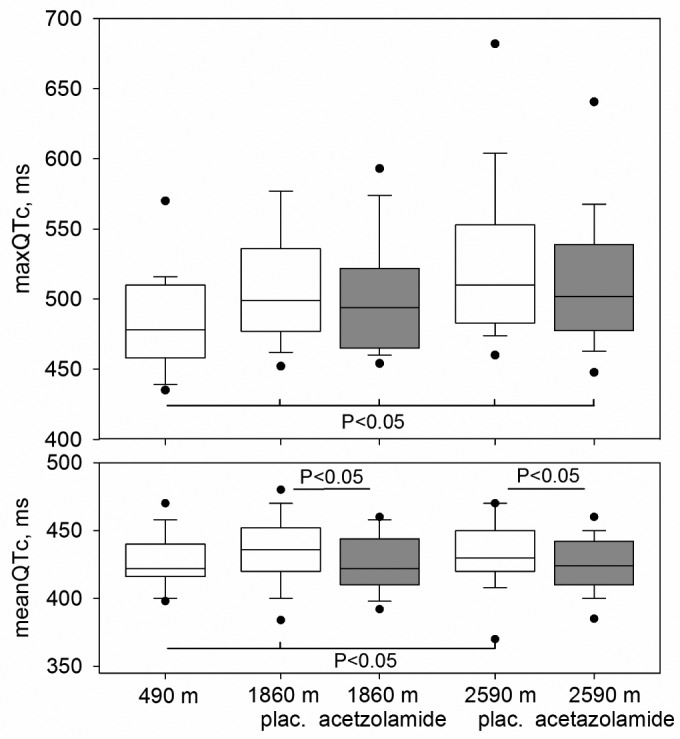
QTc intervals in patients with obstructive sleep apnea at three different altitudes during discontinuation of continuous positive airway pressure therapy. White boxes with whiskers and dots represent medians, quartiles, 5th, 10th, 90th and 95th percentiles during placebo treatment, gray boxes represent corresponding values during acetazolamide treatment. Mean QTc intervals during entire nights (meanQTc, lower panel) and mean QTc intervals during minutes with the highest values of the nights (maxQTc, upper panel) are shown. Significant differences (P < 0.05) between values at the higher altitudes versus values at 490 m, and between acetazolamide and placebo are indicated.
Figure 3.
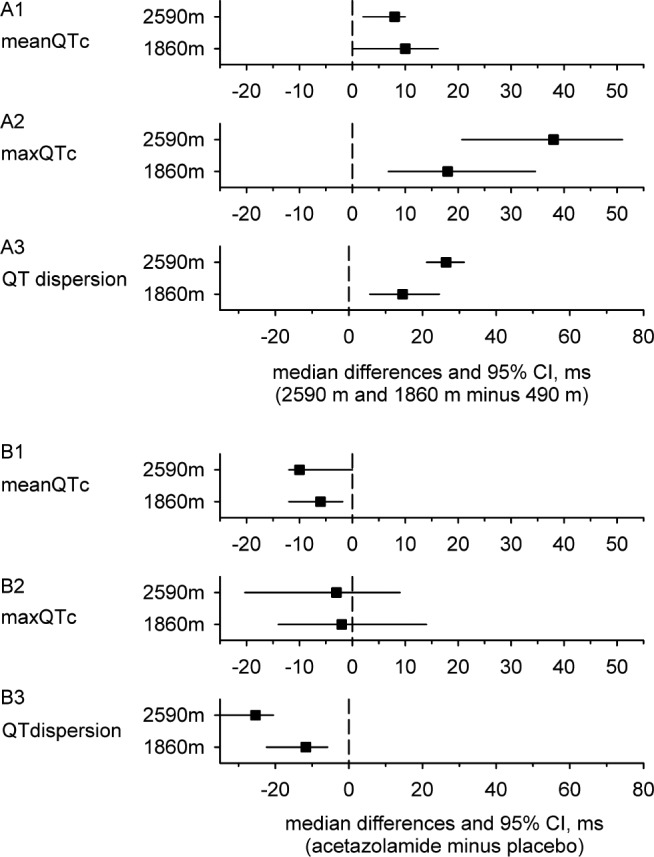
The effects of exposure to higher altitudes in patients using placebo (1860 and 2590 m, respectively) versus 490 m are illustrated by plotting median differences with 95% confidence interval (CI) of the corresponding mean QTc intervals during entire nights (meanQTc, panel A1), mean QTc intervals during minutes with the highest values of the nights (maxQTc, panel A2), and the QT dispersion (panel A3). The effects of acetazolamide vs. placebo at 1860 and 2590 m on meanQTc, maxQTc, and QT dispersion are illustrated in a similar way in panels B1-B3. MeanQTc, maxQTc and QT dispersion were prolonged at the higher altitudes and acetazolamide prevented the altitude induced increase in meanQTc and in QT dispersion.
