Abstract
Background
Lifecourse studies suggest that the metabolic syndrome (MetS) may be rooted in the early life environment. This study aims to examine the pathways linking early nutritional and psychosocial exposures and the presence of MetS in midlife.
Methods
Data are from the National Child Development Study including individuals born during 1 week in 1958 in Great Britain and followed-up until now. MetS was defined based on the National Cholesterol Education Program Adult Treatment Panel III classification. Mother’s pre-pregnancy body mass index (BMI) was used as a proxy of the early nutritional environment and Adverse Childhood Experiences (ACE) as a proxy for early psychosocial stress. Socioeconomic characteristics, pregnancy and birth conditions were extracted as potential confounders. Adult health behaviors, BMI, socioeconomic environment and psychological state were considered as mediating variables.
Multivariate models were performed by including variables sequentially taking a lifecourse approach.
Results
37.5 % of men and 19.8 % of women had MetS. Participants with an obese/overweight mother presented a higher risk of MetS than those whose mother had a normal pre-pregnancy BMI. Men exposed to two ACE or more, and women exposed to one ACE, were more at risk of MetS compared to unexposed individuals. After including confounders and mediators, mother’s pre-pregnancy BMI was still associated with MetS in midlife but the association was weakened after including participant’s adult BMI. ACE was no longer associated with MetS after including confounders in models.
Conclusions
The early nutritional environment, represented by mother’s pre-pregnancy BMI, was associated with the risk of MetS in midlife. An important mechanism involves a mother-to-child BMI transmission, independent of birth or perinatal conditions, socioeconomic characteristics and health behaviors over the lifecourse. However this mechanism is not sufficient for explaining the influence of mother’s pre-pregnancy BMI which implies the need to further explore other mechanisms in particular the role of genetics and early nutritional environment. ACE is not independently associated with MetS. However, other early life stressful events such as emergency caesarean deliveries and poor socioeconomic status during childhood may contribute as determinants of MetS.
Keywords: Metabolic syndrome, Early nutritional exposure, Early psychosocial exposures, Cohort studies, Social epidemiology, Lifecourse
Background
Metabolic syndrome (MetS) is a cluster of factors associated with a higher risk of type 2 diabetes, cardiovascular diseases and mortality [1, 2]. Although various definitions exist for MetS, its component factors generally include central obesity, dyslipidemia (elevated triglycerides, low high-density lipoproteins), hypertension and hyperglycemia. The prevalence of MetS is estimated at around 30 % in the US or in Europe for adult mainly above 30 years [3, 4] and it is likely to increase alongside the high frequency of related factors including obesity, sedentary lifestyles and unbalanced diets. Moreover recent evidence suggests a link between MetS and various chronic diseases such as cancer, notably through proinflammatory mechanisms and hormonal processes [3, 5, 6], but also cognitive decline [7] and dementia [8] through metabolic and vascular mechanisms. MetS is therefore potentially associated with a wide range of chronic diseases.
It has been suggested that MetS could be partly rooted in early life environments [9] and therefore taking a lifecourse perspective to understanding the development of MetS is relevant. Lifecourse studies have shown a relationship between socioeconomic position during childhood, measured retrospectively or prospectively, and the body mass index (BMI), ischaemic heart disease [10, 11] as well as MetS itself during adulthood [12–15]. One of the proposed pathways by which early socioeconomic conditions could influence MetS involves the early nutritional environment. In fact parental BMI, in particular maternal BMI, has been associated with offspring’s adiposity and BMI. Individuals whose parents had a higher BMI during their childhoods were more likely to be obese in adulthood [16]. Such lifecourse studies specifically on MetS are rarer, but evidence exists for a link between parental BMI and the subsequent risk for offspring to have higher levels of some components of MetS such as an atherosclerotic lipid profile [17]. This association seems to be explained only partially by adult lifestyles and lifetime socioeconomic position [16, 17]. Potential explanations for this parent–child BMI transmission may include biological mechanisms operating through genetic predisposition, prenatal “programming” during intrauterine and early development that constitute critical windows of development particularly sensitive to environmental challenges through activation of the stress axis and metabolic modifications involving epigenetic changes [18, 19], or shared environments such as cultural and familial eating patterns [20]. Whatever the mechanisms involved in the parent–child BMI transmission, they deserve to be further studied.
In addition to early nutritional exposures, another pathway by which early socioeconomic conditions could influence MetS involves early psychosocial stress. To study early life stress in human populations, adverse childhood experiences (ACE), that may be defined as a set of traumatic psychosocial conditions not under the child’s control that tend to co-occur usually before the age of 16, causing chronic or acute stress responses which may alter fundamental biological functions [21] like trauma abuse or maltreatment in childhood, have been used. Although definitions may vary, ACE has been identified as a factor influencing global physiological functioning in adulthood [22], impacting global health in particular cardiovascular health [23–25]. A large majority of such studies use retrospective measures for ACE some studies have also used a prospective measure and found it to be related to premature mortality [26], cancer risk [27] or cardiovascular health [28–30]. A number of mechanisms from animal to population studies linking early life stress and subsequent risk of symptoms composing MetS like obesity or glycemia have been proposed [31, 32] however, these pathways deserve to be examined in more detail.
An important remaining issue is to disentangle common and separate pathways by which both early nutritional and psychosocial stress can influence MetS. In fact, few studies combine both early nutritional and psychosocial stress as determinants of MetS. However biological links between nutrition and stress have been identified [33] and some common pathways may exist for these two exposures [34]. Identifying the respective role of early nutritional and psychosocial environment on the subsequent risk of MetS involves implementing studies to analyze the joint influence of these two exposures using a comprehensive lifecourse approach to take confounders into account and identify potential pathways.
Our study aims to investigate the pathways linking both early nutritional and psychosocial exposures to the presence of the MetS in midlife in the 1958 British birth cohort study taking a lifecourse approach. Three main pathways have been tested: (i) a socioeconomic/materialist pathway, (ii) a health behaviors pathway, (iii) a psychological pathway.
Method
This study used data from the 1958 National Child Development Study (NCDS) which included all births during 1 week in March 1958 (n = 18 558) in Great Britain. Subsequent data collections were carried out on cohort members aged 7, 11, 16, 23, 33, 42, 46 and 50 years. The NCDS has been described in detail elsewhere [35]. A biomedical survey (9377 cohort members participating) was conducted when participants were aged 44–46 years. The flow chart corresponding to the sample selection used for this study is presented in Fig. 1.
Fig. 1.
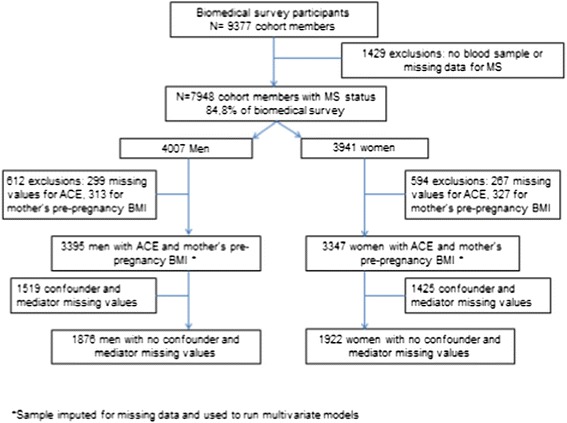
Flow chart showing the sample selection
Our study sample consisted of 3395 men and 3347 women with data on MetS and our two main exposure variables. The complete sample consisted respectively of 1876 men and 1922 women by defining complete cases as people with complete data for all the covariates.
Outcome variable
MetS was defined based on the NCEP-ATP III (National Cholesterol Education Program Adult Treatment Panel III) clinical criteria except for plasma glucose, which was not recorded in the NCDS biomedical survey and replaced here by using glycosylated hemoglobin (HbA1c) ≥6.5 %. MetS was identified at the age of 44–46 years old if three or more of the following occurred: blood pressure > =130/85 mmHg; High Density Lipoprotein <0.40 g/L for men and <0.50 g/l for women; Triglycerides > =150 mg/dL; waist circumference >88 cm for women and > 102 cm for men; HbA1c ≥6.5 % [36].
Exposure variables
Maternal BMI before pregnancy was used as a proxy of early nutritional stress, as an indicator of a high calorie/fat nutritional environment during pregnancy which has been identified as a risk factor of subsequent metabolic diseases [9]. Mother’s pre-pregnancy weight, that was self-reported at birth, and her height measured after the birth were used to construct maternal BMI before pregnancy and was grouped as follows: <18.5 kg/m2 for underweight, 18.5–24.9 for normal, 25–29.9 for overweight and ≥30 kg/m2 for obese adults.
Adverse childhood experiences (ACE) were used as a proxy of early psychosocial stress. Our measure of ACE has been presented in details in previous works [26, 27]. From previous works on ACE, specifically work conducted by a WHO expert committee in 2009 [37], we constructed a theoretical framework prior to extracting any data, in order to create a measurement with robust content validity. We have identified ACE as a set of traumatic and stressful psychosocial conditions that are out of the child’s control, that tend to co-occur and often persist over time. We have restricted ACE to intra-familial events or conditions in the child’s immediate environment causing chronic stress responses. From variables prospectively collected at age 7, 11, 16 by the child’s parent or their teacher, exposure to adversity was identified by a positive response to any of the following categories:
Child in care: child has ever been in public/voluntary care services or foster care at age 7, 11 or 16;
Physical neglect: child appears undernourished/dirty aged 7 or 11, information collected from the response from child’s teacher to the Bristol Social Adjustment Guide;
Offenders: The child lived in a household where a family member (person living in the same household as the child) was in prison or on probation (age 11 years) or is in contact with probation service at 7 or 11 years; the child has ever been to prison or been on probation at 16 years;
Parental separation: The child has been separated from their father or mother due to death, divorce, or separation at 7, 11 or 16 years;
Mental illness: Household has contact with mental health services at 7 or 11 years; Family member has mental illness at 7 and 11 or 16 years;
Alcohol abuse: Family member has alcohol abuse problem at 7 years.
A three category variable was then constructed by counting the reports of adversities (0 adversities/1 adversity/2or + adversities).
Respondents were excluded if they had missing data for all six categories. Respondents were considered as having no adversities if they answered ‘no’ all the categories or if they answered ‘no’ to one or more category and the other categories were missing.
