Abstract
Background:
Current risk stratification of idiopathic dilated cardiomyopathy (IDC) lacks sufficient sensitivity and specificity. The objective of this study was to investigate the predictive role of frontal QRS-T angles in IDC.
Methods:
A prospective study with 509 IDC patients was performed from February 2008 to December 2013 in the Affiliated Drum Tower Hospital, Nanjing University School of Medicine. Baseline values and changes in QRS-T angles were recorded. Follow-up was conducted every 6 months. Analyses by Cox Proportional Hazards model were performed to evaluate the association between QRS-T angle and outcomes. The primary outcome of interest was all-cause mortality.
Results:
During a median follow-up of 34 months, 90 of 316 patients with QRS-T angles >90° died compared to 31 of 193 patients with QRS-T angles ≤90° (hazard ratio [HR] =2.4, P < 0.001). Cardiac death was more prevalent in patients with a wide QRS-T angle (HR = 2.4, P < 0.001), similar to heart failure rehospitalization (HR = 2.5, P < 0.001). After adjustment for potential prognostic factors, the QRS-T angle was independently associated with all-cause mortality (HR = 2.5, P < 0.05), cardiac mortality (HR = 1.9, P < 0. 05), and heart failure rehospitalization (HR = 2.3, P < 0.01). Optimized therapy significantly narrowed the frontal QRS-T angle (100.9 ± 53.4° vs. 107.2 ± 54.4°, P < 0.001). The frontal QRS-T angle correlated well with established risk factors, such as left ventricular ejection fraction, brain natriuretic peptide, and New York Heart Association functional class.
Conclusions:
The frontal QRS-T angle is a powerful predictor of all-cause mortality, cardiac mortality, and worsening heart failure in IDC patients, independent of well-established prognostic factors. Optimized therapy significantly narrows the QRS-T angle, which might be an indicator of medication compliance, but this requires further investigation.
Keywords: Electrocardiography, Frontal QRS-T Angle, Idiopathic Dilated Cardiomyopathy, Prognosis
INTRODUCTION
Idiopathic dilated cardiomyopathy (IDC) remains the third most common cause of heart failure behind coronary artery disease and hypertension. The incidence of IDC is 5.5 cases per 100,000 per year, and the prevalence is 36 cases per 100,000 people, which greatly increases medical and social burdens.[1,2] The annual mortality rate ranges from 10% to 13% after the diagnosis of IDC is established.[3] Despite remarkable progress in pharmacological therapies, particularly the use of beta-blockers and angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), and device implantation, considerable morbidity and mortality of IDC patients remain a challenge for physicians. An effective risk stratification technique might improve the management of IDC patients. Currently, numerous clinical covariates have been well-documented to predict the prognosis of dilated cardiomyopathy (DCM) patients. These include advanced age, protodiastolic gallop, ventricular arrhythmia, and more commonly used parameters such as left ventricular ejection fraction (LVEF), QRS duration, and New York Heart Association (NYHA) functional class.[4,5,6] Several factors are widely used in routine practice. For example, LVEF is the key determinant of device implantation to primarily prevent sudden cardiac death (SCD) according to the latest guidelines.[7] However, large risk stratification challenges remain due to insufficient sensitivity and specificity of these known predictors.
Attention has recently focused on QRS-T angles, which address the deviations between ventricular depolarization and repolarization.[8] The spatial QRS-T angle shows its predictive value in the general population and certain clinical patients, but research and utility are limited because of the inconvenience of its acquisition from the standard 12-lead electrocardiogram (ECG). Instead, the frontal QRS-T angle is easy to obtain by visually reviewing the ECG report. The significance of the frontal QRS-T angle has rarely been studied in DCM patients, except in one study of nonischemic DCM (NIDCM) with a relatively mixed population and a majority of white and black patients.[9] The NIDCM population is a relatively mixed population because the etiology of DCM in this population is varied, including primary valvular diseases and myocarditis, which compromise the detection power of the frontal QRS-T angle in a more specific IDC population. Therefore, we conducted a prospective study to investigate the long-term predictive information from frontal QRS-T angles in Chinese patients with homogenous IDC.
METHODS
Patients
The study enrolled 509 consecutive patients with IDC admitted to a tertiary hospital (Affiliated Drum Tower Hospital, Nanjing University School of Medicine) between February 2008 and December 2013. All demographic information and clinical history were obtained by thorough communication. All patients underwent careful physical examination, 12-lead ECG, chest radiography, and echocardiography, on which the diagnosis of DCM was based. The diagnosis of IDC was largely made according to the definition of the World Health Organization/International Society and Federation of Cardiology Task Force[10] and was restricted to patients with LVEF <45%. Because ventricular pacing can change the morphology and polarity of QRS and T waves and, thus, affect the frontal QRS-T angle, we excluded patients with a permanent pacemaker, including cardiac resynchronization therapy. All patients had a minimum duration of 6 months since symptom onset. At the day of discharge, a 12-lead ECG examination was reperformed on each patient to evaluate the frontal QRS-T angle change after optimized therapy. The Local Ethics Committee approved this study, and informed consistent was obtained from all patients. The study was conducted according to the principles of the Declaration of Helsinki.
Electrocardiogram, 24-h electrocardiogram, and echocardiography
A 12-lead ECG was recorded for all patients at admission, discharge, and rehospitalization using the ECG-1350p machine (Nihon Kohden Corp., Tokyo, Japan). The ECG recorded at admission was used to estimate the frontal QRS-T angles for prognostic analysis. A paper speed of 25 mm/s and a voltage of 1 mV/10 mm were applied. The PR interval, QRS duration, and QT interval were measured as previously described.[11] QT intervals corrected for heart rates were generated using the Bazett's formula. The presence or absence of left bundle branch block (LBBB) and right bundle branch block was determined by two experienced cardiologists. Electrocardiographic reports of the P-wave axis, QRS axis, and T-wave axis were manually checked, and the frontal QRS-T angle was calculated as the absolute value of the difference between QRS and T wave axes.