Multivariable, random-effects, generalized least-square regression analysis was performed with the mean QTc interval as the dependent variable and percent time spent with oxygen saturation below 90%, acetazolamide/placebo therapy, AHI, age, and sex as independent variables (Table 3). This analysis confirmed independent effects of acetazolamide and of hypoxemia.
There were fewer bradycardia events on acetazolamide at 2590 m compared to placebo. The number of supraventricular and ventricular arrhythmias was not significantly influenced by altitude or treatment. Mean nocturnal heart rate was increased at 2590 m on placebo and acetazolamide.
DISCUSSION
We studied measures of cardiac repolarization and arrhythmias in patients with OSA who discontinued their CPAP therapy during altitude travel. The nocturnal recordings revealed that ascending from 490 m to 2590 m induced considerable prolongations of the mean and maximal QTc intervals (median increase in meanQTc +8 ms, in maxQTc +38 ms), and an increase of the QT dispersion (median increase +28 ms). In 24 of 38 patients (63%) staying 1 night at 2590 m (on placebo) the maxQTc reached very high values exceeding 500 ms. Because prolongation and increased dispersion of cardiac repolarization have been associated with malignant cardiac arrhythmia and sudden cardiac death9–12,20,27,28 our data suggest that untreated OSA patients are at increased risk of such adverse cardiac events when traveling to altitude without treatment. The current randomized, placebo-controlled trial further demonstrates that acetazolamide prevented the altitude-induced prolongation of meanQTc and of QT dispersion in OSA patients and may therefore provide some benefit if CPAP is not feasible.
Intermittent hypoxia is a physiological consequence of OSA that promotes cardiac arrhythmias by autonomic nervous system activation, increased oxidative stress and altered myocardial excitability.5 Recurrent arousals following the respiratory events lead to sympathetic activation and possibly coronary vasoconstriction. Furthermore, increased negative intrathoracic pressure swings during obstructive apnea/ hypopnea may stretch the myocardial wall and intrathoracic vessels. These mechanical effects could enforce changes in myocardial excitability and may also lead to structural remodeling of the myocardium.6 Disturbances of cardiac repolarization have been reported in OSA patients based on prolonged and variable QT intervals that suggested myocardial electrical instability.11,12,29,30 Gillis et al.31 observed a significant prolongation of QTc and decreasing heart rate during severe apneas as well as shortening of QTc and abrupt increases in the heart rate during the post apneic hyperventilation period. These sudden changes in cardiac repolarization and heart rate may be significant triggers in the development of ventricular arrhythmias and may contribute to the cardiovascular mortality of OSA in particular during the night.8,31
We have previously shown that untreated OSA patients traveling to altitude experience pronounced hypoxemia and an exacerbation of sleep apnea due to frequent central events.15 This was associated with an increase in the incidence of ventricular extra beats, suggesting that aggravation of intermittent and sustained hypoxia promoted cardiac electrical instability. Rossi et al.7 demonstrated in OSA patients on long-term CPAP therapy that withdrawal of the treatment for 2 w was associated with a prolongation of QTc measured during daytime. The amount of QTc prolongation was correlated with the severity of the recurring sleep apnea. The findings of the current trial corroborate and extend these findings by suggesting that the exposure to hypobaric hypoxia during a stay at altitude without CPAP therapy represents an even greater risk of malignant cardiac arrhythmia and sudden cardiac death for OSA patients compared to discontinuation of CPAP in normobaric conditions near sea level.9,10,27,28,32,33 Regression analysis revealed that the QTc prolongation observed at higher altitude was related to the greater degree of hypoxemia rather than to the increase in central apneas (Table 3). In the current study, the incidence of ventricular arrhythmias at 490 m was low and it was not significantly increased at the higher altitudes despite the prolongation of QTc. This may have been related to an insufficient sample size and to the fact that only 4 of the 39 patients in the current study had (stable) coronary heart disease that predisposes to arrhythmia34 during exposure to hypoxia.
