Abstract
Objective To examine the association between payments made by the manufacturers of pharmaceuticals to physicians and prescribing by physicians within hospital referral regions.
Design Cross sectional analysis of 2013 and 2014 Open Payments and Medicare Part D prescribing data for two classes of commonly prescribed, commonly marketed drugs: oral anticoagulants and non-insulin diabetes drugs, overall and stratified by physician and payment type.
Setting 306 hospital referral regions, United States.
Participants 45 949 454 Medicare Part D prescriptions written by 623 886 physicians to 10 513 173 patients for two drug classes: oral anticoagulants and non-insulin diabetes drugs.
Main outcome measures Proportion, or market share, of marketed oral anticoagulants and non-insulin diabetes drugs prescribed by physicians among all drugs in each class and within hospital referral regions.
Results Among 306 hospital referral regions, there were 977 407 payments to physicians totaling $61 026 140 (£46 174 600; €54 632 500) related to oral anticoagulants, and 1 787 884 payments totaling $108 417 616 related to non-insulin diabetes drugs. The median market share of the hospital referral regions was 21.6% for marketed oral anticoagulants and 12.6% for marketed non-insulin diabetes drugs. Among hospital referral regions, one additional payment (median value $13, interquartile range, $10-$18) was associated with 94 (95% confidence interval 76 to 112) additional days filled of marketed oral anticoagulants and 107 (89 to 125) additional days filled of marketed non-insulin diabetes drugs (P<0.001). Payments to specialists were associated with greater prescribing of marketed drugs than payments to non-specialists (212 v 100 additional days filled per payment of marketed oral anticoagulants, 331 v 114 for marketed non-insulin diabetes drugs, P<0.001). Payments for speaker and consulting fees for non-insulin diabetes drugs were associated with greater prescribing of marketed drugs than payments for food and beverages or educational materials (484 v 110, P<0.001).
Conclusions and study limitations Payments by the manufacturers of pharmaceuticals to physicians were associated with greater regional prescribing of marketed drugs among Medicare Part D beneficiaries. Payments to specialists and payments for speaker and consulting fees were predominantly associated with greater regional prescribing of marketed drugs than payments to non-specialists or payments for food and beverages, gifts, or educational materials. As a cross sectional, ecological study, we cannot prove causation between payments to physicians and increased prescribing. Furthermore, our findings should be interpreted only at the regional level. Our study is limited to prescribing by physicians and the two drug classes studied.
Introduction
Pharmaceutical manufacturers spend billions of dollars annually in payments to physicians in the form of food and beverages, gifts, and educational materials, as well as for speaker and consulting fees.1 These payments compensate physicians for clinical and scientific input, support educational events, and promote products. Most physicians believe these gifts do not influence their prescribing.2 3 4 5 However, many studies have shown that physician detailing6 and overall marketing expenditures by the manufacturers of pharmaceuticals6 7 are associated with greater prescribing of marketed drugs, although these studies did not have data on payments to physicians. Studies from more than 20 years ago showed that physicians who receive payments from manufacturers were more likely to prescribe or recommend the manufacturer’s products.8 9 10 However, these single institution studies were largely based on self reports of payments and prescribing. More recent data provide a unique opportunity to better understand whether payments to physicians from the manufacturers of pharmaceuticals are associated with prescribing behavior.
The Open Payments program, enacted as part of the Affordable Care Act, mandated manufacturers of pharmaceuticals and medical devices to report payments to physicians and teaching hospitals to the Centers for Medicare & Medicaid Services (CMS). The resulting data include direct and indirect payments as well as payments in kind, such as the value of food and gifts, and detail the manufacturers’ products associated with the payment (see box 1). We used 2013 and 2014 data on Open Payments, along with Medicare Part D pharmaceutical prescribing data over the same period, to examine associations between payments to physicians and prescribing within hospital referral regions for drugs within two of the most commonly prescribed and commonly marketed drug classes: oral anticoagulants and non-insulin diabetes drugs.11 We focused our analyses on hospital referral regions, as previous work has shown regional variation in the prescribing of branded versus generic drugs for Part D beneficiaries,12 and in order to capture the effect of payments to physicians on broader prescribing, perhaps through peer effects. As part of this effort, we also examined whether payment-prescribing associations differed between specialist and non-specialist physicians (see box 1) or between payment types. Payments reported include those generally intended for physicians who provide expert guidance, also known as “key opinion leadership,”13 14 through speaking to and educating the clinical community, as well as payments likely intended for physicians who receive information from these expert physicians and from representatives of manufacturers, such as food and beverages and journal articles. We hypothesised that payments to specialists and payments such as speaker fees, consulting fees, honorariums, travel costs, and non-research grants would have a greater impact on prescribing than payments to non-specialists or payments for food and beverages, gifts, or educational materials such as journal articles and textbooks.
Methods
Data sources and sample—Open Payments data
Payments from pharmaceutical and medical device manufacturers to physicians and academic medical centers reported by manufacturers to CMS were available from August 2013 through December 2014, the entirety of the Open Payments program thus far. The program requires reporting of payments for speaker fees for education lectures, consulting fees, honorariums, gifts, food and beverages, journal article reprints or textbooks, travel and lodging, research support, grants, charitable donations in lieu of payment, fees for rental of space or use of facility, and royalties or licensing fees. Items intended for use with or by patients, or payments to physicians totaling less than $100 in a year, were exempt from reporting.
We included payments to allopathic and osteopathic physicians and excluded payments to academic medical centers and non-physician clinicians. CMS did not require payments to non-physician clinicians to be reported, and though there was some voluntary reporting, the extent and uniformity of reporting is unclear. We excluded payments for research and royalties, or reports of ownership or investments, as such payments are substantially larger than other types of payments, potentially biasing our results, and some are compensation for intellectual property. We aggregated all payments to hospital referral regions using national provider identifiers, the practice zip code of the recipient in the national plan and provider enumeration system, and a Dartmouth Atlas hospital referral region-zip code crosswalk.15 We excluded payments not linked to a national provider identifier, and recipient zip codes not assigned a hospital referral region (see supplement for details).
