Abstract
Background:
Concussion injuries have been highlighted to the American public through media and research. While recent studies have shown increased traumatic brain injuries (TBIs) diagnosed in emergency departments across the United States, no studies have evaluated trends in concussion diagnoses across the general US population in various age groups.
Purpose:
To evaluate the current incidence and trends in concussions diagnosed across varying age groups and health care settings in a large cross-sectional population.
Study Design:
Descriptive epidemiological study.
Methods:
Administrative health records of 8,828,248 members of a large private-payer insurance group in the United States were queried. Patients diagnosed with concussion from years 2007 through 2014 were stratified by year of diagnosis, age group, sex, classification of concussion, and health care setting of diagnosis (eg, emergency department vs physician’s office). Chi-square testing was used for statistical analysis.
Results:
From a cohort of 8,828,248 patients, 43,884 patients were diagnosed with a concussion. Of these patients, 55% were male and over 32% were in the adolescent age group (10-19 years old). The highest incidence of concussion was seen in patients aged 15 to 19 years (16.5/1000 patients), followed by those aged 10 to 14 years (10.5/1000 patients), 20 to 24 years (5.2/1000 patients), and 5 to 9 years (3.5/1000 patients). Overall, there was a 60% increase in concussion incidence from 2007 to 2014. The largest increases were in the 10- to 14-year (143%) and 15- to 19-year (87%) age groups. Based on International Classification of Disease–9th Revision classification, 29% of concussions were associated with some form of loss of consciousness. Finally, 56% of concussions were diagnosed in the emergency department and 29% in a physician’s office, with the remainder in urgent care clinics or inpatient settings.
Conclusion:
The incidence of concussion diagnosed in the general US population is increasing, driven largely by a substantial rise in the adolescent age group. The youth population should be prioritized for ongoing work in concussion education, diagnosis, treatment, and prevention.
Clinical Relevance:
The rise of concussions in the adolescent age group across the general population is concerning, and clinical efforts to prevent these injuries are needed.
Keywords: concussion, traumatic brain injury (TBI), trends, epidemiology, adolescents, youth
In the past decade, the United States Centers for Disease Control and Prevention’s (CDC’s) Heads Up campaign and the media spotlight have brought the topic of concussion to the attention of the American public. Concussions are a form of mild traumatic brain injury (mTBI) resulting in transient functional and biochemical changes in the brain.10,13,24 Acutely, these injuries can lead to time lost from sport, work, and school as well as significant medical costs.18,42 Alarmingly, the CDC reported increasing rates of TBI-related emergency department (ED) visits from 2001 through 2010, with mild TBI representing 75% of the visits.6,7 These findings were supported by multiple studies of TBI and concussion diagnosis incidence in EDs, including a 2014 article demonstrating an 8-fold increase in ED visits for TBI (compared with all ED visits) from 2006 to 2010.1,8,12,22,45
Recent attention has been paid to sports-related concussion at the youth through professional levels, and in particular, in adolescent athletes.10,20,21,27,31,33,46 Smaller cohort studies of pediatric and high school athletes have indicated a rise in concussions for certain sports such as boys’ football and girls’ soccer.20,21,33 However, a recent report on athletes from the National Collegiate Athletic Association (NCAA) from 2009 to 2014 suggests that in this population, there has not been a linear increase in concussions nationally.46 Varying trends from these cohorts and from ED visits in the United States demonstrate the need for investigation of concussion incidence across the general population, accounting for different age groups and health care settings.
Understanding the long-term sequelae of concussion has been challenging for investigators due to range of severity of injury, diversity of symptomatology, and feasibility of extended follow-up. Though the majority of concussion patients experience symptom resolution within weeks of injury,17,26 postconcussive syndrome,4,28,39 depression,11,19 and movement and balance disorders3,34,37 have been described in subsets of patients after concussion. Furthermore, neuroimaging and neuropathologic studies suggest that there may be chronic structural abnormalities in the brain after multiple concussions.9,16 Anecdotal links between repetitive mTBI and neurodegenerative disorders such as chronic traumatic encephalopathy and Parkinsonism have caused alarm but have not been studied systematically.23,25,38 In conjunction with rising concern over the possibility of long-term consequences, concussion rehabilitation protocol recommendations have been updated by numerous organizations.2,14,15,24,35 A stepwise return to play is now recommended by the American Academy of Neurology and was outlined at the 4th International Conference on Concussion in Sport in Zurich in 2012.14,18
While beyond the scope of this study, these controversies highlight the need for further research on epidemiology, diagnosis, management, and surveillance for long-term sequelae in the concussion population. The purpose of this study was to evaluate recent trends in the diagnosis of concussion in a large cross-sectional population in the United States, stratified by patient age, sex, and health care setting. We hypothesized that the incidence of concussions diagnosed is rising over time, particularly in the younger population.
