Abstract
Background:
The previous studies agree that minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has better function outcomes, less blood loss, and shorter hospital stay, when compared to open-TLIF. However, there are no significance differences on operative time, complication, and reoperation rate between the two procedures. This could be from less relative literatures and lower grade evidence. The further meta-analysis is needed with more and higher grade evidences to compare the above two TLIF procedures.
Methods:
Prospective and retrospective studies that compared open-TLIF and MIS-TLIF were identified by searching the Medline, Embase, Web of Science, China National Knowledge Infrastructure, Wanfang, and VIP database (the literature search comprised Medical Subject Heading terms and key words or Emtree term). The retrieval time ranged from the date when the database was founded to January 2015. Pooled risk ratios (RRs) and weighted mean differences (WMDs) with 95% confidence intervals were calculated for the clinical outcomes and perioperative data.
Results:
Twenty-four studies (n = 1967 patients) were included in this review (n = 951, open-TLIF, n = 1016, MIS-TLIF). MIS-TLIF was associated with a significant decrease in the visual analog score (VAS)-back pain score (WMD = −0.44; P = 0.001), Oswestry Disabilities Index (WMD = −1.57; P = 0.005), early ambulation (WMD = −1.77; P = 0.0001), less blood loss (WMD = −265.59; P < 0.00001), and a shorter hospital stay (WMD = −1.89; P < 0.0001). However, there were no significant differences in the fusion rate (RR = 0.99; P = 0.34), VAS-leg pain (WMD = −0.10; P = 0.26), complication rate (RR = 0.84; P = 0.35), operation time (WMD = −5.23; P = 0.82), or reoperation rate (RR = 0.73; P = 0.32).
Conclusions:
MIS-TLIF resulted in a similar fusion rate with better functional outcome, less blood loss, shorter ambulation, and hospital stay; furthermore, it did not increase the complication or reoperation rate based on the existing evidence.
Keywords: Clinical Outcomes, Meta-analysis, Minimally Invasive Surgery, Transforaminal Lumbar Interbody Fusion
INTRODUCTION
In 1943, the open bilateral posterior lumbar interbody fusion procedure was proposed by Cloward.[1] This technique not only enables nerve root decompression but also interbody fusion from a single posterior approach.[2] The clinical outcomes were satisfying. However, to further reduce the risk of neurological complications, transforaminal lumbar interbody fusion (TLIF), which achieves an interbody fusion through a unilateral posterior process, has obtained popularity.[3] Since the introduction of TLIF by Harms and Rolinger, it has been used for treating multifarious lumbar degenerative disease.[4,5,6,7] TLIF results in higher rates of fusion compared with other interbody fusion approaches.[4] In 2003, Foley et al.[8] demonstrated that minimally invasive TLIF (MIS-TLIF) results in fewer muscle and tissue lesions compared with traditional open-TLIF; thus, this approach has a better outcome, although there are disadvantages.[4]
Meta-analyses that have compared open-TLIF and MIS-TLIF have indicated that MIS-TLIF is associated with better functional outcomes, less blood loss, and a shorter hospital stay compared with open-TLIF. However, both of these procedures had no significant effect on the fusion rate, operation time, complications, or reoperation rate. Moreover, there were several limitations such as a lower evidence level and a lack of important data in some studies.[4,5,6] Thus, we aimed to determine whether MIS-TLIF and open-TLIF had a significant effect on the fusion and complication rate with the technical development of the minimally invasive approach and the inclusion of additional studies. The question arose as to whether an updated meta-analysis would provide additional information and a higher clinic reference value. Thus, we aimed to provide an updated review of the literature to compare these two methods.
METHODS
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses.[9]
Literature search
The literature searches comprised Medical Subject Heading (MeSH) terms and key words in Medline: the MeSH term was degenerative intervertebral disc degeneration and the subheadings were surgery or therapy (n = 1146); the keywords combined “transforaminal lumbar interbody fusion” or “TLIF” with “MIS”, “minimally invasive”, or “minimally invasive spine surgery (n = 246)”. In Embase, the Emtree term included intervertebral disk degeneration and the subheadings were surgery or therapy (n = 929); the keywords combined “transforaminal lumbar interbody fusion” or “TLIF” with “MIS”, “minimally invasive”, or “minimally invasive spine surgery (n = 327)”. A web of science search was conducted by combining the keywords “transforaminal lumbar interbody fusion” or “TLIF” with “MIS”, “minimally invasive”, or “minimally invasive spine surgery (n = 386)”. In China National Knowledge Infrastructure (CNKI), Wanfang, and VIP database, the search was conducted using the keywords “minimally invasive, MIS” and “transforaminal lumbar interbody fusion (CNKI = 154, Wanfang = 168, and VIP = 59)”. A linguistic restriction was imposed on the search as recommended by the Cochrane Back Review Group editorial board.[10,11] The retrieval time ranged from the date when the database was founded to January 2015. To identify other relevant articles, the reference lists of the identified studies and review articles were also reviewed. Two reviewers independently screened all articles via the titles, abstracts, or full texts to determine the study inclusion. The authors and journals were known to the two reviewers. When different viewpoints occurred regarding a single study, a discussion ensued until a consensus was reached.
Study eligibility criteria
The inclusion criteria were as follows: (1) English and Chinese literature; (2) the study design was a comparative article (MIS-TLIF versus open-TLIF); (3) the article reported at least one clinic outcome or perioperative data; (4) the patients suffered from degenerative disc diseases (disc herniation, canal stenosis, or spondylolisthesis); isthmic spondylolisthesis was also included; (5) the sample size comprised at least ten patients for both groups; and (6) the full text was available. Reduplicated studies, case reports, cadaveric or biomechanical studies, non-English/Chinese articles, and patients treated via MIS-TLIF or open-TLIF for other diseases were excluded.
Data extraction
We obtained data from the included studies in the following categories: (1) authors and year of publication; (2) study design; (3) class of evidence; (4) total number of enrolled patients and number per group (MIS-TLIF and open-TLIF); (5) mean follow-up time; (6) follow-up time and rate (%); (7) mean age; (8) percentage of male and female patients; (9) diagnosis (divided into three categories: degenerative disc disease, spondylolisthesis, and others); (10) inclusion/exclusion criteria; (11) clinical outcomes; (12) perioperative data; (13) fusion definition and evaluation measure; (14) number of lumbar segments treated; (15) level of fusion (divided into L4–L5, L5–S1, and others); (16) use of grafts and types; (17) use of cages and types; (18) use of screw fixation and means; and (19) number of complications. We did not define complications in advance. Rather, the overall complications were collected.
Study quality
The study evidence class was determined using the Oxford Centre for Evidence-based Medicine-Levels of Evidence (March 2009). Good quality randomized controlled trials (RCTs) were considered Class I evidence. Moderate or poor quality RCT and good quality cohort studies were considered Class II evidence. Moderate or poor quality cohort studies and case–control studies were considered Class III evidence. Case series studies were considered Class IV evidence.[12] The articles were independently assessed by two reviewers, and discrepancies were resolved by discussion until a consensus was reached.
Statistical analysis
Continuous variables (Oswestry Disabilities Index [ODI], visual analog score [VAS], mean blood loss, length of stay, and operation time) were analyzed using weighted mean differences (WMDs) with the 95% confidence interval (CI). Dichotomous data (fusion rate, overall complication rate, and reoperation rate) were analyzed using the relative risk (RR) measure and 95% CI. The included studies were different in several variables such as the fusion definition, estimation of blood loss, VAS or ODI scale, surgical techniques, and patient conditions; thus, these variables were not the same for the overall studies within each group. Therefore, a random-effects model was more suited for this study because it enables a distribution in contrast to a fixed-effects model. All tests defined P < 0.05 as significant. Funnel plots were used to assess the publication bias. A symmetrical plot indicates no bias, whereas an asymmetric plot indicates publication bias [Supplementary Figure 1 (257.5KB, tif) ]. Further analysis of the database was conducted using Review Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Funnel plots: Complication rate. SE: Standard error; RR: Relative risk.