Data sources and sample—Medicare Part D data
Medicare Part D provided drug coverage to more than 37 million fee-for-service and Medicare Advantage beneficiaries in 2014, representing 70% of all eligible Medicare beneficiaries.16 We used prescribing data from the CMS prescription drug event database for the last five months of 2013, and calendar year 2014, overlapping with the available payment data. The prescribing data contained both the generic and the brand (if any) names of the prescriptions filled, the number of days of drug filled, and the national provider identifier of the prescriber. Prescriptions were aggregated to hospital referral regions using the same process used for payment data as described above and were linked to payments using national provider identifiers with exact matching (see supplement for details).
Hospital referral region aggregated payments to physicians
We identified payments associated with two drug classes: oral anticoagulants and non-insulin diabetes drugs. For each of the two drug classes we calculated the aggregate number and dollar value of payments per 1000 person years of Part D coverage for each hospital referral region. Since the number of Medicare Part D enrollees varies throughout the calendar year,17 we used the total number of months of Part D coverage during calendar year 2014 to calculate person years of coverage per hospital referral region.
Payments per 1000 person years of Part D coverage were calculated overall by physician type and by payment type. We categorized physicians as specialists and as non-specialists based on which physicians in the United States are generally considered experts relative to the drug class’ major indication and use (see box 1). Oral anticoagulants are most commonly used for atrial fibrillation and venous thromboembolism, thus we considered cardiologists and hematologists as specialists for oral anticoagulants, and endocrinologists as specialists for non-insulin diabetes drugs. We categorized all other physicians as non-specialists. We also categorized payments as those generally intended for “key opinion leadership,” including speaker fees, consulting fees, honorariums, travel costs, and non-research grants, or as those generally intended for physicians who receive information from these expert physicians and from representatives of manufacturers, including food and beverages, gifts, or educational materials such as journal articles and textbooks.
Hospital referral region aggregated prescribing by physicians
We identified all Medicare Part D prescriptions written by physicians for two drug classes: oral anticoagulants and non-insulin diabetes drugs. Oral anticoagulants included warfarin and the direct thrombin and factor Xa inhibitors (see supplement table 1); we excluded oral antiplatelet drugs such as clopidogrel because their indications and use are different from those of other oral anticoagulants, as well as aspirin because it is an over-the-counter drug. Non-insulin diabetes drugs included biguanides, sulfonylureas, thiazolidinediones, dipeptidyl peptidase-4 inhibitors, glucagon-like peptide 1 receptor agonists, meglitinides, and sodium-glucose cotransporter 2 inhibitors.
Within each class we categorized drugs as marketed or non-marketed (see supplement table 1); a marketed drug was defined as any drug for which there were 100 payments or more during the study period. Of note, generic drugs are included in our analysis, but there were no generic drugs for which physicians received a sufficient number of payments to be considered “marketed,” with one exception: a generic version of the diabetes drug metformin, marketed as Glumetza. Thus, we categorized all Glumetza prescriptions (0.19% of all metformin prescriptions) as marketed drugs.
For each of the two drug classes, we calculated the market share (%) of prescription days filled of the marketed drug from among all drugs within the drug class within a hospital referral region. Here is an example to clarify how market share was calculated. Among oral anticoagulants, dabigatran, rivaroxaban, and apixaban were marketed drugs, whereas warfarin was the only non-marketed drug in the class. In a hypothetical hospital referral region with 100 prescription days filled by oral anticoagulants, if 20 prescription days filled were for dabigatran, rivaroxaban, and apixaban, whereas 80 prescriptions days filled were for warfarin, the market share for marketed oral anticoagulants would be calculated to be 20%.
Covariates
We included measures of patient age, sex, race, income status, and clinical comorbidity, as measured using the hierarchical condition category score. CMS uses these scores to adjust payments to Medicare Advantage insurers according to beneficiaries’ risk. Scores are calculated using personal, diagnoses, and disease factors. We obtained these measures from the chronic conditions warehouse at the individual level for all Part D enrollees. We then calculated mean age and hierarchical condition category score at the level of hospital referral region, along with the proportion of Part D enrollees of female sex, minority race, and of enrollees eligible for Part D subsidies, a surrogate marker of beneficiary income. We also included estimated median household income for 2014 from the US census’ American community survey. The estimates were obtained at the zip code tabulation area level and aggregated to the hospital referral region level (see supplement for details).
Statistical analysis
Independent analyses were carried out for each drug class. We used descriptive statistics to estimate the median number and value of payments per 1000 person years of Part D coverage across hospital referral regions, along with the median days filled of the marketed drug. We used linear regression models fitted using ordinary least squares to analyze the association between payments and prescribing at the level of hospital referral region, calculating the predicted change in market share associated with one payment per 1000 person years of coverage. We then calculated the effect of the predicted change in market share on the days filled of the marketed drug associated with one additional payment. All analyses were adjusted for hospital referral region age, sex, race, income, and hierarchical condition category, and these were repeated, stratified by physician and payment type. We then evaluated whether it was the number of payments or the dollar value of payments that was underlying the association between payments and prescribing. For this we compared the effect magnitude of an additional payment in a region to the effect of an increase in the average dollar value of those payments. We then calculated the predicted market share change associated with a one unit increase in the number of payments versus a dollar value equivalent increase in the size of an average payment (see supplement for details).
Analysis and data visualization were conducted using Stata (StataCorp) and ArcGIS (Esri).
