Abstract
Study Objectives:
To investigate the cross-sectional relationship between objectively measured sleep characteristics and multiple indices of adiposity in racially/ethnically diverse older adults within the MESA Sleep study (n = 2,146).
Methods:
7-day actigraphy was used to assess sleep duration, sleep efficiency, and night-to-night variability. Body mass index (BMI), waist circumference, and total body fat were modeled continuously and according to obesity cut-points. Models were adjusted for demographic, socioeconomic, and behavioral variables.
Results:
Participants who slept less than 6 hours a night had significantly higher BMI, waist circumference, and body fat relative to those who slept 7–8 hours. Those who slept less than 5 hours had a 16% higher prevalence of general obesity (BMI ≥ 30 vs. < 25 kg/m2) (95% [CI]: 0.08–0.24) and a 9% higher prevalence of abdominal obesity (waist circumference: women ≥ 88 centimeters, men ≥ 102 centimeters; 95% CI: 0.03–0.16) compared to those who slept 7–8 hours. Results were similar for sleep efficiency and night-to-night sleep variability.
Conclusions:
Among an older multi-ethnic cohort, we found robust associations across multiple indices of sleep and adiposity. Targeting sleep characteristics may be of benefit in obesity interventions, but more research is needed to rule out reverse causality.
Citation:
Ogilvie RP, Redline S, Bertoni AG, Chen X, Ouyang P, Szklo M, Lutsey PL. Actigraphy measured sleep indices and adiposity: the Multi-Ethnic Study of Atherosclerosis (MESA). SLEEP 2016;39(9):1701–1708.
Keywords: sleep duration, obesity, body mass index, waist circumference, sleep efficiency
Significance.
Although numerous studies on sleep and obesity have been conducted, results have been inconsistent. Most previous research has been limited by relying on self-reported sleep measures, including only one measure of obesity, and/or racially/ethnically homogenous populations. In this study, we found significant associations between multiple actigraphy-derived sleep indices and measures of adiposity in a multi-ethnic cohort of older adults. Future research using objective sleep measures should focus on longitudinal and randomized designs to determine if the relationship is causal. Sleep characteristics should also be considered in the development of obesity interventions.
INTRODUCTION
According to the most recent data, 69.2% of Americans self-reported that they did not get enough sleep at least one day in the previous month,1 and 68.5% of American adults were over-weight or obese (2011–2012).2 Because the prevalence of these conditions is high, Healthy People 2020 objectives include increasing the proportion of adults who get sufficient sleep and are at a healthy weight.3 These co-occurring high prevalences, together with pathophysiologic evidence,4 have suggested that sleep and obesity are interrelated. Although there is a strong inverse association between sleep and obesity in children,5 the relationship is less consistent in adults, and studies have reported inverse associations, U-shaped associations, or no association.6–10 Most studies, however, have used self-reported measures of sleep duration, only one measure of obesity, and racially/ethnically homogenous populations.
Literature on other measures of sleep, such as sleep efficiency and night-to-night sleep variability, is more limited because it cannot be assessed well with self-report measures. Previous studies have found that lower sleep efficiency and higher sleep variability are associated with higher levels of obesity.11–13
The Multi-Ethnic Study of Atherosclerosis (MESA) provides an opportunity to evaluate the relationship between actigraphy-measured sleep indices and multiple measures of adiposity in a racially diverse population. We hypothesized that short sleep duration, low sleep efficiency and high sleep duration variability will be associated with higher levels of adiposity independently of other confounders. We also evaluated whether the association differed by age, sex, or race/ethnicity.
METHODS
MESA is a cohort study designed to study risk factors for clinical and subclinical cardiovascular diseases in four racial/ ethnic groups.14 The study began in July 2000 and recruited 6,814 adults free of clinical CVD and aged 45–84 years from 6 field centers across the United States: Baltimore, MD; Chicago, IL; Los Angeles, CA; New York, NY; Saint Paul, MN; and Winston-Salem, NC. Five exams have now taken place, with the most recent occurring from April 2010 to February 2013. All of the 4,077 participants who attended Exam 5 were approached for participation in MESA Sleep, an ancillary study of objective measures of sleep and their relationship to cardiovascular disease. The median time interval between Exam 5 and MESA Sleep was 301 days (range 0–1,024 days). Sleep data was received from 2,261 participants, and the current cross-sectional analysis included 2,146 participants with data on both sleep and adiposity measures. Local institutional review boards approved study protocols, and all participants gave written informed consent.