RESULTS
Selected studies and characteristics
The details of the search strategy and selection are shown in Figure 1. We identified 24 eligible, comparative cohort studies from 780 potential studies in the initial literature search by independently judging the titles, abstracts, and full texts of all potential studies. The eligible studies included one RCT, eight prospective, and 15 retrospective cohort studies.[13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] All included studies were written in English or Chinese, and the full text was available. Ten studies were excluded because they included data from patients in previously published studies[37,38,39,40,41,42,43,44,45,46] and seven studies were removed because the included diseases did not fulfill the inclusion criteria.[47,48,49,50,51,52,53] One study had three subgroups, which were grouped by the number of surgery segments. We included only the one segment group because the number of patients in the other groups did not meet the inclusion criteria.[20] There were 1967 patients in this study. There were 19 studies in which the diagnoses included degenerative disc disease; however, the diagnostic information was not clearly classified in two studies. Eighteen papers reported patients with only one segment surgery and one paper did not provide relevant information. The interbody device was used in all studies. All papers reported the use of bone graft information. Five of the included studies applied rhBMP-2.[13,14,15,23,30] The detailed information regarding these studies is shown in Table 1.
Figure 1.

Flow diagram for the selection of studies.
Table 1.
Characteristics of the include trials
| Characteristics | Wong et al.[25] | Sulaiman and Singh[30] | Tian et al.[31] | Singh et al.[18] | Zheng et al.[32] | Chu et al.[36] |
|---|---|---|---|---|---|---|
| Year of publication | 2014 | 2014 | 2014 | 2014 | 2014 | 2014 |
| Study design | Prospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort |
| Class of evidence* | III | III | III | III | III | III |
| Number of enrolled patient (MIS:open) | 198 (144:54) | 68 (57:11) | 61 (30:31) | 66 (33:33) | 48 (22:26) | 51 (15:36) |
| Mean follow-up time (months; MIS:open) | 45.0:46.0 | 24:24 | 25.63:25.63 | 6.0:6.0 | 12:12 | 13.6:13.6 |
| Follow-up rate (%, months) (MIS:open) | 100:100 (33) NR (>33) | 100:100 (12) NR (>12) | 100:100 (24) NR (>24) | 100:100 (6) | 100:100 (6) NR (>6) | 100:100 (6) NR (>6) |
| Mean age (years, MIS:open) | 61.0:58.0 | 61.1:56.4 | 48.21:48.90 | 51.7:49.9 | 49.4:50.7 | 53:53 |
| Gender (% male; MIS:open) | 42.4:46.3 | 30:36 | 53:74 | 69.7:63.6 | 31.8:42.3 | 66.7:66.7 |
| Diagnosis (MIS:open) | ||||||
| DDD | 27:10 | 27:25 | 19:9 | 22:21 | 15:36 | |
| Spondylolisthesis | 66:25 | 57:11 | 3:6 | 6:9 | 0:5 | |
| Others | 51:24 | 8:5 | ||||
| Inclusion/exclusion criteria | NR | Inclusion Evidence on magnetic resonance imaging of Grades I or II degenerative lumbar spondylolisthesis; Mechanical low back pain and radicular leg symptoms Lack of response to at least 6 weeks of conservative therapy Age 18–80 years Exclusion Patient had an active medical or worker’s compensation lawsuit or any pre-existing spinal pathology |
Inclusion Symptomatic degenerative disease of the lumbosacral spine (L2 to S1) No response to nonoperative treatments for 6 months Single-level involvement Exclusion Age <18 years or >65 years Previous lumbar surgery Osteoporosis spinal trauma or infections |
Inclusion Diagnosis of either lumbar DDD, degenerative spondylolisthesis, or spinal stenosis; Patients had failed conservative management, including medications, a minimum of 6 weeks of physical therapy, and epidural injections when indicated Exclusion Patients requiring 2 or more levels of fusion Who were undergoing revision surgeries |
Inclusion Symptomatic and refractory to prior conservative treatment for low back pain with or without unilateral leg pain Single-level DDD or degenerative I grade spondylolisthesis; Lack of response to at least 12 weeks of conservative therapy Exclusion Patients associated with previous spinal surgery, lumbar fracture, active infection, tumor, malformation Patients who have severe adjacent segment degeneration |
Inclusion Patients need to have evidence on magnetic resonance imaging of lumbar DDD, degenerative Have mechanical low back pain and radicular symptoms Unresponsive to at least 12 weeks of conservative therapy At least 6 months of follow-up Exclusion NR |
| Clinical outcome | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, ODI | OPT, MBL, LOS, complications, VAS, ODI, fusion rate, ambulation time | ORT, MBL, LOS, VAS | OPT, MBL, complications, VAS, ODI, JOA, fusion rate | OPT, MBL, LOS, complications, VAS, ODI, fusion rate |
| Definition fusion/evaluation measure | NR/dynamic flexion- extension lumbar radiographs in conjunction with a CT scan within the 16–24 months | NR | Grades I or II (Bridwell interbody fusion grading system)/radiographs (antero-posterior and lateral images) were employed to affirm the fusion rates and CT scans at 24 months | NR | Trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, and <4° segmental movement/dynamic flexion-extension lumbar radiographs in conjunction with a CT scan within the 24 months | Trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, and <4° segmental movement/dynamic flexion-extension lumbar radiographs |
| Surgical information | ||||||
| Number of segments treated | One (79:35) Two (55:21) | One (45:2) Two (12:9) | One (30:30) | One (33:33) | One (22:26) | One (15:36) |
| Level of fusion | ||||||
| L4–L5 | 62:14 | 37:8 | 14:17 | NR | 11:15 | NR |
| L5 to S1 | 65:21 | 12:9 | 14:13 | 11:10 | ||
| Others | 17:9 | 2:4 | 2:1 | 0:1 | ||
| Interbody device | PEEK cage | PEEK cage | PEEK/titanium cage | Cage | PEEK cage | Cage |
| Graft use | Autologous | Autologous | Autologous | Autologous | Autologous | Autologous |
| Screw use | Bilateral | Bilateral | Bilateral | Bilateral (O) | Bilateral | Bilateral |
| Unilateral (MI) | ||||||
| Characteristics | Parker et al.[17] | Saetia et al.[29] | Gu et al.[28] | Brodano et al.[27] | Zairi et al.[26] | Lau et al.[14] |
| Year of publication | 2013 | 2013 | 2013 | 2013 | 2013 | 2013 |
| Study design | Prospective cohort | Retrospective cohort | Prospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort |
| Class of evidence* | II | III | III | III | III | III |
| Number of enrolled patient (MIS:open) | 100 (50:50) | 24 (12:12) | 82 (44:38) | 64 (30:34) | 100 (40:60) | 127 (78:49) |
| Mean follow-up time (months; MIS:open) | 24:24 | 28:28 | 20.6:20.0 | 23:25 | 27.0:30.0 | NR |
| Follow-up rate (%, months) (MIS:open) | 100:100 (24) | 100:100 (24) NR (>24) | 100:100 (16) NR (>16) | 100:100 (12) NR (>12) | 100:100 (24) NR (>24) | NR |
| Mean age (years, MIS:open) | 53.5:52.6 | 63.10:67.40 | 66.4:64.1 | 46:51 | 49:48 | 54.1:52.5 |
| Gender (% male; MIS:open) | 32.0:36.0 | 10:50 | 43.1:39.5 | 60:58.8 | 50:47 | 52.2:50.0 |
| Diagnosis (MIS:open) | ||||||
| DDD | 15:11 | 30:34 | 18:25 | 12:14 | ||
| Spondylolisthesis | 50:50 | 12:12 | 22:35 | 11:24 | ||
| Others | 29:27 | |||||
| Inclusion/exclusion criteria | Inclusion Patients need to have evidence on magnetic resonance imaging of Grade I degenerative lumbar spondylolisthesis; Have mechanical low back pain and radicular symptoms Unresponsive to at least 6 weeks of conservative therapy Age 18–70 years Exclusion Undergone a previous back operation An extraspinal cause of back pain or sciatica An active medical or workman’s compensation lawsuit Any pre-existing spinal pathology Unwilling or unable to participate with follow-up procedures |
Inclusion Patients were Grades I or II spondylolisthesis presenting with mechanical low back pain, radiculopathy, and/or neurogenic claudication Preoperative evaluation with static (antero-posterior and lateral) and dynamic (flexion- extension) plain L-S spine radiography and MRI Patients had failed conservative management (minimum 6 months) before surgery Exclusion NR |