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
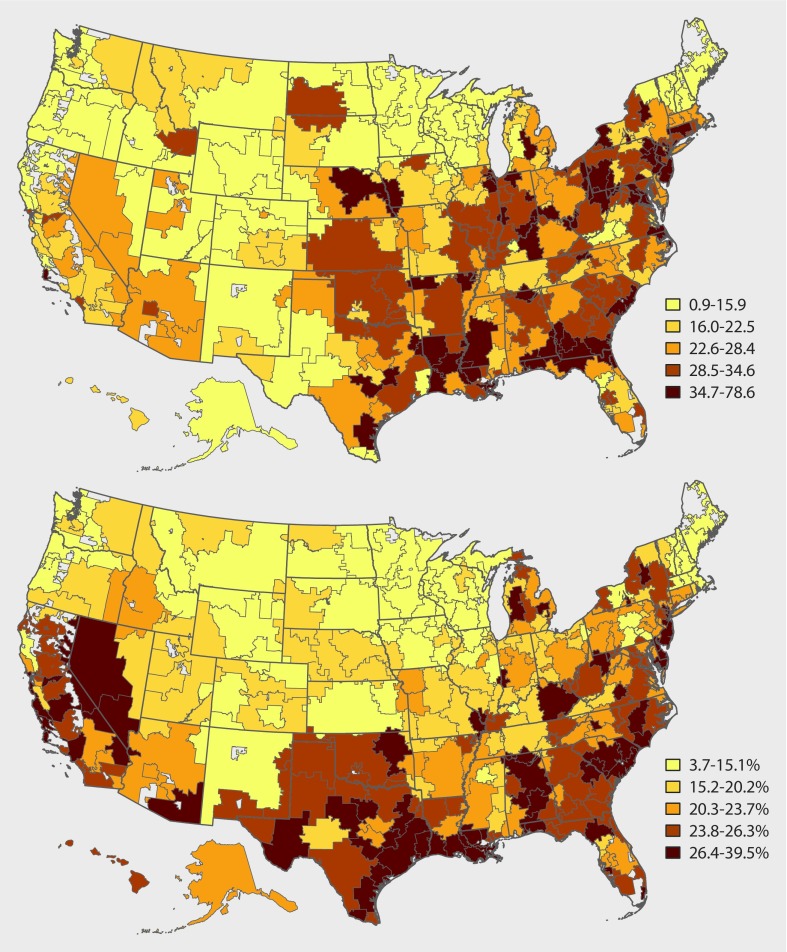
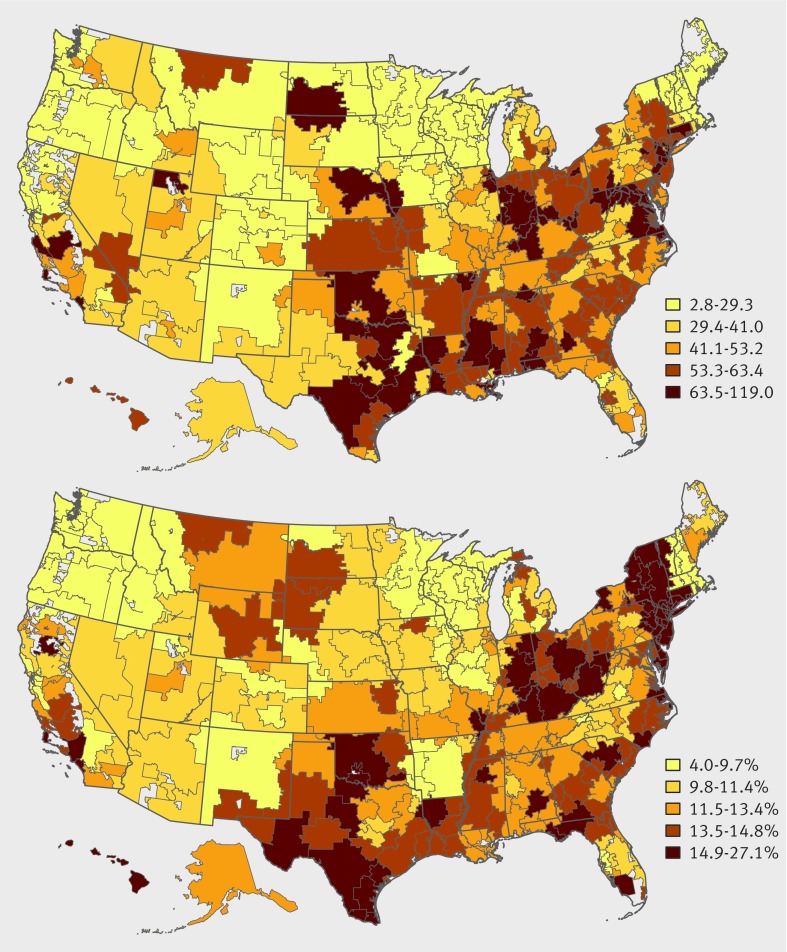
Among 306 hospital referral regions, 977 407 payments to 120 110 physicians were related to oral anticoagulants (table 1). Among all hospital referral regions, the median number of payments per 1000 person years of Part D coverage was 25.4 (interquartile range 18-33) and the median value of payments was $13 ($10-$17). The top panel in figure 1 illustrates the distribution of the number of payments for oral anticoagulants by hospital referral region, categorized by fifths. In addition, among 306 hospital referral regions, there were 14 855 478 prescriptions for oral anticoagulants for 3 469 152 patients by 308 622 physicians, totaling 1 106 613 241 filled prescription days. Among all hospital referral regions, the median market share for marketed oral anticoagulants was 21.6% (16-26%). The bottom panel in figure 1 illustrates the distribution of the market share for marketed oral anticoagulants by hospital referral region, categorized by fifths.