Covariates
Potential confounders for the associations between the two main exposures studied (mother’s pre-pregnancy BMI and ACE) and MetS were selected a priori based on literature including recent work we performed on MetS during adulthood on the same cohort [38]. Selected variables concerned early life socioeconomic conditions: household and parental characteristics [mother’s education level (left school at 15 y or later/before 14 y), mother’s partner’s (or father’s if unavailable) social class (non-manual/manual), overcrowded household (people per room >1.5 or ≤1.5)]. To capture elements in the early environment potentially related to stressful socioeconomic or psychosocial conditions and subsequent MetS, we selected proxy variables on birth and perinatal conditions [38]: maternal smoking during pregnancy (no smoking, sometimes, moderately, heavily), type of delivery (vaginal, emergency caesarean, elective caesarean), Mother’s parity in 1958, maternal age at birth (divided according quartiles), birthweight (divided according quartiles) and gestational age (<38, 38, 39–41 and >41 weeks) collected at birth; breastfed collected at 7 years (no, yes for less than 1 month, yes more than 1 month) .
Potential adult mediating factors were also selected to explore three main pathways:
-
i)
a socioeconomic/materialist one, including respondent’s educational attainment at 23 years (A level/O level/no qualification), respondent’s occupational social class at 33 years (non-manual/manual active), wealth based on information about home ownership and the price of the house adjusted for economic inflation of the year of purchase and then divided in quartiles (not owner/Q1—owner lowest price/owner-Q2/owner-Q3/owner-Q4);
-
ii)
a health behaviors pathway including physical activity [physically active/moderately active/inactive], alcohol consumption [abstainers (reported not consuming any alcohol in the previous week)/moderate (women: between 1 and 14 units in the previous week; men: between 1 and 21 units in the previous week) /heavy drinkers (women: >14 units in the previous week; men: >21 units in the previous week)], smoking status [nonsmoker/former smoker/smoker (<10 cigarettes/smoker; 10–19 cigarettes/smoker; >20 cigarettes)] and BMI (normal/underweight/overweight/obese) at 23 years. Adult life style variables are available at other points along the lifecourse, however in our model, these adult variables at the age 23 are considered as a proxy of behavioural patterns in early adulthood and controlling for them serve as a first step to understanding possible mechanism.
-
iii)
a psychological one including the Rutter’s malaise inventory that measures psychological distress at 23 years [39, 40]. It comprises 24 binary items on both emotional and somatic symptoms, the individual being considered as having a psychological malaise if s/he reported experiencing more than 7 out of 24 symptoms (no malaise/malaise); and marital status at 33 y (couple/single/divorced or widowed).
Statistical analyses
Sample characteristics were first described. Bivariate crosstabulations were done between our two main exposures, mother’s pre-pregnancy BMI and ACE, and the subsequent risk of MetS. Then data were analyzed in multivariate models. A series of logistic regression models were performed taking a lifecourse perspective: Model 1 included mother’s pre-pregnancy BMI and all variables measured at or around birth; in Model 2 we added ACE measured between 7 and 16 years old; in Model 3 we then added potential mediators measured at 23 years except for participants’ BMI at 23 years; in Model 4 we included all variables measured at 23 years including participant’s BMI; finally, in Model 5 we added variables measured at 33 years corresponding to the full model.
We determined the respective statistical contributions of confounders and mediators in explaining the association between pre pregnancy maternal BMI or ACE and MetS by using a traditional approach to mediation analyses [41]. We calculated the percentage attenuation in the β coefficient for maternal pre-pregnancy BMI and adversity after inclusion of confounders and mediators in models using the following formula:
This approach has been used elsewhere to explore the influence of social determinants on health inequalities [12, 42, 43]. A 95 % CI was then calculated around the percentage attenuation using a bootstrap method with 1000 re-samplings. When the 95 %CI did not include 0, the attenuation was considered as significant.
All the analyses were performed separately for men and women given that sex/gender differences regarding biological pathways towards MetS having been shown, notably in the same study [44].
To control for possible bias due to missing data, multivariate analyses were performed using imputed data for covariates with missing data using the multiple imputation program ICE in STATA V.11. Ten imputations were conducted taking the missing-at-random (MAR) assumption. Each covariate with missing values was imputed including in the imputation model all confounders and mediators of the multivariate model as well as variables from other sweeps correlated with the variable to impute. These variables from other sweeps were selected a priori because they could improve the imputation model estimations and we keep only those that achieved the 5 % significance cutoff. For example, we imputed self-reported alcohol consumption at 23 y using information on the individual drinking at 33 and 42 years. Neither the exposure variables of interest (maternal BMI before pregnancy and ACE) not the MetS variable were included in the multiple imputation.
Sensitivity analyses were performed by replicating analyses on complete cases.
Results
The sample characteristics are presented in Table 1. Among men, 19.1 and 4.2 % of their mothers were overweight or obese before pregnancy respectively. These proportions were similar in women (19.6 % and 3.8 % for overweight and obese mother respectively). Regarding ACE, 20.4 % of men and 19.8 % of women had been exposed to one adversity during their childhood, 6.5 % of men and 6.4 % of women being exposed to at least two adversities.
Table 1.
Characteristics of the studied sample
| Men (N = 3395) | Women (N = 3347) | |||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| Metabolic syndrome | ||||
| No | 2121 | 62.5 | 2685 | 80.2 |
| Yes | 1274 | 37.5 | 662 | 19.8 |
| Metabolic syndrome components | ||||
| High systolic blood pressure | 1861 | 54.8 | 828 | 24.7 |
| High diastolic blood pressure | 1261 | 37.1 | 593 | 17.7 |
| Low HDL cholesterol | 286 | 8.4 | 429 | 12.8 |
| High triglycerides | 2115 | 62.3 | 1097 | 32.8 |
| High waist circumference | 1090 | 32.1 | 1188 | 35.5 |
| High HbA1c | 101 | 3.0 | 61 | 1.8 |
| Mother’s BMI | ||||
| Normal | 2 474 | 72.9 | 2 396 | 71.6 |
| Underweight | 129 | 3.8 | 167 | 5.0 |
| Overweight | 648 | 19.1 | 656 | 19.6 |
| Obese | 144 | 4.2 | 128 | 3.8 |
| Adverse childhood experiences | ||||
| None | 2 482 | 73.1 | 2 471 | 73.8 |
| One | 693 | 20.4 | 662 | 19.8 |
| Two or more | 220 | 6.5 | 214 | 6.4 |
| Mother’s education level | ||||
| Left school at 15 or later | 921 | 27.1 | 903 | 27.0 |
| Left school before 14 | 2 453 | 72.3 | 2 431 | 72.6 |
| Missing | 21 | 0.6 | 13 | 0.4 |
| Father’s social class at birth | ||||
| Non-manual | 988 | 29.1 | 922 | 27.5 |
| Manual | 2 271 | 66.9 | 2 274 | 67.9 |
| Missing | 136 | 4.0 | 151 | 4.5 |
| Overcrowding | ||||
| > 1.5 person/room | 360 | 10.6 | 408 | 12.2 |
| < =1.5 person/room | 2 949 | 86.9 | 2 870 | 85.7 |
| Missing | 86 | 2.5 | 69 | 2.1 |
| Birthweight | ||||
| Q1 - Low weight | 711 | 20.9 | 727 | 21.7 |
| Q2 | 935 | 27.5 | 871 | 26.0 |
| Q3 | 871 | 25.7 | 829 | 24.8 |
| Q4 - High weight | 763 | 22.5 | 828 | 24.7 |
| Missing | 115 | 3.4 | 92 | 2.7 |
| Mother smoked during pregnancy | ||||
| No | 2 301 | 67.8 | 2 225 | 66.5 |
| Sometimes | 212 | 6.2 | 196 | 5.9 |
| Moderately | 479 | 14.1 | 507 | 15.1 |
| Heavily | 367 | 10.8 | 385 | 11.5 |
| Missing | 36 | 1.1 | 34 | 1.0 |
| Mother’s age at birth | ||||
| 23 years or less | 866 | 25.5 | 889 | 26.6 |
| 24 to 27 years | 974 | 28.7 | 924 | 27.6 |
| 28 to 31 years | 770 | 22.7 | 732 | 21.9 |
| 32 years or more | 784 | 23.1 | 799 | 23.9 |
| Missing | 1 | 0.0 | 3 | 0.1 |
| Breastfed | ||||
| No | 956 | 28.2 | 922 | 27.5 |
| Yes, for less than 1 month | 757 | 22.3 | 756 | 22.6 |
| Yes, more than 1 month | 1 477 | 43.5 | 1 482 | 44.3 |
| Missing | 205 | 6.0 | 187 | 5.6 |
| Parity | ||||
| Oldest child | 1 221 | 36.0 | 1 255 | 37.5 |
| 2nd child | 1 151 | 33.9 | 1 016 | 30.4 |
| 3rd child or more | 1 023 | 30.1 | 1 076 | 32.1 |
| 38 weeks or less | 275 | 8.1 | 261 | 7.8 |
| Gestational age | ||||
| 38 weeks or less | 275 | 8.1 | 261 | 7.8 |
| 39 to 41 weeks | 1 970 | 58.0 | 1 893 | 56.6 |
| 42 weeks or more | 855 | 25.2 | 875 | 26.1 |
| Missing | 295 | 8.7 | 318 | 9.5 |
| Type of delivery | ||||
| Vaginal | 3 302 | 97.3 | 3 271 | 97.7 |
| Emergency caesarean | 51 | 1.5 | 44 | 1.3 |
| Elective caesarean | 42 | 1.2 | 32 | 1.0 |
| Smoking status at 23 | ||||
| Non-smoker | 858 | 25.3 | 991 | 29.6 |
| Former smoker | 928 | 27.3 | 840 | 25.1 |
| Smoker - Less than 10 cig. | 201 | 5.9 | 293 | 8.8 |
| Smoker - 10 to 19 cig. | 398 | 11.7 | 430 | 12.8 |
| Smoker - More than 20 cig. | 529 | 15.6 | 408 | 12.2 |
| Missing | 481 | 14.2 | 385 | 11.5 |
| Alcohol consumption at 23 | ||||
| Moderate | 1 412 | 41.6 | 1 567 | 46.8 |
| Abstainers | 346 | 10.2 | 1 031 | 30.8 |
| Heavy drinkers | 1 155 | 34.0 | 363 | 10.8 |
| Missing | 482 | 14.2 | 386 | 11.5 |
| Physical activity at 23 | ||||
| Physically active | 1 254 | 36.9 | 730 | 21.8 |
| Moderately active | 542 | 16.0 | 420 | 12.5 |
| Inactive | 1 114 | 32.8 | 1 812 | 54.1 |
| Missing | 485 | 14.3 | 385 | 11.5 |
| Malaise inventory at 23 | ||||
| No | 2 815 | 82.9 | 2 677 | 80.0 |
| Yes | 94 | 2.8 | 282 | 8.4 |
| Missing | 486 | 14.3 | 388 | 11.6 |
| Education level at 23 | ||||
| Passed A levels | 731 | 21.5 | 682 | 20.4 |
| Passed O levels | 1 119 | 33.0 | 1 342 | 40.1 |
| No qualifications | 1 062 | 31.3 | 936 | 28.0 |
| Missing | 483 | 14.2 | 387 | 11.6 |
| BMI at 23 | ||||
| Normal | 2 299 | 67.7 | 2 377 | 71.0 |
| Underweight | 68 | 2.0 | 183 | 5.5 |
| Overweight | 447 | 13.2 | 300 | 9.0 |
| Obese | 52 | 1.5 | 73 | 2.2 |
| Missing | 529 | 15.6 | 414 | 12.4 |
| Occupational social class at 33 | ||||
| Non-manual | 1 518 | 44.7 | 1 981 | 59.2 |
| Manual | 1 314 | 38.7 | 850 | 25.4 |
| Missing | 563 | 16.6 | 516 | 15.4 |
| Wealth at 33 | ||||
| Not owner | 672 | 19.8 | 672 | 20.1 |
| Owner - Q1 (Low price) | 561 | 16.5 | 570 | 17.0 |
| Owner - Q2 | 569 | 16.8 | 591 | 17.7 |
| Owner - Q3 | 594 | 17.5 | 566 | 16.9 |
| Owner - Q4 | 544 | 16.0 | 588 | 17.6 |
| Missing | 455 | 13.4 | 360 | 10.8 |
| Marital status at 33 | ||||
| Couple | 2 396 | 70.6 | 2 496 | 74.6 |
| Single | 417 | 12.3 | 276 | 8.2 |
| Divorced or widowed | 144 | 4.2 | 254 | 7.6 |
| Missing | 438 | 12.9 | 321 | 9.6 |
MetS was frequent, in particular in men among whom 37.5 % had MetS versus 19.8 % of women. This difference was mainly due to a higher proportion of high blood pressure in men as a higher proportion of triglycerides > =150 mg/dL, the proportion of high level for the other components of MetS being close in men and women (Table 1). MetS proportions increased in men and women gradually as mother’s pre pregnancy BMI increased (Table 2). In men, compared to the proportion (35.7 %) of MetS when their mothers had a normal BMI before pregnancy, 42.3 % had MetS when their mothers were overweight before pregnancy (crude OR = 1.32, 95 % CI: 1.11–1.57) and 47.2 % when their mothers were obese before pregnancy (crude OR = 1.61, 95 % CI: 1.15–2.26). In women, compared to the proportion (17.9 %) of MetS when their mothers had a normal BMI before pregnancy, 25.0 % had MetS when their mothers were overweight before pregnancy (crude OR = 1.53, 95 % CI: 1.25–1.88) and 29.7 % had MetS when their mothers were obese before pregnancy (crude OR = 1.94, 95 % CI: 1.31–2.88).