Inclusion: Two-level fusions were needed between L3 and S1 Persistent or recurrent low back pain or leg pain lasting at least 6 months and resulting in a significant reduction of quality of life, despite conservative therapy, including physical therapy and pain management Segmental instability was >4 mm of translation or 10 of angular motion on preoperative flexion-extension radiographs Exclusion Patients associated with previous spinal surgery, lumbar fracture, active infection, severe osteoporosis, and severe obesity Combination of coronal and/or sagittal deformities that needed a surgical correction Degenerative spondylolisthesis with major instability or isthmic spondylolisthesis Any major psychological problem |
Inclusion Symptomatic and refractory to prior conservative treatment low back pain with or without unilateral leg pain Single-level DDD or degenerative I grade spondylolisthesis documented with both X-Ray and MRI of the lumbar spine Minimum follow-up period after operation 6 months Exclusion: Patients with DDD or degenerative spondylolisthesis at more than one level Patients with spinal stenosis with neurogenic claudication or bilateral leg pain Patients with isthmic spondylolisthesis Patients with <12 months follow-up Patients who had previously undergone spinal surgery |
Inclusion Patients who underwent single-level TLIF for DDD or degenerative low-grade (1 or 2) spondylolisthesis Exclusion Patients who underwent a multi-level TLIF and the patients with a history of lumbar arthrodesis |
Inclusion NR Exclusion Age <18 years BMI <30.0 kg/m2 TLIF of >1 level Patients who have undergone additional spinal instrumentation Patients who have undergone posterior fusion beyond 1 vertebra above and below the site of TLIF |
| Clinical outcome | OPT, MBL, LOS, complications, VAS, ODI, SF-12, QALY, EQ-5D | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | MBL, LOS, complications |
| Definition fusion/evaluation measure | NR | Grades I or II (Bridwell interbody fusion grading System)/plain film and CT of the L-S spine at 24 months | Grades I or II (Bridwell interbody fusion grading system)/radiographs (AP and lateral images) at 12 months | NR/posterior-anterior and lateral view as well as dynamic X-rays of the lumbar spine (max flexion - max extension) at 12 months | Bony bridging anterior to the cage and bony continuity between the two endplates through the cage/CT scan at 12 months | NR |
| Surgical information | ||||||
| Number of segments treated | One (50:50) | One (12:12) | Two (44:38) | One (30:34) | One (40:60) | One (23:38) |
| Level of fusion | ||||||
| L4–L5 | 32:30 | 11:7 | 23:24 7:10 | NR | 9:17 8:17 6:4 | |
| L5 to S1 | 14:17 | 1:3 | ||||
| Others | 4:3 | 0:2 | 44:38 | |||
| Interbody device | Cage | Cage | PEEK cage | PEEK cage | PEEK cage | PEEK cage |
| Graft use | Autologous | Autologous | Autologous | Autologous | Autologous (30) BCP (30 + 40) | Autologous |
| Screw use | Bilateral | Bilateral | Bilateral | Unilateral | Bilateral | Bilateral |
| Characteristics | Rodríguez-Vela et al.[19] | Yang et al.[33] | Lee et al.[16] | Lau et al.[15] | Wang et al[34] | Liang et al.[35] |
| Year of publication | 2013 | 2013 | 2012 | 2011 | 2011 | 2011 |
| Study design | Prospective cohort | Retrospective cohort | Prospective cohort | Retrospective cohort | Randomized controlled trial | Retrospective cohort |
| Class of evidence* | III | III | II | III | I | III |
| Number of enrolled patient (MIS:open) | 41 (21:20) | 147 (43:104) | 144 (72:72) | 22 (10:12) | 79 (41:38) | 87 (42:45) |
| Mean follow-up time (months; MIS:open) | 45.0:45.0 | 21:23 | 24.0:24.0 | 15.2:12.6 | 32.7:32.7 | 33.6:34.8 |
| Follow-up rate (%, months) (MIS:open) | 100:100 (36) NR (>36) | 100:100 (18) NR (>18) | 95.8:100 (6) 95.8:91.7 (24) | 100:100 (12) NR (>12) | 100:100 (24) NR (>24) | 100:100 (26) NR (>26) |
| Mean age (years, MIS:open) | 41.81:43.15 | 55:52 | 52.2:56.6 | 46.9:56.9 | 51.4:57.3 | 49.8:51.3 |
| Gender (% male; MIS:open) | 66.7:65.0 | 34.9:35.6 | 27.8:30.6 | 40.0:42.0 | 65.9:60.5 | 54.8:57.8 |
| Diagnosis (MIS:open) | ||||||
| DDD | 21:20 | 23:52 | NR | 5:6 | 30:24 11:14 | 42:45 |
| Spondylolisthesis | 20:52 | 4:6 | ||||
| Others | 1:0 | |||||
| Inclusion/exclusion criteria | Inclusion Patients without previous medical conditions, who underwent a one-level TLIF 6 months of failed nonoperative treatment or neurologic deficit progression DDD Exclusion: Patients with lumbar stenosis or isthmic spondylolisthesis |
Inclusion Diagnosis of either lumbar DDD, degenerative spondylolisthesis, or spinal stenosis No response to nonoperative treatments for 3 months Patients had clinic dates with at least 18 months of follow-up |
Inclusion Single-level TLIF (open or MIS) MIS cases utilizing sextant ITM (Medtronic, MN) pedicle screw-rod instrumentation and capstone (Medtronic MN) interbody cage Exclusion Previous spinal instrumentation |
NR | Inclusion Unilateral or bilateral lower limb pain, numbness, or symptoms of intermittent claudication, with or without significant low back pain Imaging studies showing single-level lumbar disc herniation, spinal stenosis, or spondylolisthesis 6 months of regular conservative treatment without relief of symptoms Informed consent |
Inclusion Diagnosis of either lumbar DDD, degenerative spondylolisthesis, or spinal stenosis Imaging studies showing single-level lumbar disc herniation, spinal stenosis or spondylolisthesis |
| Previous lumbar spine surgery (except single discectomy) Presence of MRI degenerative changes in other lumbar levels | Exclusion Undergone a previous back operation Any pre-existing spinal pathology Any major psychological problem |
Tumor spinal pathologies Spinal infections Acute spinal trauma | Exclusion Multisegment lumbar disc herniation, spinal stenosis or, abnormal vertebral alignment Severe osteoporosis or other metabolic bone disease Fractured vertebra, cracked pedicle, or a congenital, isthmic or other abnormal bone structure Infection in the intervertebral space or other areas Previous surgical treatment of segmental defects Severe systemic disease which contraindicated surgery Consent not given |
Exclusion Undergone a previous back operation Any pre-existing spinal pathology Any major psychological problem |
||
| Clinical outcome | Complications, VAS, ODI, SF-36, NASS | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, ODI, fusion rate, SF-36, NASS, ambulation time | ORT, MBL, complications, ambulation time, postoperative drainage, pain outcome scores | OPT, MBL, LOS, complications, VAS, ODI | ORT, MBL, complications, VAS, ODI, fusion rate |
| Definition fusion/evaluation measure | NR | Fusion was defined as Brantigan–Steffee classification D or E, translation movement <2 mm and SA <5°/dynamic flexion-extension lumbar radiographs in conjunction with a CT scan within the 12 months | The fusion was defined as Grades I or II. (Bridwell interbody fusion grading system)/static and dynamic plain at 6 months and 24 months | NR | NR | NR |
| Surgical information | ||||||
| Number of segments treated | One (21:20) | One (43:104) | One (72:72) | One (9:7) Two (1:5) | One (41:38) | One (42:45) |
| Level of fusion | ||||||
| L4–L5 | NR | 24:63 | 54:49 | 5:6 | 11:15 | 21:21 |
| L5 to S1 | 17:39 | 14:17 | 4:1 | 11:10 | 16:11 | |
| Others | 2:2 | 4:6 | 1:5 | 0:1 | 5:7 | |
| Interbody device | CIO®/CAPASTONE® | Cage | PEEK/titanium cage | Cage | PEEK cage | PEEK cage |
| Graft use | Autologous | Autologous and DBM | Autologous | Autologous | Autologous | PMMA |
| Screw use | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral |
| Characteristics | Shunwu et al.[22] | Wang et al.[24] | Villavicencio et al.[23] | Schizas et al.[21] | Dhall et al.[13] | Scheufler et al.[20] |
| Year of publication | 2010 | 2010 | 2010 | 2009 | 2008 | 2007 |
| Study design | Prospective cohort | Prospective cohort | Retrospective cohort | Prospective cohort | Retrospective cohort | Retrospective cohort |