Acetazolamide has been shown to prevent acute mountain sickness and reduce high altitude periodic breathing in healthy subjects.35,36 This carbonic anhydrase inhibitor stimulates ventilation and improves oxygenation by promoting renal elimination of bicarbonate thereby counteracting the altitude induced respiratory alkalosis. In patients with OSA at low altitude, acetazolamide has no clinically relevant effect on sleep-related breathing disturbances. However, in OSA patients traveling to altitude and on acetazolamide, we have shown that acetazolamide improves nocturnal arterial oxygen saturation, AHI,16,17 and cerebral tissue oxygenation37 when used as the sole therapy or in combination with CPAP therapy. The current trial indicates that the improvement in arterial oxygen saturation by acetazolamide may have additional beneficial effects in OSA patients during altitude travel by preventing the prolongation of QTc and the associated risks (Table 2).
In summary, our study in patients with OSA who discontinued CPAP therapy during a stay at 1860 m and 2590 m demonstrates that sustained and intermittent hypoxia at moderate altitude leads to disturbed cardiac repolarization with a prolongation of the QTc interval and greater dispersion, suggesting an increase in the risk of malignant arrhythmias. This may apply particularly to those suffering from coronary heart disease or using drugs that prolong QT duration such as certain antidepressants or macrolide antibiotics. Because acetazolamide improves arterial oxygen saturation and AHI and prevents prolongation of the meanQTc and QT dispersion, the drug might be beneficial for OSA patients who are unable to use CPAP therapy during altitude travel.
DISCLOSURE STATEMENT
This was not an industry supported study. Grant support was provided by the Swiss National Science Foundation (Grant 32003B-122081), and the Lung League of Zurich, Switzerland. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: Dr. Bloch is the guarantor and take responsibility for the content of the manuscript, including the data and analysis. Dr. Latshang contributed substantially to acquiring, analyzing and interpreting the data, writing and revising the manuscript critically for important intellectual content. Ms. Kaufmann, Dr. Nussbaumer-Ochsner, Dr. Ulrich, Mr. Furian, Dr. Kohler, Dr. Thurnheer, Dr. Saguner, and Dr. Duru contributed to data collection, analysis and revising the article critically for important intellectual content.