Table 2.
Proportion and odds of having the metabolic syndrome according to mother’s pre-pregnancy BMI and childhood adversity
| Metabolic syndrome | ||||
|---|---|---|---|---|
| Men (N = 3395) | ||||
| N (%) | p value | OR (95 %CI) | p value | |
| Mother’s pre-pregnancy BMI | ||||
| Normal | 883 (35.7) | 0.001 | 1 | |
| Underweight | 49 (38) | 1.10 (0.77–1.59) | 0.596 | |
| Overweight | 274 (42.3) | 1.32 (1.11–1.57) | 0.002 | |
| Obese | 68 (47.2) | 1.61 (1.15–2.26) | 0.006 | |
| Adverse childhood experiences | ||||
| None | 922 (37.1) | 0.06 | 1 | |
| One | 253 (36.5) | 0.97 (0.82–1.16) | 0.76 | |
| Two or more | 99 (45.0) | 1.38 (1.05–1.83) | 0.02 | |
| Women (N = 3347) | ||||
| N (%) | p value | OR (95 %CI) | p value | |
| Mother’s pre-pregnancy BMI | ||||
| Normal | 428 (17.9) | <0.001 | 1 | |
| Underweight | 32 (19.2) | 1.09 (1.73–1.62) | 0.673 | |
| Overweight | 164 (25.0) | 1.53 (1.25–1.88) | <0.001 | |
| Obese | 38 (29.7) | 1.94 (1.31–2.88) | <0.001 | |
| Adverse childhood experiences | ||||
| None | 463 (18.7) | 0.04 | 1 | |
| One | 151 (22.8) | 1.28 (1.04–1.58) | 0.02 | |
| Two or more | 48 (22.4) | 1.25 (0.90–1.76) | 0.19 | |
MetS was also associated with ACE but not on a gradient. In men, 45 % of those exposed to at least two adversities during childhood had MetS compared to 37.1 % in non-exposed men (crude OR = 1.38, 95 % CI: 1.05–1.83). In women, 22.8 % of those exposed to one adversity during childhood had MetS compared to 18.7 % in non-exposed women (crude OR = 1.28, 95 % CI: 1.04–1.58).
Results of multivariate analyses are presented in Tables 3, 4 and in Fig. 2. In men (Table 3, Fig. 2a) the link between mother’s pre-pregnancy BMI and MetS persisted after adjustment for perinatal confounders (model 1), as after inclusion of ACE (model 2). The inclusion in the model of potential mediators at 23 years did not change the strength of this association (model 3) except when participants’ BMI at 23 years was added (model 4). Compared with model 1, after adding participant’s BMI at 23 years, the association between mother’s pre-pregnancy BMI and MetS was attenuated by 54.7 % (95 % CI: 25.4–170.7 %) for obese (OR = 1.24, 95 % CI: 0.86–1.77) and by 21.4 % (95 % CI: 0.3–78.8 %) for overweight mother’s before pregnancy (OR = 1.24, 95 % CI: 1.03–1.50) respectively. Including variables at 33 years (model 5) did not change the association further.
Table 3.
Odds of having metabolic syndrome. Lifecourse multivariate logistic regression models using data from multiple imputations. Men (N = 3395)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | |
| Mother’s BMI | |||||||||||||||
| Normal | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Underweight | 1.06 | (0.73–1.53) | 0.760 | 1.06 | (0.73–1.53) | 0.771 | 1.05 | (0.72–1.52) | 0.798 | 1.11 | (0.76–1.62) | 0.599 | 1.13 | (0.77–1.65) | 0.533 |
| Overweight | 1.31 | (1.09–1.57) | 0.003 | 1.30 | (1.08–1.56) | 0.004 | 1.29 | (1.07–1.54) | 0.007 | 1.24 | (1.03–1.50) | 0.024 | 1.24 | (1.03–1.49) | 0.025 |
| Obese | 1.52 | (1.07–2.15) | 0.018 | 1.50 | (1.06–2.13) | 0.022 | 1.49 | (1.05–2.11) | 0.026 | 1.24 | (0.86–1.77) | 0.244 | 1.22 | (0.85–1.75) | 0.282 |
| Mother’s education level | |||||||||||||||
| Left school at 15 or later | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Left school before 14 | 1.38 | (1.16–1.65) | <0.001 | 1.38 | (1.16–1.65) | <0.001 | 1.36 | (1.13–1.63) | 0.001 | 1.34 | (1.11–1.61) | 0.002 | 1.34 | (1.11–1.61) | 0.002 |
| Father’s social class at birth | |||||||||||||||
| Non-manual | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Manual | 1.25 | (1.05–1.49) | 0.013 | 1.25 | (1.05–1.49) | 0.013 | 1.23 | (1.02–1.47) | 0.029 | 1.17 | (0.98–1.41) | 0.087 | 1.18 | (0.98–1.42) | 0.082 |
| Overcrowding | |||||||||||||||
| > 1.5 personne/chambre | 1 | 1 | 1 | 1 | 1 | ||||||||||
| < =1.5 personne/chambre | 0.97 | (0.77–1.22) | 0.775 | 0.97 | (0.77–1.22) | 0.789 | 0.98 | (0.77–1.24) | 0.842 | 0.97 | (0.76–1.24) | 0.805 | 0.98 | (0.77–1.25) | 0.882 |
| Birthweight | |||||||||||||||
| Q1 - Low weight | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Q2 | 0.87 | (0.70–1.07) | 0.187 | 0.87 | (0.71–1.08) | 0.204 | 0.88 | (0.71–1.09) | 0.229 | 0.87 | (0.70–1.08) | 0.207 | 0.88 | (0.71–1.09) | 0.239 |
| Q3 | 1.02 | (0.82–1.27) | 0.832 | 1.03 | (0.83–1.28) | 0.800 | 1.04 | (0.83–1.29) | 0.741 | 1.01 | (0.80–1.26) | 0.961 | 1.01 | (0.81–1.27) | 0.900 |
| Q4 - High weight | 0.90 | (0.72–1.14) | 0.390 | 0.91 | (0.73–1.15) | 0.430 | 0.92 | (0.73–1.16) | 0.471 | 0.84 | (0.66–1.07) | 0.151 | 0.84 | (0.66–1.07) | 0.161 |
| Mother smoked during pregnancy | |||||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Sometimes | 1.16 | (0.87–1.56) | 0.308 | 1.16 | (0.86–1.55) | 0.328 | 1.14 | (0.85–1.53) | 0.389 | 1.07 | (0.79–1.45) | 0.644 | 1.07 | (0.79–1.45) | 0.645 |
| Moderately | 1.12 | (0.91–1.38) | 0.268 | 1.12 | (0.91–1.38) | 0.272 | 1.12 | (0.91–1.38) | 0.286 | 1.06 | (0.86–1.31) | 0.594 | 1.06 | (0.86–1.31) | 0.576 |
| Heavily | 0.98 | (0.78–1.24) | 0.878 | 0.97 | (0.77–1.23) | 0.824 | 0.95 | (0.75–1.20) | 0.639 | 0.90 | (0.70–1.14) | 0.371 | 0.89 | (0.70–1.14) | 0.361 |
| Mother’s age at birth | |||||||||||||||
| 23 years or less | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 24 to 27 years | 1.09 | (0.90–1.33) | 0.377 | 1.09 | (0.90–1.33) | 0.381 | 1.10 | (0.90–1.35) | 0.335 | 1.11 | (0.91–1.36) | 0.300 | 1.12 | (0.91–1.37) | 0.274 |