| Class of evidence* | II | III | III | III | III | III |
| Number of enrolled patient (MIS:open) | 62 (32:30) | 85 (42:43) | 139 (76:63) | 36 (18:18) | 42 (21:21) | 94 (43:51) |
| Mean follow-up time (months; MIS:open) | 24.0:24.0 | 26.3:26.3 | 37.5:37.5 | 22.0:24.0 | 24.0:34.0 | 16.0:16.0 |
| Follow-up rate (%, months) (MIS:open) | 96:93 (24) NR (>24) |
100:100 (13) NR (>13) |
100:100 (24) NR (>24) |
100:100 (12) NR (>12) |
100:100 (>12) 38:62 (>24) 19:38 (>36) |
100:100 (16) |
| Mean age (years, MIS:open) | 51.4:52.0 | 47.9:53.2 | 50.5:58.9 | 45.5:48.1 | 53.0:53.0 | 52.6:53.4 |
| Gender (% male; MIS:open) | 56.3:46.7 | 30.1:37.2 | 38.0:45.0 | NR | NR | 45.2:47.8 |
| Diagnosis (MIS:open) | ||||||
| DDD | 14:8 | NR | 2:6 | 14:10 | 18:25 | |
| Spondylolisthesis | 5:8 | 24:22 | 15:12 | 7:11 | 33:37 | |
| Others | 3:4 | 18:21 | 1:0 | |||
| Inclusion/exclusion criteria | Inclusion One-level pathological process Patients were confirmed by antero-posterior and lateral plain radiographs, (CT) scans, and (MRI) Have low back pain, with varying degrees of radiating pain and neurologic symptoms Unresponsive or inadequate to 6 months of conservative therapy Exclusion Patients with previous spinal surgery |
Inclusion Patients with degenerative or isthmic spondylolisthesis Patients presented low back pain as their predominant complaint, with varying degrees of radiating pain, neurological complaints, or a combination of these Unresponsive to at least 3 months of conservative therapy Exclusion NR |
Inclusion At least 24 months of follow-up Patients were confirmed by antero-posterior and lateral plain radiographs, (CT) scans, and (MRI) Unresponsive to at least 6 months of conservative therapy; unless their symptoms were progressive or existed in conjunction with major spinal instability confirmed in imaging studies Exclusion NR |
NR | Inclusion Single-level DDD or degenerative Grade I spondylolisthesis Exclusion NR Inclusion Single-level DDD or degenerative Grade I spondylolisthesis Exclusion NR |
Inclusion Patients presented with either axial back pain, neurogenic claudication, radiculopathy, pseudoradicular pain, or a combination of these Unresponsive to at least 3 months of conservative therapy Exclusion NR |
| Clinical outcome | OPT, MBL, LOS, complications, VAS, ODI, fusion rate, ambulation time, postoperative drainage | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, VAS, fusion rate, MacNab’s criteria | OPT, MBL, LOS, complications, VAS, ODI, fusion rate | OPT, MBL, LOS, complications, fusion rate, mPS scores | OPT, MBL, VAS, fusion rate, Roland-Morris low back pain, AAOS-lumbar spine questionnaire |
| Definition fusion/evaluation measure | Bony trabeculation crossed the cages or endplate interfaces/CT scans at 6 months | Trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, and <4° segmental movement/static and dynamic plain X-rays at 6 months | Trabecular bone bridging on the CT scans and less than a 5° difference in angular motion between flexion and extension, and/or no radiolucency lines >2 mm in thickness covering more than 50% of the superior or inferior surface of the grafts on the plain radiographs/CT scans or plain radiographs | NR/CT scans at 12 months | NR/dynamic radiographs and with CT scans in questionable cases at 12 months | Formation of trabecular bony bridges between contiguous vertebral bodies at the instrumented levels/2-mm thin-slice CT scans at 16 months |
| Surgical information | ||||||
| Number of segments treated | One (32:30) | One (42:43) | One (47:57) Two (16:19) | NR | One (21:21) | One (43:51) |
| Level of fusion | ||||||
| L4–L5 | 20 : 16 | 21 : 23 | NR | NR | NR | |
| L5 to S1 | 11 : 12 | 18 : 17 | 12 : 11 | |||
| Others | 1 : 2 | 3 : 3 | ||||
| Interbody device | Titanium cage | PEEK cage | Structural allograft | PEEK cage | Cage | PEEK cage |
| Graft use | Autologous | Autologous | Autologous | Autologous | Autologous | Autologous |
| Screw use | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral |
*Class of evidence was assessed by Oxford Centre for Evidence-based Medicine-Levels of Evidence (March 2009). MIS: Minimally invasive surgery; Open:open surgery; CT: Computed tomography; MRI: Magnetic resonance imaging; BCP: Biphasic calcium phosphate; PEEK: Polyether ether ketone; DBM: Demineralized bone matrix; PM: Polymethyl methacrylic; OPT: Operation time; MBL: Mean blood loss; LOS: Length of hospital stay; VAS: Visual analog score; ODI: Oswestry Disabilities Index; SF-36: Short Form 36 Health Survey; SF-12: Short Form 12 Health Survey; NASS: North American Spine Society; EQ-5D: EuroQol-5D; AAOS: American Academy of Orthopedic Surgeons; mPS: Modified Prolo Scale; NR: Not report; DDD: Degenerative disc disease; JOA: Japanese Orthopaedic Association Scores; L-S: Lumbo-sacral; TLIF: Transforaminal lumbar interbody fusion.
We also compared the baseline of the 24 included studies. One study considered nine aspects when comparing the two groups, five studies considered eight aspects, twelve studies considered seven aspects, three studies considered six aspects, two studies considered five aspects, and one study considered three aspects. However, there were different factors in the same number of aspects in the comparison of the MIS and open groups. There were significant differences between groups in several study variables, including the number of patients in both groups in eight studies, the mean age in one study and gender in one study. The other baseline characteristics were not significantly different between the two groups in the included studies [Table 2].
Table 2.
Comparison of baseline characteristics between the MIS group and open group
| Studies | Gender | Mean age | BMI | Number of enrolled patients | Level of surgery | Comorbidity | Preoperative diagnosis | Preoperative pain score | Preoperative function score |
|---|---|---|---|---|---|---|---|---|---|
| Wong et al.[25] | NS | NS | NR | S | NS | NR | NS | NS | NS |
| Sulaiman and Singh[30] | S | NS | NS | S | S | NR | NS | NS | NS |
| Tian et al.[31] | NS | NS | NS | NS | NS | NR | NS | NS | NS |
| Singh et al.[18] | NS | NS | NR | NS | NS | NR | NS | NS | NR |
| Chu et al.[36] | NS | NS | NR | S | NS | NR | NS | NS | NS |
| Zheng et al.[32] | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Saetia et al.[29] | S | NS | NS | NS | NS | NR | NS | NS | NS |
| Gu et al.[28] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Brodano et al.[27] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Zairi et al.[26] | NS | NS | NR | S | NS | NR | NS | NS | NS |
| Lau et al.[14] | NS | NS | NS | S | NS | NS | NS | NR | NR |
| Rodríguez-Vela et al.[19] | NS | NS | NR | NS | NS | NR | NR | NS | NS |
| Parker et al.[17] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Yang et al.[33] | NS | NS | NR | S | NS | NR | NS | NS | NS |
| Lee et al.[16] | NS | NS | NS | NS | NS | NR | NS | NS | NS |
| Lau et al.[15] | NS | S | NR | NS | NS | NR | NS | NR | NS |
| Wang et al.[34] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Liang et al.[35] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Shunwu et al.[22] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Wang et al.[24] | NS | NS | NR | NS | NS | NR | NS | NS | NS |
| Villavicencio et al.[23] | NS | NS | NR | S | NS | NR | NR | NS | NR |
| Schizas et al.[21] | NR | NR | NR | NS | NR | NR | NR | NS | NS |
| Dhall et al.[13] | NS | NS | NR | NS | NR | NR | NS | NR | NS |
| Scheufler et al.[20] | NS | NS | NR | S | NS | NS | NS | NS | NS |
BMI: Body mass index; NS: No statistical significance (P>0.05); S: Statistical significance (P<0.05); NR: Not report; MIS: Minimally invasive surgery.
Methodological quality assessment
There were one Level I evidence study, three Level II evidence studies, and twenty Level III evidence studies according to the previously described assessment criteria for class of evidence.