Exposures
Sleep measures were assessed using at home 7-day actigraphy. All participants wore the Actiwatch Spectrum wrist actigraph (Philips Respironics, Murrysville, PA) on the non-dominant wrist. Output was scored by a certified technician using an event marker, a self-reported sleep diary, and data on light levels at the Sleep Reading Center at Brigham and Women's Hospital in Boston, Massachusetts.15 Sleep interval start and end time were determined by activity count increases and decreases, respectively. These times were compared to the event marker, sleep journal bed and wake times, and light level changes. The Cole-Kripke algorithm was used to generate data on sleep duration and sleep efficiency.16 Sleep duration was defined as the average sleep time in main sleep periods across all days, defined as the sum of the sleep time over each night divided by the total number of days. This variable was modeled in 5 categories: < 5 h, 5–6, 6–7, 7–8, and > 8 hours. Sleep efficiency was defined as the percentage of time spent asleep in the sleep interval (“lights off” to “lights on”). For modeling purposes, we first categorized sleep efficiency according to quartiles of the distribution, then we further divided the lowest category according to the commonly used threshold of less than 85. The 5 categories were then < 85%, 85–87.9%, 87.9–90.4%, 90.4–92.4%, and > 92.4%. Night-to-night variability in sleep duration was measured in minutes using the within person between-night standard deviation (SD) of the sleep duration variable, and was modeled in approximate quartiles (≤ 48, 48–70, 70–99, and 99–262).
Outcomes
All measures of adiposity were obtained during the MESA Exam 5 clinic visits. Participants wore light clothing and no shoes. Height was measured to the nearest 0.5 cm using an Accu-Hite measure device and weight was measured to the near 0.5 kg using a Detecto Platform Balance Scale. BMI was calculated in kg/m2. Waist circumference was measured at the umbilicus to the nearest 0.1 cm using a Gulick II 150 cm anthropometric tape. Total body fat was measured in kilograms via full body bioelectrical impedance analysis (BIA) using the Valhalla BCS-2 Body Composition scale and printer. In validation studies, bioelectrical impedance was highly correlated with dual-energy X-ray absorptiometry and was a much better estimator of body fat than BMI.17
Covariates
Additional information on sociodemographics and behaviors was assessed via questionnaire at Exam 5. Alcohol use was characterized as present drinking of alcoholic beverages or not. Smoking status was categorized as current, former, or never smoker. Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale (CES-D) and was modeled dichotomously with a cutpoint at 16; scores at this point or higher are typically indicative of clinically significant symptomatology.18 Antidepressant use was categorized as yes based on use of tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and other depressants. Sleeping pill use was categorized as no use in the past 4 weeks, less than once a week, 1 or 2 times a week, 3 or 4 times a week, or ≥ 5 times a week. Sleep apnea was measured using in-home overnight polysomnography, as has been previously described.15 It included all central and obstructive apneas and hypopneas ≥ 4% desaturation and was modeled in 4 categories according to apnea-hypopnea index: 0 to < 5, 5 to < 15, 15 to < 30, and 30+ per night.
Analysis
Descriptive statistics were calculated for the exposure variables, stratified by sleep duration category. We used linear regression and logistic regression to model the relationship between the sleep indices and each anthropometric measure. Outcome measures were modeled both as continuous variables (linear regression) and according to dichotomous categories (logistic regression). Using the margins command in Stata, adjusted probabilities standardized to the total population were calculated for each category of the sleep exposure in the logistic models, and these probabilities were used to calculate prevalence differences for each obesity outcome.19 In the models with dichotomized outcomes, cutoffs for each measure were chosen according to standard guidelines. Participants with a BMI ≥ 30 kg/m2 were categorized as having overall obesity, those with a BMI between 25 and 29.9 kg/m2 were categorized as overweight, and those with a BMI l < 25 kg/m2 were categorized in the normal weight reference group. Abdominal obesity was defined as ≥ 88 cm for women and ≥ 102 cm for men.