Twenty-four hour ECG recordings were performed in 313 patients. During the examination, daily-intensity activities were encouraged. Nonsustained ventricular tachycardia (NSVT) was defined as more than three consecutive beats of ventricular prematurely. The number of NSVT in 24 h was calculated, as well as that of premature ventricular complexes (PVC).
Echocardiography was performed in all patients with the iE33 xMATRIX echo system (Philips, Eindhoven, the Netherlands) and was reviewed by experienced operators who were blind to the ECG results and clinical status of patients. Standard apical four- and two-chamber and long axis views were used. Baseline left ventricular end-diastolic diameter (LVEDd), left ventricular end-systolic diameter, left atrial diameter, interventricular septum thickness, left ventricular posterior wall thickness, LVEF, and pulmonary arterial pressure were calculated according to the American Society of Echocardiography.[12]
Follow-up and endpoints
Follow-up was conducted every 6 months through telephone interviews and medical records. The primary endpoint was all-cause death. Two additional secondary endpoints were also defined as follows: (1) cardiac death, including sudden death and death from worsening heart failure and (2) rehospitalization due to decompensated heart failure. An investigator (Jian-Zhou Chen) who was blind to the ECG results and clinical status performed the clinical outcome data collection.
Statistical analysis
Baseline characteristics stratified by the dichotomous presence or absence of a frontal QRS-T angle >90° were available for all patients. The cutoff of 90° was applied in our study based on results of numerous published studies.[9,13,14] Categorical data were expressed as number (percentage) whereas continuous data were presented as the mean ± standard deviation (SD) or median (interquartile range, IQR) where appropriate. Categorical variables were compared by Chi-square test, and continuous variables were compared by unpaired Student's t-test or the Mann-Whitney U test. Survival analyses were performed for all three endpoints. Survival curves were estimated by the Kaplan-Meier method and compared with the log-rank test. The associations between baseline covariates and each endpoint were first tested by a univariate Cox proportional hazards model, and variables with P < 0.05 were entered into the multivariable model to identify independent predictors for each endpoint. The results for both univariate and multivariable analyses were reported as hazard ratios (HRs) and 95% confidence intervals (CIs). Changes in frontal QRS-T angles from admission to discharge were assessed by Wilcoxon match-pairs analysis. The correlation between frontal QRS-T angle and well-established risk factors (LVEF, brain natriuretic peptide [BNP], and NYHA functional class) were analyzed by Spearman correlation test. All analyses were conducted using the statistical software SPSS version 17.0 (Chicago, IL, USA). A two-tailed P < 0.05 was considered statistically significant.
RESULTS
A total of 532 consecutive patients met the inclusion criteria. Twenty-three patients (4.3%) were lost to follow-up; therefore, complete follow-up was obtained in 509 (95.7%) patients. The mean age was 63 ± 16 years, LVEF was 33 ± 8%, and NYHA functional class ≥III was 71% [Table 1]. The mean QRS-T angle was 107 ± 54°. One hundred ninety-three (37.9%) patients had a QRS-T angle ≤90°, and 316 patients (62.1%) had a QRS-T angle >90°. Compared to patients with QRS-T angles ≤90°, patients with wide angles were more likely to have diabetes, more severe symptomatic heart failure (HF) evidenced by a higher NYHA functional class rating, longer symptom duration, a lower LVEF, a higher LVEDd and a higher BNP level, coupled with higher rates of loop diuretic and aldosterone antagonist treatments. Consistently, a lower beta-blocker treatment rate was observed in patients with wide QRS-T angles. In addition, patients with QRS-T angles >90° had a longer PR interval, QRS duration, and QT interval and higher T-wave axis and leftward QRS axis. A higher percentage of LBBB and higher numbers of PVC and NSVT were also observed.
Table 1.
Baseline characteristics stratified by QRS-T angle
| Items | All patients (n = 509) | QRS-T angle ≤90° (n = 193) | QRS-T angle >90° (n = 316) | Statistical value | P |
|---|---|---|---|---|---|
| Age (years) | 63 ± 16 | 63 ± 18 | 64 ± 15 | −0.207* | 0.836 |
| Male | 338 (66) | 133 (69) | 205 (65) | 0.876† | 0.349 |
| Current smoker | 147 (29) | 52 (27) | 95 (30) | 0.568† | 0.467 |
| Diabetes mellitus | 116 (23) | 32 (17) | 84 (27) | 6.812† | 0.009 |