Meta-analysis results
Functional outcomes
Multiple measurements were used to assess the patient functional outcome, such as lower back and/or leg pain VAS (VAS-BP/LP), ODI, EuroQol-5D, Japanese Orthopaedic Association Scores (JOA), Short Form 12 Health Survey or Short Form 36 Health Survey; however, the most reported measurements were the VAS-BP/LP and ODI. Thus, we selected these variables as the functional outcome standard. The mean preoperative VAS-LP was MIS: open = 7.0:6.9; the VAS-BP was MIS: open = 6.9:6.9; and the ODI was MIS: open = 49:50. The details are shown in Table 3, and there were no significant differences between the groups.
Table 3.
Preoperative VAS-BP/LP score and ODI of included studies (MIS: open), mean±SD
| Studies | VAS-BP | VAS-LP | ODI |
|---|---|---|---|
| Wong et al.[25] | 6.37:6.72 | 8.90:8.82 | 52.8:51.2 |
| Sulaiman and Singh[30] | 7.3 ± 0.91:7.3 ± 1.41 | NR | 53.7 ± 6.32:57.8 ± 9.41 |
| Tian et al.[31] | 4.86 ± 1.16:4.87 ± 1.29 | 6.35 ± 1.41:6.41 ± 1.32 | 43.56 ± 4.85:44.71 ± 5.42 |
| Singh et al.[18] | 6.94 ± 1.85:7.67 ± 1.29 | NR | NR |
| Chu et al.[36] | 7.64 ± 0.78:7.64 ± 0.78 | NR | 62.15 ± 4.51:59.17 ± 5.05 |
| Zheng et al.[32] | 4.9 ± 2.5:5.4 ± 2.2 | 6.6 ± 2.4:6.0 ± 2.8 | 23.3 ± 10.2:23.8 ± 9.0 |
| Saetia et al.[29] | 8.75 ± 1.60:7.92 ± 1.62 | NR | 61.80 ± 12.89:58.33 ± 15.96 |
| Gu et al.[28] | 7.3 ± 1.2:7.4 ± 1.0 | 7.6 ± 0.9:7.7 ± 0.9 | 43.7 ± 4.3:44.3 ± 5.2 |
| Brodano et al.[27] | 7.8 ± 1.4:8.1 ± 1.5 | NR | 42 ± 6.2:46 ± 7.1 |
| Zairi et al.[26] | 7.3:7.2 | 7.1:6.8 | 60:60 |
| Rodríguez-Vela et al.[19] | 7.04 ± 1.12:7.19 ± 2.21 | 7.31 ± 2.05:7.53 ± 1.23 | 28.85 ± 5.52:27.19 ± 8.19 |
| Parker et al.[17] | 8.1 ± 2.6:8.5 ± 2.2 | 6.5 ± 3.6:6.9 ± 3.3 | 32.3 ± 6.7:34.3 ± 7.9 |
| Yang et al.[33] | 7.79 ± 0.88:7.71 ± 0.86 | NR | 57.95 ± 4.61:58.17 ± 5.05 |
| Lee et al.[16] | 6.3 ± 2.9:6.3 ± 2.9 | 5.8 ± 3.3:6.2 ± 3.1 | 48.1 ± 18.8:44.4 ± 18.0 |
| Wang et al.[34] | 4.9 ± 1.0:5.0 ± 1.0 | NR | 58.8 ± 6.7:57.8 ± 6.7 |
| Liang et al.[35] | 5.7 ± 1.3:5.6 ± 1.4 | 7.1 ± 1.3:7.2 ± 1.3 | 80.9 ± 6.8:81.3 ± 7.5 |
| Shunwu et al.[22] | 6.8 ± 1.2:6.8 ± 1.4 | NR | 49.7 ± 11.8:52 ± 12 |
| Wang et al.[24] | 7.2 ± 2.1:7.4 ± 1.6 | NR | 41.2 ± 6.6:38.5 ± 7.4 |
| Villavicencio et al.[23] | 7.4:8.0 | NR | NR |
| Schizas et al.[21] | 7.7:5.0 | NR | 55:53 |
VAS-BP/LP: Visual analog score-back pain/leg pain; ODI: Oswestry Disabilities Index; SD: Standard deviation; NR: Not report; MIS: Minimally invasive surgery.
Twenty studies reported the VAS-BP; however, four studies only reported a mean VAS-BP score. Statistical analysis was feasible after standardization pooling to compare the functional outcome. The pooled postoperative analysis indicated that the MIS group had a significantly lower mean VAS-BP compared with the open group (WMD = −0.44; 95% CI: −0.71 to −0.18; P = 0.001; random-effects model) [Figure 2]. In addition, nine studies reported the VAS-LP, including seven studies that reported the mean and standard deviation (SD) score. Statistical analysis was feasible after standardization pooling to compare the functional outcome. The pooled postoperative analysis indicated that the MIS group had a lower score; however, there was no significant difference between the groups (WMD = −0.10; 95% CI: −0.27 to 0.08; P = 0.26; random-effects model) [Figure 2].
Figure 2.

Forest plot: postoperative VAS-BP/LP and ODI. MIS: Minimally invasive surgery; Open: Open surgery; VAS-BP/LP: Visual analog score-back pain/leg pain; ODI: Oswestry Disabilities Index; CI: Confidence interval; SD: Standard deviation.
Eighteen studies reported the ODI score; however, only 15 studies provided the mean and SD of the ODI. Statistical analysis was feasible after standardization pooling to compare the functional outcome. The pooled postoperative analysis indicated that the MIS group had a significantly lower ODI score compared with the open group (WMD = −1.57; 95% CI: −2.66 to −0.48; P = 0.005; random-effects model) [Figure 2].
To more effectively compare both the procedures, we also pooled the mean VAS-LP, VAS-BP, and ODI improvement [Table 4]. The findings suggested that the MIS group exhibited a better outcome compared with the open procedure; the mean VAS-LP, VAS-BP, and ODI improvement were 0.2, 0.5, and 2.9, respectively.
Table 4.
Comparison between the MIS group and open group
| Mean | Fusion rate (%) | Complication rate (%) | Reoperation rate (%) | VAS-LP improvement | VAS-BP improvement | ODI improvement | MBL (ml) | OPT (min) | LOS (days) | Ambulation time (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| MIS (overall) | 95.9 | 15.1 | 0.4 | 5.2 | 4.7 | 31.6 | 224.4 | 195 | 5.1 | 1.9 |
| Open (overall) | 97.7 | 16.4 | 0.5 | 5.0 | 4.2 | 28.7 | 506.8 | 198 | 6.9 | 3.7 |
MIS: Minimally invasive surgery; Open: Open surgery; OPT: Operation time; MBL: Mean blood loss; LOS: Length of hospital stay; VAS-BP/LP: Visual analog score-back pain/leg pain; ODI: Oswestry Disabilities Index.
Operation time
Twenty-two studies reported the mean operation time; however, only 15 studies provided both the mean and SD of the operation time. Statistical analysis was feasible after standardization pooling to compare the functional outcome. The pooled postoperative analysis indicated that MIS had similar operation time to open group (WMD = −5.23; 95% CI: −50.55 to 40.09; P = 0.82; random-effects model) [Figure 3].
Figure 3.
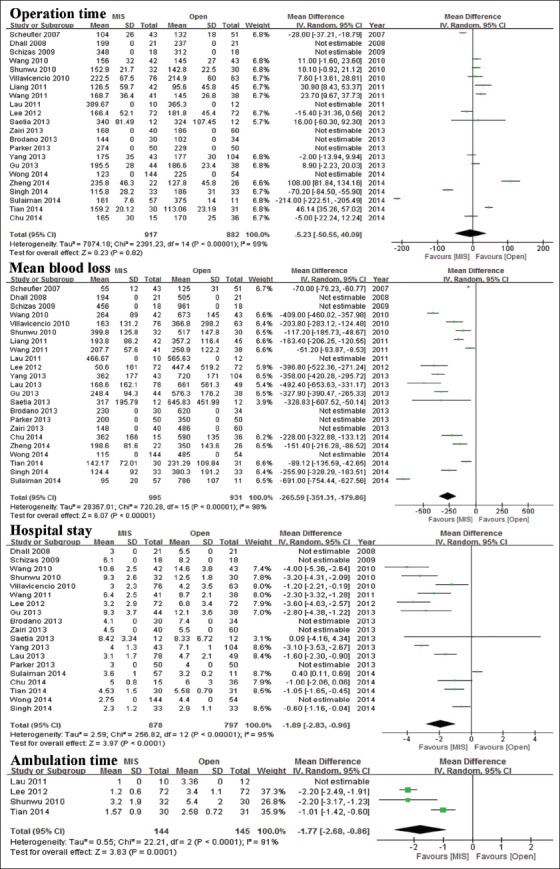
Forest plot: Operation time, mean blood loss, hosptial stay, and ambulation time. MIS: Minimally invasive surgery; Open: Open surgery; CI: Confidence interval; SD: Standard deviation.