REFERENCES
- 1.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–8. doi: 10.1016/S2213-2600(15)00043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Amer Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009;108:246–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoeahypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 5.Kohler M, Stradling JR. Mechanisms of vascular damage in obstructive sleep apnea. Nature reviews. Cardiology. 2010;7:677–85. doi: 10.1038/nrcardio.2010.145. [DOI] [PubMed] [Google Scholar]
- 6.Rossi VA, Stradling JR, Kohler M. Effects of obstructive sleep apnoea on heart rhythm. Eur Respir J. 2013;41:1439–51. doi: 10.1183/09031936.00128412. [DOI] [PubMed] [Google Scholar]
- 7.Rossi VA, Stoewhas AC, Camen G, et al. The effects of continuous positive airway pressure therapy withdrawal on cardiac repolarization: data from a randomized controlled trial. Eur Heart J. 2012;33:2206–12. doi: 10.1093/eurheartj/ehs073. [DOI] [PubMed] [Google Scholar]
- 8.Gami AS, Howard DE, Olson EJ, Somers VK. Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med. 2005;352:1206–14. doi: 10.1056/NEJMoa041832. [DOI] [PubMed] [Google Scholar]
- 9.Straus SM, Kors JA, De Bruin ML, et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol. 2006;47:362–7. doi: 10.1016/j.jacc.2005.08.067. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Post WS, Blasco-Colmenares E, Dalal D, Tomaselli GF, Guallar E. Electrocardiographic QT interval and mortality: a meta-analysis. Epidemiology. 2011;22:660–70. doi: 10.1097/EDE.0b013e318225768b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shamsuzzaman AS, Somers VK, Knilans TK, Ackerman MJ, Wang Y, Amin RS. Obstructive sleep apnea in patients with congenital long QT syndrome: implications for increased risk of sudden cardiac death. Sleep. 2015;38:1113–9. doi: 10.5665/sleep.4824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shamsuzzaman A, Amin RS, van der Walt C, et al. Daytime cardiac repolarization in patients with obstructive sleep apnea. Sleep Breath. 2015;19:1135–40. doi: 10.1007/s11325-015-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol. 1983;52:490–4. doi: 10.1016/0002-9149(83)90013-9. [DOI] [PubMed] [Google Scholar]
- 14.Camen G, Clarenbach CF, Stowhas AC, et al. The effects of simulated obstructive apnea and hypopnea on arrhythmic potential in healthy subjects. Eur J Appl Physiol. 2013;113:489–96. doi: 10.1007/s00421-012-2457-y. [DOI] [PubMed] [Google Scholar]
- 15.Nussbaumer-Ochsner Y, Schuepfer N, Ulrich S, Bloch KE. Exacerbation of sleep apnoea by frequent central events in patients with the obstructive sleep apnoea syndrome at altitude: a randomised trial. Thorax. 2010;65:429–35. doi: 10.1136/thx.2009.125849. [DOI] [PubMed] [Google Scholar]
- 16.Nussbaumer-Ochsner Y, Latshang TD, Ulrich S, Kohler M, Thurnheer R, Bloch KE. Patients with obstructive sleep apnea syndrome benefit from acetazolamide during an altitude sojourn: a randomized, placebo-controlled, double-blind trial. Chest. 2012;141:131–8. doi: 10.1378/chest.11-0375. [DOI] [PubMed] [Google Scholar]
- 17.Latshang TD, Nussbaumer-Ochsner Y, Henn RM, et al. Effect of acetazolamide and autoCPAP therapy on breathing disturbances among patients with obstructive sleep apnea syndrome who travel to altitude: a randomized controlled trial. JAMA. 2012;308:2390–8. doi: 10.1001/jama.2012.94847. [DOI] [PubMed] [Google Scholar]
- 18.Burke GM, Wang N, Blease S, Levy D, Magnani JW. Assessment of reproducibility--automated and digital caliper ECG measurement in the Framingham Heart Study. J Electrocardiol. 2014;47:288–93. doi: 10.1016/j.jelectrocard.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mason JW, Moon TE. Automated measurements for individualized heart rate correction of the QT interval. Clin Trials. 2015;12:149–55. doi: 10.1177/1740774514566332. [DOI] [PubMed] [Google Scholar]