Table 1.
Number and dollar value of payments to physicians for two classes of drugs studied, by physician and payment type
| Payments | Oral anticoagulants | Non-insulin diabetes drugs | |||
|---|---|---|---|---|---|
| No (%) | Sum $ (%) | No (%) | Sum $ (%) | ||
| Overall payments | 977 407 | 61 026 140 | 1 787 884 | 108 417 616 | |
| Payments by physician type: | |||||
| Specialists | 306 801 (31) | 36 172 546 (59) | 199 482 (11) | 59 900 148 (55) | |
| Non-specialists | 670 606 (69) | 24 853 593 (41) | 1 588 402 (89) | 48 517 467 (45) | |
| Payment type: | |||||
| For speaker fees, consulting fees, honorariums, travel costs, and non-research grants | 33 267 (3) | 43 773 562 (72) | 74 368 (4) | 77 477 450 (71) | |
| For food and beverages, gifts, or educational materials | 944 140 (97) | 17 252 578 (28) | 1 713 516 (96) | 30 940 165 (29) | |
Fig 1 Distribution of payments by pharmaceutical manufacturers to physicians, and physician prescribing of marketed drugs among Medicare Part D beneficiaries for oral anticoagulants, by hospital referral region. Payments per 1000 person years of Part D coverage for oral anticoagulants (top panel); market share (%) of marketed oral anticoagulants (bottom panel)
Among 306 hospital referral regions, there were 1 787 884 payments to 111 936 physicians related to non-insulin diabetes drugs (table 1). Among all hospital referral regions, the median number of payments per 1000 person years of Part D coverage was 47.5 (33-61) and the median value of payments was $13 ($10-$18). The top panel in figure 2 illustrates the distribution of the number of payments for non-insulin diabetes drugs by hospital referral region, categorized by fifths. In addition, among these 306 hospital referral regions, there were 31 093 976 prescriptions for diabetes drugs for 7 044 021 patients by 315 264 physicians, totaling 3 413 562 498 filled prescription days. Among all hospital referral regions, the median market share for marketed non-insulin diabetes drugs in hospital referral regions was 12.6% (10-14%). The bottom panel in figure 2 illustrates the distribution of the market share for marketed non-insulin diabetes drugs by hospital referral region, categorized by fifths.
Fig 2 Distribution of payments by pharmaceutical manufacturer to physicians, and physician prescribing of marketed drugs among Medicare Part D beneficiaries for non-insulin diabetes drugs, by hospital referral region. Payments per 1000 person years of Part D coverage for non-insulin diabetes drugs (top panel); market share (%) of marketed non-insulin diabetes drugs (bottom panel)
Association of payments and prescribing
For both oral anticoagulants and non-insulin diabetes drugs, we found that the number of payments to physicians was associated with greater prescribing of marketed drugs within a hospital referral region. After adjustment for age, sex, race, income, and hierarchical condition category risk score, one payment per 1000 person years of Part D coverage was associated with a 0.32% increase in market share for marketed oral anticoagulants and a 0.12% increase for marketed non-insulin diabetes drugs (table 2). In prescribing terms, one additional payment in a hospital referral region (median dollar value $13) was associated with 94 (95% confidence interval 76 to 112) and 107 (89 to 125) additional days filled of the marketed drug for oral anticoagulants and non-insulin diabetes drugs, respectively.
Table 2.
Changes in market share of marketed drugs and association of regional prescribing with all payments, payments to specialists versus non-specialists, and food and education payments versus speaker and consulting payments
| Payments | Oral anticoagulants | Non-insulin diabetes drugs | |||||
|---|---|---|---|---|---|---|---|
| Market share change* (95% CI) | P value | Days filled per payment†(95% CI) | Market share change* (95% CI) | P value | Days filled per payment† (95% CI) | ||
| All payments to all physicians | 0.32 (0.26 to 0.38) | <0.001 | 94 (76 to 112) | 0.12 (0.1 to 0.14) | <0.001 | 107 (89 to 125) | |
| Payment by physician type: | |||||||
| Non-specialists | 0.32 (0.23 to 0.41) | <0.001 | 100 (68 to 123) | 0.12 (0.01 to 0.15) | <0.001 | 114 (93 to 144) | |
| Specialists | 0.71 (0.58 to 0.84) | <0.001 | 212 (174 to 250) | 0.36 (0.25 to 0.47) | <0.001 | 331 (230 to 442) | |
| P value for difference between groups | <0.001 | <0.001 | |||||
| Payment type: | |||||||
| For food and beverage, gifts, or educational materials | 0.32 (0.23 to 0.41) | <0.001 | 96 (77 to 114) | 0.12 (0.01 to 0.14) | <0.001 | 110 (91 to 128) | |
| For speaker fees, consulting fees, honoraria, travel costs, and non-research grants | 1.09 (0.21 to 1.98) | 0.02 | 326 (62 to 590) | 0.53 (0.24 to 0.81) | <0.001 | 484 (222 to 745) | |
| P value for difference between groups | 0.17 | 0.01 | |||||
*Percent change in market share for one additional payment per 1000 person years of Part D coverage in an hospital referral region.
†Number of additional prescription days filled of marketed drug associated with an increase of one payment in a region.
Payments to specialist versus non-specialist physicians
For both oral anticoagulants and non-insulin diabetes drugs, payments to specialists were associated with greater regional prescribing of marketed drugs than payments to non-specialists (P<0.001). For oral anticoagulants, payments to specialists represented 31% of the total number of payments and 59% of the sum value of payments, whereas for non-insulin diabetes drugs, payments to specialists represented 11% of the total number of payments and 55% of the sum value of payments (table 1). For oral anticoagulants, an increase of one payment per 1000 person years to cardiologists or hematologists was associated with a 0.71% increase in regional market share, compared with 0.32% for other physicians, translating to 212 (95% confidence interval 174 to 250) and 100 (68 to 123) additional days filled of the marketed drug for one additional payment, respectively. For non-insulin diabetes drugs, the corresponding association was a 0.36% and a 0.12% increase, translating to 331 (230 to 442) and 114 (93 to 144) additional days filled of the marketed drug for one additional payment in a region, respectively (table 2; P values <0.001).