Methods
A cross-sectional analysis was performed using administrative health records of members of a large private-payer insurance group in the United States (Humana Inc). Humana Inc provides health coverage to over 8.8 million patients younger than 65 years, including patients from across the West, South, Northeast, and Midwest regions of the country. Deidentified, Health Insurance Portability and Accountability Act (HIPAA)–compliant data from this population was queried using the PearlDiver Technologies database.36,43,44
International Classification of Disease–9th Revision (ICD-9) codes for concussion (see Appendix Table A1) were used to retrospectively identify patients with diagnoses made between 2007 and 2014. Search results yielded number of patients with the coding parameters queried, year of diagnosis, age group (by 5-year interval), sex, and health care setting. Classification of concussion and association with loss of consciousness (LOC) were analyzed using ICD-9 coding. Population demographics for the Humana cohort were used to calculate incidence for each parameter (see Appendix Table A2).
Patients aged 0 to 64 years were included in this analysis because Humana data may not be an accurate cross-sectional analysis of the population older than 65 years, as those patients are more likely to have Medicare rather than private insurance.
Chi-square analysis was performed to determine statistical significance of concussion diagnosis with regard to year of diagnosis, age group, sex, ICD-9 classification, and health care setting. Concussion diagnoses were stratified according to each category, and chi-square analysis was used to determine significant distribution differences within each area. The Cochrane-Armitage trend test was then used to evaluate temporal trends for diagnosis between age groups. The level of significance was defined to be P < .05. All statistical calculations were performed using SAS software version 9.3 (SAS Institute).
This study was considered exempt from review from the University of California–San Francisco Human Research Protection Program because it did not involve human subjects; we received deidentified data only.
Results
A total of 8,828,248 patients from years 2007 through 2014 were included for analysis. During this period, 43,884 patients were diagnosed with a concussion (Table 1). Males accounted for 55% of concussion patients (24,066), with females accounting for the other 45% (19,818). The incidence of concussion in males was nearly 1.5 times higher than in females (9.4/1000 patients vs 6.6/1000 patients, respectively).
TABLE 1.
Distribution of Concussions by Year, Age Group, and Sex
| Patients Diagnosed With Concussion, n | Concussion Incidence per 1000 Patients | P Valuea | |
|---|---|---|---|
| Year | <.001 | ||
| 2007 | 3529 | 1.4 | |
| 2008 | 4038 | 1.6 | |
| 2009 | 4798 | 2.1 | |
| 2010 | 4740 | 2.1 | |
| 2011 | 5149 | 2.2 | |
| 2012 | 6477 | 2.5 | |
| 2013 | 6936 | 2.5 | |
| 2014 | 8217 | 2.3 | |
| Age group, y | <.001 | ||
| <5 | 1322 | 1.7 | |
| 5-9 | 1855 | 3.5 | |
| 10-14 | 5425 | 10.5 | |
| 15-19 | 8499 | 16.5 | |
| 20-24 | 3061 | 5.2 | |
| 25-29 | 2046 | 2.7 | |
| 30-34 | 1973 | 2.5 | |
| 35-39 | 2167 | 2.5 | |
| 40-44 | 2588 | 2.6 | |
| 45-49 | 2997 | 2.6 | |
| 50-54 | 3671 | 2.8 | |
| 55-59 | 4088 | 3 | |
| 60-64 | 4192 | 3.1 | |
| Sex | <.001 | ||
| Female | 19,818 | 6.6 | |
| Male | 24,066 | 9.4 |
aChi-square analysis was used to determine statistical significance for each group.