| 28 to 31 years | 1.01 | (0.82–1.26) | 0.894 | 1.02 | (0.82–1.27) | 0.879 | 1.04 | (0.83–1.30) | 0.719 | 1.05 | (0.83–1.31) | 0.697 | 1.04 | (0.83–1.31) | 0.712 |
| 32 years or more | 0.83 | (0.66–1.05) | 0.119 | 0.84 | (0.66–1.06) | 0.134 | 0.86 | (0.68–1.09) | 0.209 | 0.85 | (0.66–1.08) | 0.179 | 0.85 | (0.66–1.08) | 0.182 |
| Breastfed | |||||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Yes, for less than 1 month | 1.02 | (0.83–1.24) | 0.877 | 1.01 | (0.83–1.24) | 0.887 | 1.01 | (0.83–1.24) | 0.913 | 1.02 | (0.83–1.26) | 0.852 | 1.02 | (0.83–1.26) | 0.863 |
| Yes, more than 1 month | 1.00 | (0.84–1.19) | 0.993 | 1.00 | (0.84–1.19) | 0.995 | 1.01 | (0.84–1.20) | 0.934 | 1.03 | (0.86–1.22) | 0.781 | 1.03 | (0.86–1.23) | 0.780 |
| Parity | |||||||||||||||
| Oldest child | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 2nd child | 0.88 | (0.74–1.05) | 0.168 | 0.88 | (0.74–1.05) | 0.159 | 0.87 | (0.73–1.04) | 0.132 | 0.88 | (0.73–1.05) | 0.165 | 0.87 | (0.73–1.05) | 0.148 |
| 3rd child or more | 1.00 | (0.82–1.23) | 0.965 | 1.00 | (0.81–1.22) | 0.973 | 0.97 | (0.78–1.19) | 0.747 | 0.99 | (0.80–1.23) | 0.946 | 0.99 | (0.80–1.23) | 0.924 |
| Gestational age | |||||||||||||||
| 38 weeks or less | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 39 to 41 weeks | 1.19 | (0.89–1.60) | 0.248 | 1.19 | (0.88–1.60) | 0.253 | 1.21 | (0.90–1.62) | 0.215 | 1.17 | (0.87–1.57) | 0.295 | 1.18 | (0.87–1.60) | 0.284 |
| 42 weeks or more | 1.18 | (0.85–1.62) | 0.323 | 1.17 | (0.85–1.61) | 0.331 | 1.18 | (0.86–1.63) | 0.299 | 1.17 | (0.86–1.61) | 0.318 | 1.19 | (0.86–1.63) | 0.297 |
| Type of delivery | |||||||||||||||
| Vaginal | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Emergency caesarean | 1.86 | (1.06–3.29) | 0.032 | 1.83 | (1.03–3.23) | 0.038 | 1.83 | (1.03–3.25) | 0.038 | 1.98 | (1.11–3.56) | 0.022 | 2.02 | (1.13–3.63) | 0.018 |
| Elective caesarean | 0.73 | (0.37–1.44) | 0.359 | 0.73 | (0.37–1.44) | 0.361 | 0.77 | (0.39–1.54) | 0.465 | 0.75 | (0.37–1.50) | 0.412 | 0.75 | (0.37–1.51) | 0.423 |
| Adverse childhood experiences | |||||||||||||||
| None | 1 | 1 | 1 | 1 | |||||||||||
| One | 0.93 | (0.78–1.12) | 0.452 | 0.91 | (0.76–1.09) | 0.296 | 0.91 | (0.76–1.10) | 0.331 | 0.91 | (0.76–1.10) | 0.341 | |||
| Two or more | 1.19 | (0.89–1.59) | 0.243 | 1.12 | (0.83–1.50) | 0.469 | 1.18 | (0.87–1.59) | 0.294 | 1.16 | (0.86–1.57) | 0.340 | |||
| Smoking status at 23 | |||||||||||||||
| Non-smoker | 1 | 1 | 1 | ||||||||||||
| Former smoker | 0.95 | (0.78–1.15) | 0.575 | 0.94 | (0.77–1.15) | 0.541 | 0.94 | (0.77–1.14) | 0.521 | ||||||
| Smoker - Less than 10 cig. | 1.13 | (0.82–1.56) | 0.438 | 1.15 | (0.82–1.60) | 0.414 | 1.15 | (0.82–1.60) | 0.424 | ||||||
| Smoker - 10 to 19 cig. | 0.95 | (0.74–1.22) | 0.685 | 0.98 | (0.76–1.27) | 0.883 | 0.97 | (0.76–1.26) | 0.839 | ||||||
| Smoker - More than 20 cig. | 1.11 | (0.88–1.40) | 0.378 | 1.13 | (0.90–1.44) | 0.295 | 1.13 | (0.89–1.44) | 0.304 | ||||||
| Alcohol consumption at 23 | |||||||||||||||
| Moderate | 1 | 1 | 1 | ||||||||||||
| Abstainers | 1.00 | (0.76–1.31) | 0.991 | 1.02 | (0.77–1.35) | 0.893 | 0.99 | (0.75–1.31) | 0.937 | ||||||
| Heavy drinkers | 1.08 | (0.91–1.27) | 0.368 | 1.06 | (0.90–1.26) | 0.497 | 1.06 | (0.89–1.25) | 0.521 | ||||||
| Physical activity at 23 | |||||||||||||||
| Physically active | 1 | 1 | 1 | ||||||||||||
| Moderately active | 1.13 | (0.91–1.40) | 0.259 | 1.13 | (0.91–1.40) | 0.283 | 1.12 | (0.90–1.40) | 0.297 | ||||||
| Inactive | 1.25 | (1.04–1.52) | 0.020 | 1.25 | (1.03–1.53) | 0.026 | 1.25 | (1.02–1.52) | 0.029 | ||||||
| Malaise inventory at 23 | |||||||||||||||
| No | 1 | 1 | 1 | ||||||||||||
| Yes | 1.30 | (0.87–1.94) | 0.200 | 1.28 | (0.85–1.94) | 0.237 | 1.30 | (0.86–1.97) | 0.218 | ||||||
| Education level at 23 | |||||||||||||||
| Passed A levels | 1 | 1 | 1 | ||||||||||||
| Passed O levels | 1.04 | (0.84–1.31) | 0.705 | 0.98 | (0.79–1.23) | 0.893 | 1.00 | (0.78–1.28) | 0.991 | ||||||
| No qualifications | 1.12 | (0.88–1.43) | 0.356 | 0.99 | (0.77–1.26) | 0.913 | 1.00 | (0.75–1.34) | 0.986 | ||||||
| BMI at 23 | |||||||||||||||
| Normal | 1 | 1 | |||||||||||||
| Underweight | 0.52 | (0.28–0.96) | 0.036 | 0.50 | (0.27–0.93) | 0.028 | |||||||||
| Overweight | 2.27 | (1.83–2.82) | <0.001 | 2.27 | (1.83–2.82) | <0.001 | |||||||||
| Obese | 3.52 | (1.92–6.46) | <0.001 | 3.43 | (1.87–6.31) | <0.001 | |||||||||
| Occupational social class at 33 | |||||||||||||||
| Non-manual | 1 | ||||||||||||||
| Manual | 0.94 | (0.77–1.14) | 0.516 | ||||||||||||
| Wealth at 33 | |||||||||||||||
| Not owner | 1 | ||||||||||||||
| Owner - Q1 (Low price) | 0.79 | (0.62–1.01) | 0.062 | ||||||||||||
| Owner - Q2 | 0.83 | (0.65–1.06) | 0.131 | ||||||||||||
| Owner - Q3 | 0.83 | (0.64–1.07) | 0.145 | ||||||||||||
| Owner - Q4 | 0.78 | (0.60–1.02) | 0.066 | ||||||||||||
| Marital status at 33 | |||||||||||||||
| Couple | 1 | ||||||||||||||
| Single | 0.96 | (0.76–1.20) | 0.709 | ||||||||||||
| Divorced or widowed | 0.69 | (0.47–1.00) | 0.050 | ||||||||||||
Model 1 included mother’s pre-pregnancy BMI and all variables measured at or around birth; Model 2: Model 1 + ACE; Model 3: Model 2 + potential mediators measured at 23 years except for participants’ BMI at 23 years; Model 4: Model 3 + participant’s BMI at 23 years; Model 5: Full model
Table 4.