- 20.Rautaharju PM, Surawicz B, Gettes LS, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53:982–91. doi: 10.1016/j.jacc.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–70. [Google Scholar]
- 22.Saguner AM, Ganahl S, Baldinger SH, et al. Usefulness of electrocardiographic parameters for risk prediction in arrhythmogenic right ventricular dysplasia. Am J Cardiol. 2014;113:1728–34. doi: 10.1016/j.amjcard.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 23.Bloch KE. Polysomnography: a systematic review. Technol Health Care. 1997;5:285–305. [PubMed] [Google Scholar]
- 24.Bloch KE, Li Y, Sackner MA, Russi EW. Breathing pattern during sleep disruptive snoring. Eur Respir J. 1997;10:576–86. [PubMed] [Google Scholar]
- 25.Senn O, Clarenbach CF, Kaplan V, Maggiorini M, Bloch KE. Monitoring carbon dioxide tension and arterial oxygen saturation by a single earlobe sensor in patients with critical illness or sleep apnea. Chest. 2005;128:1291–6. doi: 10.1378/chest.128.3.1291. [DOI] [PubMed] [Google Scholar]
- 26.Uberoi A, Stein R, Perez MV, et al. Interpretation of the electrocardiogram of young athletes. Circulation. 2011;124:746–57. doi: 10.1161/CIRCULATIONAHA.110.013078. [DOI] [PubMed] [Google Scholar]
- 27.Barr CS, Naas A, Freeman M, Lang CC, Struthers AD. QT dispersion and sudden unexpected death in chronic heart failure. Lancet. 1994;343:327–9. doi: 10.1016/s0140-6736(94)91164-9. [DOI] [PubMed] [Google Scholar]
- 28.Haugaa KH, Edvardsen T, Amlie JP. Prediction of life-threatening arrhythmias--still an unresolved problem. Cardiology. 2011;118:129–37. doi: 10.1159/000327093. [DOI] [PubMed] [Google Scholar]
- 29.Kilicaslan F, Tokatli A, Ozdag F, et al. Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio are prolonged in patients with moderate and severe obstructive sleep apnea. Pacing Clin Electrophysiol. 2012;35:966–72. doi: 10.1111/j.1540-8159.2012.03439.x. [DOI] [PubMed] [Google Scholar]
- 30.Baumert M, Smith J, Catcheside P, et al. Variability of QT interval duration in obstructive sleep apnea: an indicator of disease severity. Sleep. 2008;31:959–66. [PMC free article] [PubMed] [Google Scholar]
- 31.Gillis AM, Stoohs R, Guilleminault C. Changes in the QT interval during obstructive sleep apnea. Sleep. 1991;14:346–50. doi: 10.1093/sleep/14.4.346. [DOI] [PubMed] [Google Scholar]
- 32.Passman R, Kadish A. Polymorphic ventricular tachycardia, long Q-T syndrome, and torsades de pointes. Med Clin North Am. 2001;85:321–41. doi: 10.1016/s0025-7125(05)70318-7. [DOI] [PubMed] [Google Scholar]
- 33.el-Sherif N, Turitto G. The long QT syndrome and torsade de pointes. Pacing Clin Electrophysiol. 1999;22:91–110. doi: 10.1111/j.1540-8159.1999.tb00305.x. [DOI] [PubMed] [Google Scholar]
- 34.Holmes J, Kubo SH, Cody RJ, Kligfield P. Arrhythmias in ischemic and nonischemic dilated cardiomyopathy: prediction of mortality by ambulatory electrocardiography. Am J Cardiol. 1985;55:146–51. doi: 10.1016/0002-9149(85)90317-0. [DOI] [PubMed] [Google Scholar]
- 35.Basnyat B, Gertsch JH, Johnson EW, Castro-Marin F, Inoue Y, Yeh C. Efficacy of low-dose acetazolamide (125 mg BID) for the prophylaxis of acute mountain sickness: a prospective, double-blind, randomized, placebo-controlled trial. High Alt Med Biol. 2003;4:45–52. doi: 10.1089/152702903321488979. [DOI] [PubMed] [Google Scholar]
- 36.Fischer R, Lang SM, Leitl M, Thiere M, Steiner U, Huber RM. Theophylline and acetazolamide reduce sleep-disordered breathing at high altitude. Eur Respir J. 2004;23:47–52. doi: 10.1183/09031936.03.00113102. [DOI] [PubMed] [Google Scholar]
- 37.Ulrich S, Nussbaumer-Ochsner Y, Vasic I, et al. Cerebral oxygenation in patients with obstructive sleep apnea. Effects of hypoxia at altitude and of acetazolamide. Chest. 2014;146:299–308. doi: 10.1378/chest.13-2967. [DOI] [PubMed] [Google Scholar]