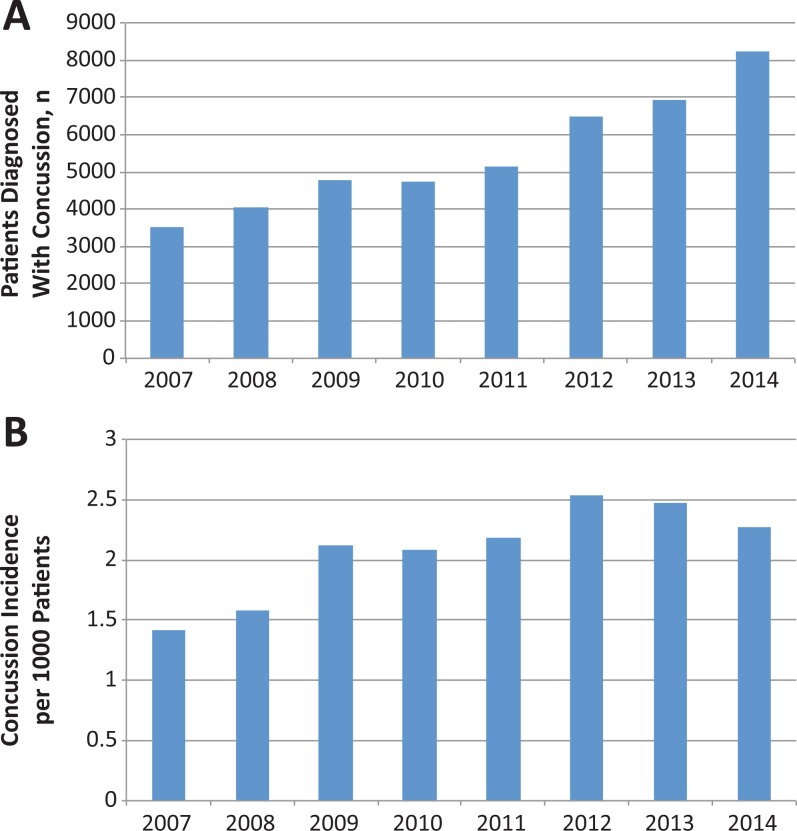
The total number of patients diagnosed with concussion increased from 3529 in 2007 to 8217 in 2014 (Figure 1A). The incidence of patients diagnosed with concussion increased by over 60%, from 1.4 cases for every 1000 patients in 2007 to 2.3 per 1000 in 2014, peaking in 2012 and 2013 with 2.5 per 1000 patients (P < .001) (Figure 1B).
Figure 1.
(A) Total number of patients diagnosed with concussions by year and (B) incidence of patients diagnosed with concussions for every 1000 patients in the cohort, years 2007 through 2014.
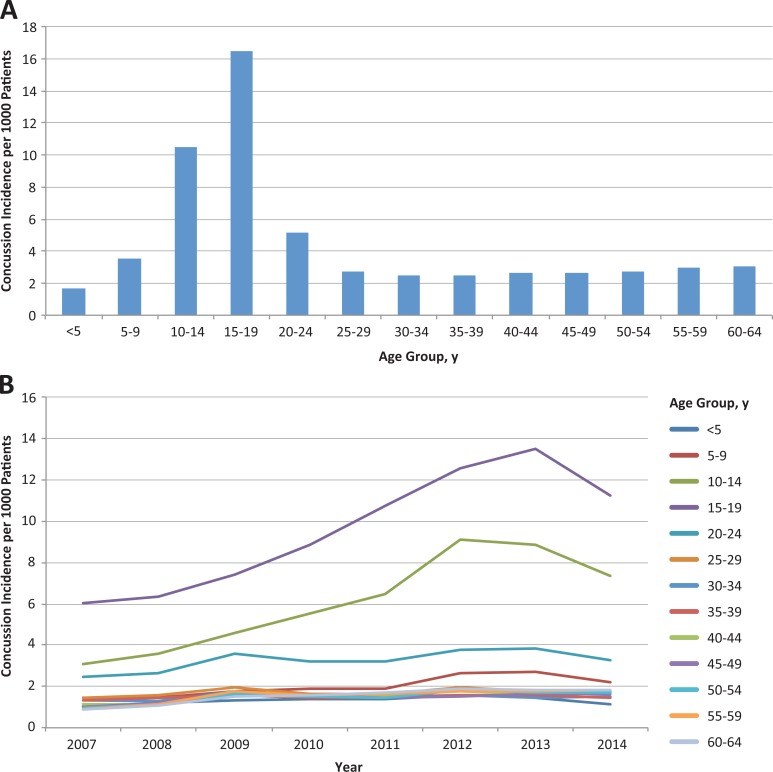
Analysis by age group demonstrated that adolescent patients accounted for the highest percentage of concussion in this cross-sectional cohort. Patients aged 10 to 19 years accounted for 32% of concussions (n = 13,924). The highest incidence was seen in the 15- to 19-year age group, with 16.5 cases for every 1000 patients, followed by the 10- to 14-year age group, with 10.5 cases for every 1000 patients. The 20- to 24-year (5.2/1000 patients) and 5- to 9-year (3.5/1000 patients) age groups had the next highest incidences (Figure 2A). Further analysis showed that the incidence of diagnosed concussion increased dramatically in the adolescent age group from 2007 to 2014 (Figure 2B). The 10- to 14-year and 15- to 19-year age groups showed increases of 143% and 87%, respectively, while the incidence in all other age groups showed lesser increases during this time period (P < .001).