Type of payment
For non-insulin diabetes drugs but not for oral anticoagulants, payments for speaker fees, consulting fees, honorariums, travel costs, and non-research grants were associated with greater regional prescribing of marketed drugs than payments for food and beverage gifts or educational materials. Payments for speaker fees, consulting fees, honorariums, travel costs, and non-research grants represented 4% of the total number of payments and 72% of the sum payment dollar value (table 1). For oral anticoagulants, an increase of one payment per 1000 person years for speaker fees, consulting fees, honorariums, travel costs, and non-research grants was associated with a 1.09% increase in market share, compared with 0.32% for food and beverages, gifts, or educational materials (P=0.17), translating to 326 (95% confidence interval 62 to 590) and 96 (77 to 114) additional days filled of the marketed drug for one additional payment in a region, respectively. For non-insulin diabetes drugs, the corresponding impact was a 0.53% and a 0.12% increase (P=0.007), translating to 484 (222 to 745) and 110 (91 to 128) additional days filled of the marketed drug for one additional payment in a region, respectively (table 2).
Number of payments versus average dollar value of payments
For both oral anticoagulants and non-insulin diabetes drugs, the number of payments was associated with greater regional prescribing of marketed drugs than a dollar equivalent increase in the average value of those payments. For oral anticoagulants, an increase of one in the number of payments per 1000 person years of Part D coverage (average payments per hospital referral region=26) was associated with a 0.25% (95% confidence interval 0.20% to 0.31%, P<0.001) increase in prescribing of marketed drugs, whereas an equivalent change in the average value of payments ($2 per payment; average payment $54) was associated with a 0.04% (0.01% to 0.08%, P=0.01) increase in prescribing. For non-insulin diabetes drugs, an increase of one in the number of payments (average payments per hospital referral region=47) was associated with a 0.09% (0.07% to 0.11%) increase in prescribing, whereas an equivalent change in the average value of payments ($1.16 per payment; average payment $55) was not significantly associated with prescribing (0.003%, −0.278 to 0.010, P=0.57).
Discussion
In this analysis of Open Payments and Medicare Part D data, payments from manufacturers of pharmaceuticals to physicians were associated with greater regional prescribing of both marketed oral anticoagulant and non-insulin diabetes drugs among Medicare Part D beneficiaries. Payments to specialists and payments for speaker fees, consulting fees, honorariums, travel costs, and non-research grants were associated with greater regional prescribing of marketed drugs than payments to non-specialists or payments for food and beverage, gifts, or educational materials. In addition, we found that the number of payments within a hospital referral region was associated with greater regional prescribing of marketed drugs than dollar equivalent increases in the average value of payments.
In separate analyses for oral anticoagulants and non-insulin diabetes drugs, we found similar overall regional payment-prescribing associations, and for both drug classes, payments to non-specialists were associated with less regional prescribing than payments to specialists. It is notable that while the proportion of the sum value of payments for specialists was similar for oral anticoagulants and non-insulin diabetes drugs (59% and 55% of the total sum value spent in drug class, respectively, table 1), cardiologists and hematologists accounted for a larger proportion of payments for oral anticoagulants than endocrinologists did for diabetes drugs (31% v 11%). This may be due to there being many more practicing cardiologists and hematologists in the United States (22 020 and 13 774, respectively)18 than practicing endocrinologists (6519). Furthermore, while the overall payment types were similar between the drug classes (see supplement table 3a), endocrinologists received far more payments for speaking and consulting fees than cardiologists and hematologists (28 518 v 14 159, supplement tables 3b and 3c).
Before the Open Payments program was initiated, the scope and frequency of payments to physicians was poorly understood. Surveys of physicians and state specific disclosure data suggested that payments were common, but most often were for lower value items such as food and beverages and educational materials.19 This finding is consistent with our work and other early analyses of the Open Payments data.20 21 22 23 24 25 26 Our findings are also consistent with a physician level analysis of payments to physicians in Massachusetts and statin prescribing,27 which showed increased prescribing of brand names among physicians who received payments from industry.
Our analysis also showed that these small payments are associated with greater regional prescribing of marketed oral anticoagulants and non-insulin diabetes drugs, such that one additional payment in an average hospital referral region, despite a median value of only $13, was associated with nearly three months of additional prescription days filled of the marketed over a 17 month period. Of note, the $13 encompasses only the value transferred to the physician and not the overall cost to the manufacturer, which includes the development of promotional material and the salary and travel expenses of the detailing representative, among others. Thus, it is not possible to calculate the “return on investment” based solely on Open Payments data. Our findings also showed that though less frequent, certain payments, such as those for specialists, as well as payments generally intended for physicians who provide “key opinion leadership” through speaking to and educating the clinical community, have demonstrably larger effects on the prescribing of marketed drugs within hospital referral regions among all physicians.