| Hypertension | 195 (38) | 77 (40) | 118 (37) | 0.331† | 0.565 |
| Atrial fibrillation | 150 (29) | 60 (31) | 90 (28) | 0.392† | 0.531 |
| Duration of CHF >1 (years) | 277 (54) | 88 (46) | 189 (60) | 9.760† | 0.002 |
| Clinical variables | |||||
| NYHA class ≥III | 360 (71) | 117 (61) | 243 (77) | 15.333† | <0.001 |
| Beta-blockers | 369 (72) | 152 (79) | 217 (69) | 6.112† | 0.013 |
| ACEI/ARB | 427 (84) | 173 (90) | 254 (80) | 7.598† | 0.006 |
| Loop diuretics | 434 (85) | 151 (78) | 283 (90) | 12.218† | <0.001 |
| Spironolactone | 370 (73) | 125 (65) | 245 (78) | 9.835† | 0.002 |
| Digoxin | 226 (44) | 87 (45) | 139 (44) | 0.058† | 0.810 |
| Aspirin | 186 (37) | 70 (36) | 116 (37) | 0.010† | 0.920 |
| Warfarin | 47 (9) | 25 (13) | 22 (7) | 5.132† | 0.023 |
| Amiodarone | 26 (5) | 12 (6) | 14 (4) | 0.790† | 0.374 |
| Systolic blood pressure (mmHg) | 125 ± 20 | 127 ± 18 | 125 ± 21 | 0.983* | 0.326 |
| Diastolic blood pressure (mmHg) | 78 ± 13 | 79 ± 13 | 78 ± 13 | 0.796* | 0.426 |
| Heart rate (beats/min) | 77 ± 22 | 76 ± 21 | 77 ± 23 | −0.510* | 0.610 |
| ICD | 56 (11) | 14 (7) | 42 (13) | 4.460† | 0.035 |
| ECG parameters | |||||
| PR interval (ms) | 181 ± 43 | 174 ± 40 | 185 ± 45 | −2.325* | 0.025 |
| QRS duration (ms) | 119 ± 31 | 109 ± 28 | 125 ± 32 | −5.273* | <0.001 |
| QT interval (ms) | 401 ± 54 | 392 ± 48 | 406 ± 56 | −2.867* | 0.004 |
| QTc (ms) | 438 ± 44 | 429 ± 37 | 443 ± 47 | −3.557* | <0.001 |
| P-wave axis (°) | 46 (30–61) | 46 (30–61) | 47 (30–61) | −0.028‡ | 0.978 |
| QRS axis (°) | 5 (−33 to 46) | 28.5 (−1.5 to 58.0) | −12 (−43 to 36) | –6.056‡ | <0.001 |
| T-wave axis (°) | 90 (47–150) | 59 (19–90) | 116 (90–166) | −9.792‡ | <0.001 |
| QRS-T angle (°) | 107 ± 54 | 45 ± 25 | 145 ± 25 | −42.165* | <0.001 |
| Any bundle branch block | 194 (38) | 49 (25) | 145 (46) | 21.343† | <0.001 |
| LBBB | 153 (30) | 32 (17) | 121 (38) | 33.250† | <0.001 |
| RBBB | 40 (8) | 17 (9) | 23 (7) | 0.387† | 0.534 |
| 24-h ECG recording | |||||
| PVC | 495 (38–2449) | 154 (14–2242) | 629 (79–2679) | −2.533‡ | 0.049 |
| NSVT | 3 (4–37) | 1 (0–19) | 4 (7–61) | −1.928‡ | 0.041 |
| Echocardiography | |||||
| LVEF (%) | 33 ± 8 | 36 ± 8 | 31 ± 7 | 6.643* | <0.001 |
| LVEDd (cm) | 6.7 ± 0.8 | 6.6 ± 0.8 | 6.8 ± 0.8 | −3.432* | 0.001 |
| LVEDs (cm) | 5.7 ± 1.9 | 5.7 ± 2.9 | 5.7 ± 0.9 | −0.299* | 0.765 |
| LAD (cm) | 4.90 (4.40–5.40) | 4.9 ± 0.8 | 5.00 (4.40–5.50) | −1.535‡ | 0.125 |
| Interventricular septum (cm) | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.9 ± 1.0 | 0.341* | 0.733 |
| Posterior wall (cm) | 0.85 (0.80–0.94) | 0.90 ± 0.10 | 0.85 (0.79–0.95) | −0.456‡ | 0.648 |
| PAP (mmHg) | 48 ± 12 | 45 ± 13 | 49 ± 12 | −2.524* | 0.012 |
| Laboratory examination | |||||
| Creatinine (mg/L) | 800 (670–1000) | 790 (630–930) | 810 (680–1040) | −1.950‡ | 0.038 |
| Hemoglobin (10−4×mg/L) | 132 ± 22 | 133 ± 22 | 132 ± 22 | 0.211* | 0.833 |
| Sodium (mmol/L) | 142 ± 3 | 142 ± 3 | 142 ± 4 | 0.178* | 0.859 |
| BNP (10−6×mg/L) | 672 (312–1495) | 463 (156–1060) | 786 (406–1535) | −4.556‡ | <0.001 |
Data were presented as n (%), mean ± SD, or median (IQR). *t value; †χ2 value; ‡Z value. P values were from comparisons between patients with QRS-T angles ≤90°and >90°. CHF: Congestive heart failure; NYHA: New York Heart Association; ACEI: Angiotensin-converting enzyme inhibitor; ARB: Angiotensin receptor blocker; BNP: B-type natriuretic peptide; ICD: Implantable cardioverter-defibrillator; QTc: Corrected QT; LBBB: Left bundle branch block; RBBB: Right bundle branch block; PVC: Premature ventricular complexes; NSVT: Nonsustained ventricular tachycardia; LVEF: Left ventricular ejection fraction; LVEDd: Left ventricular end-diastolic diameter; LVEDs: Left ventricular end-systolic diameter; LAD: Left atrial diameter; PAP: Pulmonary arterial pressure; SD: Standard deviation; IQR: Interquartile range; 1 mmHg = 0.133 kPa.
All-cause mortality
During a median follow-up period of 34 months, 121 deaths were recorded. Ninety of 316 patients (28.5%) with a QRS-T angle >90° reached the primary endpoint compared to 31 of 193 patients (16.1%) with a QRS-T angle ≤90° [HR: 2.4; 95% CI: 1.5 – 3.6, P < 0.001; Figure 1a, and Tables 2 and 3]. After multivariable Cox regression analysis, the QRS-T angle >90° remained the most remarkable and significant independent predictor of all-cause mortality [HR: 2.5, 95% CI: 1.2–5.1, P < 0.05; Tables 2 and 4]. Other variables independently associated with all-cause mortality were NYHA functional class (HR: 1.8, 95% CI: 1.2 – 2.6, P < 0.01), age (HR: 1.013, 95% CI: 1.002–1.024, P < 0.05), QRS interval (HR: 1.011, 95% CI: 1.003–1.019, P < 0.01), and the use of ACEI/ARB (HR: 0.52, 95% CI: 0.30–0.92, P < 0.05).