Figure 2.
Incidence of patients diagnosed with concussion for every 1000 patients (A) in each age group and (B) in that age group stratified by year, 2007 through 2014.
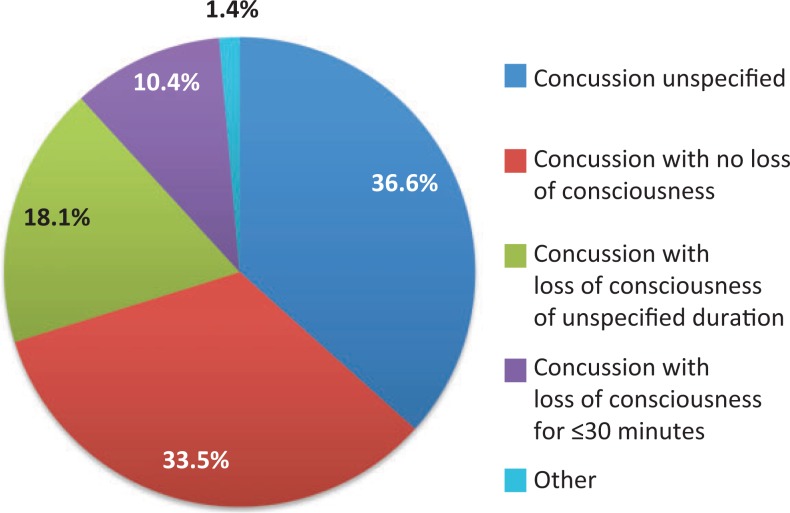
Classification of concussions by ICD-9 diagnosis codes showed that 37% of cases were reported as “concussion unspecified” followed by “concussion with no loss of consciousness” (34%). The remaining 29% of concussions were associated with some form of LOC: “concussion with loss of consciousness of unspecified duration” (18%), “concussion with loss of consciousness of 30 minutes of less” (10%), and “concussion with loss of consciousness greater than 30 minutes” (<1%) (P < .001) (Figure 3). For the cases with descriptive coding, approximately half (53%) involved no LOC and the other half (47%) involved some form of LOC.
Figure 3.
Classification of concussion according to International Classification of Disease–9th Revision diagnosis codes. The “other” category includes codes 850.12 (concussion with loss of consciousness from 31 to 59 minutes), 850.2 (concussion with moderate loss of consciousness), 850.3 (concussion with prolonged loss of consciousness and return to preexisting conscious level), 850.4 (concussion with prolonged loss of consciousness without return to preexisting conscious level), and 850.1 (concussion with brief loss of consciousness).