We also compared the overall mean surgical operation time between the groups [Table 4]. The findings indicated that the operation time of the two groups was basically the same (MIS: open = 195:198).
Mean blood loss
Twenty-three studies reported the mean blood loss for both the MIS and open-TLIF procedures; however, seven studies did not provide the mean and SD of the mean blood loss. Statistical analysis was feasible after standardization pooling to compare the functional outcome. The findings indicated that there was less blood loss in the MIS group. The pooled analysis suggested that the MIS group had significantly less blood loss compared with the open group (WMD = −265.59; 95% CI: −351.31 to −179.86; P < 0.00001; random-effects model) [Figure 3].
We also compared the overall mean surgery estimation of blood loss between the groups [Table 4]. The findings indicated that MIS-TLIF was associated with less blood loss (224.4 ml) and reduced bleeding (506.8 ml).
Length of hospital stay
Twenty-one studies reported the mean length of stay; however, only 15 studies provided the mean and SD of the hospital stay. Statistical analysis was feasible after standardization pooling to compare the functional outcome. Nineteen studies indicated a shorter hospital stay in the MIS group. Our pooled analysis suggested that the MIS group had a significantly shorter length of stay compared with the open group (WMD = −1.89; 95% CI: −2.83 to −0.96; P < 0.0001; random-effects model) [Figure 3].
We also compared the overall mean length of stay between the groups [Table 3]. The findings suggested that MIS-TLIF decreased the hospital stay about 2 days compared with open-TLIF.
Ambulation time
Four studies reported the ambulation time; however, one study did not report the mean and SD. Statistical analysis was feasible after standardization pooling to compare the functional outcome. All studies indicated a shorter time to ambulate in the MIS group. The pooled analysis suggested that the MIS group had a significantly shorter ambulation time compared with the open group (WMD = −1.77; 95% CI: −2.68 to −0.86; P = 0.0001; random-effects model) [Figure 3].
Fusion rate
Sixteen studies reported the fusion rate from a minimum of 6 months to a maximum of 24 months. Fusion was assessed with the use of dynamic flexion-extension radiographs and/or computed tomography scan. However, only 13 studies reported the fusion definition. The fusion rate was 95.9% (658/686) in the MIS-TLIF group and 97.7% (668/684) in the open-TLIF group. There was no significant difference in the fusion rate between the two groups (RR = 0.99; 95% CI: 0.97–1.01; P = 0.34; random-effects model) [Figure 4].
Figure 4.

Forest plot: Fusion rate, complication rate, and reoperation rate. MIS: Minimally invasive surgery; Open: Open surgery; CI: Confidence interval.
Complication rate
Twenty-two studies reported the complication rate. The complication rate was 15.1% (142/940) in the MIS-TLIF group and 16.4% (142/867) in the open-TLIF group. The pooled analysis suggested that the MIS group had a lower complication rate; however, there was no significant difference between the two groups (RR = 0.84; 95% CI: 0.58–1.21; P = 0.35; random-effects model) [Figure 4].
Reoperation rate
Thirteen studies reported the reoperation rate. The reoperation rate was 0.4% (34/788) in the MIS-TLIF group and 0.5% (37/767) in the open-TLIF group. The pooled analysis suggested that the MIS group had a lower reoperation rate; however, there was no significant difference between the two groups (RR = 0.73; 95% CI: 0.39–1.35; P = 0.32; random-effects model) [Figure 4].
DISCUSSION
To determine the efficacy of both treatments, we analyzed the relative information as much detail as possible. Our findings indicated that MIS-TLIF had a better performance in all fields with the exception of the fusion rate [Table 4]. The meta-analysis suggested that MIS-TLIF attained a similar fusion rate, with a significantly shorter hospital stay and quicker ambulation, as well as less blood loss compared with open-TLIF. Patients suffered fewer lesions with less blood loss. MIS-TLIF resulted in quicker rehabilitation and less complications because patients exhibited earlier ambulation, as well as lower medical costs and a shorter hospital stay. For clinical functional outcomes, the preoperative baseline variables were similar between the groups, and the pooled analysis suggested that the MIS group exhibited significantly lower postoperative VAS and ODI scores compared with the open group. Thus, MIS-TLIF resulted in better outcomes and less trauma. These findings are consistent with the studies by Wu et al.[4] and Tian et al.[5]
Despite the many fusion technologies, TLIF has become a widely accepted and familiar surgical approach, which decreases the relative nervous complication rate.[54,55,56] However, open-TLIF technology also requires splitting of the paraspinal muscle. Although it does not hurt, it breaks a major section of the posterior compartment, which may result in relevant muscle complications and low back pain.[57] Therefore, minimally invasive TLIF was introduced by Foley and Lefkowitz[58] approximately 10 years ago. To date, it has become an increasingly accepted approach with advantages, compared with traditional open surgery, that are attributed to decreased damage to spinal soft tissues and paravertebral muscles.[20,56,59]
The advantages associated with MIS-TLIF may be attributed to the less intraoperative dissection and retraction of paravertebral muscles.[4,5,8,60]
Our meta-analysis indicated that MIS-TLIF was associated with a shorter operation time and lower complication and reoperation rate; however, there was no significant difference between MIS and open-TLIF, which is consistent with the findings of Tian et al.[5] Nevertheless, it is interesting that the compilation and reoperation rate were significantly decreased in the MIS group compared with the open-TLIF group. As shown in Figure 5, there are several potential reasons for this phenomenon; one major reason may be that the learning curve is very steep and it requires more years and experience to absorb and master minimally invasive surgery skills.[5,13,15,21] The other major one may be possible with surgical devices and the development of equipment.
Figure 5.
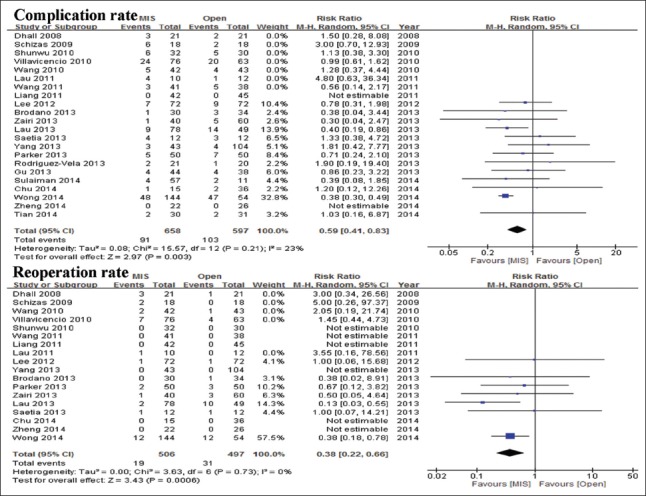
Forest plot: Complication rate and reoperation rate. MIS: Minimally invasive surgery; Open: Open surgery; CI: Confidence interval.
There are several potential weaknesses in our meta-analysis. First, we included only prospective and retrospective studies in this study; thus, methodological defects were inevitable in these studies and included incorrect blinding or nonblinding, data bias, insufficient baseline comparisons, and insufficient data collection. Second, there were fewer outcome measures in the current study; additional objective or subjective parameters should be used to estimate the clinical outcomes. Third, the fusion definition and judgment were different across the included studies. Moreover, many of the studies comprised short- or medium-term research. Additional, long-term, follow-up studies should be conducted to evaluate both the approaches. Finally, there was unavoidable bias when the data were pooled. Despite these limitations, this updated meta-analysis provides an important clinical reference for the field.