Figure 1.
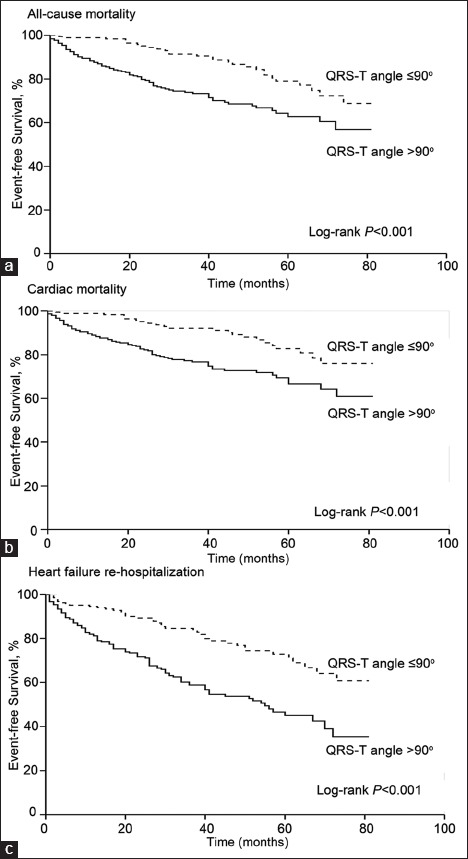
Kaplan-Meier curves for each endpoint according to frontal QRS-T angle. All-cause mortality (a), cardiac mortality (b), and heart failure rehospitalization (c) were presented, respectively. Survival curves were significantly different between QRS-T angle >90° and ≤90° for all endpoints.
Table 2.
Summary of outcome data regarding QRS-T angle
| Items | QRS-T angle ≤90° (%) | QRS-T angle >90° (%) | HR (95% CI) | Adjusted HR (95% CI) |
|---|---|---|---|---|
| All-cause mortality | 31/193 (16.1) | 90/316 (28.5) | 2.4 (1.5–3.6) | 2.5 (1.2–5.1) |
| Cardiac mortality | 25/193 (13.0) | 79/316 (25.0) | 2.4 (1.5–3.9) | 1.9 (1.0–3.5) |
| Heart failure rehospitalization | 41/193 (21.2) | 126/316 (39.9) | 2.5 (1.7–3.5) | 2.3 (1.3–4.2) |
Data were presented as n/N (%) or 95% CI. HR: Hazard ratio; CI: Confidence interval.
Table 3.
HRs for all-cause mortality in univariate analyses
| Items | HR (95% CI) | β coefficient | P |
|---|---|---|---|
| QRS-T angle | 2.365 (1.542–3.628) | 0.861 | <0.001 |
| Age | 1.011 (1.003–1.019) | 0.029 | 0.009 |
| Gender | 1.439 (0.987–2.097) | 0.356 | 0.058 |
| Current smoker | 1.019 (0.684–1.516) | 0.367 | 0.927 |
| Diabetes mellitus | 1.471 (0.985–2.196) | 0.406 | 0.059 |
| Atrial fibrillation | 1.529 (1.063–2.199) | 0.544 | 0.221 |
| Heart rate | 0.996 (0.987–1.006) | −0.004 | 0.442 |
| NYHA | 1.872 (1.432–2.447) | 0.605 | <0.001 |
| Beta-blockers | 0.471 (0.325–0.681) | −0.776 | <0.001 |
| ACEI/ARB | 0.486 (0.317–0.744) | −0.825 | 0.001 |
| Loop diuretics | 1.417 (0.795–2.525) | 0.287 | 0.237 |
| Spironolactone | 1.239 (0.805–1.908) | 0.095 | 0.330 |
| Digoxin | 1.075 (0.745–1.550) | 0.348 | 0.701 |
| Aspirin | 0.858 (0.580–1.269) | −0.043 | 0.443 |
| Warfarin | 0.653 (0.304–1.403) | −0.053 | 0.275 |
| Amiodarone | 0.517 (0.190–1.404) | −0.337 | 0.196 |
| Systolic blood pressure | 0.991 (0.981–1.001) | −0.005 | 0.085 |
| Diastolic blood pressure | 0.986 (0.971–1.001) | −0.006 | 0.071 |
| PR interval | 1.005 (1.000–1.010) | 0.005 | 0.053 |
| QRS interval | 1.011 (1.006–1.017) | 0.011 | <0.001 |
| QTc | 1.005 (1.000–1.009) | 0.005 | 0.043 |
| P-wave axis | 0.999 (0.993–1.005) | −0.001 | 0.712 |
| QRS axis | 1.002 (0.998–1.005) | 0.002 | 0.331 |
| T-wave axis | 1.001 (0.998–1.003) | 0.000 | 0.557 |
| LBBB | 1.809 (1.244–2.631) | 0.615 | 0.002 |
| RBBB | 1.546 (1.047–2.926) | 0.670 | 0.053 |
| PVC | 1.000 (1.000–1.000) | 0.000 | 0.886 |
| NSVT | 1.001 (0.763–1.374) | −0.011 | 0.913 |
| LVEF | 0.967 (0.944–0.991) | −0.044 | 0.008 |
| LVEDd | 1.129 (0.892–1.430) | 0.162 | 0.039 |
| LAD | 1.040 (1.007–1.097) | −0.003 | 0.626 |
| BNP | 1.000 (1.000–1.001) | 0.000 | <0.001 |
| Creatinine | 1.006 (0.922–1.016) | −0.002 | 0.054 |
| Sodium | 0.904 (0.856–0.954) | 0.025 | 0.066 |
Variables with a P<0.05 were entered into the multivariable model. HR: Hazard ratio; CI: Confidence interval; NYHA: New York Heart Association; ACEI: Angiotensin-converting enzyme inhibitor; ARB: Angiotensin receptor blocker; QTc: Corrected QT; LBBB: Left bundle branch block; RBBB: Right bundle branch block; PVC: Premature ventricular complexes; NSVT: Nonsustained ventricular tachycardia; LVEF: Left ventricular ejection fraction; LVEDd: Left ventricular end-diastolic diameter; LAD: Left atrial diameter; BNP: B-type natriuretic peptide.