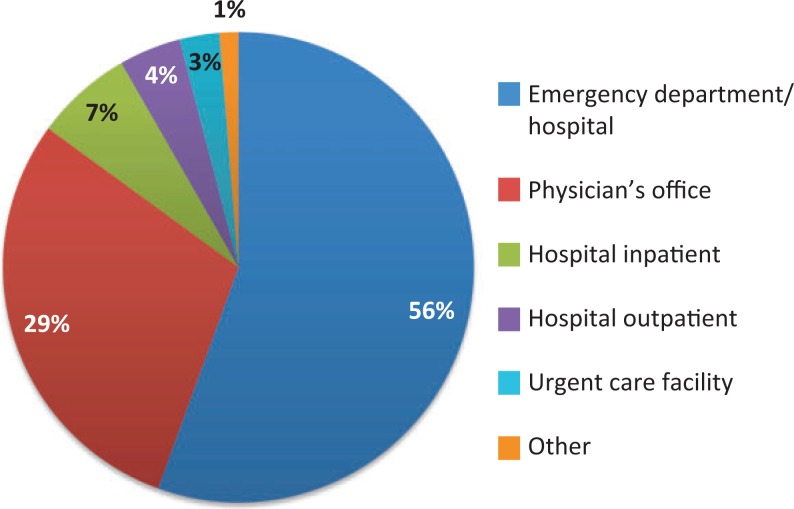
Finally, analysis of the health care setting of the diagnosis demonstrated that the majority of cases (56%) were diagnosed in the ED of a hospital, followed by 29% in a physician’s office (Figure 4). Seven percent were diagnosed during inpatient hospital stays, with urgent care facilities and other locations such as skilled nursing facilities accounting for the remainder (P < .001).
Figure 4.
Health care setting of patient visit in which concussion was diagnosed. The “other” category includes the following: ambulance (land), ambulance (air or water), skilled nursing facility, rural health clinic, patient’s home, and independent laboratory.
Discussion
This is the first cross-sectional analysis of concussion diagnosis in the general US population. We analyzed more than 8.8 million patients younger than 65 years from 2007 through 2014 and found that patients diagnosed with concussion are on the rise. A significant increase in concussions diagnosed in adolescents aged 10 to 19 years was largely responsible for this trend.
Adolescents accounted for the largest proportion of concussions in patients younger than 65 years (32%), with temporal analysis revealing that the incidence of concussion diagnosed in 10- to 19-year-olds more than doubled from 2007 to 2014. This rise of concussions in the youth was largely responsible for the overall trend of increased concussions in recent years as other age groups exhibited fewer gains. One explanation for the epidemic of youth concussion is that it may result from increased sports-related events, as evidence supporting the benefits of exercise in youth has caused a recent national promotion of exercise and sports participation.32,40,41 Furthermore, it is largely this age group that participates in organized contact sports. Because our analysis lacks information concerning the mechanism of injury, we cannot delineate the percentage of concussions that were sports-related; however, our findings are consistent with epidemiological studies demonstrating increased visits for sports-related TBI in US EDs.5,8 Moreover, other causes of concussion such as high-level trauma have been reported to decrease in recent years in the United States, further supporting sports-related causes as a factor for the rise of concussions in the youth population.30
Previous reports from pediatric and high school athlete cohorts have indicated a rise of concussions in certain sports such as boys’ football and girls’ soccer,10,20,21,27,31,33 but a recent analysis of NCAA athletes suggests that there has not been an overall increase in this population.46 This may be due to the health care setting in which NCAA athletes are treated, as team providers may work closely with these athletes on a daily basis to more stringently assess true concussion diagnoses. Yet, with an estimated 8 million high school athletes in the general US population, of which only 6% go on to play at the NCAA level,29 data from our cross-sectional analysis may offer a more representative sample of the current national trend. The increased diagnosis of concussion demonstrated here may indicate increased frequency of injury, but it may also be indicative of an improved awareness for the injury by patients, parents, coaches, sideline medical staff, and treating physicians. During this study period, the CDC’s Heads Up program has caused numerous states to alter guidelines for treatment of youth concussions.5–7 For example, California amended state laws in 2012 that included concussion training as a requirement for all high school sports coaches. While this study cannot determine which factor is responsible for the findings, clearly concussion is becoming an injury that is seen frequently in youth sports as well as the health care setting. Therefore, because of the rise of concussion diagnoses in young patients aged 10 to 19 years and due to the association between concussion and participation in sports, we suggest that work to advance the education, treatment, and prevention of concussion should target the youth athlete.