Our findings do not necessarily suggest that payments by pharmaceutical manufacturers are harmful for patient care. Patients may benefit from physicians being made aware of newly approved, effective treatments that may have fewer adverse effects, reduce the need for monitoring tests, or improve adherence. However, our findings support long voiced concerns about the potential influence of even small payments to physicians by pharmaceutical companies, such as for food and beverages.28 29 30 This influence on prescribing can potentially negatively affect patients through inappropriate prescribing, or more likely prescribing of more expensive branded drugs when cheaper, generic alternatives exist. By one estimate, the geographic variation in high cost or low cost drug prescribing cost Medicare $4.5bn in 2008.12
Since the advent of Open Payments in the United States, there have been increasing efforts at improving transparency of the relations between industry and medicine in other countries, including England, Scotland, France, Denmark, Australia, and others.31 The European Federation of Pharmaceutical Industries and Associations, a Brussels based trade association of large pharmaceutical manufacturers, voluntarily adopted payment disclosure guidelines in 2013, with reporting to begin in June 2016, though implementation will vary by country.31 32 Some of these regulations go even farther than Open Payments, with the French Sunshine Act mandating disclosures of payments to all clinicians, not just physicians, and levying financial penalties for non-disclosure.33 Payments to physicians may have declined in the United States in expectation of increased transparency,34 but any effect on the larger drug market or on patient care is unclear. However, disclosure of these payments may have greater impact in countries with tighter control of formularies and drug prices than in the US pharmaceutical market.
Limitations of this study
Our study has important limitations. Firstly, as the study was cross sectional, we cannot prove the causality that marketing causes prescribing; it is possible that pharmaceutical companies market in regions where prescribing is already higher. Secondly, our results likely underestimate the association between payments by the manufacturers of pharmaceuticals and physician prescribing since we only had data on prescriptions filled, not prescribed, and our analyses were focused solely on Medicare Part D enrollees, who receive approximately 25% of all prescriptions written in the United States.35 Furthermore, our data only included prescriptions filled during the 17 months for which payment data were available, whereas the influence of payments might last beyond the date of payment through a persistent effect on prescribing over subsequent months36 and because of the likelihood that once patients start a drug, they tend to remain with that drug.37 Thirdly, our data included only payments for 17 months; thus we were not able to differentiate any effect of payments made to physicians prior to this period. Fourthly, while the hospital referral region aggregated data allowed us to evaluate the regional association of payments and prescribing, as well as the impact of payments to “key opinion leaders” on regional prescribing, the potential of ecological fallacy38 limits individual level inferences. Fifthly, we did not have access to data on other forms of pharmaceutical marketing, such as direct to consumer marketing, journal advertisements, or physician interactions with pharmaceutical representatives that do not involve a transfer of value or payment, which may also affect prescribing.10 Sixthly, to address possible incomplete reporting in the initial months of Open Payments, we conducted a sensitivity analysis for oral anticoagulants using only 2014 data and found that the estimated associations between payment and prescribing had somewhat larger magnitudes of effect (see table 2 in supplement). Finally, formularies have known associations with prescribing,39 and they vary across the more than 2500 drug plans available to Medicare Part D beneficiaries nationwide, with up to 250 active formularies in some hospital referral regions. We were thus unable to control for the differences in formularies across hospital referral regions. However, our examination of the 2014 Medicare Part D formulary coverages for non-insulin diabetes drugs showed that 97% included at least one marketed non-insulin diabetes drug on tier 1 or tier 2 of its formulary, implying that the drug was preferred and available at low to modest cost to beneficiaries. Therefore, though formularies likely varied across hospital referral regions, this variation is unlikely to fully account for regional variation in prescribing.
Conclusion
Payments by the manufacturers of pharmaceuticals to physicians were associated with greater regional prescribing of marketed oral anticoagulant and non-insulin diabetes drugs among Medicare Part D beneficiaries. Physicians and policymakers should consider these findings and their implications for patient care when establishing personal, institutional, or legislative policy related to payments by manufacturers of pharmaceuticals to physicians.
Box 1: US Open Payments program, and study definitions
Open Payments
A program initiated as part of the 2010 Affordable Care Act and administered by the US Centers for Medicare and Medicaid Services
Manufacturers of pharmaceuticals and devices are required to report most transfers of value to physicians, which include items such as food and beverages and speaker and consulting fees
The data are searchable through a US government website and available to the public
Medicare Part D
Provides drug coverage to Medicare beneficiaries. In 2014, Part D provided drug coverage to more than 37 million Medicare beneficiaries, representing 70% of eligible Medicare beneficiaries
Hospital referral region
Hospital referral regions represent regional healthcare markets for tertiary medical care, and are commonly used to examine regional variation in care. Each hospital referral region contains at least one hospital that performs major cardiovascular procedures and neurosurgery
Specialists versus non-specialists
In the United States, general practitioners may refer patients with atrial fibrillation for consultation with a cardiologist to advise on management. Similar consultations are common with hematologists for the care of patients with venous thromboembolism, and with endocrinologists for the care of patients with diabetes
Oral anticoagulants are most commonly used for atrial fibrillation and venous thromboembolism, thus in this study cardiologists and hematologists were categorized as specialists for oral anticoagulants. All other physicians were considered non-specialists
Endocrinologists were considered specialists for non-insulin diabetes drugs. All other physicians were considered non-specialists
Marketed versus non-marketed drugs and market share
A drug was considered “marketed” if 100 reported payments were made to physicians during the study period
Nearly all marketed drugs were brand name versions without generic equivalents
We calculated the market share (%) of prescription days filled by marketed drugs from among all prescription days filled within the drug class
For example, in a hypothetical hospital referral region with 100 prescription days filled for oral anticoagulants, if 20 prescription days filled were for marketed dabigatran, rivaroxaban, and apixaban, while 80 prescriptions days filled were for non-marketed warfarin, the market share for marketed oral anticoagulants would be calculated to be 20%
What is already known on this topic
Pharmaceutical manufacturers spend billions of dollars annually in payments to physicians
Most physicians believe these gifts do not influence their prescribing
Several small studies have suggested that payments influence prescribing
What this study adds
Newly available data on payments and on prescribing covering a large swath of US physicians and patients suggest that payments to physicians are associated with substantial differences in regional prescribing
One additional payment in a region (median value $13) was associated with approximately 80 additional days filled of the marketed drug in the region
Payments to specialists and payments for speaking and consulting fees were associated with larger regional changes in prescribing than payments for non-specialists or payments for food and beverages or education
Web extra.