We explored a series of models. The first model controlled for age, field center, race/ethnicity, and sex. Model 2 added socioeconomic and behavioral variables, including marital status, income, education, smoking, depressive symptoms, sleeping pill use, and alcohol use. Model 3 included covariates in Model 2 plus sleep apnea. For models with sleep efficiency and night-to-night variability as an exposure, we also adjusted for sleep duration (Model 4). Interactions between sleep and age, sex, and race/ethnicity on indices of adiposity were tested using cross-product terms in the linear models and stratified results were reported, as appropriate. Sensitivity analyses excluded individuals with long sleep (duration > 9 h) or sleep apnea (AHI ≥ 15).
RESULTS
The mean age in the analytic sample was 68.6 (SD 9.2) years, and 53.7% were female. Mean hours of sleep were 6.5 (SD 1.4). The mean BMI in the sample was 28.8 (SD 5.6), and mean waist circumference was 99.7 cm (SD 14.5); these indicators were approximately normally distributed. Indices of adiposity varied by race/ethnicity; general obesity (BMI ≥ 30 kg/m2) was present in 30.1% of whites, 49.2% of African Americans, 4.9% of Chinese, and 44.3% of Hispanics. For abdominal obesity (waist circumference: women ≥ 88 cm, men ≥ 102 cm) these proportions were 56.7%, 69.9%, 27.1%, and 65.0%, respectively.
Table 1 shows sociodemographic and behavioral characteristics by sleep duration category. Those averaging < 5 h of sleep per night were more likely to be male, African American, and current smokers. There was also important variation by race/ethnicity, with a range of 7.9% (whites) to 20.8% (African Americans).
Table 1.
Participant characteristics by sleep duration category: the Multi-Ethnic Study of Atherosclerosis 2010–2013.
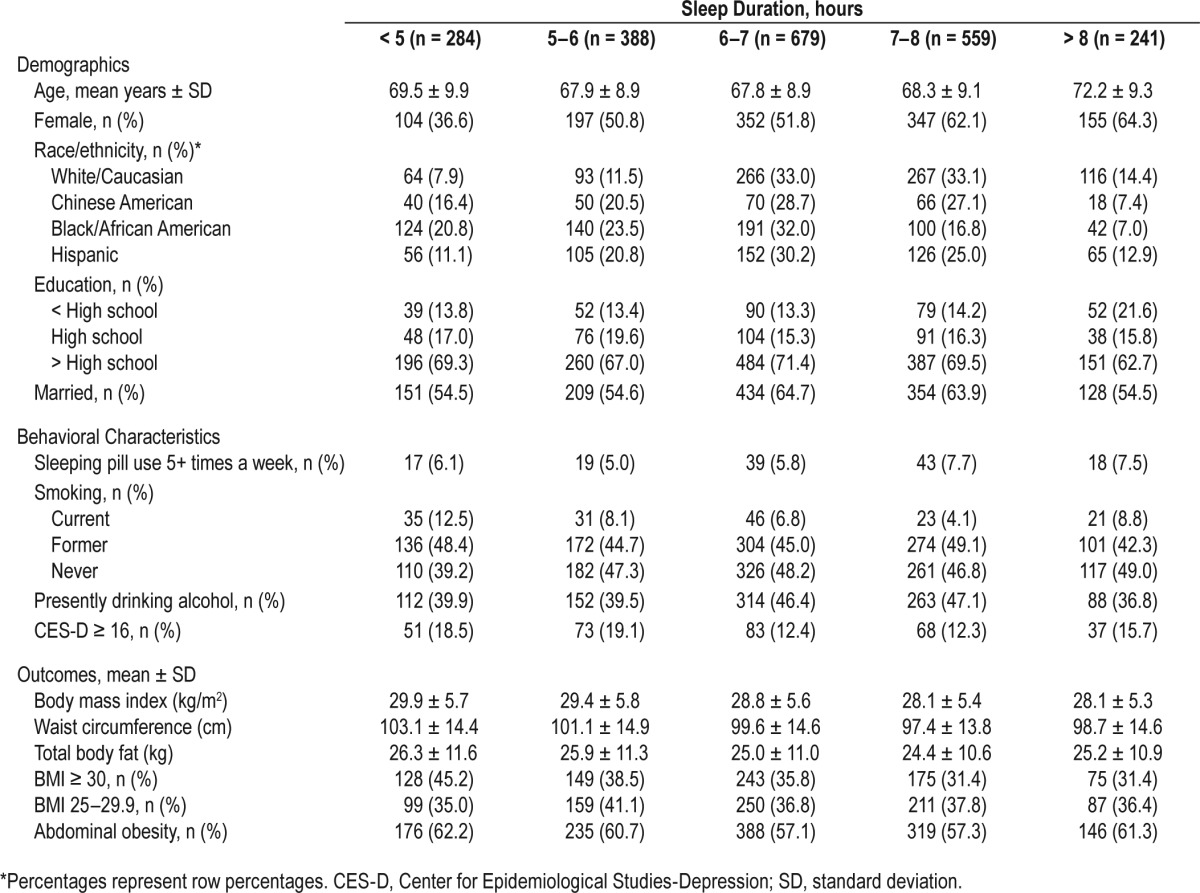
Table 2 shows adjusted means of adiposity measures by categories of the sleep indices from the linear models. Overall, we found significant associations between each sleep exposure and BMI, waist circumference, and total body fat. For example, after accounting for demographics, BMI was 1–2 units larger among those with short sleep duration (< 5 h), low sleep efficiency, or high sleep variability relative to those who slept 7–8 h/night, had high sleep efficiency, or low sleep variability, respectively. Similar results were found for waist circumference and total body fat, where those with short sleep duration, low sleep efficiency, or high sleep variability had a waist circumference 2.5 to 5 cm larger and body fat 2 to 3 kg more than those who slept 7–8 h/night, had high sleep efficiency, or low sleep variability. Further adjustment for socioeconomic and behavioral variables did not significantly alter the estimates, though the effect of sleep efficiency and variability was reduced with adjustment for sleep duration. Models where each exposure was treated continuously per one standard deviation can be found in Table S1 in the supplemental material. Results were similar to the exposures modeled categorically. Results were also similar in sensitivity analyses when we removed from the analysis the 41 individuals who slept > 9 h/night (data not shown). Associations were attenuated, but some retained statistical significance, when sleep apnea was added into the model and when analyses were restricted to those with AHI < 15 (Table 2 and Table S2 in the supplemental material).