Odds of having metabolic syndrome. Lifecourse multivariate logistic regression models using data from multiple imputations. Women (N = 3347)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | OR | CI 95 % | p | |
| Mother’s BMI | |||||||||||||||
| Normal | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Underweight | 0.99 | (0.66–1.48) | 0.946 | 0.97 | (0.64–1.46) | 0.879 | 0.98 | (0.65–1.48) | 0.933 | 1.06 | (0.69–1.62) | 0.804 | 1.05 | (0.68–1.60) | 0.838 |
| Overweight | 1.54 | (1.25–1.90) | <0.001 | 1.55 | (1.25–1.91) | <0.001 | 1.51 | (1.22–1.87) | <0.001 | 1.38 | (1.10–1.72) | 0.005 | 1.37 | (1.10–1.71) | 0.005 |
| Obese | 2.05 | (1.36–3.08) | <0.001 | 2.05 | (1.36–3.09) | <0.001 | 2.06 | (1.36–3.11) | <0.001 | 1.43 | (0.92–2.22) | 0.116 | 1.39 | (0.89–2.18) | 0.145 |
| Mother’s education level | |||||||||||||||
| Left school at 15 or later | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Left school before 14 | 1.38 | (1.10–1.73) | 0.006 | 1.37 | (1.09–1.72) | 0.007 | 1.29 | (1.02–1.63) | 0.037 | 1.32 | (1.04–1.69) | 0.024 | 1.31 | (1.03–1.68) | 0.029 |
| Father’s social class at birth | |||||||||||||||
| Non-manual | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Manual | 1.53 | (1.22–1.94) | <0.001 | 1.52 | (1.20–1.92) | <0.001 | 1.43 | (1.13–1.82) | 0.003 | 1.36 | (1.06–1.75) | 0.015 | 1.33 | (1.04–1.71) | 0.026 |
| Overcrowding | |||||||||||||||
| > 1.5 personne/chambre | 1 | 1 | 1 | 1 | 1 | ||||||||||
| < =1.5 personne/chambre | 1.07 | (0.82–1.40) | 0.593 | 1.08 | (0.83–1.40) | 0.586 | 1.09 | (0.84–1.43) | 0.508 | 1.11 | (0.84–1.47) | 0.469 | 1.12 | (0.84–1.48) | 0.444 |
| Birthweight | |||||||||||||||
| Q1 - Low weight | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Q2 | 0.78 | (0.60–1.00) | 0.049 | 0.77 | (0.60–1.00) | 0.048 | 0.79 | (0.62–1.03) | 0.078 | 0.80 | (0.61–1.04) | 0.090 | 0.79 | (0.61–1.03) | 0.088 |
| Q3 | 0.77 | (0.59–1.00) | 0.049 | 0.77 | (0.59–1.00) | 0.050 | 0.80 | (0.61–1.04) | 0.095 | 0.78 | (0.59–1.02) | 0.072 | 0.78 | (0.59–1.03) | 0.082 |
| Q4 - High weight | 0.81 | (0.61–1.06) | 0.122 | 0.81 | (0.61–1.06) | 0.122 | 0.84 | (0.64–1.11) | 0.220 | 0.79 | (0.60–1.05) | 0.111 | 0.79 | (0.60–1.05) | 0.110 |
| Mother smoked during pregnancy | |||||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Sometimes | 1.60 | (1.14–2.24) | 0.007 | 1.59 | (1.13–2.23) | 0.008 | 1.51 | (1.07–2.14) | 0.019 | 1.45 | (1.01–2.08) | 0.043 | 1.41 | (0.98–2.02) | 0.061 |
| Moderately | 1.24 | (0.97–1.59) | 0.081 | 1.24 | (0.97–1.59) | 0.082 | 1.23 | (0.96–1.58) | 0.104 | 1.16 | (0.89–1.51) | 0.260 | 1.15 | (0.88–1.49) | 0.306 |
| Heavily | 1.43 | (1.09–1.86) | 0.009 | 1.42 | (1.09–1.86) | 0.010 | 1.35 | (1.03–1.77) | 0.030 | 1.22 | (0.92–1.63) | 0.174 | 1.23 | (0.92–1.63) | 0.162 |
| Mother’s age at birth | |||||||||||||||
| 23 years or less | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 24 to 27 years | 0.64 | (0.50–0.81) | <0.001 | 0.64 | (0.50–0.82) | <0.001 | 0.67 | (0.52–0.85) | 0.001 | 0.69 | (0.54–0.90) | 0.005 | 0.69 | (0.54–0.90) | 0.005 |
| 28 to 31 years | 0.72 | (0.55–0.94) | 0.016 | 0.73 | (0.56–0.95) | 0.021 | 0.77 | (0.58–1.01) | 0.058 | 0.82 | (0.62–1.08) | 0.163 | 0.83 | (0.62–1.10) | 0.190 |
| 32 years or more | 0.73 | (0.55–0.96) | 0.023 | 0.73 | (0.55–0.96) | 0.027 | 0.79 | (0.59–1.05) | 0.103 | 0.82 | (0.61–1.11) | 0.195 | 0.83 | (0.62–1.12) | 0.220 |
| Breastfed | |||||||||||||||
| No | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Yes, for less than 1 month | 1.00 | (0.78–1.27) | 0.983 | 1.01 | (0.79–1.28) | 0.966 | 1.02 | (0.80–1.30) | 0.895 | 1.01 | (0.78–1.30) | 0.965 | 1.01 | (0.78–1.30) | 0.969 |
| Yes, more than 1 month | 1.10 | (0.89–1.36) | 0.386 | 1.11 | (0.90–1.38) | 0.330 | 1.15 | (0.92–1.42) | 0.212 | 1.15 | (0.92–1.43) | 0.231 | 1.16 | (0.93–1.45) | 0.194 |
| Parity | |||||||||||||||
| Oldest child | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 2nd child | 0.88 | (0.71–1.10) | 0.260 | 0.88 | (0.70–1.09) | 0.239 | 0.86 | (0.68–1.07) | 0.180 | 0.89 | (0.70–1.12) | 0.309 | 0.88 | (0.70–1.12) | 0.300 |
| 3rd child or more | 0.87 | (0.68–1.11) | 0.273 | 0.86 | (0.67–1.10) | 0.227 | 0.80 | (0.62–1.04) | 0.097 | 0.83 | (0.63–1.08) | 0.158 | 0.81 | (0.62–1.06) | 0.133 |
| Gestational age | |||||||||||||||
| 38 weeks or less | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 39 to 41 weeks | 0.83 | (0.59–1.15) | 0.266 | 0.84 | (0.60–1.17) | 0.294 | 0.83 | (0.59–1.16) | 0.277 | 0.88 | (0.62–1.23) | 0.449 | 0.87 | (0.62–1.23) | 0.435 |
| 42 weeks or more | 0.89 | (0.62–1.26) | 0.505 | 0.89 | (0.63–1.27) | 0.527 | 0.88 | (0.61–1.26) | 0.482 | 0.91 | (0.63–1.32) | 0.629 | 0.91 | (0.63–1.31) | 0.616 |
| Type of delivery | |||||||||||||||
| Vaginal | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Emergency caesarean | 1.79 | (0.91–3.52) | 0.092 | 1.81 | (0.92–3.56) | 0.087 | 1.85 | (0.93–3.65) | 0.078 | 1.74 | (0.85–3.56) | 0.128 | 1.79 | (0.87–3.66) | 0.112 |
| Elective caesarean | 0.92 | (0.37–2.31) | 0.865 | 0.93 | (0.37–2.32) | 0.875 | 0.97 | (0.39–2.44) | 0.956 | 0.93 | (0.36–2.37) | 0.875 | 0.94 | (0.37–2.40) | 0.894 |
| Adverse childhood experiences | |||||||||||||||
| None | 1 | 1 | 1 | 1 | |||||||||||
| One | 1.19 | (0.96–1.48) | 0.106 | 1.15 | (0.93–1.43) | 0.194 | 1.15 | (0.92–1.44) | 0.222 | 1.12 | (0.90–1.41) | 0.314 | |||
| Two or more | 1.07 | (0.76–1.52) | 0.695 | 1.01 | (0.71–1.45) | 0.942 | 0.96 | (0.66–1.39) | 0.836 | 0.94 | (0.65–1.36) | 0.735 | |||
| Smoking status at 23 | |||||||||||||||
| Non-smoker | 1 | 1 | 1 | ||||||||||||
| Former smoker | 0.81 | (0.64–1.04) | 0.097 | 0.83 | (0.64–1.07) | 0.155 | 0.83 | (0.64–1.08) | 0.173 | ||||||
| Smoker - Less than 10 cig. | 0.92 | (0.65–1.30) | 0.628 | 0.95 | (0.67–1.36) | 0.797 | 0.95 | (0.66–1.35) | 0.763 | ||||||
| Smoker - 10 to 19 cig. | 0.88 | (0.65–1.19) | 0.409 | 0.97 | (0.71–1.33) | 0.860 | 0.94 | (0.69–1.28) | 0.694 | ||||||
| Smoker - More than 20 cig. | 1.08 | (0.81–1.44) | 0.602 | 1.14 | (0.85–1.53) | 0.393 | 1.09 | (0.81–1.47) | 0.555 | ||||||
| Alcohol consumption at 23 | |||||||||||||||
| Moderate | 1 | 1 | 1 | ||||||||||||
| Abstainers | 0.98 | (0.79–1.21) | 0.846 | 0.91 | (0.73–1.13) | 0.384 | 0.87 | (0.70–1.09) | 0.230 | ||||||
| Heavy drinkers | 0.80 | (0.58–1.10) | 0.174 | 0.75 | (0.54–1.04) | 0.089 | 0.75 | (0.54–1.05) | 0.093 | ||||||
| Physical activity at 23 | |||||||||||||||
| Physically active | 1 | 1 | 1 | ||||||||||||
| Moderately active | 0.84 | (0.60–1.18) | 0.309 | 0.83 | (0.58–1.17) | 0.281 | 0.83 | (0.59–1.18) | 0.306 | ||||||
| Inactive | 1.18 | (0.93–1.50) | 0.167 | 1.12 | (0.88–1.44) | 0.354 | 1.10 | (0.85–1.41) | 0.472 | ||||||
| Malaise inventory at 23 | |||||||||||||||
| No | 1 | 1 | 1 | ||||||||||||
| Yes | 1.25 | (0.91–1.72) | 0.161 | 1.19 | (0.86–1.66) | 0.300 | 1.17 | (0.84–1.64) | 0.346 | ||||||
| Education level at 23 | |||||||||||||||
| Passed A levels | 1 | 1 | 1 | ||||||||||||
| Passed O levels | 1.11 | (0.84–1.46) | 0.455 | 1.05 | (0.79–1.40) | 0.723 | 1.01 | (0.76–1.35) | 0.950 | ||||||
| No qualifications | 1.23 | (0.90–1.69) | 0.191 | 1.08 | (0.78–1.50) | 0.632 | 0.97 | (0.69–1.37) | 0.869 | ||||||
| BMI at 23 | |||||||||||||||
| Normal | 1 | 1 | |||||||||||||
| Underweight | 0.41 | (0.22–0.74) | 0.003 | 0.41 | (0.23–0.75) | 0.004 | |||||||||
| Overweight | 2.71 | (2.08–3.52) | <0.001 | 2.63 | (2.02–3.44) | <0.001 | |||||||||
| Obese | 7.82 | (4.63–13.21) | <0.001 | 7.41 | (4.39–12.51) | <0.001 | |||||||||
| Occupational social class at 33 | |||||||||||||||
| Non-manual | 1 | ||||||||||||||
| Manual | 1.09 | (0.85–1.40) | 0.487 | ||||||||||||
| Wealth at 33 | |||||||||||||||
| Not owner | 1 | ||||||||||||||
| Owner - Q1 (Low price) | 0.95 | (0.71 - 1.27) | 0.722 | ||||||||||||
| Owner - Q2 | 0.83 | (0.61–1.13) | 0.240 | ||||||||||||
| Owner - Q3 | 0.74 | (0.54–1.03) | 0.072 | ||||||||||||
| Owner - Q4 | 0.72 | (0.50–1.03) | 0.076 | ||||||||||||
| Marital status at 33 | |||||||||||||||
| Couple | 1 | ||||||||||||||
| Single | 0.92 | (0.64–1.32) | 0.646 | ||||||||||||
| Divorced or widowed | 1.06 | (0.75–1.52) | 0.728 | ||||||||||||
Model 1 included mother’s pre-pregnancy BMI and all variables measured at or around birth; Model 2: Model 1 + ACE; Model 3: Model 2 + potential mediators measured at 23 years except for participants’ BMI at 23 years; Model 4: Model 3 + participant’s BMI at 23 years; Model 5: Full model
Fig. 2.