Concussion diagnosis frequently occurs in the ED; however, concussion is also treated in other settings. Our study included health care settings in addition to the ED, demonstrating that while over half of all concussions were diagnosed in the ED of a hospital, approximately 30% of the diagnoses were made in a physician’s office. Capturing health care locations where a concussion can be initially diagnosed offers a more representative cross-sectional analysis. These data suggest that not only should emergency physicians have the knowledge and skills to care for patients with concussion, but outpatient clinicians also should have the confidence and competence to manage concussion cases.
Concussion patients were more likely to be male in this population. This may be attributed to contact sports such as football and other high-risk activities such as skateboarding and boxing that are male dominated. Although previous studies have shown that the rate of concussion in female athletes from sports such as soccer can be high,31,33 our results reveal that based solely on sex and irrespective of sport, the incidence of concussion in male patients was one and a half times greater than that in female patients. Finally, classification of concussions as reported by ICD-9 code established that 29% of concussions were accompanied with some form of loss of consciousness. This accounted for approximately half of concussions where association with LOC was specified. The 37% of cases classified as “concussion unspecified” may be cases where LOC could not be determined and represent an example of the limitation of using administrative data records.
Limitations to this study include biases inherent to the use of a large administrative database and lack of patient-reported outcomes. Using ICD-9 codes, errors in coding are undetectable. The private payer population database is merely a sample of patients and thus may not be a true representation of incidence among the US population. Patients without health care insurance were not captured in this study. The PearlDiver database is structured to preserve patient confidentiality, and thus, patient-level data are unavailable for regression analysis of relevant demographic and epidemiologic factors. For HIPAA compliance, the actual age of each patient is unavailable, only allowing identification of age group. Concussion diagnosis codes can be used after a major trauma or polytrauma such as a motor vehicle accident, but these codes can also represent injuries suffered during sporting events. As we lack information about the mechanism of injury, we cannot delineate the percentage of concussions that were sports-related or the type of sport, and as an administrative database study we could not capture diagnoses made by athletic trainers during games or in the training room. In addition, the rise in diagnoses may be from increased awareness from physicians as well as from increased injuries, and this analysis cannot resolve these variables. This study also cannot account for underreporting of concussion symptoms by athletes, and follow-up information after diagnosis was not tracked. Finally, the database only includes records from years 2007 through 2014. There appears to be an early trend for decrease in concussions in 2014 compared with 2013, but more data are needed to track incidence in the future to see the effects of increased awareness and protection protocols for concussion.
Conclusion
The incidence of concussion diagnosed in the general population in the United States is increasing, driven largely by a substantial rise in the adolescent age group. The youth population should be prioritized for ongoing work in concussion education, diagnosis, treatment, and prevention.
Appendix
TABLE A1.
ICD-9 Diagnosis Codes for Concussiona
| Concussion with no loss of consciousness | ICD-9-D-850.0 |
| Concussion with brief loss of consciousness | ICD-9-D-850.1 |
| Concussion with loss of consciousness of 30 minutes or less | ICD-9-D-850.11 |
| Concussion with loss of consciousness from 31 to 59 minutes | ICD-9-D-850.12 |
| Concussion with moderate loss of consciousness | ICD-9-D-850.2 |
| Concussion with prolonged loss of consciousness and return to pre-existing conscious level | ICD-9-D-850.3 |
| Concussion with prolonged loss of consciousness without return to pre-existing conscious level | ICD-9-D-850.4 |
| Concussion with loss of consciousness of unspecified duration | ICD-9-D-850.5 |
| Concussion unspecified | ICD-9-D-850.9 |
aICD-9, International Classification of Diseases–9th Revision.
TABLE A2.