In conclusion, the current meta-analysis indicated that MIS-TLIF resulted in a similar fusion rate with better functional outcome, less blood loss, shorter ambulation, and hospital stay. Furthermore, MIS-TLIF was not associated with an increase in the complication or reoperation rate based on the existing evidence. Thus, we recommend minimally invasive surgery as the first option if the patient meets the indication because it results in fewer lesions, better outcome, and a similar fusion rate compared with the traditional open surgery. Interestingly, MIS-TLIF has been associated with significantly decreased complication and reoperation rate in the recent years. We suggest that this finding is a result of greater acceptance in using MIS-TLIF, familiarity with the procedure, the ability to grasp and master minimally invasive surgery skills, and the relevant development of surgical instructions and apparatuses. Additional, high-quality studies are needed to confirm these findings and further compare the two methods.
Supplementary information is linked to the online version of the paper on the Chinese Medical Journal website.
Financial support and sponsorship
This work was supported by grants from the Science and Technology Commission of Shanghai Municipality (No. 12411951000) and the New Advanced Technologies of Shanghai Municipal Hospitals Joint Research Projects (No. SHDC1203108).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg. 1953;10:154–68. doi: 10.3171/jns.1953.10.2.0154. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 2.Schwender JD, Hsu BC. Minimally invasive posterior surgery for the lumbar spine. In: Bridwell KH, editor. The Textbook of Spinal Surgery. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2011. pp. 1076–7. [Google Scholar]
- 3.Lowe TG, Tahernia AD, O’Brien MF, Smith DA. Unilateral transforaminal posterior lumbar interbody fusion (TLIF): Indications, technique, and 2-year results. J Spinal Disord Tech. 2002;15:31–8. doi: 10.1097/00024720-200202000-00005. doi: 10.1097/00024720-200202000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Wu RH, Fraser JF, Härtl R. Minimal access versus open transforaminal lumbar interbody fusion: Meta-analysis of fusion rates. Spine (Phila Pa 1976) 2010;35:2273–81. doi: 10.1097/BRS.0b013e3181cd42cc. doi: 10.1097/BRS.0b013e3181cd42cc. [DOI] [PubMed] [Google Scholar]
- 5.Tian NF, Wu YS, Zhang XL, Xu HZ, Chi YL, Mao FM. Minimally invasive versus open transforaminal lumbar interbody fusion: A meta-analysis based on the current evidence. Eur Spine J. 2013;22:1741–9. doi: 10.1007/s00586-013-2747-z. doi: 10.1007/s00586-013-2747-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun ZJ, Li WJ, Zhao Y, Qiu GX. Comparing minimally invasive and open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: A meta-analysis. Chin Med J. 2013;126:3962–71. doi: 10.3760/cma.j.issn.0366-6999.20131539. [PubMed] [Google Scholar]
- 7.Houten JK, Post NH, Dryer JW, Errico TJ. Clinical and radiographically/neuroimaging documented outcome in transforaminal lumbar interbody fusion. Neurosurg Focus. 2006;20:E8. doi: 10.3171/foc.2006.20.3.9. doi: 10.3171/foc.2006.20.3.9. [DOI] [PubMed] [Google Scholar]
- 8.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28:S26–35. doi: 10.1097/01.BRS.0000076895.52418.5E. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. doi: 10.1371/journal.pmed.1000100.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang L, Wang Y, Li Z, Yu B, Li Y. Unilateral versus bilateral pedicle screw fixation of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF): A meta-analysis of randomized controlled trials. BMC Surg. 2014;14:87. doi: 10.1186/1471-2482-14-87. doi: 10.1186/1471-2482-14-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furlan AD, Pennick V, Bombardier C, van Tulder M Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 12.Brain Trauma Foundation; American Association of Neurological Surgeons;Congress of Neurological Surgeons;Joint Section on Neurotrauma and Critical Care, AANS/CNS Carney NA. Guidelines for the management of severe traumatic brain injury. Methods. J Neurotrauma. 2007;24(Suppl 1):S3–6. doi: 10.1089/neu.2007.9996. doi: 10.1089/neu.2007.9996. [DOI] [PubMed] [Google Scholar]
- 13.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up: Clinical article. J Neurosurg Spine. 2008;9:560–5. doi: 10.3171/SPI.2008.9.08142. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 14.Lau D, Khan A, Terman SW, Yee T, La Marca F, Park P. Comparison of perioperative outcomes following open versus minimally invasive transforaminal lumbar interbody fusion in obese patients. Neurosurg Focus. 2013;35:E10. doi: 10.3171/2013.5.FOCUS13154. doi: 10.3171/2013.5.focus13154. [DOI] [PubMed] [Google Scholar]
- 15.Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF) J Clin Neurosci. 2011;18:624–7. doi: 10.1016/j.jocn.2010.09.004. doi: 10.1016/j.jocn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21:2265–70. doi: 10.1007/s00586-012-2281-4. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: Comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82:230–8. doi: 10.1016/j.wneu.2013.01.041. doi: 10.1016/j.wneu.2013.01.041. [DOI] [PubMed] [Google Scholar]
- 18.Singh K, Nandyala SV, Marquez-Lara A, Fineberg SJ, Oglesby M, Pelton MA, et al. A perioperative cost analysis comparing single-level minimally invasive and open transforaminal lumbar interbody fusion. Spine J. 2014;14:1694–701. doi: 10.1016/j.spinee.2013.10.053. doi: 10.1016/j.spinee.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 19.Rodríguez-Vela J, Lobo-Escolar A, Joven E, Muñoz-Marín J, Herrera A, Velilla J. Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Eur Spine J. 2013;22:2857–63. doi: 10.1007/s00586-013-2853-y. doi: 10.1007/s00586-013-2853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007;60(4 Suppl 2):203–12. doi: 10.1227/01.NEU.0000255388.03088.B7. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]
- 21.Schizas C, Tzinieris N, Tsiridis E, Kosmopoulos V. Minimally invasive versus open transforaminal lumbar interbody fusion: Evaluating initial experience. Int Orthop. 2009;33:1683–8. doi: 10.1007/s00264-008-0687-8. doi: 10.1007/s00264-008-0687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–20. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 23.Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010;1:12. doi: 10.4103/2152-7806.63905. doi: 10.4103/2152-7806.63905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19:1780–4. doi: 10.1007/s00586-010-1404-z. doi: 10.1007/s00586-010-1404-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong AP, Smith ZA, Stadler JA, 3rd, Hu XY, Yan JZ, Li XF, et al. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): Surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am. 2014;25:279–304. doi: 10.1016/j.nec.2013.12.007. doi: 10.1016/j.nec.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Zairi F, Arikat A, Allaoui M, Assaker R. Transforaminal lumbar interbody fusion: Comparison between open and mini-open approaches with two years follow-up. J Neurol Surg A Cent Eur Neurosurg. 2013;74:131–5. doi: 10.1055/s-0032-1330956. doi: 10.1055/s-0032-1330956. [DOI] [PubMed] [Google Scholar]
- 27.Brodano GB, Martikos K, Lolli F, Gasbarrini A, Cioni A, Bandiera S, et al. Transforaminal lumbar interbody fusion in degenerative disc disease and spondylolisthesis grade I: Minimally invasive versus open surgery. J Spinal Disord Tech. 2013;3(Suppl 5):S355–61. doi: 10.1097/BSD.0000000000000034. doi: 10.1097/BSD.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 28.Gu G, Zhang H, Fan G, He S, Cai X, Shen X, et al. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop. 2014;38:817–24. doi: 10.1007/s00264-013-2169-x. doi: 10.1007/s00264-013-2169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saetia K, Phankhongsab A, Kuansongtham V, Paiboonsirijit S. Comparison between minimally invasive and open transforaminal lumbar interbody fusion. J Med Assoc Thai. 2013;96:41–6. [PubMed] [Google Scholar]
- 30.Sulaiman WA, Singh M. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis grades 1-2: Patient-reported clinical outcomes and cost-utility analysis. Ochsner J. 2014;14:32–7. doi: 10.1043/1524-5012-14.1.32. [PMC free article] [PubMed] [Google Scholar]