Table 2.
Adjusted means of adiposity measures by categories of sleep duration, efficiency and variability: the Multi-Ethnic Study of Atherosclerosis 2010–2013.

Effect modification by age, sex, and race/ethnicity was also tested in each linear model. Significant interaction terms were found between sleep efficiency and sex for each outcome; sexstratified results are presented in Table S3 in the supplemental material. Across sleep efficiency categories, men had similar BMIs, while for women lower sleep efficiency was associated with higher BMI. Similar results were found for waist circumference, where men had similar waists across sleep efficiency categories, but for women lower sleep efficiency was associated with higher waist circumference. Significant interaction terms were also found between age (dichotomized at the median) and sleep efficiency when waist circumference was the outcome (P = 0.03). Across sleep efficiency categories, those over age 68 had similar waists, while for those younger than 68, lower sleep efficiency was associated with higher waist circumference (Table S4 in the supplemental material). Although interactions terms approached significance for sex and sleep duration when the outcomes were BMI and waist circumference, no major differences between men and women were detected (Table S5 in the supplemental material). No significant interactions were found between sleep variability and the adiposity outcomes. Additionally, no significant interactions were found by race/ethnicity for any of the exposures or outcomes.
Figure 1 shows the prevalence differences for models with dichotomous outcomes. After accounting for demographics, those who slept < 5 h/night had a 16% higher prevalence of obesity (BMI ≥ 30 vs. < 25 kg/m2; P < 0.001) and a 7% higher prevalence of overweight (P = 0.133) compared to those who slept 7–8 h/night (Figure 1A; Table S6 in the supplemental material). They also had a 10% higher prevalence of abdominal obesity (defined as waist circumference ≥ 102 cm in men, ≥ 88 cm in women) (P = 0.002). Participants with lower sleep efficiency tended to be more obese by all definitions, though associations did not always achieve statistical significance (Figure 1B). Those in the highest quartile of sleep variability had a 5% higher prevalence of general obesity (P = 0.167) and a 6% higher prevalence of abdominal obesity (P = 0.037) compared to those in the lowest quartile (Figure 1C). For all exposures, further adjustment for socioeconomic and behavioral variables slightly reduced the estimates, while adjustment for sleep apnea resulted in substantial attenuation (Tables S6, S7 in the supplemental material).
Figure 1.