Humana Patient Populationa
| No. of Patients | |
|---|---|
| Year | |
| 2007 | 2,499,976 |
| 2008 | 2,551,535 |
| 2009 | 2,260,750 |
| 2010 | 2,275,816 |
| 2011 | 2,356,233 |
| 2012 | 2,558,379 |
| 2013 | 2,803,778 |
| 2014 | 3,617,599 |
| Age group, y | |
| <5 | 782,505 |
| 5-9 | 526,099 |
| 10-14 | 515,240 |
| 15-19 | 516,331 |
| 20-24 | 593,143 |
| 25-29 | 753,331 |
| 30-34 | 802,749 |
| 35-39 | 862,326 |
| 40-44 | 987,374 |
| 45-49 | 1,149,707 |
| 50-54 | 1,328,665 |
| 55-59 | 1,384,879 |
| 60-64 | 1,365,498 |
| Sex | |
| Female | 4,697,125 |
| Male | 4,131,123 |
aAll patients were younger than 65 years.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–e556. [DOI] [PubMed] [Google Scholar]
- 2. Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers’ Association position statement: management of sport concussion. J Athl Train. 2014;49:245–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brown JA, Dalecki M, Hughes C, Macpherson AK, Sergio LE. Cognitive-motor integration deficits in young adult athletes following concussion. BMC Sports Sci Med Rehabil. 2015;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cancelliere C, Hincapié CA, Keightley M, et al. Systematic review of prognosis and return to play after sport concussion: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(suppl):S210–S229. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years—United States, 2001-2009. MMWR Morb Mortal Wkly Rep. 2011;60:1337–1342. [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. CDC grand rounds: reducing severe traumatic brain injury in the United States. MMWR Morb Mortal Wkly Rep. 2013;62:549–552. [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Traumatic brain injury. 2014. http://www.cdc.gov/traumaticbraininjury. Accessed September 15, 2015.
- 8. Coronado VG, Haileyesus T, Cheng TA, et al. Trends in sports- and recreation-related traumatic brain injuries treated in US emergency departments: the National Electronic Injury Surveillance System–All Injury Program (NEISS-AIP) 2001-2012. J Head Trauma Rehabil. 2015;30:185–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dean PJ, Sato JR, Vieira G, McNamara A, Sterr A. Long-term structural changes after mTBI and their relation to post-concussion symptoms [published online June 11, 2015]. Brain Inj. doi:10.3109/02699052.2015.1035334 [DOI] [PubMed] [Google Scholar]
- 10. Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr. 2015;169:659–665. [DOI] [PubMed] [Google Scholar]
- 11. Ellis MJ, Ritchie LJ, Koltek M, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. 2015;16:709–718. [DOI] [PubMed] [Google Scholar]
- 12. Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci. 2015;66(pt B):75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2014;75(suppl 4):S24–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250–2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47:15–26. [DOI] [PubMed] [Google Scholar]
- 16. Hart J, Jr, Kraut MA, Womack KB, et al. Neuroimaging of cognitive dysfunction and depression in aging retired National Football League players: a cross-sectional study. JAMA Neurol. 2013;70:326–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Iverson GL, Brooks BL, Collins MW, Lovell MR. Tracking neuropsychological recovery following concussion in sport. Brain Inj. 2006;20:245–252. [DOI] [PubMed] [Google Scholar]
- 18. Kayani NA, Homan S, Yun S, Zhu BP. Health and economic burden of traumatic brain injury: Missouri, 2001-2005. Public Health Rep. 2009;124:551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kerr ZY, Marshall SW, Harding HP, Jr, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 2012;40:2206–2212. [DOI] [PubMed] [Google Scholar]
- 20. Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39:958–963. [DOI] [PubMed] [Google Scholar]
- 21. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40:747–755. [DOI] [PubMed] [Google Scholar]
- 22. Marin JR, Weaver MD, Yealy DM, Mannix RC. Trends in visits for traumatic brain injury to emergency departments in the United States. JAMA. 2014;311:1917–1919. [DOI] [PubMed] [Google Scholar]
- 23. Marras C, Hinca, pié CA, Kristman VL, et al. Systematic review of the risk of Parkinson’s disease after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(suppl):S238–S244. [DOI] [PubMed] [Google Scholar]
- 24. McCrory P, Meeuwisse W, Aubry M, et al. Consensus Statement on Concussion in Sport—the 4th International Conference on Concussion on Sport held in Zurich, November 2012. Clin J Sport Med. 2013;23:89–117. [DOI] [PubMed] [Google Scholar]
- 25. McCrory P, Meeuwisse WH, Kutcher JS, Jordan BD, Gardner A. What is the evidence for chronic concussion-related changes in retired athletes: behavioural, pathological and clinical outcomes? Br J Sports Med. 2013;47:327–330. [DOI] [PubMed] [Google Scholar]
- 26. Miller JH, Gill C, Kuhn EN, et al. Predictors of delayed recovery following pediatric sports-related concussion: a case-control study. J Neurosurg Pediatr. 2016;17:491–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mitka M. Reports of concussions from youth sports rise along with awareness of the problem. JAMA. 2010;304:1775–1776. [DOI] [PubMed] [Google Scholar]
- 28. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15:589–598. [DOI] [PubMed] [Google Scholar]
- 29. The National Collegiate Athletic Association. Probability of competing in sports beyond high school. http://www.ncaa.org/about/resources/research/probability-competing-beyond-high-school. Accessed October 5, 2015.