Table 4.
HRs for all endpoints in multivariable analyses
| Items | HR (95% CI) | β coefficient | P |
|---|---|---|---|
| All-cause mortality | |||
| QRS-T angle | 2.453 (1.188–5.065) | 0.951 | 0.015 |
| NYHA | 1.780 (1.202–2.634) | 0.784 | 0.004 |
| Age | 1.013 (1.002–1.024) | 0.031 | 0.016 |
| QRS interval | 1.011 (1.003–1.019) | 0.017 | 0.008 |
| ACEI/ARB | 0.523 (0.299–0.915) | −0.607 | 0.023 |
| Cardiac mortality | |||
| QRS-T angle | 1.866 (1.004–3.468) | 1.024 | 0.049 |
| LBBB | 1.831 (1.126–2.976) | 0.687 | 0.015 |
| NYHA | 1.668 (1.108–2.510) | 0.508 | 0.014 |
| Age | 1.032 (1.013–1.052) | 0.032 | 0.001 |
| BNP | 1.000 (1.000–1.001) | 0.000 | 0.011 |
| Heart failure Rehospitalization | |||
| QRS-T angle | 2.321 (1.275–4.224) | 0.784 | 0.006 |
| BNP | 1.051 (1.013–1.079) | 0.000 | 0.008 |
P<0.05 indicates that this item is an independent predictor of the endpoint. HR: Hazard ratio; CI: Confidence interval; NYHA: New York Heart Association; ACEI: Angiotensin-converting enzyme inhibitor; ARB: Angiotensin receptor blocker; LBBB: Left bundle branch block; RBBB: Right bundle branch block; BNP: B-type natriuretic peptide.
Cardiac mortality
Of the 121 deaths, 104 (86.0%) were classified as cardiac deaths. A QRS-T angle >90° was associated with a significantly higher risk of cardiac death [25.0% vs. 13.0%; HR: 2.4, 95% CI: 1.5–3.9, P < 0.001; Figure 1b and Table 2]. This association remained significant after adjustment for other significant covariates in the univariate analysis [HR: 1.9, 95% CI: 1.0–3.5, P < 0.05; Tables 2 and 4]. LBBB (HR: 1.831, 95% CI: 1.126–2.976, P < 0.05), NYHA functional class (HR: 1.668, 95% CI: 1.108–2.510, P < 0.05), age (HR: 1.032, 95% CI: 1.013–1.052, P < 0.01), and BNP (HR: 1.000, 95% CI: 1.000–1.001, P < 0.05) were additional independent predictors of cardiac death in the multivariable model after controlling for other covariates [Table 4].
Heart failure rehospitalization
Rehospitalization due to decompensated heart failure occurred in 126 of 316 patients (39.9%) with a QRS-T angle >90° and 41 of 193 patients (21.2%) with a QRS-T angle ≤90° [HR: 2.5, 95% CI: 1.7–3.5, P < 0.001; Figure 1c and Table 2]. Following adjustment for other variables, the QRS-T angle >90° (HR: 2.321, 95% CI: 1.275–4.224, P < 0.01) and BNP (HR: 1.051, 95% CI: 1.013–1.079, P < 0.01) were independent predictors of heart failure rehospitalization [Table 4].
Stratified analysis
We also performed a subgroup analysis stratified by gender. The frontal QRS-T angle was a predictor of all-cause mortality following both univariate and multivariable analyses, exhibiting independent association with all-cause death in both men [HR: 2.29, 95% CI: 1.33–3.93, P < 0.01 for men; Figure 2a] and women [HR: 2.43, 95% CI: 1.21–4.90, P < 0.05 for women; Figure 2b].
Figure 2.
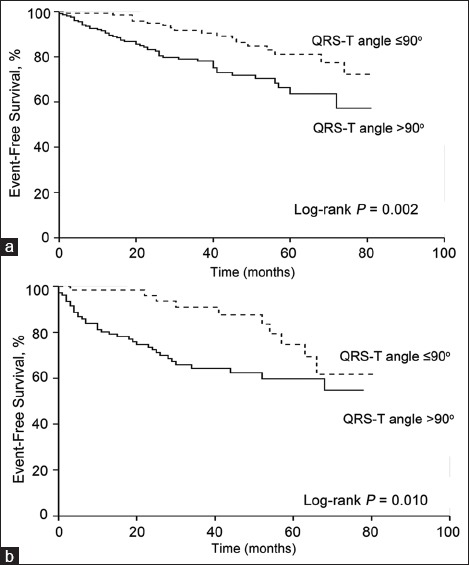
Kaplan-Meier curves for all-cause mortality stratified by gender. Significant difference was observed between QRS-T angle >90° and ≤90° in both men (a) and women (b) patients.
Other analyses
Following optimized therapy, QRS-T angles at the time of discharge were significantly decreased compared to those at admission (100.9 ± 53.4° vs. 107.2 ± 54.4°, P < 0.001 from Wilcoxon match-pairs analysis), which was more evident in patients with a wide QRS-T angle than that in patients with a narrow angle (−9.9 ± 17.5° vs. −1.1 ± 6.2°, P < 0.01). The correlation between QRS-T angle and well-established risk factors (LVEF, BNP, and NYHA functional class) were also evaluated. Overall, 167 patients rehospitalized in our center were included for analyses. A significant positive correlation was observed between the QRS-T angle and BNP level (P = 0.005), and a negative but significant correlation between the QRS-T angle and LVEF was also detected (P = 0.048).