- 31.Tian W, Xu YF, Liu B, Liu YJ, He D, Yuan Q, et al. Computer-assisted minimally invasive transforaminal lumbar interbody fusion may be better than open surgery for treating degenerative lumbar disease. J Spinal Disord Tech. 2016 doi: 10.1097/BSD.0000000000000165. In Press]. doi: 10.1097/BSD.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 32.Zheng Y, Li WS, Chen ZQ, Qi Q, Guo ZQ, Yan Z, et al. The minimal invasive posterior transforminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion in the treatment of single level lumbar spine degenerative diseases (in Chinese) Chin J Spine Spinal Cord. 2014;24:1064–71. doi: 10.3969/j.issn.1004-406X.2014.12.03. [Google Scholar]
- 33.Yang J, Kong Q, Song Y, Liu H, Zeng J. Comparison of short-term effectiveness between minimally invasive surgery- and open-transforaminal lumbar interbody fusion for single-level lumbar degenerative disease (in Chinese) Chin J Repar Reconstr Surg. 2013;27:262–7. doi: 10.7507/1002-1892.20130061. [PubMed] [Google Scholar]
- 34.Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL, Wang LX. Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: A prospective randomized clinical trial. Chin Med J. 2011;124:3868–74. doi: 10.3760/cma.j.issn.0366-6999.2011.23.007. [PubMed] [Google Scholar]
- 35.Liang B, Yin G, Zhao J, Li N, Hu Z. Surgical treatment of degenerative lumbar instability by minimally invasive transforaminal lumbar interbody fusion (in Chinese) Chin J Repar Reconstr Surg. 2011;25:1449–54. [PubMed] [Google Scholar]
- 36.Chu YW, Cheng L, Zhu HM, Ding T. Comparison of the curative effect of minimally invasive transforaminal lumber interbody fusion via channel and traditional operation in treating single-level lumber degenerative disease (in Chinese) J Trauma Surg. 2014;16:307–10. [Google Scholar]
- 37.Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24:479–84. doi: 10.1097/BSD.0b013e3182055cac. doi: 10.1097/BSD.0b013e3182055cac. [DOI] [PubMed] [Google Scholar]
- 38.Villavicencio AT, Burneikiene S, Nelson EL, Bulsara KR, Favors M, Thramann J. Safety of transforaminal lumbar interbody fusion and intervertebral recombinant human bone morphogenetic protein-2. J Neurosurg Spine. 2005;3:436–43. doi: 10.3171/spi.2005.3.6.0436. doi: 10.3171/spi.2005.3.6.0436. [DOI] [PubMed] [Google Scholar]
- 39.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385–9. doi: 10.1097/BRS.0b013e3181a4e3be. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 40.Parker SL, Adogwa O, Bydon A, Cheng J, McGirt MJ. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg. 2012;78:178–84. doi: 10.1016/j.wneu.2011.09.013. doi: 10.1016/j.wneu.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 41.Wang J, Zhou Y, Feng Zhang Z, Qing Li C, Jie Zheng W, Liu J. Comparison of the clinical outcome in overweight or obese patients after minimally invasive versus open transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2014;27:202–6. doi: 10.1097/BSD.0b013e31825d68ac. doi: 10.1097/BSD.0b013e31825d68ac. [DOI] [PubMed] [Google Scholar]
- 42.Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo W, Tan SB, et al. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: A matched-pair comparison study. Spine (Phila Pa 1976) 2013;38:2049–55. doi: 10.1097/BRS.0b013e3182a8212d. doi: 10.1097/BRS.0b013e3182a8212d. [DOI] [PubMed] [Google Scholar]
- 43.Zaïri F, Allaoui M, Thines L, Arikat A, Assaker R. Transforaminal lumbar interbody fusion: Goals of the minimal invasive approach. Neurochirurgie. 2013;59:171–7. doi: 10.1016/j.neuchi.2013.05.002. doi: 10.1016/j.neuchi.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 44.Adogwa O, Johnson K, Min ET, Issar N, Carr KR, Huang K, et al. Extent of intraoperative muscle dissection does not affect long-term outcomes after minimally invasive surgery versus open-transforaminal lumbar interbody fusion surgery: A prospective longitudinal cohort study. Surg Neurol Int. 2012;3(Suppl 5):S355–61. doi: 10.4103/2152-7806.103868. doi: 10.4103/2152-7806.103868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Terman SW, Yee TJ, Lau D, Khan AA, La Marca F, Park P. Minimally invasive versus open transforaminal lumbar interbody fusion: Comparison of clinical outcomes among obese patients. J Neurosurg Spine. 2014;20:644–52. doi: 10.3171/2014.2.SPINE13794. doi: 10.3171/2014.2.SPINE13794. [DOI] [PubMed] [Google Scholar]
- 46.Pelton MA, Phillips FM, Singh K. A comparison of perioperative costs and outcomes in patients with and without workers’ compensation claims treated with minimally invasive or open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2012;37:1914–9. doi: 10.1097/BRS.0b013e318257d490. doi: 10.1097/BRS.0b013e318257d490. [DOI] [PubMed] [Google Scholar]
- 47.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Minimally invasive or open transforaminal lumbar interbody fusion as revision surgery for patients previously treated by open discectomy and decompression of the lumbar spine. Eur Spine J. 2011;20:623–8. doi: 10.1007/s00586-010-1578-4. doi: 10.1007/s00586-010-1578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Archavlis E, Carvi y Nievas M. Comparison of minimally invasive fusion and instrumentation versus open surgery for severe stenotic spondylolisthesis with high-grade facet joint osteoarthritis. Eur Spine J. 2013;22:1731–40. doi: 10.1007/s00586-013-2732-6. doi: 10.1007/s00586-013-2732-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oliveira DD, Rosa MG, Machado WD, Falcon RS. Comparison of the results of MIS-TLIF and open TLIF techniques in laborers. Coluna/Columna. 2014;13:124–8. doi: 10.1590/S1808-18512014130200337. [Google Scholar]
- 50.Cheng JS, Park P, Le H, Reisner L, Chou D, Mummaneni PV. Short-term and long-term outcomes of minimally invasive and open transforaminal lumbar interbody fusions: Is there a difference? Neurosurg Focus. 2013;35:E6. doi: 10.3171/2013.5.FOCUS1377. doi: 10.3171/2013.5.focus1377. [DOI] [PubMed] [Google Scholar]
- 51.Ding RH, Liu B, Zhang B, Wang YQ, Xiao B, Su HT. Minimally invasive versus open transforaminal lumbar interbody fusion in the treatment of single-level lumbar disc herniation (in Chinese) Chin J Tissue Eng Res. 2013;17:5452–9. doi: 10.3969/j.issn.2095-4344.2013.30.006. [Google Scholar]
- 52.Zhang HL, Gu X, He SS, Gu GF, Zhang LG, Ding Y, et al. Minimally invasive transforaminal lumbar interbody fusion versus posterior open-surgery in treatment of lumbar spondylolisthesis (in Chinese) Chin J Orthop. 2011;31:1088–92. doi: 10.3760/cma.j.issn.0253-2352.2011.10.017. [Google Scholar]
- 53.Wang J, Zhou Y, Zhang ZF, Li CQ, Ren XJ, Chu TW, et al. Clinical study on lumbar spondylolisthesis treated by minimally invasive transforaminal lumbar interbody fusion (in Chinese) Chin J Surg. 2011;49:1076–80. doi: 10.3760/cma.j.issn.0529-5815.2011.12.005. [PubMed] [Google Scholar]
- 54.Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002;33:359–66. doi: 10.1016/s0030-5898(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 55.Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: A safe technique with satisfactory three to five year results. Eur Spine J. 2005;14:551–8. doi: 10.1007/s00586-004-0830-1. doi: 10.1007/s00586-004-0830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–6. doi: 10.1097/01.bsd.0000132291.50455.d0. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 57.Tsahtsarlis A, Wood M. Minimally invasive transforaminal lumber interbody fusion and degenerative lumbar spine disease. Eur Spine J. 2012;21:2300–5. doi: 10.1007/s00586-012-2376-y. doi: 10.1007/s00586-012-2376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002;49:499–517. [PubMed] [Google Scholar]
- 59.Mummaneni PV, Rodts GE., Jr The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005;57(4 Suppl):256–61. doi: 10.1227/01.neu.0000176408.95304.f3. doi: 10.1227/01.NEU.0000176408.95304.F3. [DOI] [PubMed] [Google Scholar]
- 60.Karikari IO, Isaacs RE. Minimally invasive transforaminal lumbar interbody fusion: A review of techniques and outcomes. Spine (Phila Pa 1976) 2010;v35(26 Suppl):S294–301. doi: 10.1097/BRS.0b013e3182022ddc. doi: 10.1097/BRS.0b013e3182022ddc. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Funnel plots: Complication rate. SE: Standard error; RR: Relative risk.