Extra material supplied by authors
Supplement: supplementary online content
We thank David J Margolis and Douglas J Wiebe of the University of Pennsylvania for their input on study design, and the staff at the Yale Center for Research Computing for their analysis support. None of the acknowledged received financial compensation.
Contributors: WF conceived and designed the study assisted by SA, MK, AKV, DMcK, and JSR. WF acquired the data and performed analyses assisted by MK and DMcK, and interpreted the data assisted by all authors. WF drafted the manuscript and all authors critically revised it. JSR and SA supervised the study. WF is the guarantor and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
Funding: This work was not supported by any external grants or funds.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: WF serves as a volunteer researcher at the Centers for Medicare and Medicaid Services (CMS), the agency that administers the Open Payments program. SA and DB worked at CMS at the time of writing. AKV, HMK, and JSR receive support through Yale University from CMS to develop and maintain performance measures that are used for public reporting. HMK and JSR receive support through Yale University from Medtronic and Johnson and Johnson to develop methods for the sharing of clinical trial data, from the Blue Cross Blue Shield Association to better understand the generation of medical technology evidence, and from the Food and Drug Administration to develop methods for post-market surveillance of medical devices.
Ethical approval: Yale University institutional review board approved and provided oversight of this study.
Data sharing: Requests for the statistical code can be made to the corresponding author at wf3@buffalo.edu.
Transparency: The lead author (WF) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
- 1.Centers for Medicare & Medicaid Services. Open Payments Data Summary. OpenPaymentsData.CMS.gov https://openpaymentsdata.cms.gov/summary (accessed 2 Aug 2016).
- 2.Austad KE, Avorn J, Franklin JM, Kowal MK, Campbell EG, Kesselheim AS. Changing interactions between physician trainees and the pharmaceutical industry: a national survey. J Gen Intern Med 2013;28:1064-71. 10.1007/s11606-013-2361-0 pmid:23444007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halperin EC, Hutchison P, Barrier RC Jr. A population-based study of the prevalence and influence of gifts to radiation oncologists from pharmaceutical companies and medical equipment manufacturers. Int J Radiat Oncol Biol Phys 2004;59:1477-83. 10.1016/j.ijrobp.2004.01.052 pmid:15275735. [DOI] [PubMed] [Google Scholar]
- 4.Steinman MA, Shlipak MG, McPhee SJ. Of principles and pens: attitudes and practices of medicine housestaff toward pharmaceutical industry promotions. Am J Med 2001;110:551-7. 10.1016/S0002-9343(01)00660-X pmid:11347622. [DOI] [PubMed] [Google Scholar]
- 5.Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift?JAMA 2000;283:373-80. 10.1001/jama.283.3.373 pmid:10647801. [DOI] [PubMed] [Google Scholar]
- 6.Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med 2010;7:e1000352 10.1371/journal.pmed.1000352 pmid:20976098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King M, Essick C. The geography of antidepressant, antipsychotic, and stimulant utilization in the United States. Health Place 2013;20:32-8. 10.1016/j.healthplace.2012.11.007 pmid:23357544. [DOI] [PubMed] [Google Scholar]
- 8.Orlowski JP, Wateska L. The effects of pharmaceutical firm enticements on physician prescribing patterns. There’s no such thing as a free lunch. Chest 1992;102:270-3. 10.1378/chest.102.1.270 pmid:1623766. [DOI] [PubMed] [Google Scholar]
- 9.Bowman MA, Pearle DL. Changes in drug prescribing patterns related to commercial company funding of continuing medical education. J Contin Educ Health Prof 1988;8:13-20. 10.1002/chp.4750080104 pmid:10294441. [DOI] [PubMed] [Google Scholar]
- 10.Chren MM, Landefeld CS. Physicians’ behavior and their interactions with drug companies. A controlled study of physicians who requested additions to a hospital drug formulary. JAMA 1994;271:684-9. 10.1001/jama.1994.03510330062035 pmid:8309031. [DOI] [PubMed] [Google Scholar]
- 11.Ornstein C, Grochowski Jones R. Vying for Market Share, Companies Heavily Promote “Me Too” Drugs. ProPublica 2015. http://bit.ly/1xScCd2 (accessed 2 Aug 2016).
- 12.Donohue JM, Morden NE, Gellad WF, et al. Sources of regional variation in Medicare Part D drug spending. N Engl J Med 2012;366:530-8. 10.1056/NEJMsa1104816 pmid:22316446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moynihan R. Key opinion leaders: independent experts or drug representatives in disguise?BMJ 2008;336:1402-3. 10.1136/bmj.39575.675787.651 pmid:18566074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steensma DP. Key Opinion Leaders. J Clin Oncol 2015;33:3213-4. 10.1200/JCO.2015.63.1275 pmid:26261246. [DOI] [PubMed] [Google Scholar]
- 15.The Dartmouth Institute for Health Policy and Clinical Practice. The Dartmouth Atlas of Health Care. http://bit.ly/28zQV46 (accessed 2 Aug 2016).
- 16.Hoadley J, Summer L, Hargrave E, Cubanski J, Newman T. Medicare Part D in Its Ninth Year. Kaiser Family Foundation; 2014. http://kaiserf.am/1VpeYue (accessed 2 Aug 2016).
- 17.Centers for Medicare & Medicaid Services. Monthly Contract and Enrollment Summary Report. http://go.cms.gov/2avyBTl (accessed 2 Aug 2016).