DISCUSSION
In a large cohort of 509 patients with IDC, we demonstrated that the frontal QRS-T angle was associated with an increased risk of all-cause mortality and cardiac mortality. The association was independent of well-established predictors, such as age and NYHA functional class. Following multivariable analyses, the adjusted HRs for IDC patients with QRS-T angles >90° were 2.5 and 1.9 for all-cause mortality and cardiac mortality, respectively. For the first time, we also showed that wide QRS-T angles were significantly associated with worsening heart failure in IDC patients and that using optimized therapy during hospitalization, QRS-T angles were significantly narrowed in patients with wide angles.
The frontal QRS-T angle is readily available from routine 12-lead ECGs and reflects both ventricular depolarization and repolarization. Wide QRS-T angles might be associated with myocardial structure abnormalities and electrophysiological alterations and are always documented in patients with ischemia, cardiac hypertrophy, and other nonischemic cardiomyopathies. These structural and functional abnormalities might give patients a higher risk of ventricular arrhythmias and fatal cardiovascular events. Indeed, in our study, the incidence of ventricular ectopic rhythm, including PVC and NSVT on ambulatory monitoring, was higher in IDCM patients with wide QRS-T angles, as were total mortality and cardiac mortality.
The prognostic significance of the frontal QRS-T angle was first reported in the Atherosclerosis Risk in Communities study, which was a population-based multicenter study.[15] The frontal QRS-T angle was a strong predictor of total mortality, with >50% increased risk.[15] Since then, the frontal QRS-T angle has been intensively studied in various populations, including ischemic heart disease (IHD),[13] acute coronary syndrome,[16,17] NIDCM,[9] heart failure,[18] heart failure with preserved ejection fraction,[19] and the general population.[20,21] Most of these studies were performed in mixed cohorts. The heterozygous population of these studies limited the accuracy of the conclusions. To evaluate the predictive value of the frontal QRS-T angle in DCM, the study with the most homogeneous population was a post hoc analysis of the DEFINITE trial, which enrolled 458 patients with NIDCM.[9] Of note, the cohort of the DEFINITE study was not as homogeneous as that of our study because they enrolled all NIDCM patients with a variety of etiologies, such as primary valvular diseases and tachycardia-induced cardiomyopathy, which were all excluded in our study. To the best of our knowledge, the study is a rare prospective study designed to assess the prognostic significance of frontal QRS-T angle in IDC patients.
In our study, despite higher rates of ICD implantation, IDC patients with a QRS-T angle >90° had a poorer prognosis. Therefore, the significant prognostic value of the frontal QRS-T angle was further highlighted because device therapy is well-documented to improve outcomes in heart failure.[22,23] After adjustments for all potentially confounding factors, a QRS-T angle >90° increased the risk of mortality by 145% in IDC patients, which was higher than that in NIDCM patients from the DEFINITE study (by 64%)[9] and a meta-analysis in a highly mixed population,[24] whereas this mirrored that in the IHD population (by 140%)[13] and patients with acute myocardial infarction and reduced LVEF (by 118%).[17] Our study provides valuable insight into the prognostic implications of frontal QRS-T angle in IDC patients because of its excellent association with the primary and secondary endpoints and it outperforms all other conventional cardiovascular risk factors and well-established predictive factors. It is important and necessary to update the risk stratification method in DCM because of considerable morbidity and mortality.[25] The current risk stratification method heavily relies on the NYHA functional class and LVEF and is far from optimal. Particularly for the primary prevention of SCD in DCM with device implantation, LVEF is not specific or sensitive enough, missing many SCDs in patients with LVEF >35%,[26,27] and only a low rate of ventricular arrhythmias occurs in patients with ICD therapy after a long-term follow-up.[28] In addition, more than 5% patients receiving ICD develop severe device-related adverse events.[29] All these problems stress the need for more precise and effective risk stratification criteria. The potential effect of the QRS-T angle in risk stratification has also been supported by other studies: both high- and low-risk patients could be identified. Strauss et al.[30] combined the QRS-T angle with the QRS score and identified high-risk patients with 1-year mortality of 8.8–13.9%. In another study of patients with IHD, patients with QRS-T angle <100° had no event of ventricular arrhythmia during 2-year follow-up.[13] It has been commonly accepted that multivariate predictors significantly outperform individual factors in risk stratification;[24,26] therefore, we expect a comprehensive method combining numerous risk factors including the QRS-T angle to well determine whether a DCM patient is at higher risk.
A wide QRS-T angle is associated with worsening heart failure as first demonstrated in our study. This was evidenced by a higher rate of rehospitalization because of heart failure and because the QRS-T angle showed significant correlation with LVEF, BNP level and NYHA functional class although the mechanism remains unclear. However, the data showed that patients with a QRS-T angle >90° had significantly larger LVEDd, indicating more significant cardiac remodeling. This cardiac remodeling might have changed the direction of vectors of depolarization and repolarization, resulting in a widened QRS-T angle.[19] These findings further reinforce the concept that frontal QRS-T angle is a promising predictor for DCM.
Interestingly, in our current study, optimized pharmacotherapy and device implantation led to significantly narrowed frontal QRS-T angle in patients with a wide angle, which is a rare report in DCM. The QRS-T angle change might be a covariate to test whether a patient has good medication compliance in DCM, but other studies are warranted to explore this hypothesis.