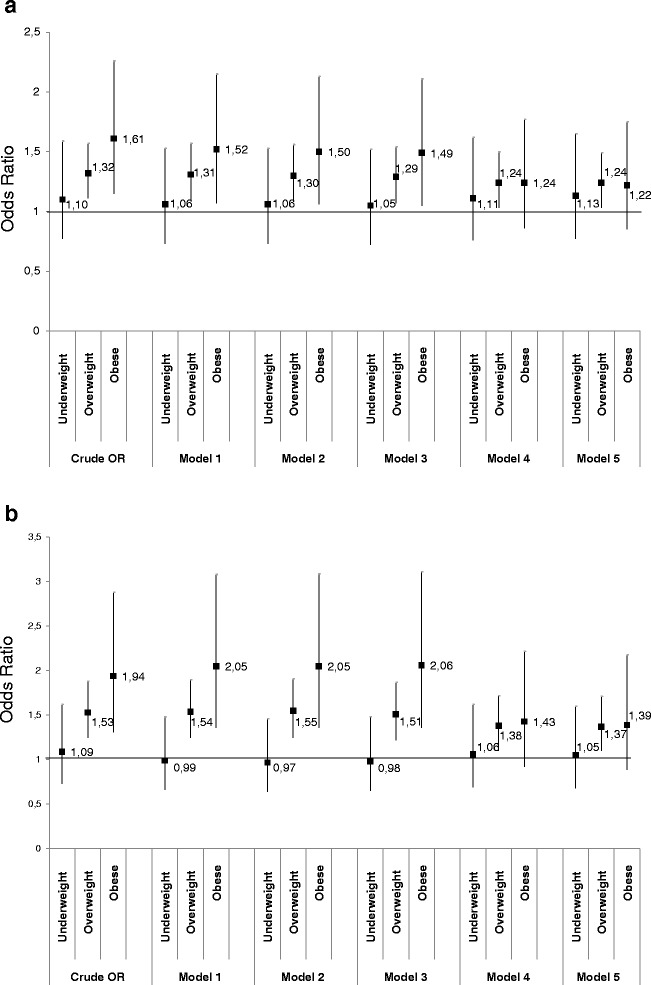
a Association between mother’s pre-pregnancy BMI and metabolic syndrome in men according to models b Association between mother’s pre-pregnancy BMI and metabolic syndrome in women according to models
Regarding the association between ACE and MetS, the association between being exposed to at least two adversities and MetS decreased by 45.5 % (95 % CI: 13.3–217.9 %) after inclusion of perinatal confounders compared with crude association and was no longer statistically significant (OR = 1.19, 95 % CI: 0.89–1.59).
Lower socioeconomic position during childhood, emergency caesarean delivery, being physically inactive and not a home owner during adulthood were independently associated with MetS.
In women (Table 4, Fig. 2b) the link between mother’s pre-pregnancy BMI and MetS persisted after adjustment for perinatal confounders (model 1), as well as after inclusion of ACE (model 2). The inclusion of potential mediators at 23 years did not change the strength of this association (model 3) except for when participants’ BMI was added (model 4). Compared with model 1, after adding participant’s BMI at 23 years, the association between mother’s pre-pregnancy BMI and MetS was attenuated by 44.6 % (95 % CI: 10.2–154.7 %) for obese (OR = 1.43, 95 % CI: 0.92–2.22) and by 25.3 % (95 % CI: 5.1–57.9 %) for overweight mothers before pregnancy (OR = 1.38, 95 % CI: 1.10–1.72) respectively. The inclusion of variables at 33 years (model 5) did not alter the association.
Regarding the association between ACE and MetS, the association between being exposed to one adversity and MetS decreased by 27.3 % (95 % CI: 2.2–122.1 %) after inclusion of perinatal confounders compared with crude association and was no longer statistically significant (OR = 1.19, 95 % CI: 0.96–1.48).
Lower socioeconomic position during childhood, emergency caesarean delivery, low birthweight, mothers younger than 23 years old at birth, smoking during pregnancy, not being a home owner during early adulthood were independently associated with MetS.
Model 1 included all variables measured at or around birth; Model 2: Model 1 + ACE; Model 3: Model 2 + potential mediators measured at 23 years except for participants’ BMI at 23 years; Model 4: Model 3 + participant’s BMI at 23 years; Model 5: Full model.
All models were also run on complete cases (1876 men and 1922 women). No significant changes regarding significant variables or direction of associations were found (data not shown).
Discussion
This study sets out a comprehensive lifecourse approach to examine the influence of both the early nutritional environment, and the psychosocial environment, on the subsequent risk of MetS. By taking a lifecourse approach, many mediating factors that may explain pathways between early nutrition and early psychosocial stress and subsequent MetS are examined. The main finding from our study is that both early nutritional and psychosocial environments are independently associated with subsequent risk of MetS. Mother’s pre-pregnancy BMI was associated with MetS in mid-life after taking into account a large range of confounders and three potential pathways (socioeconomic/materialist, psychological and behavioral). The association appeared to be mediated to a sizeable extent by offspring’s BMI at age 23, suggesting mechanisms via a mother to child transmission of BMI. However, participants’ BMI at age 23 did not fully explain the link between mother’s pre-pregnancy BMI and MetS suggesting that unidentified mechanisms may be operating other than those captured through the confounding and mediating variables used in this study, specifically health behaviors and socioeconomic pathways. The role of ACE was not clear. The positive association between ACE and MetS was indeed not significant after taking early life confounders into account, in particular childhood socioeconomic conditions and birth conditions that were independently associated with risk of MetS.
The main strength of this study is that data were prospectively measured and the large number of confounders and mediators we consider, which made that this study includes a large panel of confounders and mediators to explore MetS in a lifecourse perspective. Consequently, we were able to analyze both early nutritional and psychosocial exposures that are mainly studied separately in the literature and also to consider early birth conditions that are largely not taken into account in studies on MetS. There are also a number of limitations that need to be considered, however. The first is regarding the definition of MetS we used in the study. The definition of MetS has varied over the past decade. The prevalence of MetS may be lower when using definitions other than NCEP-ATPIII. However the risks of cardiovascular events, diabetes mellitus and hypertension are similar for NCEP-ATPIII and American Heart Association or International Diabetes Federation definitions [45]. Glycaemia was not collected in the biomedical survey used here therefore we used HbA1c with a cut-off above 6.5 % to define hyperglycaemia. HbA1c has been defined as a marker to identify diabetic status and used in other studies instead of glycaemia [46]. We were also unable to take into account whether people were treated for hypertension, diabetes or high cholesterol level because accurate data were not available. Our definition of MetS is thus a conservative one. Another weakness is the amount of missing data caused by attrition in the cohort. This weakness is partly addressed by the use of multiple imputations in our models. The standard application of multiple imputation assumes that data are MAR meaning that the probability of missing data depends on the observed data but not the missing data, which is an unverifiable assumption. Thus we cannot rule out that some data are Missing Not At Random. A way to render the MAR assumption more plausible and to limit the impact of missing not at random missingness is to include a large numbers of covariates in multiple imputations. In our analyses all important causes of missingness such as demographic characteristics, socio–economic position indicators and behavioral variables are included in the models. Any other missingness that is not accounted for by these variables is assumed to be completely random since all major systematic causes of missingness have been accounted for. We believe that this is a reasonable assumption since it has been shown that socio–economic position and age and are the main drivers of attrition in population surveys in the UK [47, 48]. Furthermore, analyses on complete cases gave a similar result which increases the robustness of our findings. Another limitation concerns the NCDS recruitment that was done in March 1958. So we do not take account for potential effects of birth-month variations that may influence the neuroendocrine regulation of metabolism and obesity [49]. Other potential limitations concern the analyses. To illustrate the influence of confounders and mediators on the associations between our two main exposures and MetS, we calculated B attenuation after inclusion of potential confounders and mediators. This approach is not a formal mediation analysis and may provide biased estimates, however when controlling for potential mediator-outcome confounders, as we did here by considering a large range of variables in analyses, the risk of bias is limited [41]. We also used a bootstrap method to improve the precision of the percent attenuation. Our use of health behaviors at 23 years as a proxy for behavioral patterns in early adulthood is also a limitation. Adult health behaviors were collected in the cohort at ages 23, 33, 41, 46. Constructing health behavior pathways using repeated measures, may explain a significantly greater part of the association between mother’s pre-pregnancy BMI and MetS compared to a baseline-only assessment of behaviors, as observed elsewhere [43]. However the inclusion of behaviors in the model did not change the association between maternal BMI before pregnancy and MetS except for BMI. So it is not likely that behaviors even by considering them in a longitudinal way, explain a significant part of the association between maternal BMI before pregnancy and MetS. Finally, it is possible that we omitted important confounders or mediators in our models. It would have been optimal to control for the mother’s gestational diabetes status, to control for an intrauterine exposure to hyperglycemia, however accurate information on this was not available. By including birthweight we should be able to capture any macrosomia effects of gestational diabetes on the cohort member. Moreover, some of the measures we used may be susceptible to measurement error, like self-reported data on maternal weight that may have resulted in some misclassification, even if self-reported weight is generally accurate in validity studies [50].