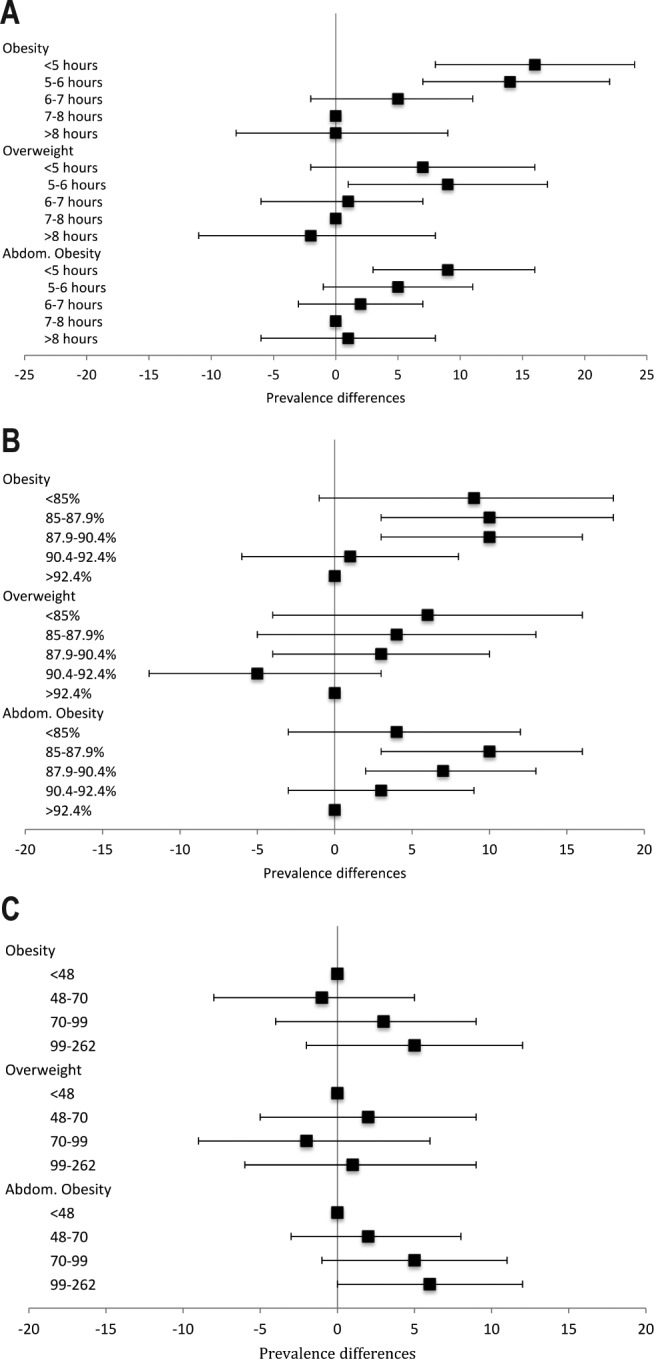
Prevalence differences* for obesity, overweight, and abdominal obesity by sleep duration, sleep efficiency, and sleep variability. (A) Sleep duration. (B) Sleep efficiency. (C) Sleep variability (in minutes). *Interpretation: Sleeping less than five hours per night was associated with an additional 16 cases of obesity per 100 individuals studied. Models adjusted for age, sex, race, field center, depressive symptoms, anti-depressants, alcohol use, sleep medication, smoking, income, marital status, and education. Obesity was defined as ≥ 30 kg/m2, overweight was defined as 25–29.9 kg/m2, abdominal obesity was ≥ 88 cm for women and ≥ 102 cm for men.
DISCUSSION
In this older, multi-racial/ethnic population of 2,146 adults from the MESA study, we found robust evidence that actigraphy measured sleep characteristics are cross-sectionally associated with several markers of adiposity. Those sleeping less than 5 hours per night had higher BMIs, larger waists, and more kilograms of body fat than those who slept 7–8 hours a night. Those with low sleep efficiency and high sleep variability also had higher BMIs, larger waists, and more body fat. Effects were smaller for sleep efficiency and variability once sleep duration was considered. There was also some evidence that effects were stronger in women compared to men, and for younger compared to older participants.