- 18.2014 Physician Specialty Databook 2014. Association of American Medical Colleges; 2014. http://bit.ly/1td3hiO (accessed 2 Aug 2016).
- 19.Ross JS, Lackner JE, Lurie P, Gross CP, Wolfe S, Krumholz HM. Pharmaceutical company payments to physicians: early experiences with disclosure laws in Vermont and Minnesota. JAMA 2007;297:1216-23. 10.1001/jama.297.11.1216 pmid:17374816. [DOI] [PubMed] [Google Scholar]
- 20.Marshall DC, Jackson ME, Hattangadi-Gluth JA. Disclosure of Industry Payments to Physicians: An Epidemiologic Analysis of Early Data From the Open Payments Program. Mayo Clin Proc 2016;91:84-96. 10.1016/j.mayocp.2015.10.016 pmid:26763512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed R, Chow EK, Massie AB, et al. Where the Sun Shines: Industry’s Payments to Transplant Surgeons. Am J Transplant 2016;16:292-300. 10.1111/ajt.13427 pmid:26317315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jairam V, Yu JB. Examination of Industry Payments to Radiation Oncologists in 2014 Using the Centers for Medicare and Medicaid Services Open Payments Database. Int J Radiat Oncol Biol Phys 2016;94:19-26. 10.1016/j.ijrobp.2015.09.004 pmid:26547386. [DOI] [PubMed] [Google Scholar]
- 23.Rathi VK, Samuel AM, Mehra S. Industry ties in otolaryngology: initial insights from the physician payment sunshine act. Otolaryngol Head Neck Surg 2015;152:993-9. 10.1177/0194599815573718 pmid:25779469. [DOI] [PubMed] [Google Scholar]
- 24.Chang JS. The Physician Payments Sunshine Act: data evaluation regarding payments to ophthalmologists. Ophthalmology 2015;122:656-61. 10.1016/j.ophtha.2014.11.003 pmid:25578254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cvetanovich GL, Chalmers PN, Bach BR Jr. Industry Financial Relationships in Orthopaedic Surgery: Analysis of the Sunshine Act Open Payments Database and Comparison with Other Surgical Subspecialties. J Bone Joint Surg Am 2015;97:1288-95. 10.2106/JBJS.N.01093 pmid:26246264. [DOI] [PubMed] [Google Scholar]
- 26.Fleischman W, Ross JS, Melnick ER, Newman DH, Venkatesh AK. Financial Ties Between Emergency Physicians and Industry: Insights From Open Payments Data. Ann Emerg Med 2016;68:153-158.e4. 10.1016/j.annemergmed.2016.01.014 pmid:26973175. [DOI] [PubMed] [Google Scholar]
- 27.Yeh JS, Franklin JM, Avorn J, Landon J, Kesselheim AS. Association of Industry Payments to Physicians With the Prescribing of Brand-name Statins in Massachusetts. JAMA Intern Med 2016;176:763-8. 10.1001/jamainternmed.2016.1709 pmid:27159336. [DOI] [PubMed] [Google Scholar]
- 28.Waud DR. Pharmaceutical promotions--a free lunch?N Engl J Med 1992;327:351-3. 10.1056/NEJM199207303270511 pmid:1620175. [DOI] [PubMed] [Google Scholar]
- 29.Kassirer JP. A piece of my mind: financial indigestion. JAMA 2000;284:2156-7. 10.1001/jama.284.17.2156 pmid:11056568. [DOI] [PubMed] [Google Scholar]
- 30.Campbell EG. Doctors and drug companies--scrutinizing influential relationships. N Engl J Med 2007;357:1796-7. 10.1056/NEJMp078141 pmid:17978288. [DOI] [PubMed] [Google Scholar]
- 31.Campbell D, Sharkey B. Ready Or Not, Full Speed Ahead For The Global Transparency Movement. Porzio LifeSciences; 2015. http://bit.ly/1S2VQP3 (accessed 2 Aug 2016).
- 32.European Federation of Pharmaceutical Industries and Associations. EFPIA - The EFPIA Code. http://transparency.efpia.eu/the-efpia-code-2 (accessed 2 Aug 2016).
- 33.Atwill N. France: New Law on Drug Safety | Global Legal Monitor. Library of Congress; 2012. http://1.usa.gov/1YoaGau (accessed 2 Aug 2016).
- 34.Ornstein C, Sagara E, Grochowski Jones R. As Full Disclosure Nears, Doctors’ Pay for Drug Talks Plummets. ProPublica 2014. http://bit.ly/1hIMNEc (accessed 2 Aug 2016).
- 35.National Center for Health Statistics (US). Health, United States, 2013: With Special Feature on Prescription Drugs. Hyattsville (MD): National Center for Health Statistics (US); 2014. http://1.usa.gov/1w2lsqX (accessed 2 Aug 2016). [PubMed]
- 36.Narayanan S, Manchanda P, Chintagunta PK. Temporal Differences in the Role of Marketing Communication in New Product Categories. J Mark Res 2005;42:278-90 10.1509/jmkr.2005.42.3.278. [DOI] [Google Scholar]
- 37.Dailey G, Kim MS, Lian JF. Patient compliance and persistence with antihyperglycemic drug regimens: evaluation of a medicaid patient population with type 2 diabetes mellitus. Clin Ther 2001;23:1311-20. 10.1016/S0149-2918(01)80110-7 pmid:11558867. [DOI] [PubMed] [Google Scholar]
- 38.Robinson WS. Ecological correlations and the behavior of individuals. Int J Epidemiol 2009;38:337-41. 10.1093/ije/dyn357 pmid:19179346. [DOI] [PubMed] [Google Scholar]
- 39.Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med 2003;349:2224-32. 10.1056/NEJMsa030954 pmid:14657430. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement: supplementary online content