We found that mother’s pre-pregnancy BMI may be an important determinant of metabolic pathology in mid-life, mainly operating via a mother-child body-size transmission pathway. Previous works have shown that children exposed to maternal obesity in early life presented higher levels of some MetS components [17]. In our study this association was mainly attenuated after including offspring’s BMI at 23 years in the model, suggesting that this association could be explained in a significant part by a mother to child transmission of BMI. An intergenerational adiposity association is a widely observed phenomenon [16, 51–53]. One of the main issues is to explain underlying pathways and notably the respective contributions of shared environments and genetic factors in this transmission. Some studies have observed a similar influence of mother and father’s BMI on the subsequent risk of obesity in offspring [52]. Such results may point towards an influence of shared family characteristics, such as diet and physical activity. However studies that included such mediators concluded that the mother to child transmission of BMI was attenuated but still persisted after taking adult health behaviors, including diet, or socioeconomic factors into account [16, 51]. In fact, the intrauterine environment may have an important role to play [9]. Offspring exposed to maternal hyperglycaemia during their intrauterine development are more at risk of metabolic disorders such as obesity in adulthood, and that changes in maternal nutrition, in particular during fetal development, may influence subsequent predisposition to the MetS [9, 19]. Such results are in accordance with the fetal overnutrition hypothesis or an early life nutritional programming of the metabolic syndrome, a phenomenon that has been shown in animals [18]. To investigate this hypothesis in humans the majority of studies use birthweight as a proxy of intrauterine exposures during pregnancy. In our study we consider birth and perinatal conditions, in particular birthweight, and the inclusion of such variables in models did not significantly change the association between mother’s pre-pregnancy BMI and MetS in offspring. Unfortunately, in our study, we had no information on mothers’ diet during pregnancy and after birth, no information on the way babies were fed except breastfeeding and no information on diet during childhood. The information collected on mother’s pre-pregnancy BMI, however, offers an opportunity for us to capture through a proxy variable something of cohort members’ early life nutritional environment of cohort members. Ideally, we would have liked to have information on weight gain during pregnancy or parents’ waist circumferences before pregnancy. However such data are not available in the NCDS cohort. The parent–child transmission of adiposity deserves further investigation using more relevant and detailed data to characterize both nutritional environment around pregnancy and early life, and mothers’ metabolic status. With this in mind, studies analyzing the effect of mother and father adiposity on offspring adiposity at different stages of life are needed.
We found no association between early ACE and MetS after adjusting for confounders such as early socioeconomic and birth conditions. Few previous studies have observed an influence of ACE by using retrospective measures for ACE [24, 54] or using both retrospective and prospective measures [30]. There is strong evidence for the role of stress in the long term etiology of cardiometabolic diseases [31]. This evidence leads to questions about the measures used to capture psychosocial stress and specifically our definition of adversity. Thomas et al. [30] have shown that the link between adversity and subsequent risk of obesity and type 2 diabetes in mid-life was different according to the definition used for adversity suggesting that we can be exposed to measurement error or that different measurements of ACE may be capturing different types of stress. In particular we did not use any variables on sexual or physical abuse that has been shown as associated with obesity [30], because these variables were retrospectively measured (at the same time as MetS was measured) as opposed to our definition which used only variables measured prospectively to avoid recall bias. Of course, childhood adversity may not be the only or best measure of stress in early life, both prenatal and postnatal periods could also a phase where early life stress may be picked-up. For example, maternal stress during pregnancy has been associated with central adiposity in children at 13 years [55]. In animals, prenatal stress has been associated with metabolic disturbances in adult offspring [56]. As we previously observed [38], emergency caesareans were associated with subsequent risk of MetS in the NCDS cohort. Recent reviews have shown that caesarean section was a risk factor of adult obesity [57, 58]. The main hypothesis refers to the nature of the offspring microbiome that could differ according the mode of delivery [59]. In our study, it was not caesarean sections per se that influenced the risk of MetS but only if they were carried-out in an emergency. Emergency caesareans may act as a proxy of perinatal stressful events that may play a role in subsequent risk of MetS. Other perinatal variables may also be proxies for early life stress [54, 60], like birthweight or smoking during pregnancy that were associated with risk of MetS in our study, in particular among women. It is noteworthy that the influence of these ‘perinatal stress’ proxies appear stronger in women than in men suggesting than women could be more sensitive to early life stress exposures than men in accordance with other studies. Early life exposures have indeed been found to be more strongly associated with autonomic nervous system reactivity in women [60]. Regarding risk of MetS, different biological and social pathways have been identified in men and women [13, 44].
Psychosocial stress is also associated with socioeconomic conditions [25] which are known to be associated with subsequent health and in particular with MetS [12, 14, 61]. In our study, psychosocial adversity was not significant after including socioeconomic variables such as mother’s level of education and father’s social class at birth which were independent risk factors of MetS. The fact that the link between childhood socioeconomic conditions and MetS persisted in the full model, after the inclusion of a large range of confounders and mediators, questions the mechanisms involved and not considered in the study. Pathways likely to explain this association deserve to be explored in more depth.
Conclusion
Our results show that it is relevant to study MetS taking a lifecourse perspective. Indeed mother’s BMI before pregnancy is strongly associated the likelihood of MetS in adulthood suggesting that some aspects of early nutritional environment may influence the risk of subsequent MetS in midlife. One of the main mechanisms may involve a mother-to-child BMI transmission which deserves more attention. Other mechanisms linking mother’s pre-pregnancy BMI and MetS are likely to be operational. The link between exposure to adversity during childhood and the risk of MetS is less clear since this association was not significant after considering early socioeconomic and birth conditions that were independently associated with risk of MetS. Pathways linking early psychosocial stress, by disentangling the various aspects and dimensions of this stress and subsequent risk of MetS deserve further investigations. These results can have potentially important implications for prevention policies targeting MetS, by identifying early life and the parent to child transmission of adiposity as possible targets. The implementation of potential prevention policies will need to understand how such transmissions occur.
Acknowledgments
The authors are grateful to the Centre for Longitudinal Studies (CLS), Institute of Education for the use of the National Child Development Study (NCDS) data and to the Economic and Social Data Service ESAD for making them available.
Funding
The present work is part of the Incorporation Biologique et Inégalités Sociales de Santé project supported by funds from Agence Nationale de la Recherche (ANR-12-DSSA-0004) and the Fond Français pour l’Alimentation et la Santé (12 D-25).
Availability of data and materials
NCDS data are open access datasets available to non-profit research organizations. None of the authors of this paper were involved in collecting data for the NCDS, this was organized and carried out by the Centre for Longitudinal Studies at the UCL Institute of Education (http://www.cls.ioe.ac.uk/) who then deposited the data on the UK Data Archive. The data can be accessed by bona fide researchers by registering through the UK Data Service at the University of Essex (https://discover.ukdataservice.ac.uk/series/?sn=2000032. Once the registration process has been approved researchers can download the data and use it to carry out the same investigation using the method described above.
Authors’ contributions
CD was involved in the conception and design of the study, analysing and interpreting the data, drafted the manuscript and made modifications. MKI, RF were involved in the conception and design of the study, analysing and interpreting the data, and revising the manuscript. MD, CBS and BL analysed and interpreted the analyses, and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Written informed consent was obtained from the parents for childhood measurements and ethical approval for the adult data collection was obtained from the National Research Ethics Advisory Panel.
Abbreviations
- ACE
Adverse childhood experiences
- BMI
Body mass index
- HbA1c
Glycosylated hemoglobin
- MAR
Missing at random
- MetS
Metabolic syndrome
- NCDS
National Child Development Study
- NCEP-ATP III
National Cholesterol Education Program Adult Treatment Panel III
Contributor Information
C. Delpierre, Phone: 00 33 5 61 14 56 74, Email: cyrille.delpierre@inserm.fr
R. Fantin, Email: romain.fantin@inserm.fr
C. Barboza-Solis, Email: cristina.barboza-solis@inserm.fr
B. Lepage, Email: benoit.lepage@univ-tlse3.fr
M. Darnaudéry, Email: muriel.darnaudery@u-bordeaux2.fr
M. Kelly-Irving, Email: michelle.kelly@inserm.fr
References
- 1.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49(4):403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 3.O’Neill S, O’Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015;16(1):1–12. doi: 10.1111/obr.12229. [DOI] [PubMed] [Google Scholar]
- 4.Qiao Q. Comparison of different definitions of the metabolic syndrome in relation to cardiovascular mortality in European men and women. Diabetologia. 2006;49(12):2837–2846. doi: 10.1007/s00125-006-0438-6. [DOI] [PubMed] [Google Scholar]
- 5.Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D. Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care. 2012;35(11):2402–2411. doi: 10.2337/dc12-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mendonca FM, de Sousa FR, Barbosa AL, Martins SC, Araujo RL, Soares R, Abreu C. Metabolic syndrome and risk of cancer: which link? Metabolism. 2015;64(2):182–189. doi: 10.1016/j.metabol.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Siervo M, Harrison SL, Jagger C, Robinson L, Stephan BC. Metabolic syndrome and longitudinal changes in cognitive function: a systematic review and meta-analysis. J Alzheimers Dis. 2014;41(1):151–161. doi: 10.3233/JAD-132279. [DOI] [PubMed] [Google Scholar]
- 8.Rios JA, Cisternas P, Arrese M, Barja S, Inestrosa NC. Is Alzheimer’s disease related to metabolic syndrome? A Wnt signaling conundrum. Prog Neurobiol. 2014;121:125–146. doi: 10.1016/j.pneurobio.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Symonds ME, Sebert SP, Hyatt MA, Budge H. Nutritional programming of the metabolic syndrome. Nat Rev Endocrinol. 2009;5(11):604–610. doi: 10.1038/nrendo.2009.195. [DOI] [PubMed] [Google Scholar]