- 30. National Highway Traffic Safety Administration. Traffic Safety Facts. http://www-nrd.nhtsa.dot.gov/Pubs/811172.pdf. Accessed October 5, 2015.
- 31. O’Kane JW, Spieker A, Levy MR, Neradilek M, Polissar NL, Schiff MA. Concussion among female middle-school soccer players. JAMA Pediatr. 2014;168:258–264. [DOI] [PubMed] [Google Scholar]
- 32. Piercy KL, Dorn JM, Fulton JE, et al. Opportunities for public health to increase physical activity among youths. Am J Public Health. 2015;105:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005-2006 to 2011-2012. Am J Sports Med. 2014;42:1710–1715. [DOI] [PubMed] [Google Scholar]
- 34. Sambasivan K, Grilli L, Gagnon I. Balance and mobility in clinically recovered children and adolescents after a mild traumatic brain injury. J Pediatr Rehabil Med. 2015;8:335–344. [DOI] [PubMed] [Google Scholar]
- 35. Sarmiento K, Hoffman R, Dmitrovsky Z, Lee R. A 10-year review of the Centers for Disease Control and Prevention’s Heads Up initiatives: bringing concussion awareness to the forefront. J Safety Res. 2014;50:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015;31:2307–2313.e2. [DOI] [PubMed] [Google Scholar]
- 37. Slobounov S, Cao C, Sebastianelli W, Slobounov E, Newell K. Residual deficits from concussion as revealed by virtual time-to-contact measures of postural stability. Clin Neurophysiol. 2008;119:281–289. [DOI] [PubMed] [Google Scholar]
- 38. Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PM R. 2011;3(suppl 2):S460–S467. [DOI] [PubMed] [Google Scholar]
- 39. Theadom A, Parag V, Dowell T, et al. Persistent problems 1 year after mild traumatic brain injury: a longitudinal population study in New Zealand. Br J Gen Pract. 2016;66:e16–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 41. US Department of Health and Human Services. Physical Activity Guidelines for Americans Midcourse Report: Strategies to Increase Physical Activity Among Youth. Washington, DC: US Department of Health and Human Services; 2012. [Google Scholar]
- 42. Wood RL, Rutterford NA. Long-term effect of head trauma on intellectual abilities: a 16-year outcome study. J Neurol Neurosurg Psychiatry. 2006;77:1180–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhang AL, Kreulen C, Ngo SS, Hame SL, Wang JC, Gamradt SC. Demographic trends in arthroscopic SLAP repair in the United States. Am J Sports Med. 2012;40:1144–1147. [DOI] [PubMed] [Google Scholar]
- 44. Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29:623–639. [DOI] [PubMed] [Google Scholar]
- 45. Zonfrillo MR, Kim KH, Arbogast KB. Emergency department visits and head computed tomography utilization for concussion patients from 2006 to 2011. Acad Emerg Med. 2015;22:872–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zuckerman SL, Kerr ZY, Yengo-Kahn A, Wasserman E, Covassin T, Solomon GS. Epidemiology of sports-related concussion in NCAA athletes from 2009-2010 to 2013-2014: incidence, recurrence, and mechanisms. Am J Sports Med. 2015;43:2654–2662. Erratum in: Am J Sports Med. 2016;44:NP5. [DOI] [PubMed] [Google Scholar]