Several limitations of our study should be acknowledged. First, this was an observational study conducted in a single center; therefore, the nature of the study design might cause bias. However, the sample size of our study was not small and was rigorously selected as a homogeneous cohort of IDC patients. We applied the multivariable Cox model to adjust for all potential confounders, and the prognostic significance of frontal QRS-T angle after adjustments was consistent with that before adjustment, which supported our conclusions. Second, the use of anticoagulation therapy was far inferior to the prevalence of atrial fibrillation in our cohort, which could also bias our results; however, endpoint verification showed that only four patients died from stroke. Therefore, this bias is unlikely to be large. Third, the use of beta-blockers and ACEI/ARB, both of which are clearly associated with the prognosis of IDC patients, was lower in patients with QRS-T angle >90° than those <90°. This might be explained by the observation that patients with wide QRS-T angles had more severe heart failure symptoms and might not be able to tolerate these drugs. We also performed multivariate analysis to adjust for these covariates.
In conclusion, the frontal QRS-T angle is a powerful predictor of all-cause mortality in patients with IDC, independent of well-established prognostic factors such as NYHA functional class, LBBB, age, BNP, and the use of ACEI/ARB. The frontal QRS-T angle also independently predicts the occurrence of cardiac mortality and heart failure rehospitalization. In addition, frontal QRS-T angle changes correlate well with LVEF, BNP, and NYHA class, and optimized therapy significantly narrows this angle, which might be an indicator of medication compliance, but this requires further investigation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Codd MB, Sugrue DD, Gersh BJ, Melton LJ., 3rd Epidemiology of idiopathic dilated and hypertrophic cardiomyopathy. A population-based study in Olmsted County, Minnesota 1975-1984. Circulation. 1989;80:564–72. doi: 10.1161/01.cir.80.3.564. doi: 10.1161/01.CIR.80.3.564. [DOI] [PubMed] [Google Scholar]
- 2.Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, et al. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006;296:1867–76. doi: 10.1001/jama.296.15.1867. doi: 10.1001/jama.296.15.1867. [DOI] [PubMed] [Google Scholar]
- 3.Konstam MA. Progress in heart failure management?Lessons from the real world. Circulation. 2000;102:1076–8. doi: 10.1161/01.cir.102.10.1076. doi: 10.1161/01.CIR.102.10.1076. [DOI] [PubMed] [Google Scholar]
- 4.Rihal CS, Nishimura RA, Hatle LK, Bailey KR, Tajik AJ. Systolic and diastolic dysfunction in patients with clinical diagnosis of dilated cardiomyopathy. Relation to symptoms and prognosis. Circulation. 1994;90:2772–9. doi: 10.1161/01.cir.90.6.2772. doi: 10.1161/01.CIR.90.6.2772. [DOI] [PubMed] [Google Scholar]
- 5.Shenkman HJ, Pampati V, Khandelwal AK, McKinnon J, Nori D, Kaatz S, et al. Congestive heart failure and QRS duration: Establishing prognosis study. Chest. 2002;122:528–34. doi: 10.1378/chest.122.2.528. doi: 10.1378/chest.122.2.528. [DOI] [PubMed] [Google Scholar]
- 6.Hombach V, Merkle N, Torzewski J, Kraus JM, Kunze M, Zimmermann O, et al. Electrocardiographic and cardiac magnetic resonance imaging parameters as predictors of a worse outcome in patients with idiopathic dilated cardiomyopathy. Eur Heart J. 2009;30:2011–8. doi: 10.1093/eurheartj/ehp293. doi: 10.1093/eurheartj/ehp.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239. doi: 10.1016/j.jacc.2013.05.019. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Macfarlane PW. The frontal plane QRS-T angle. Europace. 2012;14:773–5. doi: 10.1093/europace/eus057. doi: 10.1093/europace/eus057. [DOI] [PubMed] [Google Scholar]
- 9.Pavri BB, Hillis MB, Subacius H, Brumberg GE, Schaechter A, Levine JH, et al. Prognostic value and temporal behavior of the planar QRS-T angle in patients with nonischemic cardiomyopathy. Circulation. 2008;117:3181–6. doi: 10.1161/CIRCULATIONAHA.107.733451. doi: 10.1161/CIRCULATIONAHA.107.733451. [DOI] [PubMed] [Google Scholar]
- 10.Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation. 1996;93:841–2. doi: 10.1161/01.cir.93.5.841. doi: 10.1161/01.CIR.93.5.841. [DOI] [PubMed] [Google Scholar]
- 11.Pitzalis MV, Anaclerio M, Iacoviello M, Forleo C, Guida P, Troccoli R, et al. QT-interval prolongation in right precordial leads: An additional electrocardiographic hallmark of Brugada syndrome. J Am Coll Cardiol. 2003;42:1632–7. doi: 10.1016/j.jacc.2003.07.005. doi: 10.1016/j.jacc.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. doi: 10.1016/j.echo.2005.10.005. doi: 10.1016/j.euje.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 13.Borleffs CJ, Scherptong RW, Man SC, van Welsenes GH, Bax JJ, van Erven L, et al. Predicting ventricular arrhythmias in patients with ischemic heart disease: Clinical application of the ECG-derived QRS-T angle. Circ Arrhythm Electrophysiol. 2009;2:548–54. doi: 10.1161/CIRCEP.109.859108. doi: 10.1161/CIRCEP.109.859108. [DOI] [PubMed] [Google Scholar]
- 14.Vend N, McNitt S, Kutyifa V, Zareba W. Predictive value of a widened QRS-T angle and low AVR amplitude in patients with ischemic cardiomyopathy. Heart Rhythm. 2013;10:S110–1. [Google Scholar]