Previous research examining the cross-sectional relationship between sleep and obesity in adults has mainly focused on sleep duration, and has found a variety of different associations, including inverse, U-shaped, and no association.6–8 The majority of these studies use self-report questionnaires to assess sleep duration.20 Notably, self-reported and objectively measured sleep are only moderately correlated, and discrepancies between the two are related to a variety of pertinent confounders.21,22 Studies that did use objective measures of sleep duration also had mixed results with some finding inverse and U-shaped associations.12,23,24 Importantly, the only two longitudinal studies on this topic that used objective sleep measures found no association,23,25 which may suggest that this relationship is not causal in adults. Prospective studies using self-reported sleep data have found inverse, U-shaped, and no associations.8,20,26,27 However, there is strong and consistent evidence for a causal association between sleep duration and obesity among children and adolescents,6,28 including findings from a randomized crossover trial.29 More longitudinal and experimental studies with standardized measures are needed to determine whether the association between short sleep duration and adiposity is causal in adults.
Because few published studies used actigraphy, most did not evaluate the relationship between sleep efficiency, sleep variability, and obesity. Previous research has found that low sleep efficiency and high sleep variability is associated with both general and abdominal obesity.11–13 Better characterizing the associations between specific sleep disturbances, such as those that relate to short sleep duration vs. inconsistent sleep patterns, may be useful when designing future interventions.
In this study, the relationship between actigraphy-measured sleep characteristics and obesity was substantially attenuated with both adjustment for sleep apnea and restriction to those without sleep apnea. Few studies on sleep duration and obesity have examined sleep apnea because most relied on self-reported measures of sleep duration. Those that have examined it found that the relationship between sleep duration and obesity remained even after adjustment for OSA.25 The causal pathways between sleep duration, sleep apnea, and obesity are complicated. Obesity has been strongly and consistently associated with sleep apnea, with randomized trials of weight loss demonstrating that weight loss is causally associated with a reduction in AHI.30 It has also been suggested that weight loss may increase sleep duration through attenuating sleep apnea. However, the current evidence to support this hypothesis is limited and inconsistent, finding null or small associations.31–33 Patients with sleep apnea treated with CPAP may actually gain weight.34 Because the direction and strength of these relationships is complex, models with adjustment for sleep apnea require careful interpretation. More research is needed to disentangle the components of the relationship between sleep characteristics, sleep apnea, and obesity.
There are several potential pathways through which sleep indices can influence obesity.4 One possible mechanism is that short sleep duration may lead to increased food intake. Experimental studies have demonstrated that short sleep can lead to both self-reported and biological changes in hunger and appetite, including increases in ghrelin and decreases in leptin.6,35 Recent brain imaging data also suggest that insufficient sleep may increase central neuronal responses to high caloric foods, increasing behaviors leading to overeating.36 With more hours available in the day, short sleepers may also have more opportunities to eat. In another potential pathway, lack of sleep may lead to fatigue, which can lead to decreased physical activity. Pathways for efficiency and variability are less clear, but likely act through similar mechanisms. People with low sleep efficiency also may have selective deprivation of deep sleep (stage N3), which has been linked to central obesity,37 likely through effects on the hypothalamic pituitary adrenal axis and the autonomic nervous system.38 People with high sleep variability may represent those who engage in short sleep certain nights of the week and then compensate on other nights. Additionally, those with high sleep variability may have irregular eating patterns due to variation in their sleep-wake pattern.11 Thus, sleep variability may increase risk of adiposity through exposure to both periodic insufficient sleep, as well as by contributing to irregularity in the synchronization of eating and sleep timing, which is increasingly recognized to be important in energy balance.11
Existing studies of sleep and obesity have often relied on BMI as the sole measurement of the adiposity. Although BMI is easy to measure, it does not differentiate between lean and fat mass. Other measures, such as waist circumference better quantify the distribution of body fat. Studies that have examined sleep duration and other measures of adiposity have found inverse associations though there were some differences by sex.12,39,40 In this study, we measured adiposity with BMI, waist circumference, and total body fat measured through full body bioelectrical impedance and found that all behaved similarly within each sleep measure.