- 10.Blane D, Hart CL, Smith GD, Gillis CR, Hole DJ, Hawthorne VM. Association of cardiovascular disease risk factors with socioeconomic position during childhood and during adulthood. BMJ. 1996;313(7070):1434–1438. doi: 10.1136/bmj.313.7070.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wannamethee SG, Whincup PH, Shaper G, Walker M. Influence of fathers’ social class on cardiovascular disease in middle-aged men. Lancet. 1996;348(9037):1259–1263. doi: 10.1016/S0140-6736(96)02465-8. [DOI] [PubMed] [Google Scholar]
- 12.Chichlowska KL, Rose KM, Diez-Roux AV, Golden SH, McNeill AM, Heiss G. Life course socioeconomic conditions and metabolic syndrome in adults: the Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 2009;19(12):875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gustafsson PE, Persson M, Hammarstrom A. Life course origins of the metabolic syndrome in middle-aged women and men: the role of socioeconomic status and metabolic risk factors in adolescence and early adulthood. Ann Epidemiol. 2011;21(2):103–110. doi: 10.1016/j.annepidem.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 14.Langenberg C, Kuh D, Wadsworth ME, Brunner E, Hardy R. Social circumstances and education: life course origins of social inequalities in metabolic risk in a prospective national birth cohort. Am J Public Health. 2006;96(12):2216–2221. doi: 10.2105/AJPH.2004.049429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loucks EB, Magnusson KT, Cook S, Rehkopf DH, Ford ES, Berkman LF. Socioeconomic position and the metabolic syndrome in early, middle, and late life: evidence from NHANES 1999–2002. Ann Epidemiol. 2007;17(10):782–790. doi: 10.1016/j.annepidem.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Power C, Pouliou T, Li L, Cooper R, Hypponen E. Parental and offspring adiposity associations: insights from the 1958 British birth cohort. Ann Hum Biol. 2011;38(4):390–399. doi: 10.3109/03014460.2011.591827. [DOI] [PubMed] [Google Scholar]
- 17.Cooper R, Pinto Pereira SM, Power C, Hypponen E. Parental obesity and risk factors for cardiovascular disease among their offspring in mid-life: findings from the 1958 British Birth Cohort Study. Int J Obes (Lond) 2013;37(12):1590–1596. doi: 10.1038/ijo.2013.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li M, Sloboda DM, Vickers MH. Maternal obesity and developmental programming of metabolic disorders in offspring: evidence from animal models. Exp Diabetes Res. 2011;2011:592408. doi: 10.1155/2011/592408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang S, Rattanatray L, Morrison JL, Nicholas LM, Lie S, McMillen IC. Maternal obesity and the early origins of childhood obesity: weighing up the benefits and costs of maternal weight loss in the periconceptional period for the offspring. Exp Diabetes Res. 2011;2011:585749. doi: 10.1155/2011/585749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jaaskelainen P, Magnussen CG, Pahkala K, Mikkila V, Kahonen M, Sabin MA, Fogelholm M, Hutri-Kahonen N, Taittonen L, Telama R, et al. Childhood nutrition in predicting metabolic syndrome in adults: the cardiovascular risk in Young Finns Study. Diabetes Care. 2012;35(9):1937–1943. doi: 10.2337/dc12-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 22.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19(5):544–554. doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 24.Davis CR, Dearing E, Usher N, Trifiletti S, Zaichenko L, Ollen E, Brinkoetter MT, Crowell-Doom C, Joung K, Park KH, et al. Detailed assessments of childhood adversity enhance prediction of central obesity independent of gender, race, adult psychosocial risk and health behaviors. Metabolism. 2014;63(2):199–206. doi: 10.1016/j.metabol.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med. 2005;67(6):846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- 26.Kelly-Irving M, Lepage B, Dedieu D, Bartley M, Blane D, Grosclaude P, Lang T, Delpierre C. Adverse childhood experiences and premature all-cause mortality. Eur J Epidemiol. 2013;28(9):721–734. doi: 10.1007/s10654-013-9832-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelly-Irving M, Lepage B, Dedieu D, Lacey R, Cable N, Bartley M, Blane D, Grosclaude P, Lang T, Delpierre C. Childhood adversity as a risk for cancer: findings from the 1958 British birth cohort study. BMC Public Health. 2013;13(1):767. doi: 10.1186/1471-2458-13-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, Poulton R, Caspi A. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Non AL, Rewak M, Kawachi I, Gilman SE, Loucks EB, Appleton AA, Roman JC, Buka SL, Kubzansky LD. Childhood social disadvantage, cardiometabolic risk, and chronic disease in adulthood. Am J Epidemiol. 2014;180(3):263–271. doi: 10.1093/aje/kwu127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas C, Hypponen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- 31.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–354. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 32.Morris MJ, Beilharz JE, Maniam J, Reichelt AC, Westbrook RF. Why is obesity such a problem in the 21st century? The intersection of palatable food, cues and reward pathways, stress, and cognition. Neurosci Biobehav Rev. 2015;58:36-45. [DOI] [PubMed]
- 33.Correia-Branco A, Keating E, Martel F. Maternal undernutrition and fetal developmental programming of obesity: the glucocorticoid connection. Reprod Sci. 2015;22(2):138–145. doi: 10.1177/1933719114542012. [DOI] [PubMed] [Google Scholar]
- 34.Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21(3):159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Power C, Elliott J. Cohort profile: 1958 British birth cohort (National Child Development Study) Int J Epidemiol. 2006;35(1):34–41. doi: 10.1093/ije/dyi183. [DOI] [PubMed] [Google Scholar]
- 36.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97. [DOI] [PubMed]
- 37.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39(1):93–98. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 38.Bouhanick B, Ehlinger V, Delpierre C, Chamontin B, Lang T, Kelly-Irving M. Mode of delivery at birth and the metabolic syndrome in midlife: the role of the birth environment in a prospective birth cohort study. BMJ Open. 2014;4(5):e005031. doi: 10.1136/bmjopen-2014-005031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodgers B, Pickles A, Power C, Collishaw S, Maughan B. Validity of the Malaise Inventory in general population samples. Soc Psychiatry Psychiatr Epidemiol. 1999;34(6):333–341. doi: 10.1007/s001270050153. [DOI] [PubMed] [Google Scholar]
- 40.Rutter M, Tizard J, Kingsley W. Education, health and behaviour. 1970. [Google Scholar]
- 41.Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–1519. doi: 10.1093/ije/dyt127. [DOI] [PubMed] [Google Scholar]
- 42.Stringhini S, Batty GD, Bovet P, Shipley MJ, Marmot MG, Kumari M, Tabak AG, Kivimaki M. Association of lifecourse socioeconomic status with chronic inflammation and type 2 diabetes risk: the Whitehall II prospective cohort study. PLoS Med. 2013;10(7):e1001479. doi: 10.1371/journal.pmed.1001479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stringhini S, Sabia S, Shipley M, Brunner E, Nabi H, Kivimaki M, Singh-Manoux A. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rudnicka AR, Rumley A, Whincup PH, Lowe GD, Strachan DP. Sex differences in the relationship between inflammatory and hemostatic biomarkers and metabolic syndrome: British 1958 Birth Cohort. J Thromb Haemost. 2011;9(12):2337–2344. doi: 10.1111/j.1538-7836.2011.04517.x. [DOI] [PubMed] [Google Scholar]
- 45.Mancia G, Bombelli M, Facchetti R, Casati A, Ronchi I, Quarti-Trevano F, Arenare F, Grassi G, Sega R. Impact of different definitions of the metabolic syndrome on the prevalence of organ damage, cardiometabolic risk and cardiovascular events. J Hypertens. 2010;28(5):999–1006. doi: 10.1097/HJH.0b013e328337a9e3. [DOI] [PubMed] [Google Scholar]
- 46.The International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32(7):1327–1334. [DOI] [PMC free article] [PubMed]
- 47.Noah Uhrig S. The nature and causes of attrition in the British Household Panel Survey. 2008. [Google Scholar]
- 48.Durrant G, Goldstein H. Analysing the probability of attrition in a longitudinal survey. 2008. [Google Scholar]
- 49.Stevenson TJ, Visser ME, Arnold W, Barrett P, Biello S, Dawson A, Denlinger DL, Dominoni D, Ebling FJ, Elton S, et al. Disrupted seasonal biology impacts health, food security and ecosystems. Proc Biol Sci. 2015;282(1817):20151453. doi: 10.1098/rspb.2015.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Niedhammer I, Bugel I, Bonenfant S, Goldberg M, Leclerc A. Validity of self-reported weight and height in the French GAZEL cohort. Int J Obes Relat Metab Disord. 2000;24(9):1111–1118. doi: 10.1038/sj.ijo.0801375. [DOI] [PubMed] [Google Scholar]
- 51.Cooper R, Hypponen E, Berry D, Power C. Associations between parental and offspring adiposity up to midlife: the contribution of adult lifestyle factors in the 1958 British Birth Cohort Study. Am J Clin Nutr. 2010;92(4):946–953. doi: 10.3945/ajcn.2010.29477. [DOI] [PubMed] [Google Scholar]
- 52.Kivimaki M, Lawlor DA, Smith GD, Elovainio M, Jokela M, Keltikangas-Jarvinen L, Viikari JS, Raitakari OT. Substantial intergenerational increases in body mass index are not explained by the fetal overnutrition hypothesis: the Cardiovascular Risk in Young Finns Study. Am J Clin Nutr. 2007;86(5):1509–1514. doi: 10.1093/ajcn/86.5.1509. [DOI] [PubMed] [Google Scholar]
- 53.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 54.Ryckman KK, Borowski KS, Parikh NI, Saftlas AF. Pregnancy Complications and the Risk of Metabolic Syndrome for the Offspring. Curr Cardiovasc Risk Rep. 2013;7(3):217–223. doi: 10.1007/s12170-013-0308-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cao-Lei L, Dancause KN, Elgbeili G, Massart R, Szyf M, Liu A, Laplante DP, King S. DNA methylation mediates the impact of exposure to prenatal maternal stress on BMI and central adiposity in children at age 13½ years: Project Ice Storm. Epigenetics. 2015;10(8):749–61. [DOI] [PMC free article] [PubMed]
- 56.Lesage J, Del-Favero F, Leonhardt M, Louvart H, Maccari S, Vieau D, Darnaudery M. Prenatal stress induces intrauterine growth restriction and programmes glucose intolerance and feeding behaviour disturbances in the aged rat. J Endocrinol. 2004;181(2):291–296. doi: 10.1677/joe.0.1810291. [DOI] [PubMed] [Google Scholar]
- 57.Darmasseelane K, Hyde MJ, Santhakumaran S, Gale C, Modi N. Mode of delivery and offspring body mass index, overweight and obesity in adult life: a systematic review and meta-analysis. PLoS One. 2014;9(2):e87896. doi: 10.1371/journal.pone.0087896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li HT, Zhou YB, Liu JM. The impact of cesarean section on offspring overweight and obesity: a systematic review and meta-analysis. Int J Obes (Lond) 2013;37(7):893–899. doi: 10.1038/ijo.2012.195. [DOI] [PubMed] [Google Scholar]
- 59.Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, Knight R. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107(26):11971–11975. doi: 10.1073/pnas.1002601107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kajantie E, Raikkonen K. Early life predictors of the physiological stress response later in life. Neurosci Biobehav Rev. 2010;35(1):23–32. doi: 10.1016/j.neubiorev.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 61.Gustafsson PE, Janlert U, Theorell T, Hammarstrom A. Life-course socioeconomic trajectories and diurnal cortisol regulation in adulthood. Psychoneuroendocrinology. 2010;35(4):613–623. doi: 10.1016/j.psyneuen.2009.09.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
NCDS data are open access datasets available to non-profit research organizations. None of the authors of this paper were involved in collecting data for the NCDS, this was organized and carried out by the Centre for Longitudinal Studies at the UCL Institute of Education (http://www.cls.ioe.ac.uk/) who then deposited the data on the UK Data Archive. The data can be accessed by bona fide researchers by registering through the UK Data Service at the University of Essex (https://discover.ukdataservice.ac.uk/series/?sn=2000032. Once the registration process has been approved researchers can download the data and use it to carry out the same investigation using the method described above.