- 15.Zhang ZM, Prineas RJ, Case D, Soliman EZ, Rautaharju PM ARIC Research Group. Comparison of the prognostic significance of the electrocardiographic QRS/T angles in predicting incident coronary heart disease and total mortality (from the atherosclerosis risk in communities study) Am J Cardiol. 2007;100:844–9. doi: 10.1016/j.amjcard.2007.03.104. doi: 10.1016/j.amjcard.2007.03.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lown MT, Munyombwe T, Harrison W, West RM, Hall CA, Morrell C, et al. Association of frontal QRS-T angle –Age risk score on admission electrocardiogram with mortality in patients admitted with an acute coronary syndrome. Am J Cardiol. 2012;109:307–13. doi: 10.1016/j.amjcard.2011.09.014. doi: 10.1016/j.amjcard.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 17.Raposeiras-Roubín S, Virgós-Lamela A, Bouzas-Cruz N, López-López A, Castiñeira-Busto M, Fernández-Garda R, et al. Usefulness of the QRS-T angle to improve long-term risk stratification of patients with acute myocardial infarction and depressed left ventricular ejection fraction. Am J Cardiol. 2014;113:1312–9. doi: 10.1016/j.amjcard.2014.01.406. doi: 10.1016/j.amjcard.2014.01.406. [DOI] [PubMed] [Google Scholar]
- 18.Gotsman I, Keren A, Hellman Y, Banker J, Lotan C, Zwas DR. Usefulness of electrocardiographic frontal QRS-T angle to predict increased morbidity and mortality in patients with chronic heart failure. Am J Cardiol. 2013;111:1452–9. doi: 10.1016/j.amjcard.2013.01.294. doi: 10.1016/j.amjcard.2013.01.294. [DOI] [PubMed] [Google Scholar]
- 19.Selvaraj S, Ilkhanoff L, Burke MA, Freed BH, Lang RM, Martinez EE, et al. Association of the frontal QRS-T angle with adverse cardiac remodeling, impaired left and right ventricular function, and worse outcomes in heart failure with preserved ejection fraction. J Am Soc Echocardiogr. 2014;27:74–82.e2. doi: 10.1016/j.echo.2013.08.023. doi: 10.1016/j.echo.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aro AL, Huikuri HV, Tikkanen JT, Junttila MJ, Rissanen HA, Reunanen A, et al. QRS-T angle as a predictor of sudden cardiac death in a middle-aged general population. Europace. 2012;14:872–6. doi: 10.1093/europace/eur393. doi: 10.1093/europace/eur393. [DOI] [PubMed] [Google Scholar]
- 21.Whang W, Shimbo D, Levitan EB, Newman JD, Rautaharju PM, Davidson KW, et al. Relations between QRS |T angle, cardiac risk factors, and mortality in the third National Health and Nutrition Examination Survey (NHANES III) Am J Cardiol. 2012;109:981–7. doi: 10.1016/j.amjcard.2011.11.027. doi: 10.1016/j.amjcard.2011.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37. doi: 10.1056/NEJMoa043399. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 23.Desai AS, Fang JC, Maisel WH, Baughman KL. Implantable defibrillators for the prevention of mortality in patients with nonischemic cardiomyopathy: A meta-analysis of randomized controlled trials. JAMA. 2004;292:2874–9. doi: 10.1001/jama.292.23.2874. doi: 10.1001/jama.292.23.2874. [DOI] [PubMed] [Google Scholar]
- 24.Zhang X, Zhu Q, Zhu L, Jiang H, Xie J, Huang W, et al. Spatial/frontal QRS-T angle predicts all-cause mortality and cardiac mortality: A meta-analysis. PLoS One. 2015;10:e0136174. doi: 10.1371/journal.pone.0136174. doi: 10.1371/journal.pone.0136174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gulati A, Ismail TF, Jabbour A, Alpendurada F, Guha K, Ismail NA, et al. The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation. 2013;128:1623–33. doi: 10.1161/CIRCULATIONAHA.113.002518. doi: 10.1161/CIRCULATIONAHA.113.002518. [DOI] [PubMed] [Google Scholar]
- 26.Goldberger JJ, Subacius H, Patel T, Cunnane R, Kadish AH. Sudden cardiac death risk stratification in patients with nonischemic dilated cardiomyopathy. J Am Coll Cardiol. 2014;63:1879–89. doi: 10.1016/j.jacc.2013.12.021. doi: 10.1016/j.jacc.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 27.Adabag S, Smith LG, Anand IS, Berger AK, Luepker RV. Sudden cardiac death in heart failure patients with preserved ejection fraction. J Card Fail. 2012;18:749–54. doi: 10.1016/j.cardfail.2012.08.357. doi: 10.1016/j.cardfail.2012.08.357. [DOI] [PubMed] [Google Scholar]
- 28.Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, et al. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004;110:3760–5. doi: 10.1161/01.CIR.0000150390.04704.B7. doi: 10.1161/01.CIR.0000150390.04704.B7. [DOI] [PubMed] [Google Scholar]
- 29.Sweeney MO, Wathen MS, Volosin K, Abdalla I, DeGroot PJ, Otterness MF, et al. Appropriate and inappropriate ventricular therapies, quality of life, and mortality among primary and secondary prevention implantable cardioverter defibrillator patients: Results from the Pacing Fast VT REduces Shock ThErapies (PainFREE Rx II) trial. Circulation. 2005;111:2898–905. doi: 10.1161/CIRCULATIONAHA.104.526673. doi: 10.1161/CIRCULATIONAHA.104.526673. [DOI] [PubMed] [Google Scholar]
- 30.Strauss DG, Mewton N, Verrier RL, Nearing BD, Marchlinski FE, Killian T, et al. Screening entire health system ECG databases to identify patients at increased risk of death. Circ Arrhythm Electrophysiol. 2013;6:1156–62. doi: 10.1161/CIRCEP.113.000411. doi: 10.1161/CIRCEP.113.000411. [DOI] [PMC free article] [PubMed] [Google Scholar]