Prior research on sleep and obesity has also been conducted in mostly Caucasian populations. In our sample, as has been shown by others,41,42 minority groups slept for a shorter duration compared to white populations. Likewise, in our population, as is well established,43 obesity varied by race/ethnicity. However, in our sample the relationship between sleep duration and efficiency with obesity was not modified by race. This is consistent with a National Health and Nutrition Examination Survey analysis of whites, African Americans and Mexican Americans, which found an inverse linear association between self-reported sleep duration and obesity that did not vary by race/ethnicity.40 Notably, the Insulin Resistance Atherosclerosis Study (IRAS) previously reported that among 332 Hispanic and 775 African American participants, a U-shaped association was observed between self-reported sleep duration and change in adiposity, though only among participants less than 40 years old.26 Additional studies conducted in racially/ ethnically diverse populations are needed to make more definitive conclusions.
However, we did find effect measure modification by sex and age. Our finding that the relationship between sleep efficiency and obesity was stronger in women than men has been reported by others.11,12 In the current study, we also found effect modification by age for the relationship between sleep efficiency and waist circumference, whereby the association was stronger among younger individuals. More studies are needed to confirm this finding.
This study has several strengths. The use of actigraphy instead of self-reported sleep duration resulted in less measurement error of the exposure, and allowed for the ascertainment of both sleep efficiency and sleep variability. However, actigraphy has high sensitivity and low specificity because it detects wakefulness less accurately. Another strength of this study is its use of multiple measures of adiposity, instead of relying solely on BMI. The study also uses a population-based sample of four different racial/ethnic groups instead of a homogenous population.
This study also has several weaknesses. Foremost, no single observational study, particularly a cross-sectional one, allows establishing causality. Since measures of sleep and obesity were taken at the same time, temporality cannot be determined so the possibility of reverse causation exists. Additionally, selection bias may be present, if participation in the study was related to both sleep duration and obesity status. Because the pathway between sleep duration and obesity is not fully understood, it is possible that we neglected to control for all confounders. Additionally, residual confounding may have remained despite our attempts at adjustment.
Overall, this cross-sectional study found associations between multiple measures of objectively measured sleep and adiposity. The National Sleep Foundation presently recommends that adults aged 26–64 years get 7 to 9 hours of sleep per night, and that adults aged 65 or older get 7 to 8 hours of sleep per night.44 If short sleep is causally associated with the development of obesity in adults, as it is believed to be in children,29,45 increasing sleep duration among individuals with short sleep could represent an important public health intervention because a large proportion of the US population reports short sleep,46 and this is especially true among African Americans and Hispanics.41,42 Our study also identifies the potential importance of sleep efficiency and sleep efficiency as contributors to obesity. Future interventions that target one of more of these sleep traits in obesity prevention programs may yield novel insights into approaches for achieving the Healthy People 2020 health objectives.
DISCLOSURE STATEMENT
This was not an industry supported study. Research reported in this publication was supported by grants and contracts T32-HL-007779, R01HL098433, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-TR-001079 from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Redline has received research support from Jazz. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
REFERENCES
- 1.Centers for Disease Prevention. Perceived insufficient rest or sleep among adults - United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1175–9. [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. [Accessed March 27, 2015]. Available from: http://www.healthypeople.gov/2020/topics-objectives/2020-Topics-and-Objectives-Objectives-A-Z.
- 4.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11:163–78. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008;16:265–74. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 6.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16:231–41. doi: 10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 10.Sperry SD, Scully ID, Gramzow RH, Jorgensen RS. Sleep duration and waist circumference in adults: a meta-analysis. Sleep. 2015;38:1269–76. doi: 10.5665/sleep.4906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SR, Hayes AL, Blackwell T, et al. The association between sleep patterns and obesity in older adults. Int J Obes. 2014;38:1159–64. doi: 10.1038/ijo.2014.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mezick EJ, Wing RR, McCaffery JM. Associations of self-reported and actigraphy-assessed sleep characteristics with body mass index and waist circumference in adults: moderation by gender. Sleep Med. 2014;15:64–70. doi: 10.1016/j.sleep.2013.08.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kobayashi D, Takahashi O, Shimbo T, Okubo T, Arioka H, Fukui T. High sleep duration variability is an independent risk factor for weight gain. Sleep Breath. 2013;17:167–72. doi: 10.1007/s11325-012-0665-7. [DOI] [PubMed] [Google Scholar]
- 14.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 15.Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA) Sleep. 2015;38:877–88. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15:461–9. doi: 10.1093/sleep/15.5.461. [DOI] [PubMed] [Google Scholar]
- 17.Roubenoff R. Applications of bioelectrical impedance analysis for body composition to epidemiologic studies. Am J Clin Nutr. 1996;64:459S–62S. doi: 10.1093/ajcn/64.3.459S. [DOI] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D Scale. A self-report depression for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 19.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43:962–70. doi: 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gutierrez-Repiso C, Soriguer F, Rubio-Martin E, et al. Nighttime sleep duration and the incidence of obesity and type 2 diabetes. Findings from the prospective Pizarra study. Sleep Med. 2014;15:1398–404. doi: 10.1016/j.sleep.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Den Berg JF, Van Rooij FJ, Vos H, et al. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008;17:295–302. doi: 10.1111/j.1365-2869.2008.00638.x. [DOI] [PubMed] [Google Scholar]
- 23.Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. Am J Epidemiol. 2009;170:805–13. doi: 10.1093/aje/kwp230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Appelhans BM, Janssen I, Cursio JF, et al. Sleep duration and weight change in midlife women: the SWAN sleep study. Obesity. 2013;21:77–84. doi: 10.1002/oby.20251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010;33:289–95. doi: 10.1093/sleep/33.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiao Q, Arem H, Moore SC, Hollenbeck AR, Matthews CE. A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. Am J Epidemiol. 2013;178:1600–10. doi: 10.1093/aje/kwt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–33. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hart CN, Carskadon MA, Considine RV, et al. Changes in children's sleep duration on food intake, weight, and leptin. Pediatrics. 2013;132:e1473–80. doi: 10.1542/peds.2013-1274. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell LJ, Davidson ZE, Bonham M, O'Driscoll DM, Hamilton GS, Truby H. Weight loss from lifestyle interventions and severity of sleep apnoea: a systematic review and meta-analysis. Sleep Med. 2014;15:1173–83. doi: 10.1016/j.sleep.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 31.Alfaris N, Wadden TA, Sarwer DB, et al. Effects of a 2-year behavioral weight loss intervention on sleep and mood in obese individuals treated in primary care practice. Obesity. 2015;23:558–64. doi: 10.1002/oby.20996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shechter A, St-Onge MP, Kuna ST, et al. Sleep architecture following a weight loss intervention in overweight and obese patients with obstructive sleep apnea and type 2 diabetes: relationship to apneahypopnea index. J Clin Sleep Med. 2014;10:1205–11. doi: 10.5664/jcsm.4202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verhoef SP, Camps SG, Gonnissen HK, Westerterp KR, Westerterp-Plantenga MS. Concomitant changes in sleep duration and body weight and body composition during weight loss and 3-mo weight maintenance. Am J Clin Nutr. 2013;98:25–31. doi: 10.3945/ajcn.112.054650. [DOI] [PubMed] [Google Scholar]
- 34.Quan SF, Budhiraja R, Clarke DP, et al. Impact of treatment with continuous positive airway pressure (CPAP) on weight in obstructive sleep apnea. J Clin Sleep Med. 2013;9:989–93. doi: 10.5664/jcsm.3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Briancon-Marjollet A, Weiszenstein M, Henri M, Thomas A, Godin-Ribuot D, Polak J. The impact of sleep disorders on glucose metabolism: endocrine and molecular mechanisms. Diabetol Metab Syndr. 2015;7:25. doi: 10.1186/s13098-015-0018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.St-Onge MP, Wolfe S, Sy M, Shechter A, Hirsch J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. Int J Obes. 2014;38:411–6. doi: 10.1038/ijo.2013.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. Int J Obes. 2008;32:1825–34. doi: 10.1038/ijo.2008.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105:1044–9. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Theorell-Haglow J, Berne C, Janson C, Sahlin C, Lindberg E. Associations between short sleep duration and central obesity in women. Sleep. 2010;33:593–8. [PMC free article] [PubMed] [Google Scholar]
- 40.Ford ES, Li C, Wheaton AG, Chapman DP, Perry GS, Croft JB. Sleep duration and body mass index and waist circumference among U.S. adults. Obesity. 2014;22:598–607. doi: 10.1002/oby.20558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 44.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–3. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 45.Nielsen LS, Danielsen KV, Sorensen TI. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev. 2011;12:78–92. doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 46.National Sleep Foundation. Washington, DC: National Sleep Foundation; 2005. Sleep in America Poll. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


